Abstract
The differential diagnosis of true aneurysms and pseudoaneurysms is challenging, and multimodality cardiac imaging is often necessary. We report a case in which the limitations of these techniques are exposed, showing that post-operative evaluation of tissue layers remains the gold standard in establishing this diagnosis. (Level of Difficulty: Beginner.)
Key Words: anterior myocardial infarction, echocardiography, cardiac magnetic resonance, case report, pseudoaneurysm, ventricular aneurysm
Abbreviations and Acronyms: CMR, cardiac magnetic resonance; CMVO, coronary microvascular obstruction; HF, heart failure; LV, left ventricular; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NYHA, New York Heart Association; STEMI, ST-segment elevation myocardial infarction; TTE, transthoracic echocardiogram
Graphical abstract
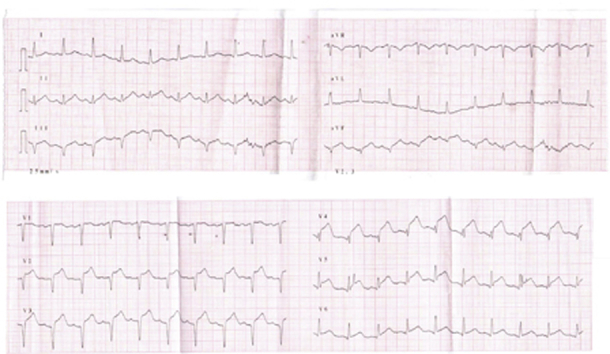
We report the case of a 55-year-old woman who was admitted to the cardiac intensive care unit due to anterior wall myocardial infarction (MI) (Figure 1). Primary percutaneous coronary intervention of the middle segment occlusion of the left anterior descending artery was successfully performed 1 h and 45 min after the onset of chest pain (Videos 1 and 2). Transthoracic echocardiogram (TTE) revealed reduced left ventricular (LV) ejection fraction (LVEF 30%), with akinesia of the anterior and septal walls as well as all apical segments (Figure 2A, Video 3). Hospitalization was complicated by heart failure (HF) (Killip-Kimball class II) and epistenocardiac pericarditis for which she was treated with furosemide and acetylsalicylic acid 1,000 mg 8/8 h. She was discharged clinically stable after 4 days (Figure 3), medicated with acetylsalicylic acid, ticagrelor 90 mg twice daily, ramipril 2.5 mg, bisoprolol 5 mg, ivabradine 5 mg twice daily, furosemide 40 mg twice daily, spironolactone 25 mg, and atorvastatin + ezetimibe 20 mg + 10 mg.
Learning Objectives
-
•
To recognize the development of true and false aneurysm as a mechanism of HF.
-
•
To understand the role and limitations of multimodality imaging in the differentiation between true and false LV aneurysm.
-
•
To discuss the mechanisms of adverse remodeling after complete revascularization in STEMI.
Figure 1.
First Electrocardiogram Revealing ST-Segment Elevation, V2 to V6
Figure 2.
Echocardiographic Evolution in Apical 4-Chamber View
(A) Day 3; (B) day 10; (C) day 19; and (D) day 27.
Figure 3.
Electrocardiogram at Discharge
Two days after discharge, the patient was readmitted due to worsening HF symptoms and recurrence of pleuritic chest pain. The TTE performed showed an apical thrombus and small circumferential pericardial effusion with a maximum diameter of 7 mm (Figure 2B, Video 4). A decision was made to start anticoagulation with warfarin along with dual antiplatelet therapy (aspirin and clopidogrel). The patient was discharged 17 days later after clinical stabilization. TTE at discharge showed worsened LV dilation and dysfunction (indexed volume 85 ml/m2 and LVEF 28%), an apical aneurysm with organized thrombus, and a small circumferential pericardial effusion (8 mm posterior, 7 mm anterior) (Figure 2C, Video 5).
One week later, the patient was re-evaluated in the outpatient clinic, and she presented in New York Heart Association (NYHA) functional class III.
Medical History
The patient had a history of arterial hypertension and former smoking habits.
Differential Diagnosis
In a patient who presents with HF symptoms after an MI, the differential diagnosis should include consideration of nonoptimized or poor adherence to medication, mechanical complications, adverse remodeling, and other HF decompensation factors (e.g., pulmonary thromboembolism, infections).
Investigations
The patient assured compliance to medication and had no other decompensation factors. TTE was performed and revealed a significant increase in LV dimensions (indexed volume 102 ml/m2), a further decline in systolic function (LVEF 21%), and a small pericardial effusion. In apical 4-chamber view, we identified a linear structure (42 mm × 5 mm) attached to the endocardial border of the apical segments of the anterolateral and septal walls, of undefined nature. The apical segments were dyskinetic and had a very thin wall, findings that could correspond to an aneurysm or pseudoaneurysm (Figure 2D, Videos 6 and 7).
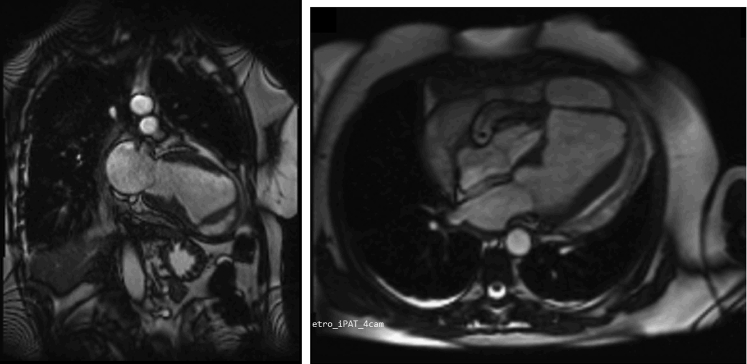
To clarify these results, the patient underwent cardiac magnetic resonance (CMR) imaging, which showed extensive anterior myocardial necrosis and severely depressed LV systolic function (LVEF 25%), suggesting rupture of the mid-distal transition of the interventricular septum (with no visible connection to the right ventricle), compatible with a large apical pseudoaneurysm. Moreover, the mid-distal segments of the septum presented a central zone of marked subendocardial hypo-signal, suggesting microvascular obstruction (Figures 4 and 5, Videos 8 and 9).
Figure 4.
Cardiac Magnetic Resonance Evaluation
2 chambers on the left; 4 chambers on the right.
Figure 5.

Late Gadolinium Enhancement on Cardiac Magnetic Resonance
Management
The case was discussed within the heart team, and it was decided to perform urgent cardiac surgery, due to the unpredictable onset of rupture and potential for complications (Video 10). However, surgical exploration revealed integrity of the septal and free walls, and the preoperative diagnosis was discarded. The patient underwent an aneurysmectomy, with no further complications (Video 11). Histological examination confirmed the presence of a thin myocardial wall with marked fibrosis and recent mural thrombus, compatible with the diagnosis of a ventricular aneurysm.
Discussion
LV aneurysm and pseudoaneurysm formation is a known consequence after acute MI, particularly in extensive MI and late presentation (1), but its prevalence has been drastically reduced due to the wide availability of percutaneous reperfusion therapy (2). In contrast to true aneurysms, which are often medically managed, LV pseudoaneurysms require urgent surgical intervention due to their higher propensity for progressive growth and rupture (2,3). The differential diagnosis of true aneurysms and pseudoaneurysms is challenging, and multimodality cardiac imaging is often necessary to establish the correct diagnosis and to help guide patient management. However, these imaging techniques are not without limitations and, occasionally, a definitive diagnosis is only found during surgical exploration and histological examination.
The patient had access to primary percutaneous coronary intervention and complete revascularization <2 h after the onset of chest pain. Because she remained symptomatic, repeated echocardiography detected an image suggestive of an incidental pseudoaneurysm 1 month after the index event. This case highlights the fast remodeling of the left ventricle that may occur after an ST-segment elevation MI (STEMI) (3) and the importance of performing early and regular echocardiography revaluation, especially in patients who remain symptomatic and have severe LV dysfunction. Also, myocardial rupture and pseudoaneurysms might occur even weeks after the index event (4). The mechanisms of adverse remodeling in a patient completely revascularized after just a few hours of evolution remain to be explained, but coronary microvascular obstruction (CMVO) could play a significant role. CMVO has been shown to be related to the no-reflow phenomenon and to adversely affect the prognosis of a revascularized STEMI, even if thorough and timely (5,6). Interestingly, the CMR of this patient showed findings compatible with CMVO.
Pseudoaneurysms rarely form at the apical segment of the left ventricle; they are more common at the posterior and inferior walls (1,4). In fact, the anterior-apical location is more often associated with true aneurysms. CMR offers noninvasive high spatial resolution and good tissue characterization. Although both types of aneurysms show late gadolinium enhancement in the wall of the aneurysmal sac, the pericardial enhancement signal is more common in pseudoaneurysms (2). In this patient, despite the preoperative diagnosis of pseudoaneurysm, corroborated by CMR imaging, surgical findings were compatible with a giant LV aneurysm. Surgery could also be considered in the case of a true aneurysm to relieve HF symptoms, as in this case; 1 year after surgical intervention, the patient remains in NYHA functional class II (7).
Follow-Up
The patient was discharged clinically stable and maintains follow-up at the cardiology outpatient clinic at our institution. She remains in NYHA functional class II.
Conclusions
The differential diagnosis between LV aneurysm or pseudoaneurysm is difficult but essential, as it entails distinct therapeutic approaches. CMR and other imaging tests are very useful in this differentiation. This case reveals that, even with significant advances in high-spatial resolution imaging modalities, post-operative evaluation of tissue layers remains the gold standard in this diagnosis.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose. The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Acknowledgment
The authors thank Pedro Cordeiro for the acquisition of the CMR images and for the review of the final paper. They also acknowledge Câmara Municipal de Loulé for the support provided.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Coronary Angiogram Before Percutaneous Coronary Intervention
Coronary Angiogram After Percutaneous Coronary Intervention
Echocardiogram at Day 3
Echocardiogram at Day 10
Echocardiogram at Day 10
Echocardiogram at Day 27 (Four Chambers)
Echocardiogram at Day 27 (Two Chambers)
Cardiac Magnetic Resonance (Four Chambers)
Cardiac Magnetic Resonance (Two Chambers)
Echocardiogram Before Discharge to Cardiac Surgery (Day 33), Showing Further Enlargement of the “Pseudoaneurysm”
Surgical Exploration
References
- 1.Prifti E., Bonacchi M., Baboci A. Surgical treatment of post-infarction left ventricular pseudoaneurysm: case series highlighting various surgical strategies. Ann Med Surg. 2017;16:44–51. doi: 10.1016/j.amsu.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benoit A., Davin L., Bruyère P.J. Une complication rare du syndrome coronarien aigu: ventriculaire gauche. Rev Med Liege. 2019;74:375–377. [PubMed] [Google Scholar]
- 3.Das A.K., Wilson G.M., Furnary A.P. Coincidence of true and false left ventricular aneurysm. Ann Thorac Surg. 1997;64:831–834. doi: 10.1016/s0003-4975(97)00758-3. [DOI] [PubMed] [Google Scholar]
- 4.Niemann M., Hermann M., Jacobs S. The third ventricle—a case of a giant post infarct pseudoaneurysm. Int J Cardiol. 2014;177:e93–e96. doi: 10.1016/j.ijcard.2014.09.090. [DOI] [PubMed] [Google Scholar]
- 5.Niccoli G., Scalone G., Lerman A., Crea F. Coronary microvascular obstruction in acute myocardial infarction. Eur Heart J. 2016;37:1024–1033. doi: 10.1093/eurheartj/ehv484. [DOI] [PubMed] [Google Scholar]
- 6.Sezer M., Van Royen N., Umman B. Coronary microvascular injury in reperfused acute myocardial infarction: a view from an integrative perspective. J Am Heart Assoc. 2018;7:1–16. doi: 10.1161/JAHA.118.009949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruzza A., Czer L.S.C., Arabia F.A. Left ventricular reconstruction for postinfarction left ventricular aneurysm: review of surgical techniques. Tex Heart Inst J. 2017;44:326–335. doi: 10.14503/THIJ-16-6068. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronary Angiogram Before Percutaneous Coronary Intervention
Coronary Angiogram After Percutaneous Coronary Intervention
Echocardiogram at Day 3
Echocardiogram at Day 10
Echocardiogram at Day 10
Echocardiogram at Day 27 (Four Chambers)
Echocardiogram at Day 27 (Two Chambers)
Cardiac Magnetic Resonance (Four Chambers)
Cardiac Magnetic Resonance (Two Chambers)
Echocardiogram Before Discharge to Cardiac Surgery (Day 33), Showing Further Enlargement of the “Pseudoaneurysm”
Surgical Exploration