Abstract
Coronary spasm is a frequent cause of angina despite unobstructed coronary arteries, and symptom control with recommended drugs is limited. We report the case of a 77-year-old woman who had refractory angina despite conventional antianginal treatment. Repurposing riociguat, a soluble guanylate cyclase stimulator, resulted in improvement of symptoms and prevention of spasm. (Level of Difficulty: Intermediate.)
Key Words: acetylcholine testing, coronary artery spasm, drug repurposing, individual treatment trial, microvascular dysfunction, riociguat, soluble guanylate cyclase
Abbreviations and Acronyms: ACh, acetylcholine; ECG, electrocardiogram; LCx, left circumflex artery; sGC, soluble guanylate cyclase
Graphical abstract
History of presentation
A 77-year-old woman presented to our hospital with recurrent angina symptoms and dyspnea occurring at rest and during exertion. She had experienced these symptoms for the last 30 years, and they had led to severe impairment of her quality of life.
Learning Objectives
-
•
Patients with angina symptoms and nonobstructed coronary arteries often have a coronary vasomotor disorder.
-
•
When symptom control cannot be achieved with recommended anti-vasospastic treatments, drug repurposing on the basis of pharmacological deliberation should be considered.
-
•
sGC-stimulating agents such as riociguat may be helpful in patients with coronary artery spasm.
Past Medical History
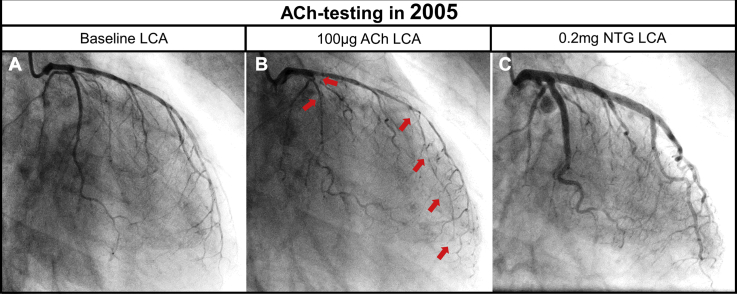
The patient’s primary presentation to our clinic dated back to 1995. At that time, the then 53-year-old woman reported already a 5-year history of chest pain at rest and exercise-related shortness of breath. She had no cardiovascular risk factors. Because of ischemic changes in an exercise electrocardiogram (ECG), she underwent diagnostic coronary angiography, which revealed unobstructed coronary arteries. In search of a coronary vasomotor disorder (coronary artery spasm), acetylcholine (ACh) provocation testing was carried out during another coronary angiogram in 2005, and it revealed diffuse epicardial coronary spasm of the left anterior descending artery and the left circumflex artery (LCx) (Figures 1A to 1C). Subsequently, anti-vasospastic treatment was initiated.
Figure 1.
ACh Provocation Testing in 2005
(A) Baseline angiogram showing an unobstructed left coronary artery (LCA). (B) Acetylcholine (ACh) testing was performed with increasing doses and intracoronary administration of 100 μg acetylcholine into the left coronary artery resulted in diffuse epicardial spasm (arrows), and (C) subsequent administration of 0.2 mg nitroglycerin led to full vasodilation of the left coronary artery.
However, the patient continued to have recurrent angina symptoms refractory to various pharmacological treatment options. Over the years, she underwent multiple cardiac diagnostic assessments, including several noninvasive stress tests, as well as 5 invasive angiograms, which (apart from one in 2013, when a focal stenosis in the LCx was found leading to stent placement) showed unobstructed coronary arteries.
In 2018, ischemic ECG changes could be observed on a resting ECG, and the patient reported increasing chest pain both during exercise and at rest. To evaluate a possible progression of coronary artery disease or an in-stent restenosis, as well as to assess coronary vasomotion again, coronary angiography was carried out, including ACh provocation testing after a standardized protocol (1). During ACh testing, microvascular coronary spasm could be observed with low doses of ACh, whereas a dose of 100 μg ACh led to diffuse epicardial coronary spasm in the left anterior descending artery similar to the previous test in 2005. However, the stent in the LCx prevented spasm at that site. Intracoronary injection of 200 μg nitroglycerin led to resolution of epicardial coronary spasm and her symptoms.
During a period of several years, various antianginal drugs were prescribed according to the guidelines of the European Society of Cardiology. These drugs included combinations of a beta-blocker, calcium-channel blockers, an angiotensin-converting enzyme inhibitor, and nitrates. Moreover, second-line drugs such as ranolazine and nicorandil did not significantly improve the patient’s symptoms.
Differential Diagnosis
Coronary artery disease and coronary vasomotor disorders were considered in the differential diagnosis.
Management
Given that the diagnosis was ascertained and recommended medical therapy options to obtain satisfactory symptom control were exhausted, we decided on an off-label use of riociguat, a drug licensed for the treatment of pulmonary hypertension. Treatment with riociguat, a stimulator of the soluble guanylate cyclase (sGC), which is an enzyme with a pivotal role in the regulation of vascular tone, was initiated under close clinical supervision. The patient was primarily discharged with 0.5 mg riociguat 3 times daily. During weekly follow-ups, we increased the dosage of riociguat stepwise up to 6 mg/day until the patient reported a significant improvement of her health status.
Investigations
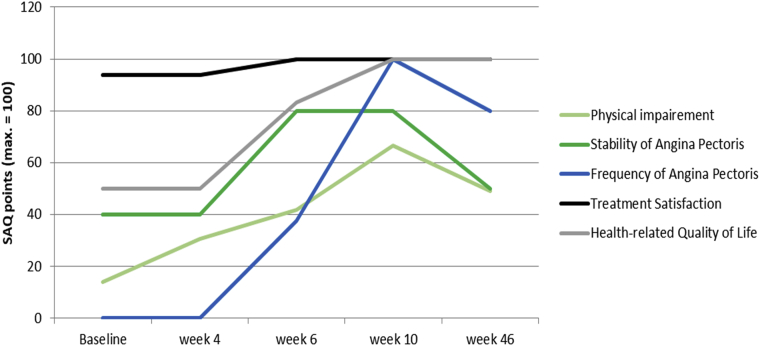
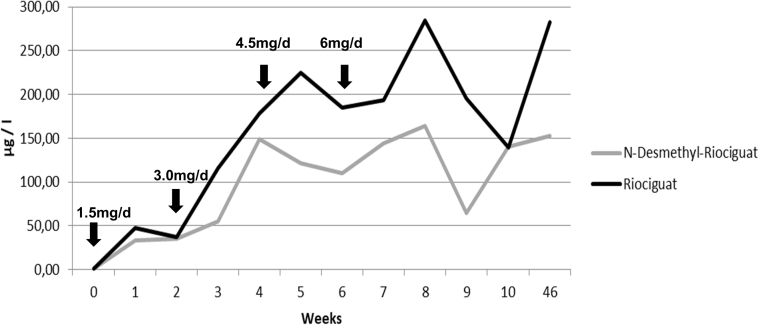
We quantitatively assessed the patient’s angina symptoms and health-related quality of life using the Seattle Angina Questionnaire during follow-up visits, as well as after a period of 10 months of riociguat treatment (6 mg/day) (Figure 2). Plasma levels of riociguat and its metabolite N-desmethyl-riociguat were analyzed using liquid chromatography with tandem mass spectrometry, resulting in a dose-dependent increase of plasma concentrations (Figure 3). Furthermore, the patient underwent repeated ACh provocation testing to validate the anti-vasospastic effect of riociguat on the coronary arteries. Strikingly, under full riociguat medication, epicardial coronary artery spasm could not be elicited with 100 μg ACh, unlike in the previous examination in 2018 (Figures 4A, 4B, and 5A to 5J).
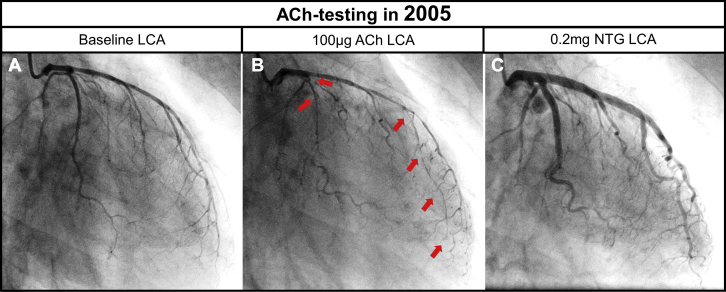
Figure 2.
Quality of Life Assessment
Seattle Angina Questionnaire (SAQ)–based assessment of quality of life during riociguat treatment (weeks 4 to 46).
Figure 3.
Riociguat and N-Desmethyl-Riociguat Plasma Concentrations
Plasma concentrations of riociguat (black) and its metabolite N-desmethyl-riociguat (gray) after stepwise dose escalation (arrows) up to 6 mg/day over a period of 46 weeks.
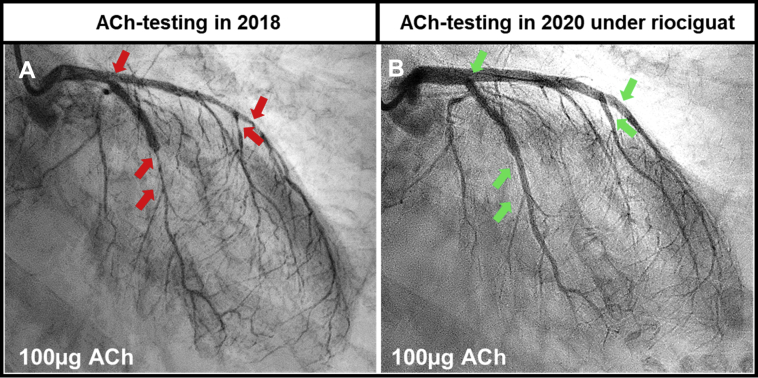
Figure 4.
ACh Provocation Testing in 2018 and 2020
Left coronary artery after intracoronary administration of 100 μg acetylcholine (ACh) (arrows)(A) in 2018 and (B) in 2020 under riociguat treatment. Under Riociguat, epicardial coronary artery spasm could not be elicited with 100 μg acetylcholine.
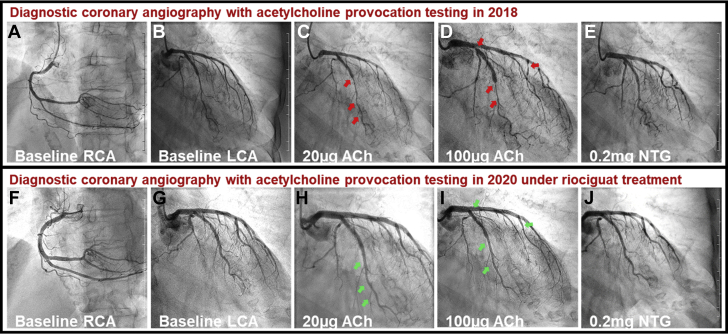
Figure 5.
Comparison of ACh Provocation Testing Outcome Without (2018) and With Riociguat (2020) in a 77-Year-Old Female Patient
Coronary angiography showing unobstructed right coronary artery (RCA) and left coronary artery (LCA) in (A and B) 2018 and (F and G) 2020. The red arrows indicate (C) diffuse epicardial spasm provoked by 20 μg acetylcholine (ACh) and (D) a combination of diffuse and focal epicardial spasm at a dose of 100 μg acetylcholine without previous riociguat treatment. Under riociguat treatment, epicardial spasm could neither be provoked with (H) 20 μg nor with (I) 100 μg acetylcholine (green arrows). (E and J) Intracoronary administration of nitroglycerin (NTG) led to full vasodilation of coronary arteries irrespective of riociguat therapy.
Discussion
Approximately 50% of patients with angina pectoris have unobstructed coronary arteries on diagnostic coronary angiography (2). In approximately 60% of these patients, the genesis of symptoms can be traced back to coronary vasomotor disorders (e.g. coronary artery spasm), which can be diagnosed with ACh provocation testing (3). A recent study showed that satisfactory symptom control often remains a challenge in these patients (4). Despite established treatments for patients with coronary spasm, including calcium-channel blockers and nitrates (5), many patients report symptoms refractory to such treatment, and new treatment options are urgently warranted. In the present case, the sGC stimulator riociguat, a substance licensed for treatment of pulmonary hypertension, resolved recurrent angina symptoms in a patient with refractory symptoms caused by coronary artery spasm. Strikingly, we observed that the drug inhibited the elicitation of epicardial coronary artery spasm with ACh in this patient. Furthermore, the patient reported a significant long-term (10 months) beneficial effect on quality of life.
These findings suggests that the sGC-pathway may be a novel therapeutic target in patients with coronary artery spasm. However, randomized controlled clinical trials are needed to reinforce this assumption.
Follow-Up
After these efforts to ameliorate the patient’s symptoms, the patient reported that she was finally almost symptom-free, leading to a significant improvement in quality of life (Figure 2).
Conclusions
Symptom control in patients with coronary spasm often remains a challenge, and available treatment options are frequently insufficient. On the basis of pathophysiological and pharmacological considerations, as well as first evidence by our case report, repurposing the sGC-stimulator riociguat appears to be a promising novel therapeutic option in patients with coronary artery spasm.
Funding Support and Author Disclosures
This work was supported by the Berthold-Leibinger-Foundation, Ditzingen, Germany and the Robert-Bosch-Stiftung, Stuttgart, Germany. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Ong P., Athanasiadis A., Sechtem U. Intracoronary acetylcholine provocation testing for assessment of coronary vasomotor disorders. J Vis Exp. 2016;114:54295. doi: 10.3791/54295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel M.R., Peterson E.D., Dai D. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:886–895. doi: 10.1056/NEJMoa0907272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ong P., Athanasiadis A., Borgulya G., Mahrholdt H., Kaski J.C., Sechtem U. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries) J Am Coll Cardiol. 2012;59:655–662. doi: 10.1016/j.jacc.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Seitz A., Gardezy J., Pirozzolo G. Long-term follow-up in patients with stable angina and unobstructed coronary arteries undergoing intracoronary acetylcholine testing. J Am Coll Cardiol Intv. 2020;13:1865–1876. doi: 10.1016/j.jcin.2020.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Knuuti J., Wijns W., Saraste A. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]