Abstract
Swallow (deglutition) syncope is a rare form of neurally mediated cardioinhibitory reflex syncope occurring during swallowing. Patients may present to clinicians across multiple disciplines, so high awareness and careful evaluation are essential. We report 3 such individuals, describing our strategies in diagnosis, investigation and treatment, particularly focusing on conservative management. (Level of Difficulty: Intermediate.)
Key Words: cardio-inhibition, deglutition, neurally mediated, swallow, syncope
Abbreviations and Acronyms: CNA, cardioneuroablation; ECG, electrocardiogram
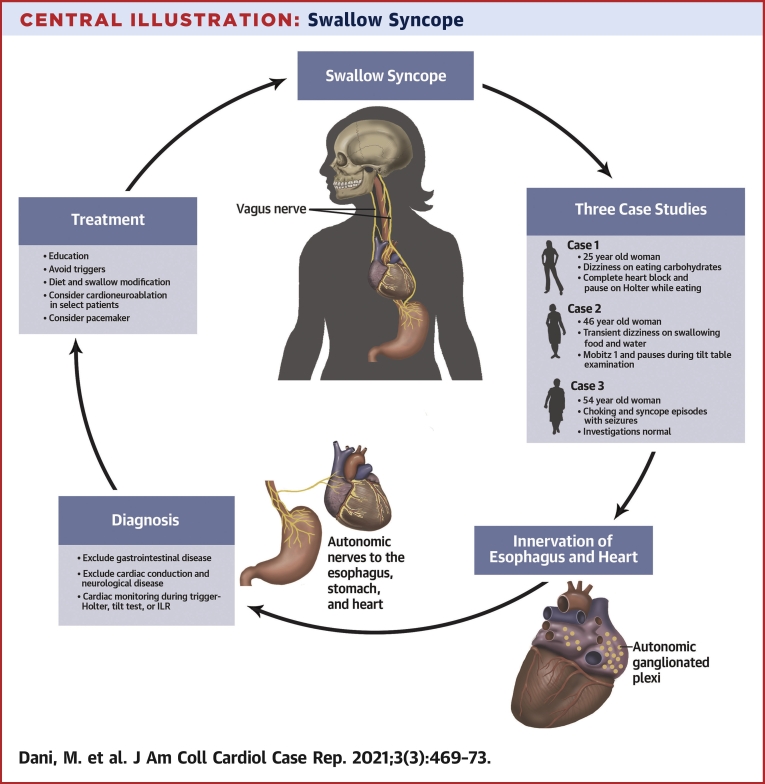
Central Illustration
Case 1
A 25-year-old healthy woman presented with episodes of transient light-headedness during eating since 12 years of age. Culprit foods were sausage rolls, sandwiches, Scotch eggs, and bananas. She was able to drink fluids without difficulty. Her symptoms improved with a modified low-carbohydrate and gluten-free diet, but she still experienced 3 to 7 episodes per week. She also noted that her symptoms were markedly worse in hot weather and when she was dehydrated. She had a younger brother with similar symptoms, but he had declined medical consultation.
Learning Objectives
-
•
Swallow syncope is a rare form of reflex neural syncope. A careful history and investigation strategy are required to make and confirm the diagnosis.
-
•
Swallow syncope should prompt the clinician to consider and exclude gastrointestinal disease.
-
•
Patient education, with a focus on conservative management, may be sufficient to effectively treat symptoms.
Baseline electrocardiogram (ECG), echocardiogram and brain magnetic resonance imaging findings were normal. There was a low suspicion for gastrointestinal pathology, so investigations for this were not performed. A 24-h Holter electrocardiogram revealed a pause of 4.3 s, which corresponded with eating a sandwich.
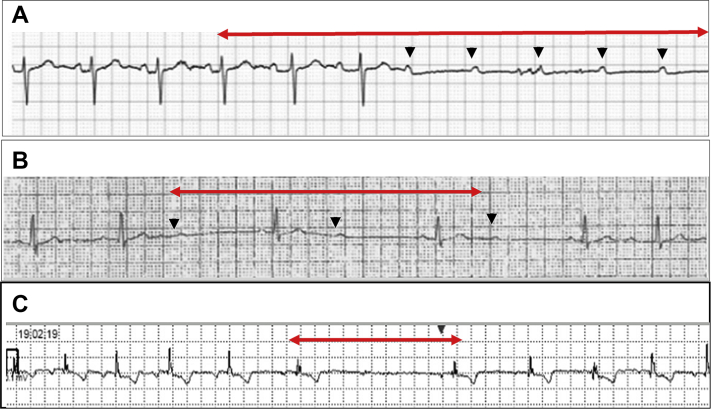
During continuous blood pressure and ECG monitoring, she ate potential precipitants such as a sausage roll and a sandwich. ECG monitoring showed a progressive prolongation of the PR interval followed by transient complete atrioventricular block and a pause of 2.7 s. Later, when she was eating a Scotch egg, she developed complete atrioventricular block with a pause of 4.5 s (Figure 1A) associated with mild light-headedness.
Figure 1.
ECG Recordings During Swallow Syncope
(A) Progressive prolongation of the PR interval, followed by a pause (red arrow) while the patient in Case 1 was eating a Scotch egg. The black arrows indicate nonconducted P waves. (B) Mobitz I atrioventricular block of 2:1 at first but of 3:2 Wenckebach in recovery while the patient in Case 2 was eating (red arrow). The black arrows indicate nonconducted P waves during the 2:1 phase. (C) A symptomatic 3-s pause in case 2.
A diagnosis of neurally mediated cardioinhibitory swallow syncope was made. Intervention was considered because she was still symptomatic despite diet modification. Pacemaker implantation was deemed inappropriate in view of a lifelong risk of pacemaker complications. Participation in a randomized controlled trial offering cardioneuroablation (CNA) was suggested, but she felt that her symptoms were manageable with a modified diet and adequate hydration and opted for conservative management.
Several aspects of this case are striking. First, her younger brother experienced identical symptoms, raising the possibility of a hereditary component. This has not previously been reported to our knowledge. Second, the precipitant foods were very specific (and were mostly dry, making them more difficult to swallow) (1). Finally, her symptoms were worse in hot weather, particularly when dehydrated and after exercise, suggesting an important role for conservative strategies such as hydration. Her symptoms improved significantly with conservative management. They were not fully eradicated, however, as she reported an occasional desire to eat bread. However, she achieved an acceptable balance of occasional bread consumption for pleasure, accepting the risk of syncope. This remains her preferred management option.
Case 2
An otherwise healthy 46-year-old woman reported episodes of light-headedness for the preceding 18 months. These episodes occurred 1 or 2 times per day, usually (but not always) during eating and swallowing liquids.
Physical examination, ECG, and echocardiogram findings were unremarkable. Results of a cardiac magnetic resonance imaging scan (performed to exclude an infiltrative disease resulting in an arrhythmia) were also normal. A 24-h Holter monitor revealed an episode of Mobitz I atrioventricular block, which corresponded to her evening meal (Figure 1B) and was associated with dizziness, which was interpreted as pre-syncope. An implantable loop recorder was inserted, recording a 3-s pause during eating (Figure 1C).
She was reviewed by a gastroenterologist, and no obvious gastrointestinal pathology was identified. Therapeutic strategies were considered. Both the patient and her clinical team believed that the long-term risks of pacemaker implantation outweighed the benefits. However, she remained troubled by her symptoms. She therefore underwent electrophysiological studies, which revealed no evidence of infranodal conduction disease. The patient was subjected to vagal maneuvers such as the Valsalva maneuver and being asked to swallow a mouthful of sandwich, but this did not result in atrioventricular block. This study suggested that she may be a candidate for CNA.
While completing her investigations, she modified her diet and swallowing, resulting in her symptoms significantly ameliorating to a frequency of 1 or 2 times per month. She thus opted for continuing a conservative strategy but allowing further consideration of ablation if her symptoms recurred.
The diagnosis in this case was readily apparent on investigation. It highlights the effectiveness of patient education and empowering each patient in managing his or her symptoms.
Case 3
A 54-year-old woman presented with recurrent syncope after choking episodes for the preceding 2 years. She described stereotyped episodes of a sensation of food getting “stuck,” prompting her to drink fluid to dislodge the food bolus. This would be followed by a sudden collapse without warning. Episodes were associated with loss of consciousness lasting up to a minute and both fecal and urinary incontinence. Witnesses denied limb convulsions or pallor or flushing but noted that she was drowsy on waking. She occasionally vomited after the episodes.
She had undergone multiple abdominal operations for colitis. She took no medications.
ECG, echocardiogram, and 24-h Holter monitor findings were unremarkable. Upper gastrointestinal endoscopy showed mild reflux esophagitis, and a barium swallow revealed mild esophageal dysmotility.
Head-up tilt table test findings were normal (this included swallowing, but the patient was too fearful to eat precipitating foods), so an implantable loop recorder was inserted. However, by the time she had these investigations, she had modified her symptoms significantly by choosing soft foods and improving her hydration. She also adopted a “slow cooking” food preparation method that involves cooking food (particularly meat) on a low heat for a long time, resulting in more tender meat that is easier to swallow. These measures eradicated her symptoms. No arrhythmias have been recorded to date.
This case highlights that despite a highly suggestive history for swallow syncope, investigations did not confirm the diagnosis because the patient had self-managed her condition. It highlights the effectiveness of conservative measures. If, however, she develops recurrent symptoms with evidence of cardioinhibition, pacemaker implantation or CNA will be considered (Central Illustration).
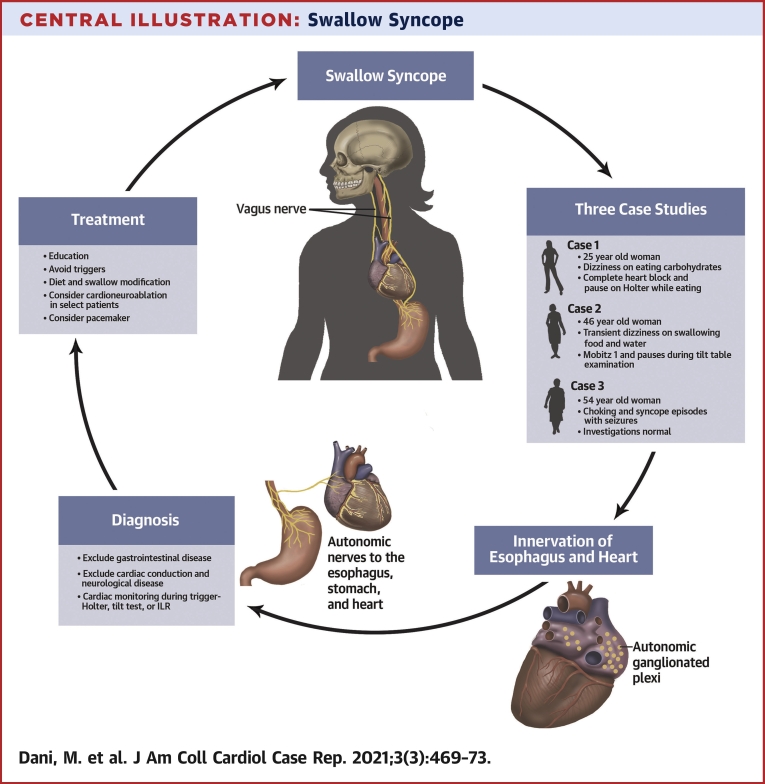
Central Illustration.
Swallow Syncope
A summary of the cases involved in this series, along with diagnosis and management.
Discussion
Swallow (deglutition) syncope is a rare form of neurally mediated situational syncope. It occurs when swallowing induces excessive vagal stimulation, leading to cardiac inhibition and bradyarrhythmias. In contrast to the individuals in this series, it has a preponderance for older men, with some case series reporting an average age of 57.5 years (1).
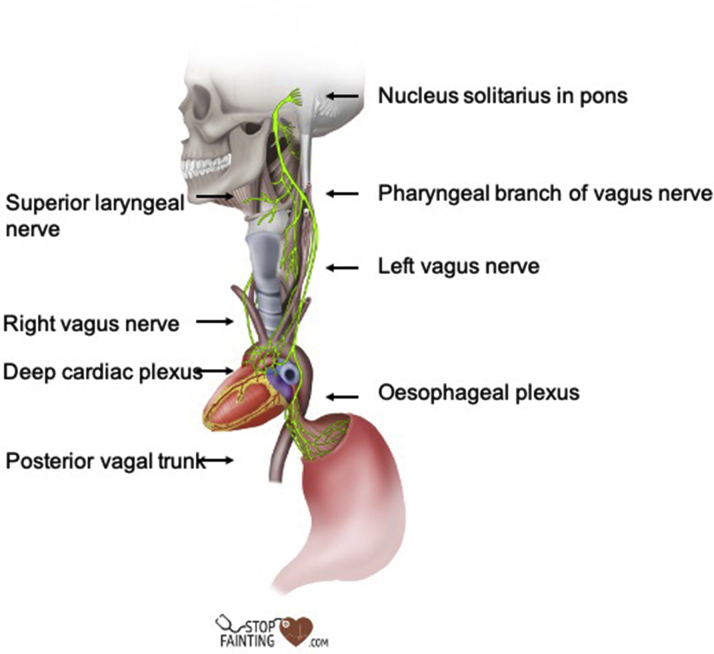
One-third of cases are associated with underlying gastrointestinal disease, particularly of the esophagus or stomach. Similarly, one-third of cases are associated with cardiac disease, and 28% with hypertension, diabetes, hypercholesterolemia, and obesity (1). The link with esophageal pathology is not coincidental—mechanoreceptors in the esophageal, pharyngeal, and laryngeal nerve plexi stimulate vagal afferent signals to the nucleus solitarius in the medulla. Vagal efferent signals then travel from the nucleus solitarius to the cardiac conduction system (Figure 2). Excessive stimulation from the esophageal afferents, for example, from esophagitis or esophageal spasm, can then lead to excessive vagal efferent stimulation and withdrawal of sympathetic tone, culminating in bradyarrhythmia, hypotension, and syncope (1). Precipitating foods may be general or specific—for example, citrus and acidic foods (1), which stimulate esophageal nociceptors. Cold and carbonated drinks are common triggers (1).
Figure 2.
Innervation of the Esophagus and Heart
Mechanoreceptors in the esophageal, pharyngeal, and laryngeal nerve plexi stimulate vagal afferent signals to the nucleus solitarius in the brainstem. Vagal efferent signals then travel from the nucleus solitarius to the cardiac conduction system. The figure is reproduced from the authors’ website (www.stopfainting.com).
Nearly one-fifth of affected cases are associated with an underlying hiatus hernia (1). The pathophysiology in these cases is related to mechanical outflow obstruction rather than cardioinhibition. As food fills the intrathoracic stomach, the left atrium becomes compressed, and cardiac output falls (2).
Treatment options are limited, as highlighted in the 3 cases described in this report. In a recent large case series of 101 cases dating from 1793 until 2019 (1), 55% of individuals underwent pacemaker implantation, with a 98% success rate in preventing syncope (1). This is in keeping with European Society of Cardiology guidelines, which recommend pacemaker implantation in individuals older than 40 years with a marked cardioinhibitory response (3). In younger individuals, there is insufficient evidence to support this, and pacemaker implantation carries significant risk related to device changes, including infective endocarditis.
Management of underlying gastrointestinal disease is essential and was the management strategy in 16% of the cases in the case series described (1). In 8 of the reported cases, atropine before eating was trialed and was effective in all but 1 individual (1). This has led some authors to recommend it as a possible approach (1). As in all the presented cases, dietary modification is very effective, and education should form a significant component of management.
Some recent case series have reported favorable outcomes from radiofrequency ablation of ganglionic plexi, containing nerves that supply the heart (4,5). Syncope frequency was reduced and pacemaker implantation was avoided in the series described. Randomized controlled trials are required before true efficacy can be determined.
Although rare, swallow syncope is debilitating, and patients may present to emergency and general physicians before cardiologists. Unless careful evaluation is performed, with detailed clinical history and ECG monitoring while the individual is exposed to potential precipitants, it can be mistaken for post-prandial syncope, cough syncope, or orthostatic hypotension. Consequently, practical and effective management strategies (including essential patient education) may be missed. Each case should be individually considered, and after the diagnosis is made, underlying causes should be promptly excluded, and an initial management strategy focused on conservative strategies should be the first step of management, as shown in Table 1.
Table 1.
Management of Swallow Syncope
| Identify and treat underlying causes—neurological, gastrointestinal, and cardiac conduction abnormalities. |
| Identify and advise avoiding specific triggers. |
| Modify swallow technique—advise smaller mouthfuls of food and chewing before swallowing. |
| If a vasovagal tendency is present, educate on conservative strategies to minimize this—increase fluid and salt intake (if the patient has low to low normal blood pressure). |
| Assess the risk of significant injury, including presence and duration of warning, frequency of symptoms, and resulting injuries. |
| Identify cardioinhibition, by assessing electrocardiograph/Holter or implantable loop recorder during provocation with typical triggering foods. |
| Even if cardioinhibition is confirmed, consider conservative strategies initially to avoid pacemaker insertion. |
| Pharmacotherapy may be trialed for symptom control—atropine before meal intake has been effective in case reports. |
| If recurrent symptoms occur despite conservative strategies, consider cardioneuroablation if the patient is young or if there is strong patient preference to avoid pacing.∗ Otherwise, consider pacemaker. |
Cardioneuroablation is not currently recommended by the syncope guidelines (1). However, the authors are of the opinion that in (particularly) young patients with debilitating symptoms, it should be explored.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Siew K.S.W., Tan M.P., Hilmi I.N., Loch A. Swallow syncope: a case report and review of literature. BMC Cardiovasc Disord. 2019;19:191–203. doi: 10.1186/s12872-019-1174-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maekawa T., Suematsu M., Shimada T., Go M., Shimada T. Unusual swallow syncope caused by huge hiatal hernia. Internal Med. 2002;41:199–201. doi: 10.2169/internalmedicine.41.199. [DOI] [PubMed] [Google Scholar]
- 3.Brignole M., Moya A., de Lange F.J. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J. 2018;39:1883–1948. doi: 10.1093/eurheartj/ehy037. [DOI] [PubMed] [Google Scholar]
- 4.Stiavnicky P., Wichterle D., Hrosova M., Kautzner J. Cardioneuroablation for the treatment of recurrent swallow syncope. Europace. 2020;22:1741. doi: 10.1093/europace/euaa060. [DOI] [PubMed] [Google Scholar]
- 5.Pachon J.C., Pachon E.I., Cunha Pachon M.Z., Lobo T.J., Pachon J.C., Santillana T.G. Catheter ablation of severe neurally meditated reflex (neurocardiogenic or vasovagal) syncope: cardioneuroablation long-term results. Europace. 2011;13:1231–1242. doi: 10.1093/europace/eur163. [DOI] [PubMed] [Google Scholar]