Abstract
Coronary artery fistula are anomalous connections with coronary vessels or cardiac chambers, potentially resulting in coronary dilatation and pseudoaneurysm formation. We present the case of a 68-year-old woman referred to our institution for a voluminous coronary pseudoaneurysm secondary to coronary artery fistula presenting as a nearly completely obstructive left atrial mass. (Level of Difficulty: Intermediate.)
Key Words: computed tomography, coronary angiography, coronary vessel anomaly, echocardiography
Abbreviations and Acronyms: CAA, coronary artery aneurysm; CAF, coronary artery fistula; RCA, right coronary artery; TTE, transthoracic echocardiogram
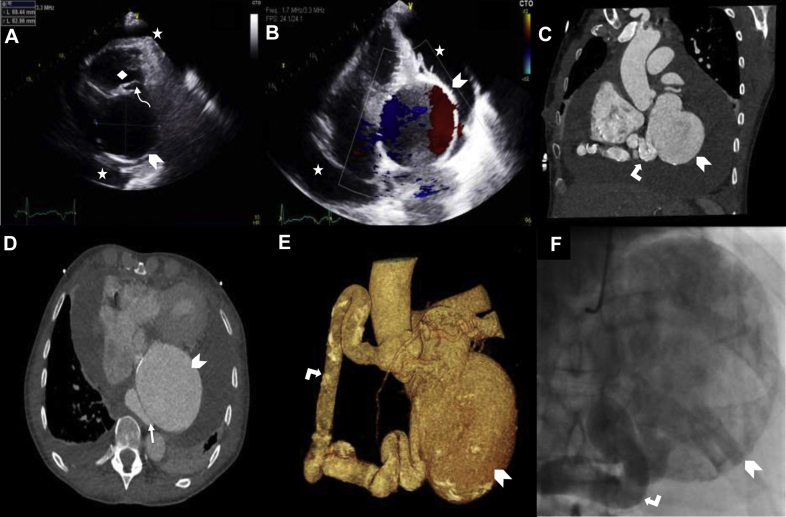
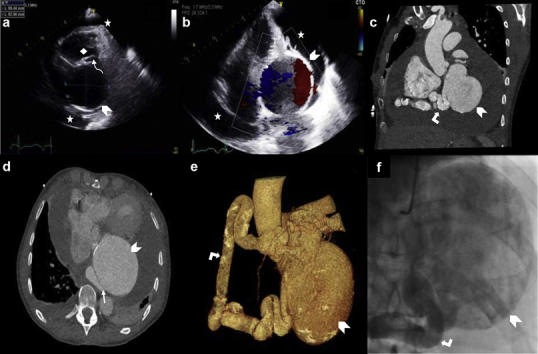
Central Illustration
A 68-year-old hypertensive, nonsmoking woman presented for 4 months of progressive dyspnea and nonproductive cough. She had no history of connective tissue disorder, autoimmune disease, sexually transmitted infection, or vasculitis. Physical examination revealed sinus tachycardia, jugular venous distension without the Kussmaul sign, and a pericardial friction rub. Chest radiography showed marked cardiomegaly.
Transthoracic echocardiogram (TTE) (Figure 1) demonstrated globally normal left ventricular function with a left ventricular ejection fraction of 60%; a 69 × 83–mm mass compressing the left atrium, with a secondary 5–mm Hg gradient across the anatomically normal mitral valve; and a circumferential 20-mm pericardial effusion, without signs of cardiac chamber compression or tamponade. Chest computed tomography angiography (Figure 1) revealed a pseudoaneurysm originating from a diffusely dilated (119 × 17 mm) right coronary artery (RCA) communicating via fistula with the coronary sinus. Coronary angiography (Videos 1 and 2) demonstrated extrinsic third marginal branch occlusion by the pseudoaneurysm. The mild cardiac compression and transmitral gradient secondary to the pseudoaneurysm’s mass effect noted on imaging support the patient’s clinical presentation.
Figure 1.
Multimodality Imaging of Giant Coronary Pseudoaneurysm
(A, B) Transthoracic echocardiogram: (A) the 69 × 83–mm pseudoaneurysm (chevron) compressing the left atrium (thin curved arrow) behind the right ventricular outflow tract (diamond) and pericardial effusion (stars) and (B) the yin-yang sign demonstrated by blue and red flow on color Doppler. (C to E) Computed tomography angiography: (C) coronal view of the dilated feeding right coronary artery (angled arrow) and pseudoaneurysm (chevron), (D) axial view of the fistula with the coronary sinus (straight arrow) and pseudoaneurysm, and (E) reconstructed image of the dilated feeding right coronary artery and pseudoaneurysm. (F) Coronary angiogram views of the pseudoaneurysm (chevron) and feeding right coronary artery (angled arrow).
High-sensitivity troponin T was slightly elevated but stable at 18 ng/l, N-terminal pro–B-type natriuretic peptide level was 767 ng/l, high-sensitivity C-reactive protein level was 69.8 ng/l, and erythrocyte sedimentation rate was 21 mm/h. Liver function test results were normal. Hepatitis B and C, HIV, and syphilis serology results were negative. Antinuclear antibodies, antineutrophilic cytoplasmic antibodies, and C3 and C4 levels were normal.
Aneurysmal flattening, coronary sinus fistula closure, ventricular remodeling, and serial saphenous vein graft onto the posterior interventricular artery and third marginal artery were performed via median sternotomy under cardiopulmonary bypass. The fistula to the coronary sinus was sutured. Pathology showed no vasculitis, infection, or neoplasia.
At the 3-month follow-up, the patient was doing very well, without complications and cardiac symptoms.
Coronary artery fistula (CAF) are rare anomalous connections (incidence: from 0.05% to 0.90%) that bypass the myocardial capillary bed and communicate with a cardiac chamber or major blood vessel (1). Coronary artery aneurysm (incidence: from 0.3% to 5.0%) is an abnormal dilatation of a segment of the coronary arterial tree (1). CAA and CAF rarely occur simultaneously, with CAA found in roughly only 5.9% of patients with CAF (2). A pseudoaneurysm, resulting from disruption of a portion of the arterial wall, may develop as a result of CAF (2).
CAA and pseudoaneurysm diagnosis may be made noninvasively by TTE, computed tomography, and magnetic resonance imaging. On TTE, the yin-yang sign, highly suggestive of a pseudoaneurysm, results from turbulent bidirectional blood flow within the mass (3). Coronary angiography remains the gold standard diagnostic test (3), although computed tomography angiography may better delineate coronary anatomy (2).
CAF closure is often performed precociously to prevent development of ischemic or congestive symptoms or complications such as rupture, and it is recommended in all cases of symptomatic CAF (1). Although percutaneous closure outcomes are comparable to surgical results, with high success and mortality of <1%, factors such as distal fistula, often causing severely dilated and highly tortuous feeding coronaries, may preclude patients from percutaneous closure. Guidelines make no recommendations for choosing between surgical or percutaneous closure techniques but, rather, recommend a multidisciplinary expert approach and defer to expert opinion on a case-by-case basis.
This case provides insight into the spectrum of coronary artery diseases and highlights the importance of multimodality imaging and hemodynamic evaluation to clarify and manage this atypical anatomy.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Coronary angiography of the left coronary artery network demonstrating extrinsic occlusion of M3 resulting from mass effect exerted by the large, obstructive pseudoaneurysm.
Coronary angiography of the RCA network demonstrating the dilated RCA feeding the pseudoaneurysm, in which the turbulent, bidirectional flow of blood can be appreciated.
References
- 1.Buccheri D., Chirco P.R., Geraci S., Caramanno G., Cortese B. Coronary artery fistulae: anatomy, diagnosis, and management strategies. Heart Lung Circ. 2018;27:940–951. doi: 10.1016/j.hlc.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 2.Pahlavan P.S., Niroomand F. Coronary artery aneurysm: a review. Clin Cardiol. 2006;29:439–443. doi: 10.1002/clc.4960291005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lupatelli T. The yin-yang sign. Radiology. 2006;238:1070–1071. doi: 10.1148/radiol.2383031884. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Coronary angiography of the left coronary artery network demonstrating extrinsic occlusion of M3 resulting from mass effect exerted by the large, obstructive pseudoaneurysm.
Coronary angiography of the RCA network demonstrating the dilated RCA feeding the pseudoaneurysm, in which the turbulent, bidirectional flow of blood can be appreciated.