To the Editor
Interferon gamma (IFNγ) is a central effector cytokine of cellular immunity. It is mainly produced by activated T-cells, natural killer cells and to a lesser extent by professional antigen presenting cells [1]. Its main roles include activation of macrophages, granuloma formation, and augmentation of anti-tumor immunity [2]. In addition, it augments antiviral immunity by inhibiting viral entry, uncoating, translation, and virion assembly [3].
Although the majority of patients infected by SARS-CoV-2 virus experience mild symptoms, approximately 15% develop a moderate phenotype resembling viral pneumonia, with a further subset presenting with severe illness characterized by hyperinflammation and acute respiratory distress syndrome [4]. These moderate and severe forms of COVID-19 typically arise after 7–10 days of illness and are characterized by hypercytokinemia and a cytokine storm, with high levels of TNF-α, IL-1β, IL-1Ra, and IL-6 [5, 6].
Neutralizing anti-IFNγ autoantibodies were first described in 2004 in the context of selective susceptibility to non-tuberculous mycobacterial (NTM) infection [7, 8]. Lymph nodes, bones/joints, and lungs are most commonly affected, with soft tissue and skin involvement (in the form of neutrophilic dermatosis, erythema nodosum, or exanthematous pustulosis) also commonly reported [7, 9].
Here, we report a case of previously fit 58-year-old man of Southeast Asian origin, who was found to have autoantibodies against IFNγ resulting in acquired IFNγ deficiency and NTM and COVID-19 co-infection (NTM-COV+). He initially became unwell in December 2018. Over the following 12 months, he developed folliculitis; episcleritis; intermittent rash with abscesses affecting his chest, arms, and hands (Supplementary Figure 1A, B); weight loss; reduced appetite; fatigue; arthralgia (hands, shoulders, and spine); cervical and supraclavicular lymphadenopathy; and intermittent fever with night sweats.
Investigations revealed a fluctuating leukocytosis (12–33 × 109/L), with neutrophilia, anemia (nadir 87 g/L), persistent thrombocytosis, elevated CRP (peak of 100 mg/L), and low albumin (nadir 28 g/L). Screening tests for autoimmunity, blood-borne viruses, and syphilis were negative. Three IFNγ release assays for tuberculosis were indeterminate. Blood microscopy and culture were negative. PET-CT demonstrated widespread noncalcified lymphadenopathy in the neck, chest, and abdomen, with avid fluorodeoxyglucose uptake. Neutrophilic dermatosis seen in an initial skin sample raised the possibility of Sweet’s syndrome, although dermal fibrosis suggested atypical mycobacterial infection. A cervical lymph node biopsy sample failed to demonstrate any of the hallmarks of lymphoproliferative disease. A differential diagnosis of sarcoidosis or Sweet’s syndrome was made and empirical treatment with prednisolone commenced in December 2019. This improved his rash, weight loss, and lymphadenopathy, but not his fever.
In February 2020, he developed right iliac fossa pain, vomiting, productive cough, and rash. There was significant leukocytosis (26 × 109/L) and CRP was elevated at 243 mg/L. CT imaging revealed new splenomegaly and splenic infarcts. Further dermatology review reported no features of neutrophilic dermatosis, instead resembling dermatitis (Supplementary Figure 1C); repeat skin biopsy histology was suggestive of granulomatous interstitial dermatitis. In light of the patient’s ethnicity, indeterminate IFNγ release assay for TB, and evolving clinical picture, a provisional diagnosis of atypical mycobacterial infection due to IFNγ autoantibodies was made. Bone marrow staining and culture demonstrated growth of mycobacterium avium intracellulare (MAI) after 1 week of incubation. Subsequent mycobacterial blood culture was also positive for MAI.
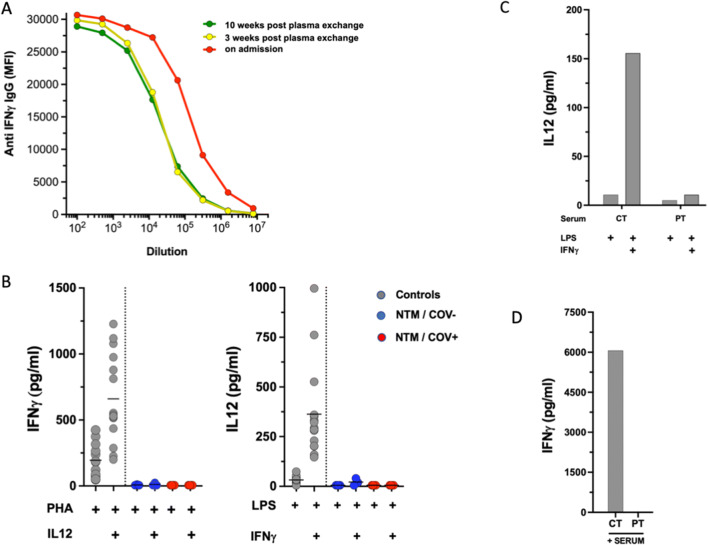
Testing for anti-IFNγ antibodies (Ab), using a Bio-Plex methodology as previously described [10], revealed high titer anti-IFNγ Ab in NTM/COV+ patient comparable to three other patients with known autoantibodies against IFNγ (NTM/COV−) (Figure 1A, Supplementary Figure 3). We then verified the neutralizing capacity of these antibodies and their ability to interfere with IFNγ pathway signaling in an ex vivo setting by functional testing using whole blood or PBMC. NTM/COV+ patient’s response to, and production of, IFNγ was measured in three independent experiments and compared to 3 other NTM/COV− patients and to healthy controls (N = 15). After 24-h stimulation with PHA, IL-12, or a combination of the two, we were unable to detect IFNγ in the supernatants from the patient samples, suggesting that anti-IFNγ Abs were neutralizing the endogenously produced IFNγ (Figure 1B, left panel). This was also observed in samples taken from NTM/COV− patients. By contrast, the HCs demonstrated good production of IFNγ in response to both stimuli. In addition, under the same experimental settings, stimulation with IFNγ failed to induce IL-12 production in the NTM/COV+ patient samples (Figure 1B, right panel). To further demonstrate the neutralizing capacity of the anti-IFNγ Ab, we activated HC PBMC with LPS or LPS + IFNγ in the presence of 20% control or NTM/COV+ patient serum, measuring IL-12 levels after 24-h incubation. Stimulation with LPS or LPS + IFNγ triggered production of IL-12 from HC PBMC incubated with control serum, while HC PBMC incubated with the patient serum failed to produce IL-12 (Figure 1C). This demonstrated that patient serum neutralized both endogenously produced IFNγ and exogenous IFNγ. The capacity of patient serum to neutralize recombinant IFNγ was further confirmed by adding 20% of control or patient serum to RPMI-containing recombinant IFNγ and measuring IFNγ levels by Luminex. The patient serum completely neutralized recombinant IFNγ (Figure 1D). Lastly, we analyzed the patient’s HLA type to determine whether he carried the high-risk HLA-DR alleles associated with anti-IFNγ autoantibodies. The patient was found to carry DRB1*15:02, DRB1*16:02, and DQB1*05:02 (homozygous), all of which have previously been reported to increase the risk of developing anti-IFNγ autoantibodies [11].
Fig. 1.
A Detection and titration of anti-IFNγ antibody. Patient sera were diluted in seven 1/5 steps starting at 1/100. Anti-IFNγ IgG was determined by particle-based flow cytometry on a Luminex analyzer and shown as mean fluorescence intensities (MFI). B Induced IFNγ and IL12 levels after whole blood activation. Cytokines were measured in whole blood after 24-h stimulation using 10 μg/mL PHA or 1 μg/mL LPS alone or in combination with 20 μg/mL IL12 or 20,000 IU/mL IFNγ, respectively. To account for lymphopenia, data were corrected for lymphocyte counts (in response to PHA) or monocyte counts (in response to LPS). Controls are shown as gray circles (N = 15), patients with acquired (a)IFNγ deficiency (N3) are shown as blue circles (NTM/COV−). For the NTM/COV+ patient, data from four experiments are shown as red circles. Cytokine levels are shown as pg/mL. C In vitro inhibition of IFNγ using patient serum. Healthy control PBMC were activated with LPS or LPS + IFNγ in the presence of 20% control (Ct) or patient (NTM/COV+) serum and IL12 levels were measured in the supernatant after 24-h incubation. D IFNγ recovery in the presence of autologous patient (NTM/COV+) serum: 20% control or patient serum was added to RPMI-containing recombinant IFNγ and IFNγ levels were determined by Luminex. No IFNγ could be recovered from the well containing patient serum showing complete antigenic neutralization by the patient’s autoantibody
Treatment for MAI was started 4 weeks after hospitalization. Due to rifabutin-induced hyperbilirubinemia, the patient was established on ethambutol, azithromycin, and amikacin. Prednisolone was continued throughout his hospitalization. Injectable IFNγ-1b (Immukin) treatment [80 μg/2.65 m2 (body surface) 3 weekly] was implemented alongside plasma exchange, in an effort to raise IFNγ levels and reduce titers of anti-IFNγ autoantibodies, respectively (Supplementary Figure 2).
Further immunological investigations showed normal lymphocyte profile with reduced naïve T cells 23% (normal 49–90%). We were interested to determine if the presence of IFNγ Ab had effects on the distribution of CD4 T-helper-cells (Th) Th1, Th2, and Th17, since this might have impacted the patient’s inability to clear the infection. Compared to HC, the patient had similar proportions of Th1, and TH17 cells, and slightly reduced Th2 (Supplementary Figure 1D, E).
At day 37 of admission, the patient was tested positive for SARS-CoV-2 with a nucleic acid amplification test (NAAT) from a nose and throat swab. A previous swab taken on admission had been negative. At the time of screening, the patient was pyrexial (38.1 °C) but had no respiratory symptoms. Chest imaging demonstrated novel subpleural nodules, but no changes indicating COVID-19 pneumonia. Between days 50 and 90, nose and throat swab SARS-CoV-2 NAAT tests were positive on six occasions (Supplementary Figure 2) but were negative from day 103 onwards. Steroid treatment continued uninterrupted throughout this period. The patient did not require oxygen supplementation and had no significant respiratory symptoms. He continued to receive regular plasma exchange and IFNγ-1b injections. However, this combination therapy was unlikely to have made a substantial difference in correcting his acquired immunodeficiency. Serial measurements of anti-IFNγ Ab showed some reduction in titers, but levels remained high (Figure 1A). Experiments looking at the effects of patient serum on levels of exogenously administered IFNγ demonstrated no detectable free IFNγ following incubation with serum (Figure 1D).
He eventually mounted an adequate IgG antibody response to several viral antigens including the trimeric S protein (Supplementary Figure 3). However, his MAI infection remained difficult to control. Plasma exchange and IFNγ-1b injection were stopped, but azithromycin, ethambutol, and rifabutin were continued. In October 2020, he was treated with rituximab to good effect. By April 2021, the patient was systemically well. A PET-CT demonstrated no enlarged LN of focal nodal uptake and his splenomegaly had reduced from 16 to 13 cm. He is due to complete 2 years of anti-MAI therapy (azithromycin, ethambutol, and rifabutin).
To determine whether autoantibodies to IFNγ are associated with severity of COVID-19 infection, we tested sera from three groups; healthy volunteers (HC), healthcare workers with asymptomatic or predominantly mild COVID-19 infection (COV-HCW), and patients hospitalized with COVID-19 (COV-PAT). Both the COV-HCW and the COV-PAT group, showed similarly increased anti-IFNγ Ab levels when compared to healthy controls. However, antibody levels remained low when compared to the NTM/COV+ patient and the NTM/COV− disease controls.
We describe here a single patient with autoantibodies to IFNγ and NTM and COVID-19 co-infection. We investigated whether severity of COVID19 infection is associated with anti-IFNγ Ab by studying two cohorts of infected individuals, one with severe disease and the other with mild/asymptomatic disease. The patient with NMT and COVID-19 co-infection, despite apparent IFNγ deficiency, did not have severe COVID-19 disease. Exploring associations between anti-IFNγ Ab and COVID-19 disease severity in a larger cohort of patients, we found no obvious link. Among infected individuals, both severe and mild or asymptomatic COVID-19 infection patients had similar levels of anti-IFNγ Ab. These autoantibodies appear to develop during the course of infection, since they were not readily detectable in a non-infected cohort. Furthermore, antibody titers were much lower compared to patients with confirmed acquired IFNγ deficiency. This suggests that anti-IFNγ Ab seen in these two groups of patents might be a transient phenomenon, with limited neutralizing capacity against IFNγ.
Unlike type I IFNs, which are required for a robust response to COVID-19 infection, the role of IFNγ is less clearly defined. In experimental models using human epithelial cells, IFNγ has been shown to promote SARS-CoV-2 infection [12]. Another study demonstrated that lower circulating levels of IFNγ are associated with more severe COVID-19 infection course and greater chance of developing lung fibrosis [13], while the functional exhaustion of both type I and type II IFN production was independently linked with a severe disease course [14]. Although serum levels of IFNγ in severe COVID-19 appear to be significantly lower than is typically seen in hyperinflammatory disease states such as secondary hemophagocytic lymphohistiocytosis (HLH) or macrophage activation syndrome (MAS) [15], IFNγ has been shown to act synergistically with TNF at a local tissue level, promoting macrophage activation and lung damage [16, 17].
Our experience suggests that the complete absence of IFNγ signaling does not result in a worse COVID-19 outcome and that IFNγ is not necessary to control this virus. However, the potential role of IFNγ in local hyperinflammatory responses and lung injury remains ill-defined. Arguably, the mild disease phenotype in our patient may have resulted from prolonged corticosteroid therapy rather than impairment of the IFNγ pathway (or both), given that corticosteroid therapy has been clearly shown to reduce inflammatory complications of COVID-19 and improve overall outcomes [18].
Although studies of inborn errors of immunity (IEI) provide unique insights into functioning of the immune system, such models are imperfect. The outcomes of COVID-19 infection in patients with various types of IEI have not been easy to predict. Various retrospective studies show that outcomes are often better than anticipated [19]. However, other factors such as age, sex, and comorbidities, known to be associated with COVID-19 disease severity, also play an important role [20].
Our study suggests a redundant role of IFNγ to control SARS-CoV-2 and provides an outline of what to expect when patients with this rare acquired immune deficiency encounter a viral illness characterized by immune hyperactivation.
Supplementary Information
(DOCX 21 kb)
Acknowledgements
We would like to thank the Royal Papworth Hospital NHS Trust (RPH) Research and Development Team staff for their support in recruitment to the study and RPH patients from who donated serum samples that were used in this study.
Abbreviations
- IFNγ
Interferon gamma
- ARDS
Acute respiratory distress syndrome
- JAK
Janus kinase
- MAS
Macrophage activation syndrome
- NTM
Non-tuberculous mycobacterium
Author Contribution
MK, VP, HM, and EGK collected clinical information; PCA, CC, PH, and GBM performed experiments; RD, GBC, HEB, and SS analyzed data; and MK, VP, and SS wrote first draft of the manuscript. HEB and EGK provided sera for COVID-19 patients and healthy control groups. All authors read, edited, and approved the manuscript. RD and SS design and funded the study.
Funding
This research is supported by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre and grant from CSL Behring. HEB received funding from the Royal Papworth Hospital NHS Trust R&D Pump priming award which was used to support COVID-19 serum surveillance studies.
EGK is supported by the NIHR CRN Greenshoots Award.
Paulina Cortes-Acevedo acknowledges the scholarship and financial support provided by the National Council of Science and Technology (CONACyT) number 829997.
GB-M is supported by grants from UNAM, PIAPI2009.
Data Availability
The data that support the findings of this study are available on request from the corresponding author.
Declarations
Ethics Approval
Ethics approval was granted by the Leeds (East) Research Ethics Committee. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards (ethics approval: IRAS project ID: 96194 REC: 12/WA/0148).
Consent to Participate
Participants provided their consent to participate in this study.
Consent for Publication
Consent was sought and gained from the participant (the main case) to publish the findings of this study.
Competing Interests
The authors declare no competing interests.
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mark Kacar and Paulina Cortes-Acevedo contributed equally to this work.
References
- 1.Castro F, Cardoso AP, Goncalves RM, Serre K, Oliveira MJ. Interferon-gamma at the crossroads of tumor immune surveillance or evasion. Front Immunol. 2018;9:847. doi: 10.3389/fimmu.2018.00847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schroder K, Hertzog PJ, Ravasi T, Hume DA. Interferon-gamma: an overview of signals, mechanisms and functions. J Leukoc Biol. 2004;75(2):163–189. doi: 10.1189/jlb.0603252. [DOI] [PubMed] [Google Scholar]
- 3.MacMicking JD. Interferon-inducible effector mechanisms in cell-autonomous immunity. Nat Rev Immunol. 2012;12(5):367–382. doi: 10.1038/nri3210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, Li P, Zhou Y, Lin YF, Duan Q, Luo G, Fan S, Lu Y, Feng A, Zhan Y, Liang B, Cai W, Zhang L, du X, Li L, Shu Y, Zou H. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Inf Secur. 2020;80(6):656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Y, Shen C, Li J, Yuan J, Wei J, Huang F, et al. Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19. J Allergy Clin Immunol. 2020;146(1):119–27 e4. [DOI] [PMC free article] [PubMed]
- 6.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed]
- 7.Doffinger R, Helbert MR, Barcenas-Morales G, Yang K, Dupuis S, Ceron-Gutierrez L, et al. Autoantibodies to interferon-gamma in a patient with selective susceptibility to mycobacterial infection and organ-specific autoimmunity. Clin Infect Dis. 2004;38(1):e10–4. [DOI] [PubMed]
- 8.Hoflich C, Sabat R, Rosseau S, Temmesfeld B, Slevogt H, Docke WD, et al. Naturally occurring anti-IFN-gamma autoantibody and severe infections with Mycobacterium cheloneae and Burkholderia cocovenenans. Blood. 2004;103(2):673–675. doi: 10.1182/blood-2003-04-1065. [DOI] [PubMed] [Google Scholar]
- 9.Ku CL, Chi CY, von Bernuth H, Doffinger R. Autoantibodies against cytokines: phenocopies of primary immunodeficiencies? Hum Genet. 2020;139(6-7):783–794. doi: 10.1007/s00439-020-02180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Puel A, Doffinger R, Natividad A, Chrabieh M, Barcenas-Morales G, Picard C, et al. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J Exp Med. 2010;207(2):291–297. doi: 10.1084/jem.20091983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ku CL, Lin CH, Chang SW, Chu CC, Chan JF, Kong XF, et al. Anti-IFN-gamma autoantibodies are strongly associated with HLA-DR*15:02/16:02 and HLA-DQ*05:01/05:02 across Southeast Asia. J Allergy Clin Immunol. 2016;137(3):945–948. doi: 10.1016/j.jaci.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 12.Heuberger J, Trimpert J, Vladimirova D, Goosmann C, Lin M, Schmuck R, et al. Epithelial response to IFN-gamma promotes SARS-CoV-2 infection. EMBO Mol Med. 2021;13(4):e13191. [DOI] [PMC free article] [PubMed]
- 13.Hu ZJ, Xu J, Yin JM, Li L, Hou W, Zhang LL, et al. Lower circulating interferon-gamma is a risk factor for lung fibrosis in COVID-19 patients. Front Immunol. 2020;11:585647. [DOI] [PMC free article] [PubMed]
- 14.Ruetsch C, Brglez V, Cremoni M, Zorzi K, Fernandez C, Boyer-Suavet S, et al. Functional exhaustion of type I and II interferons production in severe COVID-19 patients. Front Med (Lausanne) 2020;7:603961. doi: 10.3389/fmed.2020.603961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessel C, Vollenberg R, Masjosthusmann K, Hinze C, Wittkowski H, Debaugnies F, et al. Discrimination of COVID-19 from inflammation-induced cytokine storm syndromes by disease-related blood biomarkers. Arthritis Rheum. 2021. [DOI] [PMC free article] [PubMed]
- 16.Karki R, Sharma BR, Tuladhar S, Williams EP, Zalduondo L, Samir P, et al. Synergism of TNF-alpha and IFN-gamma triggers inflammatory cell death, tissue damage, and mortality in SARS-CoV-2 infection and cytokine shock syndromes. Cell. 2021;184(1):149–68 e17. [DOI] [PMC free article] [PubMed]
- 17.Zhang F, Mears JR, Shakib L, Beynor JI, Shanaj S, Korsunsky I, et al. IFN-gamma and TNF-alpha drive a CXCL10+ CCL2+ macrophage phenotype expanded in severe COVID-19 lungs and inflammatory diseases with tissue inflammation. Genome Med. 2021;13(1):64. doi: 10.1186/s13073-021-00881-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Group RC. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meyts I, Bucciol G, Quinti I, Neven B, Fischer A, Seoane E, et al. Coronavirus disease 2019 in patients with inborn errors of immunity: an international study. J Allergy Clin Immunol. 2021;147(2):520–31. [DOI] [PMC free article] [PubMed]
- 20.Shields AM, Burns SO, Savic S, Richter AG. Consortium UPC-. COVID-19 in patients with primary and secondary immunodeficiency: the United Kingdom experience. J Allergy Clin Immunol. 2021;147(3):870–875. doi: 10.1016/j.jaci.2020.12.620. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 21 kb)
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.