Abstract
Background/Aims
To perform a 12-month comparison between the different extents and locations of Schlemm’s canal incisions during suture trabeculotomy ab interno for open-angle glaucoma (OAG).
Methods
This is a prospective, single-centre, three-arm randomised trial. A total of 99 eyes of 99 patients were randomly assigned to one of three groups: the 360° incision group (n=34), the upper-180° incision group (n=34) and the lower-180° incision group (n=31). Intraocular pressure (IOP), number of medications and complications were evaluated until 12 months after surgery. Surgical success (with or without medication) was defined as IOP ≤21 mmHg and ≥20% IOP reduction (criterion A) or IOP ≤15 mmHg and ≥20% IOP reduction (criterion B).
Results
The mean IOP (±SD) in all eyes was reduced from 18.6 (5.9) mmHg with 3.1 (1.1) medications to 13.7 (3.4) mmHg (20.8% reduction; p<0.001) with 1.4 (1.3) medications (p<0.001) at postoperative 12-month. Each group produced comparable mean reductions in both IOP and the number of medications throughout 12 months of follow-up. Kaplan-Meier cumulative survival analyses showed no significance among these three groups for criterion A and criterion B. Postoperative hyphema with niveau formation occurred significantly more in the 360° group than in the lower-180° group (p=0.031).
Conclusions
The different extents and locations of Schlemm’s canal incisions during suture trabeculotomy ab interno for OAG, including the 360° incision, the upper-180° incision and the lower-180° incision, do not affect both the IOP reduction and the medications throughout 12 months of follow-up.
Trial registration number
UMIN000021169.
Keywords: Clinical Trial, Glaucoma, Intraocular pressure, Treatment Surgery
Various morphological and functional alterations of the trabecular meshwork increase aqueous outflow resistance in open-angle glaucoma (OAG). 1 2 Trabecular-targeted minimally invasive glaucoma surgeries (MIGS), including trabecular ablation via the Trabectome, iStent, Kahook Dual Blade (KDB), microhook ab interno trabeculotomy, gonioscopy-assisted transluminal trabeculotomy (GATT) and suture trabeculotomy ab interno, have gained popularity for lowering intraocular pressure (IOP). 3–9 These surgeries aim at relieving the resistance of aqueous humour outflow by removing or incising the trabecular meshwork and inner layer of Schlemm’s canal. Although MIGS procedures have an advantage with regard to safety and speed, their variability and inconsistency in lowering the IOP are still problematic. 10
Approximately 85% of aqueous outflow reportedly occurs via the conventional pathway through the trabecular meshwork, 11 which is the structure that is believed to provide the highest resistance to aqueous outflow. 1 2 If the pressure-lowering effect of the trabeculotomy increases according to the extent of incision, longer incisions may help to reduce the IOP. However, various morphological changes in the distal aqueous outflow pathway have been described in glaucomatous eyes. 12 In eyes with a pathological impairment of collector channel or aqueous vein function, which may play a major role in IOP elevation, the extent of the Schlemm’s canal incision may not affect the IOP reduction. Nevertheless, this issue has not yet been fully investigated.
We previously reported a reduction in the IOP value to approximately the middle teens after 360° suture trabeculotomy ab interno for OAG. 8 9 Changes in the extents and locations of Schlemm’s canal incisions are technically possible, and in that surgery, we used a 360° Schlemm’s canal incision. In the present study, we prospectively performed a 12-month comparison of the different extents and locations of Schlemm’s canal incisions, including a 360° incision, an upper-180° incision and a lower-180° incision, during suture trabeculotomy ab interno for OAG.
SUBJECTS AND METHODS
This investigation was a prospective, open-label, single-centre, interventional, three-arm comparative clinical study conducted at Sato Eye and Internal Medicine Clinic (Arao City, Kumamoto, Japan) between September 2015 and December 2017. By using a random number table, our Japanese patients were randomly assigned to one of the following three groups: 360° Schlemm’s canal incision (360° group), upper-180° Schlemm’s canal incision (upper-180° group) or lower-180° Schlemm’s canal incision (lower-180° group). The study protocol complied with the tenets of the Declaration of Helsinki was approved by the Institutional Review Board and the Ethics Committee at Sato Eye and Internal Medicine Clinic, and was registered with the University Hospital Medical Information Network (UMIN) Clinical Trials Registry of Japan (registration number UMIN000021169). Before surgery, all patients provided informed written consent. The dat asets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Study subjects
Patients were considered for enrollment in the study if they had OAG that was refractory to medical therapy or had OAG that required medical therapy plus had a coexisting visually significant cataract. Patients had used two or more IOP-lowering medications were enrolled. Patients included those with primary open-angle glaucoma (POAG), normal-tension glaucoma (NTG) and exfoliation glaucoma (XFG). A cataract was considered visually significant if the patient complained of glare or halos and had best-corrected visual acuity (BCVA) of 20/20 or worse. A POAG diagnosis was made if the IOP value was >21 mmHg without medication, the angle was open (Shaffer grade 3 or 4) and optic neuropathy with matching visual field changes had occurred. The NTG diagnosis was determined according to the same criterion, but the IOP value was ≤21 mmHg. An XFG diagnosis was used if exfoliation material had adhered to the lens surface or the iris–pupil margin, the angle was open in the presence of dense pigmentation, Sampaolesi’s line was present and optic neuropathy with a matching visual field loss had occurred. Subjects were excluded from this study if they had any of the following: other types of glaucoma or a history of incisional glaucoma surgery. All procedures were performed by one surgeon (TS) who used the surgical procedure described herein.
Surgical technique
The suture trabeculotomy ab interno procedure was previously described in full 8 ; the present study used a modified technique for Schlemm’s canal incision. Briefly, a 1.7 mm temporal corneal incision was created, and Schlemm’s canal was incised at 15° on the nasal side by using a microhook needle (HS-2167; Handaya, Tokyo, Japan) instead of the Trabectome (NeoMedix, Tustin, CA, USA), which was used in the original paper. 8 When the upper- or lower-180° suture trabeculotomy ab interno procedure was performed, a 5-0 nylon suture (Mani Nylon, Mani, Tochigi, Japan) was inserted into nearly half of Schlemm’s canal and pulled out after an inspection was made, by using a surgical gonio lens (AU-700-476; Ocular Instruments, Bellevue, WA, USA), to ensure that the tip of the suture was located at an opposite side. If necessary, a standard phacoemulsification with intraocular lens implantation was performed after the suture trabeculotomy ab interno through the same or a newly created upper corneal incision. At the end of the surgery, we confirmed that no wound leakage occurred and that the IOP value was 18 mmHg or more in the supine position by using iCare (M.E. Technica, Tokyo, Japan). Postoperative routine medications consisted of a 2-week regimen of moxifloxacin hydrochloride, 0.1% betamethasone and 2% pilocarpine.
Examinations
All potential patients were screened for study eligibility via slit-lamp biomicroscopy, indirect ophthalmoscopy, manifest refraction, IOP measurement, corneal endothelial cell density (cells/mm2) and BCVA assessment (conventional Landolt ring chart). All IOP assessments were performed by the surgeons or other ophthalmologists using a Goldmann tonometer. A baseline IOP was determined by using the mean of the three most recent measurements, acquired on separate days within 1 month before surgery. Corneal endothelial cell density was examined by using a non-contact specular microscope (SP-3000P; Topcon, Tokyo, Japan) at before and 12 months after surgery. Manifest refraction was measured via an Auto Ref/Keratometer (ARK-530A; Nidek, Tokyo, Japan); the decimal visual acuity values were converted to the logarithm of the minimum angle of resolution for analyses.
All patients were examined on postoperative days 1–3, every 1–2 weeks for 1 month, monthly until month 6 and every 2–3 months until month 12. The IOP was measured at every visit. Patients were given antiglaucoma medications after surgery if the IOP was higher than the desired range (<15 mmHg), as in the previous report. 8
Outcome measures
Outcome measures included the IOP value at each visit, the number of glaucoma medications, cumulative surgical success rates (Kaplan-Meier life-table analysis), and the number and kind of complications. A surgical success (with or without medication) was defined as an IOP value between 6 mmHg and 21 mmHg with a postoperative IOP reduction of at least 20% (criterion A) or an IOP value between 6 mmHg and 15 mmHg with a postoperative IOP reduction of at least 20% (criterion B). A surgical failure was defined as not meeting a success criterion at two consecutive follow-up visits at least 1 month after surgery or the need for additional glaucoma surgery. The IOP levels at later than 1 month after surgery were used as determinants of surgical success so that short-term IOP fluctuations would not influence the long-term surgical success rates.
Safety
Measures of safety included intraoperative and postoperative complications and BCVA at 1 year after surgery. Postoperative complications included intraoperative blood reflux, hyphema with niveau formation, shallow chamber, wound leaks, IOP spikes (ie, an IOP value of ≥30 mmHg within 1 month of surgery), hypotony (an IOP value of ≤5 mmHg), infection, decreased corneal endothelial cell density and vision loss.
Statistical analyses
The JMP statistical package (version 14; SAS Institute, Cary, NC, USA) was used to perform all data analyses. Continuous data were expressed as mean±SD and were compared for the three groups by using one-way analysis of variance; preoperative values and postoperative 12-month values were compared by using a paired t-test and a Wilcoxon signed-rank test with Bonferroni correction as appropriate. Categorical data were expressed as n (%) and were compared for the three groups by using Fisher’s exact test. The Kaplan-Meier survival curve analysis was used to evaluate the cumulative probability of success, and a log-rank test was used for comparisons among groups. Statistical significance was set at p<0.05. Assuming an SD of the IOP measurement of 3 mmHg as reported in previous studies 8 9 and setting a significance level of 0.05 α error, the minimum sample size was set at 28 patients with a power of 80% to detect a difference of 15% between the groups.
RESULTS
Enrollment and disposition
One hundred eyes were randomised into three groups, and planned surgeries were performed between September 2015 and December 2017. One patient who had a planned upper-180° suture trabeculotomy ab interno combined with phacoemulsification was excluded because the suture was not inserted into the upper side of Schlemm’s canal in view of the resistance at the quarter of Schlemm’s canal. For that patient, the suture was inserted into the opposite half of lower Schlemm’s canal. Therefore, 99 eyes of 99 patients (41 males, 75.5±8.3 years old) were ultimately included in the 1-year analyses (table 1). The suture trabeculotomy ab interno procedure alone was performed in 13 eyes (13.1%) and suture trabeculotomy ab interno combined with phacoemulsification was performed in 86 eyes (86.9%). All eyes except the excluded eye mentioned above had a complete 360° Schlemm’s canal incision, complete upper-180° incision or complete lower-180° incision.
Table 1.
Preoperative demographic and ocular characteristics of patients
| Characteristics | 360° Group | Upper-180° group | Lower-180° group | P value |
|---|---|---|---|---|
| N, patients/eyes (right/left) |
34/34 (16/18) |
34/34 (17/17) |
31/31 (13/18) |
0.806 |
| Age (years) | 74.0±9.1 (56–87) | 77.0±7.0 (61–93) | 75.4±8.7 (61–94) | 0.344 |
| Male/female | 20/14 | 18/16 | 13/18 | 0.388 |
| Preoperative IOP (mmHg) | 18.7±6.2 (12–37) | 18.7±5.2 (11–31) | 18.3±6.1 (12–37) | 0.947 |
| Number of medications | 3.2±1.0 (2–6) | 3.0±1.0 (2–5) | 3.2±1.2 (2–6) | 0.639 |
| Phakic/Pseudophakic | 29/5 | 28/6 | 29/2 | 0.388 |
| LogMAR BCVA | 0.41±0.50 | 0.34±0.31 | 0.29±0.21 | 0.390 |
| Visual field MD (dB) | −12.8±9.6 | −13.9±8.6 | −13.1±7.5 | 0.854 |
| Corneal endothelial cell density (cells/mm2) | 2513.5±340.6 | 2394.7±451.1 | 2425.1±343.9 | 0.438 |
| Type of glaucoma, n (%) | 0.325 | |||
| POAG | 16 (47) | 16 (47) | 19 (61) | |
| NTG | 6 (18) | 8 (23) | 8 (26) | |
| XFG | 12 (35) | 10 (29) | 4 (13) | |
| Previous surgical or laser treatment, n (%) | 0.591 | |||
| Cataract extraction | 5 (15) | 6 (18) | 32 (6) | |
| Selective laser trabeculoplasty | 1 (3) | 0 (0) | 1 (3) | |
| None | 28 (82) | 28 (82) | 28(90) |
BCVA, best-corrected visual acuity; IOP, intraocular pressure; LogMAR, logarithm of minimum angle of resolution; MD, mean deviation; NTG, normal-tension glaucoma; POAG, primary open-angle glaucoma; XFG, exfoliation glaucoma.
Outcomes
In the all three groups at 12 months after surgery, the mean IOP value for all 99 eyes was reduced from 18.6±5.9 mmHg with 3.1±1.1 medications to 13.7±3.4 mmHg (20.8% reduction; p<0.001) with 1.4±1.3 medications (p<0.001). As table 2 shows, the IOP values and the number of medications were significantly reduced at 12 months after surgery in each group (p<0.001 for all variables and groups), and no significant differences were found between the 3 groups throughout 12 months of follow-up.
Table 2.
Intraocular pressure and number of antiglaucoma medications used in patients
| Measure | 360° Group | Upper-180° group | Lower-180° group | P value |
|---|---|---|---|---|
| n, Patients/eyes | 34/34 | 34/34 | 31/31 | – |
| IOP (mmHg) | ||||
| Before surgery | 18.7±6.2 | 18.7±5.2 | 18.3±6.1 | 0.947 |
| 1 Day | 16.3±11.8 | 15.6±8.0 | 17.3±8.3 | 0.792 |
| 1 Week | 19.1±8.4 | 20.0±9.6 | 18.6±9.5 | 0.827 |
| 1 Month | 16.1±6.7 | 15.8±5.1 | 15.0±4.3 | 0.695 |
| 3 Months | 14.0±3.8 | 14.7±4.9 | 13.5±3.4 | 0.495 |
| 6 Months | 13.2±3.1 | 14.1±3.8 | 13.6±3.8 | 0.578 |
| 12 Months | 13.8±3.2 | 13.9±3.8 | 13.3±3.1 | 0.806 |
| 12-Month IOP reduction | 21.8±21.0% | 20.7±27.5% | 19.7±21.4% | 0.947 |
| Number of antiglaucoma medications | ||||
| Before surgery | 3.2±1.0 | 3.0±1.0 | 3.2±1.2 | 0.639 |
| 1 Month | 0.2±0.5 | 0.3±0.6 | 0.2±0.4 | 0.678 |
| 3 Months | 0.5±0.7 | 1.0±0.9 | 0.8±0.9 | 0.107 |
| 6 Months | 1.1±1.4 | 1.6±1.2 | 1.1±1.3 | 0.211 |
| 12 Months | 1.3±1.3 | 1.6±1.3 | 1.3±1.4 | 0.441 |
IOP, intraocular pressure.
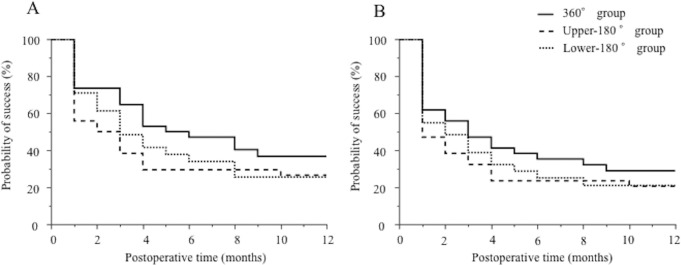
Figure 1 illustrates no significant differences in the Kaplan-Meier cumulative survival analysis curves for the three groups with regard to both criterion A and criterion B. At 12 months after surgery, the success rates for criterion A were 36.7% in the 360° group, 26.5% in the upper-180° group and 25.5% in the lower-180° group (p=0.320). When using criterion B, the success rates were 28.9% in the 360° group, 20.9% in the upper-180° group and 20.6% in the lower-180° group (p=0.519).
Figure 1.
Kaplan-Meier survival curves for patients treated with suture trabeculotomy ab interno with different extents and locations of Schlemm’s canal incision. Patients were randomly assigned to one of three groups: 360° Schlemm’s canal incision (360° group), upper-180° Schlemm’s canal incision (upper-180° group), or lower-180° Schlemm’s canal incision (lower-180° group). Surgical success (with or without medication use) was defined as an IOP value between 6 mmHg and 21 mmHg with a postoperative IOP reduction of at least 20% (criterion A) or an IOP value between 6 mmHg and 15 mmHg with a postoperative IOP reduction of at least 20% (criterion B). A surgical failure was defined as not meeting a success criterion at two consecutive follow-up visits at least 1 month after surgery or the need for additional glaucoma surgery. No significant difference was seen among these three groups for criterion A and criterion B.
Safety
Table 3 summarises the intra- and postoperative complications. The most frequent postoperative complications included hyphema with niveau formation and IOP spikes in all groups. The frequencies of postoperative hyphema with niveau formation in these 3 groups were significantly different (p=0.038), with the significant difference occurring for the 360° group (26%) and the lower-180° group (6%, p=0.031). The hyphema spontaneously resolved by 2 weeks in all but 1 eye in the 360° group; this eye required anterior chamber washout on day 2 because the massive hyphema caused IOP spikes.
Table 3.
Intraoperative and postoperative complications
| Characteristics | 360° Group | Upper-180° group | Lower-180° group | P value |
|---|---|---|---|---|
| n, patients/eyes | 34/34 | 34/34 | 31/31 | – |
| Intraoperative blood reflux, n (%) | 34 (100) | 34 (100) | 31 (100) | NA |
| Hyphema, n (%) | 9 (26) | 3 (9) | 2 (6) | 0.038 |
| Day 1 | 8 (24) | 2 (6) | 1 (3) | |
| Week 2 | 0 (0) | 0 (0) | 0 (0) | |
| Shallow chamber | 0 (0) | 0 (0) | 0 (0) | NA |
| Wound leaks | 0 (0) | 0 (0) | 0 (0) | NA |
| IOP spike (≥30 mmHg), n (%) | 16 (47) | 9 (26) | 9 (29) | 0.153 |
| Hypotony (IOP <5 mmHg) | 3 (9) | 2 (6) | 0 (0) | 0.258 |
| Infection | 0 (0) | 0 (0) | 0 (0) | NA |
| Corneal endothelial cell density reduction | 2.9±4.8% | 1.9±4.4% | 1.9±5.7% | 0.735 |
| Anterior chamber washout, n (%) | 1 (3) | 0 (0) | 0 (0) | 0.381 |
| Subsequent glaucoma surgery, n (%) | 3 (9) | 1 (3) | 2 (6) | 0.593 |
IOP, intraocular pressure; NA, not applicable.
Three eyes (8.8%) in the 360° group, one eye (2.9%) in the upper-180° group and two eyes (6.4%) in the lower-180° group required subsequent glaucoma surgeries as follows: trabeculotomy in four eyes including one eye in the 360° group, one eye in the upper-180° group and two eyes in the lower-180° group; Ahmed glaucoma valve implantation in two eyes in the 360° group.
The postoperative 12-month BCVA in each group was significantly increased (p<0.001) and was not significantly different between these three groups (p=0.423). The BCVA decreased by two or more lines from baseline in five eyes (two eyes each in the 360° group and in the upper-180° group and one eye in the lower-180° group). The causes of these decreases were the progression of glaucoma in four eyes and the additional trabeculotomy that resulted in bullous keratopathy in one eye.
DISCUSSION
In this prospective study, we investigated the 12-month surgical outcomes among a 360° incision group, an upper-180° incision group and a lower-180° incision group during suture trabeculotomy ab interno. Each group had comparable mean reductions in both IOP and the number of medications during the 12 months of postoperative follow-up. However, no significant differences occurred among these three groups, which achieved target postoperative IOP values of ≤21 mmHg and ≤15 mmHg at 12 months. The intraoperative and postoperative complications did not differ significantly among these three groups, except for the frequency of postoperative hyphema, which differed significantly between the 360° group and the lower-180° group.
It seems reasonable to hypothesise that the IOP reduction would be proportional to the extent of the diseased trabecular meshwork that was bypassed to allow aqueous humour to flow into the distal outflow system. However, our study demonstrated that the extent of the incision in Schlemm’s canal during suture trabeculotomy ab interno did not correlate with IOP reduction. Similar results were reported retrospectively for different types of MIGS: the postoperative trabeculotomy opening size (mean±SD, 53°±35°) did not correlate with IOP reduction in Trabectome surgery at a follow-up point of 125±66 days 13 ; the extent of the incision in Schlemm’s canal (275°±52.3°) during suture trabeculotomy ab externo did not correlate with IOP reduction at 1 year postoperatively 14 ; and both the KDB, which removes 90–120° of the trabecular meshwork, and the 360° trabeculotomy (via either Trab360 (Sight Sciences, Menlo Park, CA, USA) or GATT) procedures similarly lowered both the IOP and the need for medications during the first 6 postoperative months. 15 In the latter reports, interestingly, significantly more KDB eyes than Trab360/GATT eyes achieved the target IOP values of ≤18 mmHg and ≤15 mmHg. Another study reported that the 360° trabeculotomy achieved lower IOP values than did the 120° trabeculotomy. 16 However, in that study, sodium hyaluronate was injected into Schlemm’s canal before the suture insertion, which may have resulted in combined effects of viscocanalostomy and suture trabeculotomy, whereas no such injections were administered during the 120° trabeculotomy procedure. In addition, 120° incisions were created with metal probes, not suture. Thus, the differences between these incision approaches may have made it difficult to evaluate their surgical outcomes according to the extent of the incision.
In enucleated human eyes, the 120° trabeculotomy reportedly resulted in an 85% reduction in outflow resistance vs the 360° trabeculotomy. 17 This result suggests that a dose–response threshold effect exists such that a trabecular meshwork incision greater than 120° provides no additional aqueous humour outflow or IOP reduction. Given both these experimental data and several clinical results including our study, incisions greater than approximately 120° may not help reduce the IOP in each type of MIGS-targeted trabecular meshwork. Another possible explanation is that the distal outflow pathway was already dysfunctional before surgery. Several reports have shown various morphological alterations of the distal outflow pathway in glaucomatous eyes. 12 Moreover, recent publications reported an intraoperative observation of fluid waves in episcleral veins, which was correlated with better postoperative IOP reduction and/or the number of medications. 18–20 This finding indicates that a functional intrascleral drainage system distal to the trabeculotomy site is a prerequisite for both a minimum required size of the incision of the trabecular meshwork and good IOP reduction.
A previous study reported that the failure rate of trabeculotomy ab externo with metal probes increases over time. 21 A possible explanation is that the original size of the trabeculotomy opening decreases to a variable degree because of reclosure of the trabecular meshwork or because of the formation of anterior synechiae. 22 Although the extent of Schlemm’s canal incision in our study did not seem to correlate with IOP reduction during the 12-month follow-up, a longer follow-up period may reveal that longer incisions produce better outcomes because extending the incision may make it more likely that part of the incision remains open.
A significant difference in the occurrence of postoperative hyphema with niveau formation existed between the 360° group and the lower-180° group, but the three groups did not differ significantly with regard to the occurrence of IOP spikes. Longer incisions in Schlemm’s canal may cause greater blood reflux from the collector channels, which would result in a higher frequency of postoperative hyphema, but they have no significant effect on the likelihood of IOP spikes despite greater blood congestion.
The present study has certain limitations. The number of cases was relatively small. Our study population included cases of combined trabeculotomy and cataract surgery. Although the cataract surgery may have biased the IOP reduction results, the number of combined cases predominated in our study (86.9%), and no significant difference was found in these three groups with regard to the number of combined cases. Recent MIGS procedures have been routinely performed in medically well-controlled eyes to reduce the medication burden and as an early intervention in eyes requiring IOP reduction without the use of any medication or laser options at the time of cataract surgery. 23 24 Thus, such cases were included in the present study and had a relatively low baseline IOP value (18.3–18.7 mmHg) and IOP reduction (19.7–21.8%) in each group. To verify the results in eyes with a higher baseline IOP, we created a subgroup of cases with a baseline IOP of ≥21 mmHg (total 23 eyes; nine eyes in the 360° group, eight eyes in the upper-180° group and six eyes in the lower-180° group). The mean IOP in these eyes was reduced from 27.8±4.7 mmHg with 3.9±0.9 medications to 14.2±3.8 mmHg (46.8% reduction; p<0.001) with 1.8±1.7 medications at 12 months postoperatively. No significant differences in outcomes occurred among these three subgroups, and these results were comparable to those of the original study population.
In conclusion, the different extents and locations of Schlemm’s canal incisions during suture trabeculotomy ab interno for OAG, including a 360° incision, an upper-180° incision and a lower-180° incision, did not affect both the IOP reduction and the need for medications during a 12-month follow-up. A 360° circumferential incision of Schlemm’s canal may thus not be necessary for the initial surgery to treat OAG.
Footnotes
Contributors: TS and TK had the idea for the article, performed the literature search and wrote the article. TK is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
REFERENCES
- 1. Tamm ER. The trabecular meshwork outflow pathways: structural and functional aspects. Exp Eye Res 2009;88:648–55. 10.1016/j.exer.2009.02.007 [DOI] [PubMed] [Google Scholar]
- 2. Tektas O-Y, Lütjen-Drecoll E. Structural changes of the trabecular meshwork in different kinds of glaucoma. Exp Eye Res 2009;88:769–75. 10.1016/j.exer.2008.11.025 [DOI] [PubMed] [Google Scholar]
- 3. Shoji N, Kasahara M, Iijima A, et al. Short-term evaluation of trabectome surgery performed on Japanese patients with open-angle glaucoma. Jpn J Ophthalmol 2016;60:156–65. 10.1007/s10384-016-0433-5 [DOI] [PubMed] [Google Scholar]
- 4. Malvankar-Mehta MS, Iordanous Y, Chen YN, et al. iStent with phacoemulsification versus phacoemulsification alone for patients with glaucoma and cataract: a meta-analysis. PLoS One 2015;10:e0131770. 10.1371/journal.pone.0131770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Leonard KS, Jeffrey RS, David AA, et al. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am J Ophthalmol 2013;155:524–9. 10.1016/j.ajo.2012.09.023 [DOI] [PubMed] [Google Scholar]
- 6. Tanito M, Sano I, Ikeda Y, et al. Short-term results of microhook ab interno trabeculotomy, a novel minimally invasive glaucoma surgery in Japanese eyes: initial case series. Acta Ophthalmol 2017;95:e354–60. 10.1111/aos.13288 [DOI] [PubMed] [Google Scholar]
- 7. Grover DS, Godfrey DG, Smith O, et al. Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology 2014;121:855–61. 10.1016/j.ophtha.2013.11.001 [DOI] [PubMed] [Google Scholar]
- 8. Sato T, Hirata A, Mizoguchi T. Prospective, noncomparative, nonrandomized case study of short-term outcomes of 360° suture trabeculotomy ab interno in patients with open-angle glaucoma. Clin Ophthalmol 2015;9:63–8. 10.2147/OPTH.S75739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sato T, Kawaji T, Hirata A, et al. 360-degree suture trabeculotomy ab interno with phacoemulsification in open-angle glaucoma and coexisting cataract: a pilot study. BMJ Open Ophthalmol 2018;3:e000159. 10.1136/bmjophth-2018-000159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lavia C, Dallorto L, Maule M, et al. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS One 2017;12:e0183142. 10.1371/journal.pone.0183142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bill A, Phillips CI. Uveoscleral drainage of aqueous humour in human eyes. Exp Eye Res 1971;12:275–8. 10.1016/0014-4835(71)90149-7 [DOI] [PubMed] [Google Scholar]
- 12. Hann CR, Bentley MD, Vercnocke A, et al. Imaging the aqueous humor outflow pathway in human eyes by three-dimensional micro-computed tomography (3D micro-CT). Exp Eye Res 2011;92:104–11. 10.1016/j.exer.2010.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wecker T, Anton A, Neuburger M, et al. Trabeculotomy opening size and IOP reduction after Trabectome surgery. Graefes Arch Clin Exp Ophthalmol 2017;255:1643–50. 10.1007/s00417-017-3683-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Manabe SI, Sawaguchi S, Hayashi K. The effect of the extent of the incision in the Schlemm canal on the surgical outcomes of suture trabeculotomy for open-angle glaucoma. Jpn J Ophthalmol 2017;61:99–104. 10.1007/s10384-016-0487-4 [DOI] [PubMed] [Google Scholar]
- 15. Hirabayashi MT, Lee D, King JT, et al. Comparison of surgical outcomes of 360° circumferential trabeculotomy versus sectoral excisional goniotomy with the Kahook Dual Blade at 6 months. Clin Ophthalmol 2019;13:2017–24. 10.2147/OPTH.S208468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chin S, Nitta T, Shinmei Y, et al. Reduction of intraocular pressure using a modified 360-degree suture trabeculotomy technique in primary and secondary open-angle glaucoma: a pilot study. J Glaucoma 2012;21:401–7. 10.1097/IJG.0b013e318218240c [DOI] [PubMed] [Google Scholar]
- 17. Rosenquist R, Epstein D, Melamed S, et al. Outflow resistance of enucleated human eyes at two different perfusion pressures and different extents of trabeculotomy. Curr Eye Res 1989;8:1233–40. 10.3109/02713688909013902 [DOI] [PubMed] [Google Scholar]
- 18. Fellman RL, Feuer WJ, Grover DS. Episcleral venous fluid waves correlate with trabectome outcomes. Ophthalmology 2015;122:2385–91. 10.1016/j.ophtha.2015.08.038 [DOI] [PubMed] [Google Scholar]
- 19. Fellman RL, Grover DS. Episcleral venous fluid wave in the living human eye adjacent to microinvasive glaucoma surgery (MIGS) supports laboratory research: outflow is limited circumferentially, conserved distally, and favored inferonasally. J Glaucoma 2019;28:139–45. 10.1097/IJG.0000000000001126 [DOI] [PubMed] [Google Scholar]
- 20. Aktas Z, Ozmen MC, Atalay HT, et al. Evaluation of episcleral venous fluid wave during gonioscopy assisted transluminal trabeculotomy in patients with advanced glaucoma. Eye 2019;33:668–73. 10.1038/s41433-018-0254-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tanihara H, Negi A, Akimoto M, et al. Surgical effects of trabeculotomy ab externo on adult eyes with primary open angle glaucoma and pseudoexfoliation syndrome. Arch Ophthalmol 1993;111:1653–61. 10.1001/archopht.1993.01090120075025 [DOI] [PubMed] [Google Scholar]
- 22. Wang Q, Harasymowycz P. Goniopuncture in the treatment of short-term post-Trabectome intraocular pressure elevation: a retrospective case series study. J Glaucoma 2013;22:e17–20. 10.1097/IJG.0b013e3182595042 [DOI] [PubMed] [Google Scholar]
- 23. Bovee CE, Pasquale LR. Evolving surgical interventions in the treatment of glaucoma. Semin Ophthalmol 2017;32:91–5. 10.1080/08820538.2016.1228393 [DOI] [PubMed] [Google Scholar]
- 24. Agrawal P, Bradshaw SE. Systematic literature review of clinical and economic outcomes of micro-invasive glaucoma surgery (MIGS) in primary open-angle glaucoma. Ophthalmol Ther 2018;7:49–73. 10.1007/s40123-018-0131-0 [DOI] [PMC free article] [PubMed] [Google Scholar]