Abstract
Takeuchi repair is a unique surgical approach in anomalous left coronary artery from the pulmonary artery. We present an adult patient with anomalous left coronary artery from the pulmonary artery with multiple late structural complications after Takeuchi repair who was evaluated using multimodality imaging, including newly developed cardiac fusion imaging with computed tomography and echocardiography. (Level of Difficulty: Advanced.)
Key Words: adult congenital heart disease, anomalous left coronary artery from pulmonary artery, Takeuchi repair
Abbreviations and Acronyms: ACHD, adult congenital heart disease; ALCAPA, anomalous left coronary artery from the pulmonary artery; LCA, left coronary artery; LV, left ventricular; MDCT, multidetector computed tomography; MPA, main pulmonary artery; STDME, simultaneous 2-screen display of multidetector computed tomography and real-time echogram
Central Illustration
History of Presentation
A 48-year-old man was found to have anomalous left coronary artery from the pulmonary artery (ALCAPA) at 12 years of age and underwent Takeuchi repair. Although post-operative echocardiography showed a mild baffle leak and mild supravalvular pulmonary stenosis with a peak gradient of 37 mm Hg, these findings were unchanged, and he was followed up regularly without any symptoms until adolescence. As he had not received regular cardiology follow-up during adulthood, he was referred to our adult congenital heart disease (ACHD) clinic for evaluation of his current condition. A physical examination disclosed a pansystolic murmur at the left upper sternal border.
Learning Objectives
-
•
To review Takeuchi repair, which establishes a 2-coronary system in patients with ALCAPA.
-
•
To illustrate late structural complications in patients with ALCAPA after Takeuchi repair.
-
•
To enhance accurate evaluation and management of patients with ALCAPA after Takeuchi repair.
Differential Diagnosis
The differential diagnosis for the pansystolic murmur in our patient was mitral regurgitation because the patient had a history of ALCAPA, for which left ventricular (LV) dysfunction and subsequent mitral regurgitation are well-known complications.
Investigations
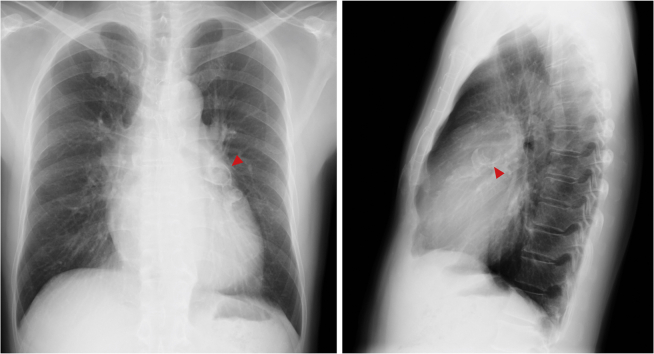
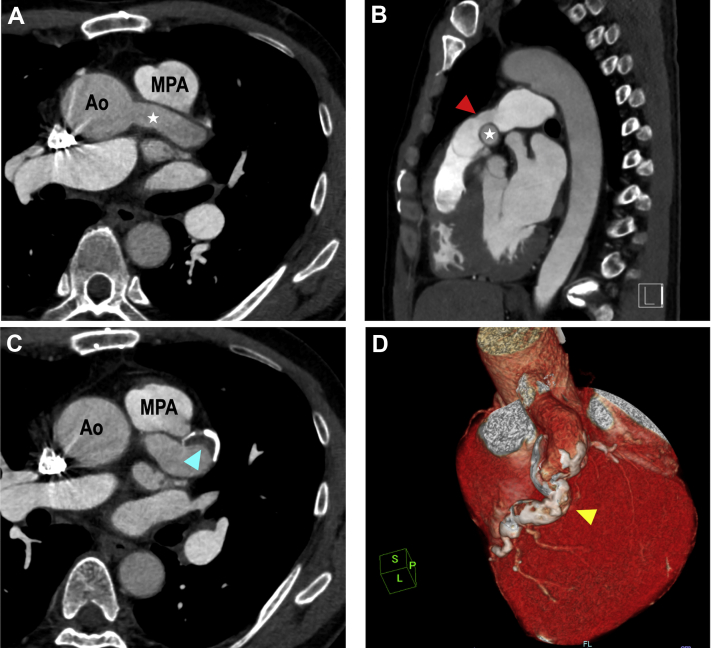
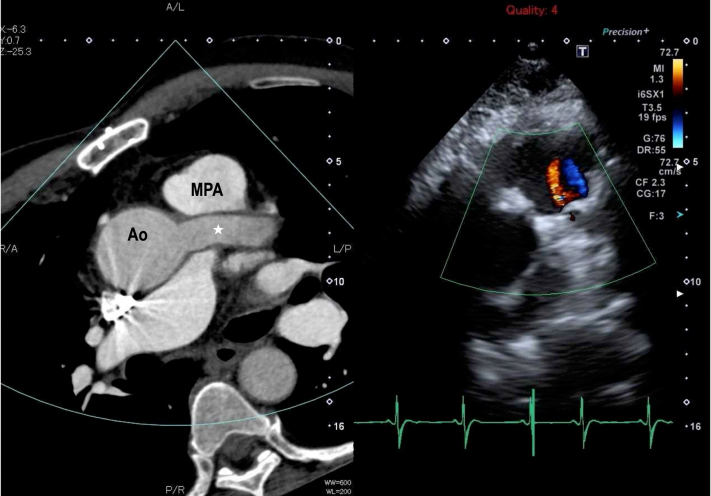
Electrocardiography demonstrated normal sinus rhythm with T-wave inversion in leads I, aVL, V4, V5, and V6. Chest radiography showed mild cardiomegaly and a calcified duct abutting the left upper cardiac contour (Figure 1). Transthoracic echocardiography revealed a mildly increased LV end-diastolic diameter of 56 mm (Video 1), preserved LV ejection fraction of 64%, mild mitral regurgitation, and a severely dilated intrapulmonary baffle followed by main pulmonary artery (MPA) obstruction with a peak gradient of 62 mm Hg (Figure 2, Video 2). Contrast-enhanced multidetector computed tomography (MDCT) revealed a severely dilated intrapulmonary baffle in the MPA and an interspersed aneurysm of the left coronary artery (LCA) with a maximal diameter of 20 mm (Figure 3, Video 3). The fusiform aneurysm of the LCA had severe circumferential calcification from the proximal coronary segment to the distal coronary segment and had a small thrombus in the proximal segment (Figure 3). The newly developed simultaneous 2-screen display of MDCT and real-time echogram (STDME) technology (Canon Medical Systems Corporation, Otawara, Japan), which can provide synchronized display of real-time ultrasound images and multiplanar reconstruction images of contrast-enhanced MDCT corresponding to the image plane of real-time ultrasound, revealed a small fistulous connection in the intrapulmonary baffle with a shunt flow from the coronary artery to the MPA (Figure 4, Video 4). STDME also demonstrated a severely calcified coronary artery aneurysm (Video 5).
Figure 1.
Chest Radiography
Chest radiography revealed a calcified duct abutting the left upper cardiac contour (red arrowheads).
Figure 2.
Conventional Transthoracic Echocardiography
Conventional transthoracic echocardiography showed a severely dilated intrapulmonary baffle (A) (white asterisk) followed by severe main pulmonary artery (MPA) obstruction (B) with a peak gradient of 62 mm Hg (C). Ao = aorta.
Figure 3.
Cardiac Computed Tomography
Cardiac computed tomography showed a severely dilated intrapulmonary baffle (A, white asterisk) in the MPA that caused MPA obstruction with the narrowest portion measuring 16 mm (B, red arrowhead). An interspersed aneurysm of the left coronary artery (LCA) with a maximal diameter of 20 mm was also identified (C). The fusiform aneurysm of the LCA had severe circumferential calcification from the proximal coronary segment to the distal coronary segment (D, yellow arrowhead) and had a small thrombus (C, blue arrowhead) in the proximal segment. Abbreviations as in Figure 2.
Figure 4.
Still Image From Simultaneous 2-Screen Display of MDCT and Real-Time Echocardiogram
Next to the real-time cross-sectional echocardiographic image (right), this system displays the corresponding contrast-enhanced cross section from multidetector computed tomography (MDCT) (left). Contrast-enhanced MDCT clearly depicted an intrapulmonary baffle (white asterisk), and a color Doppler echocardiographic image showed a small fistulous connection in the intrapulmonary baffle with a shunt flow from the coronary artery to the MPA. Abbreviations as in Figure 2.
Cardiac catherization was performed, and it showed mild supravalvular pulmonary stenosis with a peak gradient of 33 mm Hg, mildly elevated systolic right ventricular pressure of 49 mm Hg, and a pulmonary-to-systemic blood flow ratio (Qp/Qs) of 1.23. Coronary angiography revealed a large LCA aneurysm and a shunt flow from the LCA to the MPA through the intrapulmonary baffle leak. However, myocardial ischemia and damage were not demonstrated by stress thalium-201 single-photon emission computed tomography and late gadolinium-enhanced cardiac magnetic resonance imaging.
Management
As the LCA aneurysm was unlikely to rupture because of severe circumferential calcification, and as myocardial ischemia and damage were not detected by several imaging techniques, an immediate surgical intervention was not considered to be required. Therefore, the patient was prescribed aspirin and warfarin to prevent additional thrombus formation in the coronary artery aneurysm.
Discussion
ALCAPA is a rare congenital cardiac anomaly associated with a high infant mortality rate and adult sudden cardiac death if left untreated (1). Therefore, once ALCAPA is diagnosed, early surgical repair is recommended. Takeuchi repair, which creates an aortopulmonary window and an intrapulmonary tunnel that baffles the LCA to the aorta, has been widely performed, as well as direct LCA reimplantation as an alternative surgical approach to establish a 2-coronary system. Despite an excellent survival rate (2), detailed information on late complications after Takeuchi repair is limited, though intrapulmonary tunnel and baffle complications, MPA stenosis, and coronary artery aneurysm have been reported as serious complications (3).
In the present case, all of these complications associated with Takeuchi repair were observed. However, because of the unique anatomy and the history of previous open thoracic surgery, conventional transthoracic echocardiography alone was not sufficient for a conclusive evaluation in the patient. The recently developed STDME technology can display a virtual multiplanar reconstruction obtained from contrast-enhanced MDCT and corresponding to the real-time transthoracic echocardiographic image side by side. We previously reported the clinical utility of STDME for accurate assessment of the complex anatomy of patients with ACHD (4). Using STDME in the present case, a small fistulous connection in the intrapulmonary baffle with a shunt flow from the coronary artery to the MPA was clearly visualized.
The indication for surgical repair of a baffle leak after Takeuchi repair has not been described in detail. In previous studies, surgical or catheter repair was performed in patients with large baffle leaks and Qp/Qs ratios >1.5, whereas no invasive interventions were performed in patients with small leaks (3,5). In the present case, the shunt flow was small and Qp/Qs was <1.5, and we therefore decided not to intervene on the baffle leak. Details on clinical courses of coronary artery aneurysm after Takeuchi repair also remain unclear. In previous studies, intraluminal thrombi were observed in all patients with coronary artery aneurysms after Takeuchi repair (6,7). Although an intraluminal thrombus was seen in our patient, he was completely asymptomatic and myocardial ischemia was not detected, and we thus concluded that we should not intervene on the coronary artery aneurysm. Instead, an antiplatelet drug and an anticoagulant agent were administered, and close clinical follow-up was considered to be mandatory to monitor the size of the aneurysm.
Follow-Up
The patient has done well for the past 2 years, and no significant changes were observed on follow-up MDCT and echocardiography.
Conclusions
Various late complications have been reported in patients with ALCAPA after Takeuchi repair despite an excellent survival rate. This case showed multiple late structural complications, but appropriate management of structural complications has not been established. Therefore, lifelong care is essential at a center that has experience in caring for patients with complex ACHD.
Funding Support and Author Disclosures
Canon Medical Systems Corporation supported this study with equipment. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this paper.
Appendix
Parasternal Long-Axis Window on Transthoracic Echocardiography Demonstrating Mildly Increased LV Diameter With Preserved LV Ejection Fraction
Parasternal Short-Axis Window on Transthoracic Echocardiography Demonstrating a Severely Dilated Intrapulmonary Baffle
Multidetector Computed Tomography Demonstrating a Severely Dilated Intrapulmonary Baffle in the Main Pulmonary Artery and an Interspersed Aneurysm of the Left Coronary Artery
Simultaneous 2-Screen Display of Multidetector Computed Tomography and Real-Time Echogram Revealing a Small Fistulous Connection in the Intrapulmonary Baffle With a Shunt Flow From the Coronary Artery to the Main Pulmonary Artery
Simultaneous 2-Screen Display of Multidetector Computed Tomography and Real-Time Echogram Also Revealing a Severely Calcified Coronary Artery Aneurysm
References
- 1.Dodge-Khatami A., Mavroudis C., Backer C.L. Anomalous origin of the left coronary artery from the pulmonary artery: collective review of surgical therapy. Ann Thorac Surg. 2002;74:946–955. doi: 10.1016/s0003-4975(02)03633-0. [DOI] [PubMed] [Google Scholar]
- 2.Neumann A., Sarikouch S., Bobylev D. Long-term results after repair of anomalous origin of left coronary artery from the pulmonary artery: Takeuchi repair versus coronary transfer. Eur J Cardiothorac Surg. 2017;51:308–315. doi: 10.1093/ejcts/ezw268. [DOI] [PubMed] [Google Scholar]
- 3.Ginde Salil, Earing Michael G., Bartz Peter J. Late complications after Takeuchi repair of anomalous left coronary artery from the pulmonary artery: case series and review of literature. Pediatr Cardiol. 2012;22:1115–1123. doi: 10.1007/s00246-012-0260-5. [DOI] [PubMed] [Google Scholar]
- 4.Oe H., Watanabe N., Miyoshi T. Potential benefit of a simultaneous, side-by-side display of contrast MDCT and echocardiography over routine sequential imaging for assessment of adult congenital heart disease: a preliminary study. J Cardiol. 2018;72:395–402. doi: 10.1016/j.jjcc.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 5.Hai-Bo H., Kai Y., Xiang-Bin P. Transcatheter closure for baffle leak after Takeuchi repair of anomalous left coronary artery from the pulmonary artery: a case report. Eur Heart J Case Rep. 2018;2:yty028. doi: 10.1093/ehjcr/yty028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunlay S.M., Bonnichsen C., Dearani J.A. Giant coronary artery aneurysm after Takeuchi repair for anomalous left coronary artery from the pulmonary artery. Am J Cardiol. 2014;113:193–195. doi: 10.1016/j.amjcard.2013.08.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Juan Y.H., Saboo S.S., Keraliya A., Khandelwal A. Coronary strictures, intraluminal thrombus and aneurysms: unreported imaging appearance of ALCAPA syndrome post Takeuchi procedure. Int J Cardiol. 2015;186:291–293. doi: 10.1016/j.ijcard.2015.03.242. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Parasternal Long-Axis Window on Transthoracic Echocardiography Demonstrating Mildly Increased LV Diameter With Preserved LV Ejection Fraction
Parasternal Short-Axis Window on Transthoracic Echocardiography Demonstrating a Severely Dilated Intrapulmonary Baffle
Multidetector Computed Tomography Demonstrating a Severely Dilated Intrapulmonary Baffle in the Main Pulmonary Artery and an Interspersed Aneurysm of the Left Coronary Artery
Simultaneous 2-Screen Display of Multidetector Computed Tomography and Real-Time Echogram Revealing a Small Fistulous Connection in the Intrapulmonary Baffle With a Shunt Flow From the Coronary Artery to the Main Pulmonary Artery
Simultaneous 2-Screen Display of Multidetector Computed Tomography and Real-Time Echogram Also Revealing a Severely Calcified Coronary Artery Aneurysm