Abstract
To date, metformin remains the first-line oral glucose-lowering drug used for the treatment of type 2 diabetes thanks to its well-established long-term safety and efficacy profile. Indeed, metformin is the most widely used oral insulin-sensitizing agent, being prescribed to more than 100 million people worldwide, including patients with prediabetes, insulin resistance, and polycystic ovary syndrome. However, over the last decades several observational studies and meta-analyses have reported a significant association between long-term metformin therapy and an increased prevalence of vitamin B12 deficiency. Of note, evidence suggests that long-term and high-dose metformin therapy impairs vitamin B12 status. Vitamin B12 (also referred to as cobalamin) is a water-soluble vitamin that is mainly obtained from animal-sourced foods. At the cellular level, vitamin B12 acts as a cofactor for enzymes that play a critical role in DNA synthesis and neuroprotection. Thus, vitamin B12 deficiency can lead to a number of clinical consequences that include hematologic abnormalities (e.g., megaloblastic anemia and formation of hypersegmented neutrophils), progressive axonal demyelination and peripheral neuropathy. Nevertheless, no definite guidelines are currently available for vitamin B12 deficiency screening in patients on metformin therapy, and vitamin B12 deficiency remains frequently unrecognized in such individuals. Therefore, in this “field of vision” article we propose a list of criteria for a cost-effective vitamin B12 deficiency screening in metformin-treated patients, which could serve as a practical guide for identifying individuals at high risk for this condition. Moreover, we discuss additional relevant topics related to this field, including: (1) The lack of consensus about the exact definition of vitamin B12 deficiency; (2) The definition of reliable biomarkers of vitamin B12 status; (3) Causes of vitamin B12 deficiency other than metformin therapy that should be identified promptly in metformin-treated patients for a proper differential diagnosis; and (4) Potential pathophysiological mechanisms underlying metformin-induced vitamin B12 deficiency. Finally, we briefly review basic concepts related to vitamin B12 supplementation for the treatment of vitamin B12 deficiency, particularly when this condition is induced by metformin.
Keywords: Metformin, Vitamin B12 deficiency, Metformin-induced cobalamin deficiency, Diabetes, Type 2 diabetes, Prediabetes, Screening criteria, Neuropathy, Anemia
Core Tip: Over the last decades, vitamin B12 deficiency has been increasingly recognized as a possible consequence of long-term metformin therapy, potentially resulting in clinical manifestations such as hematologic abnormalities and peripheral neuropathy. Metformin-induced vitamin B12 deficiency has relevant implications in light of the growing population of individuals on metformin therapy for the treatment of type 2 diabetes, prediabetes, insulin resistance and polycystic ovary syndrome on a global scale. Notwithstanding, no definite guidelines are currently available for vitamin B12 deficiency screening in metformin-treated patients. We therefore propose a list of criteria for cost-effective vitamin B12 deficiency screening in metformin-treated patients.
INTRODUCTION
Vitamin B12, also known as cobalamin, is a water-soluble vitamin that is primarily obtained from animal-sourced foods such as red meat, poultry, shellfish, milk, eggs and other dairy products, or vitamin B12-fortified foods[1]. Once ingested, vitamin B12 is released from its food carrier proteins by proteolysis in the acidic environment of the stomach, where it binds to a glycoprotein called haptocorrin (also referred to as R-factor or R-protein). Haptocorrin is produced and secreted by the salivary glands. The haptocorrin-vitamin B12 complex protects vitamin B12 from degradation in the acidic environment of the stomach. Once the haptocorrin-vitamin B12 complex reaches the duodenum, pH change and degradation of haptocorrin by pancreatic proteases favor vitamin B12 cleavage from haptocorrin, resulting in the release of vitamin B12 in its free form. In the duodenum, the free vitamin B12 binds to intrinsic factor (IF), a glycoprotein secreted by gastric parietal cells, resulting in the formation of an IF-vitamin B12 complex. The newly formed IF-vitamin B12 complex subsequently binds, in a calcium-dependent manner, to the cubilin receptor (a protein encoded by the CUBN gene) on the enterocytes of the distal ileum, resulting in the absorption of vitamin B12 by receptor-mediated endocytosis. Upon internalization, the IF-vitamin B12 complex is released from its receptor, IF is degraded in lysosomes, and vitamin B12 enters the circulation via the multidrug resistance protein 1 (MDR1) transporter[2]. In the circulation, approximately 20%-25% of vitamin B12 is bound to its binding protein transcobalamin. The transcobalamin-vitamin B12 complex is also known as holotranscobalamin (HoloTC), which represents the biologically active form of cobalamin and allows for cellular uptake of vitamin B12 through specific cell surface transcobalamin receptors[3]. The remaining 75%-80% of vitamin B12 is bound to haptocorrin and is stored in the liver. Some vitamin B12 is excreted in bile and undergoes enterohepatic circulation[1,4,5].
At the cellular level, vitamin B12 serves as a cofactor for the enzyme methionine synthase, which catalyzes the conversion of homocysteine into methionine. The overall reaction takes place in the cytosol and transforms 5-methyl-tetrahydrofolate (5-methyl-THF) into THF while transferring a methyl group to homocysteine to synthesize methionine. THF is then converted into intermediates that are used in the synthesis of pyrimidine bases of DNA. Therefore, vitamin B12 deficiency leads to homocysteine accumulation, impaired DNA synthesis, and hematologic abnormalities such as formation of hypersegmented neutrophils and megaloblastic anemia, a condition in which the bone marrow produces unusually large, structurally abnormal and immature red blood cells called megaloblasts as a consequence of ineffective hematopoiesis[4]. Anemia can be associated with various symptoms, including pallor, palpitations, tachycardia, and fatigue, which are frequently observed in patients with vitamin B12 deficiency. Although megaloblastic anemia is the most common hematologic abnormality, vitamin B12 deficiency can potentially affect all bone marrow cell lineages, resulting in pancytopenia[6].
Vitamin B12 also acts as a cofactor for the enzyme methylmalonyl-CoA mutase, which catalyzes the conversion of methylmalonyl-CoA to succinyl-CoA, a reaction that takes place in the mitochondria[1]. Thus, vitamin B12 deficiency results in the accumulation of methylmalonyl-CoA that is subsequently converted to methylmalonic acid (MMA), whose plasma levels are often elevated in patients with vitamin B12 deficiency. In subjects with vitamin B12 deficiency, increased levels of MMA and homocysteine have been suggested to contribute to myelin damage (myelopathy) and, as a consequence, to peripheral and autonomic neuropathy[1,4,7]. Neurologic manifestations of vitamin B12 deficiency include progressive axonal demyelination, impaired sensory and peripheral nerve function, subacute combined degeneration of the spinal cord, areflexia and loss of proprioception and vibration sensitivity[5,8,9]. The aforementioned neurologic manifestations can be erroneously interpreted as features of diabetic neuropathy in diabetic patients who are chronically treated with metformin. Failure to identify the cause of neuropathy can lead to progression of central and/or peripheral nerve damage, which may be arrested, but not completely reversed, by vitamin B12 replacement in some instances[10]. Neurocognitive manifestations such as poor memory performance, cognitive impairment, dementia, delirium, depression and episodes of psychosis are also possible in the presence of severe and chronic vitamin B12 deficiency[5,8,11]. Other symptoms that have been reported in adult patients with vitamin B12 deficiency include glossitis, skin hyperpigmentation, infertility, hearing loss, bone disease and macular degeneration[8].
BIOMARKERS OF VITAMIN B12 STATUS AND DEFINITION OF VITAMIN B12 DEFICIENCY
To date, there is no consensus about the exact definition of vitamin B12 deficiency[1]. Indeed, there is still a significant debate within the scientific community about the specific cut-off values that should be applied to define a low vitamin B12 status and about the definition of the best biomarker or combination of biomarkers to assess vitamin B12 status[1,12]. Varying cut-off values invariably lead to underestimating or overestimating the incidence of vitamin B12 deficiency. With regard to the definition of an optimal vitamin B12 status, a low vitamin B12 status (frank vitamin B12 deficiency) is generally defined as total serum vitamin B12 levels of < 148 pmol/L, with levels between 148 and 221 pmol/L being considered as “borderline” or suggestive of “marginal deficiency”[5].
As a matter of fact, there has been a debate about the clinical significance of biochemical vitamin B12 deficiency vs true tissue deficiency, and whether subclinical (i.e. mild and asymptomatic) vitamin B12 deficiency represents a public health concern[13]. Discussion of issues regarding the sensitivity and specificity of individual biomarkers of vitamin B12 status led a roundtable on NHANES monitoring of those biomarkers to agree that a comprehensive and accurate assessment of true tissue vitamin B12 deficiency should include at least one biomarker of circulating vitamin B12 (total vitamin B12 or HoloTC) coupled with one functional (metabolic) biomarker of vitamin B12 status, such as MMA or total homocysteine[13]. In fact, several studies have established that serum vitamin B12 has a limited diagnostic value as a stand-alone marker because of its low specificity and sensitivity in identifying a true tissue vitamin B12 deficiency. Low serum levels of vitamin B12 thus may not necessarily represent a true tissue deficiency[5,12]. A major limitation of the measurement of total serum vitamin B12 is that it assesses total circulating vitamin B12, of which approximately 80% is bound to haptocorrin and is therefore not bioavailable for cellular uptake. Moreover, this assay does not reliably reflect the cellular vitamin B12 status[12]. Studies assessing serum and cellular vitamin B12 showed that serum vitamin B12 levels do not always reflect cellular vitamin B12 status[12,14]. For instance, patients with inborn errors of vitamin B12 metabolism can exhibit low or normal serum values of vitamin B12, while being deficient at the cellular level[12]. In addition, severe functional vitamin B12 deficiency has been documented in the presence of normal or even elevated levels of serum vitamin B12[12], given that serum vitamin B12 levels can be maintained at the expense of cobalamin tissue stores[15].
In light of the abovementioned remarks, measurement of functional biomarkers of vitamin B12 status (homocysteine and MMA) may be useful to confirm the diagnosis of true vitamin B12 deficiency, particularly in the presence of low-normal total serum vitamin B12 levels and/or clinical suspicion of vitamin B12 deficiency[1]. Therefore, total vitamin B12, its bioactive protein-bound form HoloTC, homocysteine and MMA are the preferred serum biomarkers to accurately assess vitamin B12 status[12]. However, it is worth noting that serum levels of homocysteine and MMA can be elevated even in the presence of folate deficiency, which can also be associated with macrocytic anemia and thereby confused with vitamin B12 deficiency. Thus, measurement of serum folate, MMA and homocysteine levels can help to distinguish vitamin B12 deficiency from folate deficiency. As discussed earlier, serum levels of both homocysteine and MMA are often elevated in the presence of true vitamin B12 deficiency. Conversely, homocysteine levels are elevated but MMA levels are normal in the presence of folate deficiency[4]. Yet, it is also worth reminding that both homocysteine and MMA levels can be elevated in the presence of renal impairment[1].
CAUSES OF VITAMIN B12 DEFICIENCY
Apart from long-term metformin therapy (discussed later in the text), several causes and conditions increase the risk of vitamin B12 deficiency (Table 1), as it has been reviewed elsewhere[5,8,16]. Those conditions should be identified promptly in metformin-treated patients with vitamin B12 deficiency for a proper differential diagnosis.
Table 1.
Causes of vitamin B12 deficiency and underlying mechanisms
|
Conditions potentially associated with vitamin B12 deficiency
|
Underlying mechanisms
|
| General malnutrition, chronic alcohol abuse, and vegan or strict vegetarian diets | Low or inadequate dietary intake of foods containing vitamin B12 |
| Older age | Vitamin B12 malabsorption and deficiency due to inadequate dietary intake are common in the elderly |
| Gastric bypass, partial or complete gastrectomy, gastric reduction, bariatric surgery and chronic gastritis due to Helicobacter pylori infection | Impaired IF secretion |
| Atrophic gastritis (an autoimmune disease characterized by the presence of antibodies directed against gastric parietal cells and IF) | Immune-mediated destruction of gastric parietal cells, gastric mucosal atrophy, hypochlorhydria, decreased IF production, subsequent vitamin B12 malabsorption, vitamin B12 deficiency and pernicious anemia (a type of megaloblastic anemia) |
| Long-term use (≥ 12 mo) of drugs altering gastric acid secretion or gastric pH (e.g., PPIs, H2RAs and antacids) | These drugs reduce the production of hydrochloric acid by gastric parietal cells; as a consequence, vitamin B12 is not adequately released from the food matrix due to insufficient hydrochloric acid and low pepsin activity |
| Long-term use of metformin | The underlying mechanism accounting for metformin-induced vitamin B12 deficiency is not fully understood, although it may involve one or more of the following: (1) Interference with the calcium-dependent binding of the IF-vitamin B12 complex to the cubilin receptor on enterocytes at the ileum level; (2) Interaction with the cubilin endocytic receptor; (3) Alteration in small intestine motility leading to small intestinal bacterial overgrowth and subsequent inhibition of IF-vitamin B12 complex absorption in the distal ileum; (4) Alteration in bile acid metabolism and reabsorption; (5) Increased liver accumulation of vitamin B12; and (6) Reduced IF secretion by gastric parietal cells |
| Use of medications that affect vitamin B12 absorption or metabolism including the bile acid resin cholestyramine (used to treat hypercholesterolemia), colchicine (used for acute gout) and many antibiotics such as neomycin and the anti-tuberculosis drug para-aminosalicylic acid1 | Cholestyramine can chelate IF; colchicine and antibiotics can inhibit endocytosis of the IF-vitamin B12 complex |
| Bacterial overgrowth syndromes, ileal resection or gastrointestinal diseases such as terminal ileitis, celiac disease, inflammatory bowel disease, Crohn’s disease and tropical sprue | Altered absorption of the IF-vitamin B12 complex in the terminal ileum; intestinal villous atrophy and mucosal injury (celiac disease, Crohn’s disease and tropical sprue) |
| Intestinal parasitic infestations (often accompanied by eosinophilia) caused by the protozoan Giardia lamblia or the fish tapeworm Diphyllobothrium latum | Vitamin B12 malabsorption through vitamin B12 trapping by the parasites |
| Disorders of the exocrine pancreas or pancreatectomy | Insufficient pancreatic enzyme activity leads to a reduction in the proteolytic degradation of haptocorrin (mediated by pancreatic proteases in the small intestine); as a consequence, vitamin B12 remains bound to haptocorrin, cannot form the IF-vitamin B12 complex and is not available for absorption by the enterocytes in the distal ileum |
| Nitrous oxide anesthesia or recreational use of nitrous oxide | Irreversible oxidation and inactivation of the coenzyme form of vitamin B12 (methylcobalamin) at the active site of the vitamin B12-dependent methionine synthase reaction, resulting in increased levels of MMA and homocysteine |
| Inherited disorders affecting the sequential steps in the assimilation, transport and intracellular processing and metabolism of vitamin B12 | Reduced expression, binding activity or affinity of receptors and proteins involved in transport, intracellular processing and metabolism of vitamin B12 |
Unlike long-term use of proton-pump inhibitors, histamine H2-receptor antagonists or metformin, the frequency or duration of use of these drugs is usually insufficient to result in clinical vitamin B12 deficiency. H2RAs: Histamine H2-receptor antagonists; IF: Intrinsic factor; PPIs: Proton-pump inhibitors; MMA: Methylmalonic acid.
Populations at risk for vitamin B12 deficiency
Specific populations at risk for development of vitamin B12 deficiency include elderly individuals, pregnant women and selected ethnic and racial groups[5]. Vitamin B12 deficiency is more common in older individuals, particularly among those over 65 years of age, who have a prevalence of cobalamin deficiency of approximately 10%-15%[5,17,18]. The prevalence of vitamin B12 deficiency is even higher in the “oldest-old”, with reports of approximately 23% of octogenarians and 35% of centenarians[19]. Possible causes of vitamin B12 in elderly people range from malabsorption and/or poor dietary intake to a number of age-related comorbidities and underlying conditions (Table 1).
Pregnancy can also alter maternal vitamin B12 status by facilitating the transfer of cobalamin to the fetus and infant[5]. The actual prevalence of vitamin B12 deficiency during pregnancy appears to vary across geographic regions, being reported as lower than 10% in Brazil and Canada and greater than 70% in some areas of Turkey and India[5]. Total plasma vitamin B12 levels progressively decrease during pregnancy, and the reduction is often accompanied by a moderate increase in MMA levels, suggesting a functional depletion in intracellular cobalamin status[20,21]. The pregnancy-related decline in vitamin B12 levels may result from alterations in haptocorrin-bound cobalamin[22]. Nonetheless, the assessment of vitamin B12 status as well as the evaluation of the actual prevalence of vitamin B12 deficiency during pregnancy are challenging because of the profound anatomical and physiological changes that limit the use of the established reference ranges employed for determination of cobalamin status in non-pregnant women[5,20].
The prevalence of vitamin B12 deficiency has also been reported to vary across different ethnic and racial groups, probably because of genetic factors and/or cultural and religious practices that predispose different populations to diverse levels of dietary intake of animal products, especially red meat. In a study conducted in participants of the population-based multidisciplinary Georgia Centenarian Study, Johnson et al[19] found that the probability of being vitamin B12-deficient was significantly increased (2 times higher) in whites compared to African Americans. Another observational study by Carmel et al[23] reported that vitamin B12 deficiency was most common in elderly white men and least common in black and Asian American women. A large cross-sectional survey conducted in New Zealanders aged ≥ 15 years showed that Māori/Pacific and East/South-East Asian groups had the highest vitamin B12 levels, whereas those most at risk of low vitamin B12 status were South Asians, including people with ancestral origins in the Indian subcontinent[24]. Māori and Pacific Island groups were the least likely to have inadequate vitamin B12 intakes compared with New Zealand Europeans, while the latter group was more likely to have an adequate vitamin B12 status compared with South Asians[24]. Another study confirmed a higher prevalence of vitamin B12 deficiency in South Asians compared with the general population[25].
METFORMIN-INDUCED VITAMIN B12 DEFICIENCY: CLINICAL EVIDENCE
More than 60 years after its first clinical use, metformin is still recommended as the first-line oral glucose-lowering drug in most clinical guidelines on the management of type 2 diabetes (T2D) thanks to its well-established long-term safety and efficacy profile[26]. Possible side effects of metformin include gastrointestinal intolerance[27] and the rare occurrence of lactic acidosis, which is most likely in the presence of moderate to severe chronic kidney disease. However, moderate to severe renal impairment is a major contraindication to the clinical use of metformin[28]. Metformin is usually well tolerated and effective in maintaining glucose control in the long-term[29]. Indeed, metformin is still the most widely used oral antihyperglycemic (insulin-sensitizing) agent, being prescribed to more than 100 million people worldwide, including patients with prediabetes, insulin resistance and polycystic ovary syndrome (PCOS)[30]. Yet, in recent decades, several observational studies, systematic reviews and meta-analyses have reported an association between long-term metformin therapy and biochemical vitamin B12 deficiency, including frank deficiency or borderline vitamin B12 status[31-37]. Evidence suggests that metformin impairs vitamin B12 status primarily in a dose- and duration-dependent manner (discussed later in the text).
The reported prevalence of vitamin B12 deficiency in metformin-treated patients with diabetes varies across studies, ranging from approximately 6% to 50%[31,38-41]. The first reports documenting this association were published in the late 1960s, when annual serum vitamin B12 testing was already suggested as a valid screening measure for early detection of vitamin B12 deficiency in patients on long-term metformin therapy[42,43]. However, the exact influence of both the dose and duration of metformin therapy on vitamin B12 status is still not entirely understood. A cross-sectional study conducted by de Groot-Kamphuis et al[38] found that patients with T2D using metformin had a significantly higher prevalence of vitamin B12 deficiency compared with patients not using metformin (14.1% vs 4.4%, with a median duration of metformin use of 4.9 years). Moreover, each 100 mg step in metformin dose increased by 8% the odds of having vitamin B12 deficiency, but metformin use did not predict the chance of having anemia or neuropathy[38]. A similar cross-sectional study conducted in 550 T2D patients using metformin (mean treatment duration of 64 mo and mean daily dose of 1306 mg) found that higher daily and cumulative doses of metformin (1 mg/d increase of daily dose and 10 g increase of cumulative dose) were strongly associated with lower HoloTC and cobalamin concentrations[39]. Nevertheless, authors did not find a relationship between the duration of metformin use and cobalamin/HoloTC concentrations[39]. A nested case-control study conducted in Hong Kong also suggested that an increased risk of vitamin B12 deficiency was associated with the current dose and duration of metformin therapy in patients with diabetes[44]. Authors found that each 1 g/d metformin dose increment conferred a more than 2-fold increased risk of developing vitamin B12 deficiency (adjusted odds ratio of 2.88, 95% confidence interval: 2.15-3.87; P < 0.001). In patients using metformin for 3 years or more, the adjusted odds ratio was 2.39 (95% confidence interval: 1.46-3.91; P = 0.001) compared with those receiving metformin for less than 3 years[44].
Shivaprasad et al[45] recently conducted a prospective observational study to assess the combined effect of both dose and duration of metformin therapy on vitamin B12 levels in 2887 patients with T2D. They found vitamin B12 levels of < 200 pg/mL and between 200 and 300 pg/mL in 24.5% and 34.5% of metformin users, respectively. The percentages were significantly higher than those observed in non-metformin users (17.3% and 22.6%, respectively). To quantify metformin usage, authors defined a “metformin usage index” (MUI) as the product of the daily metformin dose (mg) and its duration (years) divided by 1000. Participants who were not on continuous metformin therapy for at least 6 mo prior to recruitment were included in a non-metformin user group. Interestingly, there was a significant association between a MUI value of > 5 and a high risk of vitamin B12 deficiency. Multistep logistic regression analysis adjusted for confounding variables (age, duration of T2D, body mass index, and glycated hemoglobin) found the highest risk of developing vitamin B12 deficiency in patients with a MUI value of > 15, followed by patients with a MUI value of > 10. The lowest risk was found in T2D patients with a MUI value of < 5[45]. Therefore, MUI may be a valid tool to identify individuals at increased risk of vitamin B12 deficiency among T2D patients on continuous metformin therapy for at least 6 mo.
Even though definitive screening guidelines are lacking, the 2021 American Diabetes Association Standards of Medical Care in Diabetes recommend to consider a periodic assessment of vitamin B12 levels in patients with long-term metformin use, including those with prediabetes, peripheral neuropathy or anemia. This recommendation is based on a grade B level of evidence deriving from well-conducted case-control studies, prospective cohort studies and meta-analyses of cohort studies[46], including a report from the Diabetes Prevention Program Outcomes Study (DPPOS) published in The Journal of Clinical Endocrinology & Metabolism in 2016 by Aroda et al[32]. The design of the latter study consisted of a secondary analysis from the Diabetes Prevention Program (DPP)/DPPOS involving over 2000 patients across 27 centers in the United States. Participants with elevated fasting blood glucose, impaired glucose tolerance, and overweight or obesity were assigned to the placebo group (n = 1082) or to the metformin group (850 mg twice daily; n = 1073) for a mean follow-up of 3.2 years. Participants in the metformin group received open-label metformin for an additional 9 years. Authors found that low serum vitamin B12 levels (≤ 203 pg/mL) occurred with a significantly higher frequency in the metformin group than in the placebo group at 5 years (4.3% vs 2.3%). Furthermore, combined low and borderline-low vitamin B12 (≤ 298 pg/mL) was significantly more frequent in metformin group at 5 and 13 years. Importantly, authors reported that approximately 50% of participants with low vitamin B12 levels in their cohort had concurrently increased homocysteine levels, suggesting the presence of a true tissue deficiency of vitamin B12. Moreover, years of metformin use were associated with an increased risk of vitamin B12 deficiency. When the metformin and placebo groups were combined, the odds ratio associated with vitamin B12 deficiency per year of metformin use was 1.13 (95% confidence interval: 1.06-1.20) after adjusting for confounders such as age, sex, baseline body mass index, weight change, diabetes status, and prescription of acid suppression therapy[32]. The prevalence of anemia was higher in the metformin group, but did not differ by vitamin B12 status. The prevalence of neuropathy was significantly higher among metformin group participants with low vitamin B12 levels compared with metformin-treated participants with normal or borderline vitamin B12 levels[32]. In line with those findings, a cross-sectional study by Kim et al[33] found that metformin use in T2D patients for at least 6 mo and at a dose of ≥ 1500 mg/d may represent a major factor related to vitamin B12 deficiency. Of note, authors found that a metformin dose of ≥ 2000 mg was associated with the highest risk of vitamin B12 deficiency. Compared with the group taking a daily metformin dose of < 1000 mg, the adjusted odds ratios for 1000-1500 mg, 1500-2000 mg, and ≥ 2000 mg groups were 1.72 (P = 0.080), 3.34 (P < 0.001) and 8.67 (P < 0.001), respectively. Moreover, serum homocysteine levels were negatively correlated with vitamin B12 levels, suggesting that vitamin B12 deficiency induced by metformin may occur at the tissue level[33].
A recent retrospective study conducted in a large cohort of adult patients (n = 13489) who had received metformin for more than 1 year aimed to assess the appropriateness and benefits of screening recommendations for vitamin B12 deficiency[47]. The mean time between metformin initiation and incidence of vitamin B12 deficiency was 5.3 years. An older patient subgroup (> 65 years of age) had a significantly higher vitamin B12 deficiency rate compared with younger patients (4.2% vs 2.5%). In multivariable logistic regression models, older age was the only factor associated with vitamin B12 deficiency, while African-American ethnicity almost reached statistical significance as a protective factor. These results suggest that patients who have been using metformin for more than 5 years and patients older than 65 are at increased risk for vitamin B12 deficiency. Therefore, authors concluded that screening for vitamin B12 deficiency might be considered in such populations even if they are asymptomatic for the deficiency[47].
A prospective case-control study conducted in T2D patients with concurrent symptomatic peripheral neuropathy found that patients who had received metformin for more than 6 mo with a mean cumulative metformin exposure of 3389.5 g, compared with those without metformin exposure, had lower cobalamin levels and higher fasting MMA and homocysteine levels accompanied by more severe peripheral neuropathy (assessed by clinical and electrophysiological markers)[48]. The cumulative metformin dose was inversely correlated with serum vitamin B12 and positively correlated with fasting serum MMA and homocysteine. In addition, the median Toronto Clinical Scoring System (TCSS) and Neuropathy Impairment Score (NIS) total scores were both significantly higher in the metformin-treated group and had a strong positive correlation with increasing cumulative metformin dose[48]. In keeping with those findings, a post-hoc analysis of a randomized controlled 4.3-year trial conducted in insulin-treated T2D patients reported that addition of metformin not only reduced serum vitamin B12 levels, but also gradually increased serum MMA levels[49]. In metformin users, the increase in MMA levels was also associated with significant worsening of symptoms of neuropathy, assessed by a validated neuropathy score[49].
A possible explanation for the delayed occurrence of biochemical or clinical vitamin B12 deficiency in patients on metformin therapy relies on the low daily requirement of vitamin B12 (approximately 2.4 μg/d) and on its substantial hepatic storage of around 2500 μg. Indeed, clinical manifestations of vitamin B12 deficiency can become evident upon depletion of the body stores to as little as 5%-10%, which may occur several years (up to 10 years) after the initial exposure to metformin or to other risk factors or conditions predisposing to vitamin B12 deficiency[50]. However, older adults may exhibit depleted vitamin B12 stores[51] and may therefore be particularly susceptible to vitamin B12 deficiency even after a short-term period of metformin therapy. For instance, Leung et al[52] showed that short-term (3-mo) metformin use decreased plasma levels of total cobalamin, total haptocorrin and haptocorrin-bound cobalamin in an elderly diabetic population.
Evidence also suggests that acid-suppressing medications such as histamine H2-receptor antagonists (H2RAs) and proton-pump inhibitors (PPIs) can interfere with vitamin B12 absorption by reducing the release of dietary vitamin B12 from food proteins[53]. Notably, Long et al[54] reported that the concomitant use of metformin and PPIs in patients with T2D may increase the risk of vitamin B12 deficiency by exerting further deleterious effects on vitamin B12 status. This has relevant clinical implications, given that approximately 40% of T2D patients are reported to experience symptomatic gastroesophageal reflux disease (GERD), and PPIs and H2RAs represent the most widely prescribed drugs for treatment of GERD in this population[53].
Metformin-induced vitamin B12 deficiency: implications for diabetic neuropathy
Metformin-induced vitamin B12 deficiency (also known as MICD or metformin-induced cobalamin deficiency) can exacerbate nerve damage in diabetic patients with preexisting neuropathy, resulting in the development of a mixed “diabetic and MICD-related neuropathy”. Hashem et al[55] recently conducted a case-control, prospective, observational study in 150 adults with T2D and diabetic peripheral neuropathy (DPN) to establish whether metformin represents a risk factor for DPN. The study cohort included 75 patients who received metformin for the previous 6 mo or more and 75 patients who did not receive metformin for the previous 6 mo but had received other oral antihyperglycemic drugs. Compared with the control patients, the metformin-treated patients had significantly higher homocysteine and MMA levels, along with significantly lower plasma cobalamin levels (222 pmol/L vs 471 pmol/L; P < 0.001). Moreover, metformin-treated patients had a significantly higher frequency of moderate to severe DPN and higher TCSS total scores. Spearman’s correlation revealed a significant negative correlation between plasma cobalamin levels and higher metformin doses, as well as a significant positive correlation between TCSS and increased metformin dose. Metformin-treated patients also showed significantly lower median conduction velocity and sensory nerve action potentials for superficial peroneal and sural nerves. In addition, the severity of DPN was inversely related to plasma cobalamin levels and directly related to higher levels of both homocysteine and MMA. Importantly, multivariate logistic regression analysis of independent predictors of DPN in metformin-treated patients revealed that longer duration of diabetes and metformin therapy were significantly associated with a greater incidence of DPN. Larger doses and longer duration of metformin therapy were also independent predictors of DPN[55].
In a recent 12-mo, randomized, double-blind, placebo-controlled trial, 90 adults with T2D on metformin therapy for at least 4 years and with both diabetic peripheral and autonomic neuropathy were randomized to receive vitamin B12 (1 mg of oral methylcobalamin) or placebo on a daily basis[56]. All participants had baseline vitamin B12 levels of < 400 pmol/L. Compared with placebo, vitamin B12 supplementation led to a significant increase in vitamin B12 levels (from 232.0 ± 71.8 pmol/L at baseline to 776.7 ± 242.3 pmol/L at follow-up) that was accompanied by a significant improvement in Michigan Neuropathy Screening Instrument Questionnaire, quality of life and pain scores, vibration perception threshold, electrochemical skin conductance in the feet, and sural nerve conduction velocity and amplitude[56]. Overall, these findings highlight the importance of diagnosing and correcting vitamin B12 deficiency in metformin-treated patients with diabetes and neuropathy in order to prevent or halt the exacerbation and progression of nerve damage.
POTENTIAL PATHOPHYSIOLOGICAL MECHANISMS OF METFORMIN-INDUCED VITAMIN B12 DEFICIENCY
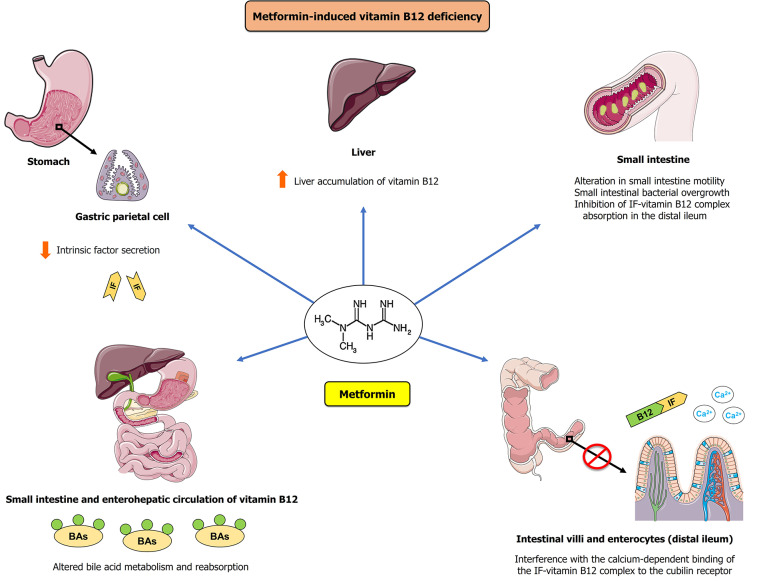
The exact mechanisms underlying metformin-induced vitamin B12 deficiency are still not fully understood[37]. However, the mechanisms are thought to cause vitamin B12 deficiency mainly through altered vitamin B12 absorption and metabolism (Figure 1)[1,57-60]. Proposed mechanisms accounting for metformin-induced vitamin B12 deficiency include: (1) Interference with calcium-dependent binding of the IF-vitamin B12 complex to the cubilin receptor on enterocytes at the ileum level and/or interaction with the cubilin endocytic receptor; (2) Alteration in small intestine motility, leading to small intestinal bacterial overgrowth and subsequent inhibition of IF-vitamin B12 complex absorption in the distal ileum; (3) Alteration in bile acid metabolism and reabsorption, resulting in impaired enterohepatic circulation of vitamin B12; (4) Increased liver accumulation of vitamin B12, resulting in altered tissue distribution and metabolism of vitamin B12; and (5) Reduced IF secretion by gastric parietal cells. Of note, inhibition of calcium-dependent absorption of the IF-vitamin B12 complex at the terminal ileum has been increasingly recognized as the most plausible mechanism accounting for metformin-induced vitamin B12 deficiency. Indeed, the inhibitory effect is reversed by calcium supplementation[61].
Figure 1.
Postulated mechanisms accounting for metformin-induced vitamin B12 deficiency. Metformin may cause vitamin B12 deficiency through one or more of the following mechanisms: (1) Interference with the calcium-dependent binding of the intrinsic factor (IF)-vitamin B12 complex to the cubilin receptor on enterocytes at the ileum level and/or interaction with the cubilin endocytic receptor; (2) Alteration in bile acid metabolism and reabsorption, resulting in impaired enterohepatic circulation of vitamin B12; (3) Reduced IF secretion by gastric parietal cells; (4) Increased liver accumulation of vitamin B12, resulting in altered tissue distribution and metabolism of vitamin B12; and (5) Alteration in small intestine motility, resulting in small intestinal bacterial overgrowth and subsequent inhibition of IF-vitamin B12 complex absorption in the distal ileum. B12: Vitamin B12; BAs: Bile acids; IF: Intrinsic factor.
VITAMIN B12 DEFICIENCY IN METFORMIN-TREATED PATIENTS: PROPOSED CRITERIA FOR A COST-EFFECTIVE SCREENING
To date, no definite guidelines are available for the screening of vitamin B12 deficiency in patients taking metformin. Thus, vitamin B12 deficiency remains frequently unrecognized in such patients. According to the British Society for Haematology guidelines for diagnosis and treatment of vitamin B12 deficiency, no definitive advice can be given on the desirable frequency of measurement of serum vitamin B12 in patients with T2D on metformin therapy. However, the same guidelines recommend to check serum vitamin B12 levels in the presence of strong clinical suspicion of deficiency[62].
Based on the current evidence, we therefore propose a list of criteria for a cost-effective vitamin B12 deficiency screening in metformin-treated patients. The criteria could serve as a practical guide for identifying individuals at high risk for vitamin B12 deficiency who may require vitamin B12 supplementation as well as a periodic assessment of their cobalamin status (Table 2). Of note, we suggest to consider screening for vitamin B12 deficiency in selected individuals even if they are asymptomatic for deficiency. The proposed screening criteria may be useful to prevent the development or worsening of the clinical consequences of vitamin B12 deficiency, particularly anemia and peripheral neuropathy, by allowing for a prompt diagnosis and treatment of vitamin B12 deficiency.
Table 2.
Proposed criteria for cost-effective screening and subsequent intermittent periodic testing of vitamin B12 status in metformin-treated patients
|
Proposed criteria
|
| (1) A comprehensive assessment of vitamin B12 status aimed to accurately detect a true tissue vitamin B12 deficiency should include at least one biomarker of circulating vitamin B12 (total vitamin B12 or HoloTC) coupled with one functional (metabolic) biomarker of vitamin B12 status (MMA and/or total homocysteine). A recent complete blood count is also recommended |
| (2) Screening for vitamin B12 deficiency should be performed in the presence of one or more of the following risk factors or conditions: (a) Strong clinical suspicion of deficiency: clinical evidence of vitamin B12 deficiency, including unexplained macrocytic anemia, neurological symptoms and peripheral neuropathy1; (b) Preexisting diabetic peripheral and/or autonomic neuropathy2; (c) Duration of metformin treatment ≥ 5 yr; (d) Older adults: age ≥ 65 yr; (e) High cumulative metformin exposure defined by a MUI value of > 5 (this criterion applies to patients with type 2 diabetes treated with metformin for at least 6 mo)3; (f) Metformin dose of ≥ 1500 mg/d for a duration of at least 6 mo (the highest risk of vitamin B12 deficiency has been observed with a daily metformin dose of ≥ 2000 mg); (g) Concomitant long-term use (≥ 12 mo) of acid-suppressing medications such as PPIs and H2RAs; and (h) Concomitant presence of risk factors or comorbidities associated with an increased risk of vitamin B12 deficiency (reviewed in Table 1) warrants screening for deficiency based on clinical judgement |
Based on results from Diabetes Prevention Program/Diabetes Prevention Program Outcomes Study[32], peripheral neuropathy refers to monofilament-defined neuropathy (detection of an abnormal monofilament examination).
Screening for vitamin B12 deficiency should be routinely performed in metformin-treated diabetic patients with a preexisting diabetic peripheral and/or autonomic neuropathy. Once diagnosed, metformin-induced vitamin B12 deficiency should be corrected promptly in such patients in order to counteract the exacerbation of nerve damage and prevent the development or progression of a mixed “diabetic and metformin-induced cobalamin deficiency-related neuropathy”.
Metformin Usage Index (MUI) is defined as the product of the daily metformin dose (mg) and its duration (yr) divided by 1000. For example, 1000 mg of metformin used for a duration of 1 yr is equivalent to 1 MUI (1000 × 1/1000 = 1 MUI). This criterion applies to patients with type 2 diabetes treated with metformin for at least 6 mo, based on the results from the prospective observational study conducted by Shivaprasad et al[45]. H2RAs: Histamine H2-receptor antagonists; HoloTC: Holotranscobalamin; MMA: Methylmalonic acid; MUI: Metformin Usage Index; PPIs: Proton-pump inhibitors.
Apart from metformin-treated patients with insulin resistance, prediabetes, T2D and PCOS, another subgroup in which routine screening for vitamin B12 deficiency may be considered includes patients with type 1 diabetes (T1D) taking metformin as non-insulin adjunct therapy, especially in the presence of peripheral neuropathy or unexplained anemia. In this regard, it is also worth reminding that T1D patients are at increased risk for other autoimmune diseases such as autoimmune gastritis and pernicious anemia, which can independently lead to the development of vitamin B12 deficiency[63,64].
TREATMENT OF VITAMIN B12 DEFICIENCY
In selected individuals who are at higher risk for marginal vitamin B12 insufficiency, the goal is first of all to prevent the development of frank vitamin B12 deficiency, then to treat such deficiency by adequate repletion when it occurs[5]. This approach allows for prevention of clinical consequences of vitamin B12 deficiency, including megaloblastic anemia and neurologic manifestations such as peripheral neuropathy.
The recommended dietary allowance of vitamin B12 for subjects without malabsorption has been set at approximately 2.4 μg/d for adult men and non-pregnant women (2.6 μg/d for pregnant women)[8], even though a daily intake of 4-7 μg has been associated with lower serum MMA levels[65]. There is no defined tolerable upper intake level of vitamin B12[66]. As vitamin B12 is relatively inexpensive, easy to administer, safe and well tolerated, a personalized approach to meet the need of the individual patient is generally deemed as harmless[5].
Synthetic vitamin B12 has long been available in the form of cyanocobalamin, both for oral and injectable use. Subsequently, naturally occurring forms of vitamin B12 have become commercially available, including hydroxycobalamin, methylcobalamin and adenosylcobalamin[67]. Hydroxycobalamin is commonly used in Europe at intervals of approximately 2-3 mo, as it appears to have better retention than cyanocobalamin[5]. Oral and intramuscular routes of vitamin B12 administration are frequently used for treatment of vitamin B12 deficiency. The efficacy of alternative routes of vitamin B12 administration (e.g., intranasal or sublingual administration) to treat vitamin B12 deficiency has also been reported[68,69]. Indeed, a recent 12-wk randomized intervention trial showed that sublingual administration of 50 μg/d cyanocobalamin restored adequate serum concentrations of vitamin B12 in vegans and vegetarians with a marginal cobalamin deficiency[69]. After intramuscular injection of cyanocobalamin, about 10%-15% of the total administered dose (e.g., 150 μg of 1000 μg) is ultimately retained in the body, primarily through storage in the liver, although a remarkable interindividual variability in vitamin B12 retention capacity has been reported[5,8]. Therefore, intramuscular injection of vitamin B12 in high doses allows for rapid replenishment of body stores of the vitamin. High-dose oral vitamin B12 supplementation is an effective alternative to parenteral treatment (e.g., in patients who do not tolerate intramuscular injections). Approximately 0.5%-4% of an oral vitamin B12 dose is usually absorbed[5]; for example, an oral dose of 1000 μg will deliver on average 5-40 μg of vitamin B12[5], which adequately meet the recommended daily intake of vitamin B12.
However, route of administration and duration of treatment primarily depend on the underlying etiology and severity of vitamin B12 deficiency. In subjects with vitamin B12 deficiency caused by malabsorption rather than by inadequate dietary intake, high-dose vitamin B12 administration should be initiated as follows: (1) Intramuscular injection of 1000 μg of cyanocobalamin or hydroxycobalamin daily or every other day for 1 wk, followed by weekly injections up to 8 wk, and every 3-4 wk afterward; or (2) Oral administration of cyanocobalamin in high daily doses (2000 μg/d) until remission, and 1000-2000 μg daily afterward[5]. Conversely, patients who are vitamin B12 deficient because of low dietary intake will require loading with high-dose vitamin B12 to restore tissue levels over 3-4 mo; subsequently, smaller doses of at least 6 μg/d will generally suffice, as conservation of biliary vitamin B12 is possible via the enterohepatic recycling and the physiologically highly efficient reabsorption of biliary vitamin B12[5]. Patients lacking IF (e.g., those with true pernicious anemia) cannot reabsorb the vitamin B12 lost in bile (which varies from 3 μg/d to 9 μg/d), and 100-300 μg of vitamin B12 should therefore be retained monthly to maintain tissue stores[5]. In this regard, it is worth mentioning that about 1% of oral vitamin B12 can be absorbed in the small intestine through a passive diffusion pathway that is independent of IF and remains unaffected in patients with pernicious anemia[70]. Thus, high oral doses of 1000-2000 μg/d vitamin B12 can meet the estimated daily requirement of 2.4 μg/d even in patients with impaired IF secretion. Notwithstanding, there are arguments against the use of oral vitamin B12 in severely deficient individuals with poor intestinal absorption (particularly in those with pernicious anemia), in whom intramuscular injection may be preferred to assure effective treatment[62]. Furthermore, patients with vitamin B12 deficiency presenting with severe neurologic manifestations should be treated by intramuscular injection of 1000 μg of vitamin B12 on alternate days until no further improvement is noted[62]. With regard to the duration of vitamin B12 supplementation, patients with an irreversible cause of vitamin B12 deficiency should be treated indefinitely, and those with a reversible cause should be treated until the deficiency is corrected and the symptoms resolve[8,71]. In the presence of concomitant folate deficiency, vitamin B12 deficiency should be corrected first to prevent subacute combined degeneration of the spinal cord[8,71].
Treatment of metformin-induced vitamin B12 deficiency
According to the British Society for Haematology guidelines for diagnosis and treatment of vitamin B12 deficiency, no recommendations can be currently given on prophylactic administration with oral vitamin B12 in patients using metformin[62]. Despite the lack of definitive guidelines or recommendations on treatment of metformin-induced vitamin B12 deficiency, patients using metformin with concomitant vitamin B12 deficiency should receive cobalamin supplementation aimed to correct this deficiency and prevent the related risk of peripheral nerve damage and/or other clinical consequences. Importantly, prompt vitamin B12 administration should be considered, particularly in metformin-treated patients with vitamin B12 deficiency accompanied by neurologic and/or hematologic manifestations such as peripheral neuropathy and megaloblastic anemia.
Although treatment of vitamin B12 deficiency in metformin-treated patients may certainly be cost-effective, an issue that still needs to be addressed relies on the fact that the most appropriate repletion method has not yet been clearly defined. As metformin appears to interfere with vitamin B12 absorption in the small intestine through different mechanisms, intramuscular or sublingual routes of administration may theoretically be superior to oral supplementation for treatment of metformin-induced vitamin B12 through bypassing the gastrointestinal tract and intestinal absorption. However, it is also plausible that high-dose oral vitamin B12 supplementation may be as effective as other routes of administration in overcoming the malabsorption caused by metformin and adequately correcting the cobalamin deficiency. Future studies are therefore warranted to establish the most effective and convenient route of administration of vitamin B12 in metformin-treated patients with concomitant vitamin B12 deficiency. As oral calcium supplementation has been shown to reverse vitamin B12 malabsorption caused by metformin[61], it would also be interesting to investigate whether this therapeutic approach may represent an alternative, safe and effective tool to treat metformin-induced vitamin B12 deficiency.
CONCLUSION
Several recent observational studies and meta-analyses have reported a significant association between long-term metformin therapy and an increased prevalence of vitamin B12 deficiency. The exact mechanisms accounting for vitamin B12 deficiency caused by metformin are still not entirely clear, although it is highly plausible that such mechanisms are related to the impaired vitamin B12 absorption in the small intestine.
Given the high global prevalence of diabetes, which affects more than 460 million people worldwide[72], the widespread use of metformin as an insulin-sensitizing agent for treatment of insulin resistance, prediabetes, T2D and PCOS, as well as the chronic nature of treatment of such conditions, it is important to recognize vitamin B12 deficiency as a potential adverse consequence of long-term and high-dose metformin therapy. As no definite guidelines are currently available for vitamin B12 deficiency screening in metformin-treated patients, this deficiency remains often unrecognized in such individuals.
Therefore, we believe that initial screening and subsequent intermittent periodic testing of vitamin B12 status in selected patients treated with metformin may be cost-effective and should be considered in order to promptly identify and correct vitamin B12 deficiency. In this regard, we have proposed a list of criteria for a cost-effective screening and subsequent intermittent periodic testing of vitamin B12 status in metformin-treated patients who are at high risk for deficiency (Table 2). The criteria include: (1) Strong clinical suspicion of vitamin B12 deficiency; (2) Preexisting diabetic peripheral and/or autonomic neuropathy; (3) Duration of metformin therapy of ≥ 5 years; (4) Age ≥ 65 years; (5) High cumulative metformin exposure defined by a MUI value of > 5; (6) A metformin dose of ≥ 1500 mg/d for a duration of at least 6 mo; (7) Concomitant long-term use (≥ 12 mo) of acid-suppressing medications; and (8) Concomitant presence of risk factors or comorbidities associated with an increased risk of vitamin B12 deficiency (reviewed in Table 1). Yet, we acknowledge that these criteria need to be validated in large prospective studies. Further studies are also needed to ascertain the desirable frequency of assessment of vitamin B12 status in patients receiving metformin therapy. Thus, additional research is required to develop protocols for screening, prevention and treatment of metformin-induced vitamin B12.
In patients with metformin-induced vitamin B12 deficiency, vitamin B12 supplementation offers a simple, safe and effective means of preventing the development or the worsening of peripheral nerve damage, anemia and/or other clinical manifestations of vitamin B12 deficiency. To date, there are no specific guidelines for the treatment of vitamin B12 deficiency induced by metformin therapy. Hence, clinicians should correct vitamin B12 deficiency in patients treated with metformin following the British Society for Haematology guidelines for diagnosis and treatment of vitamin B12 deficiency[62]. Likewise, these remarks apply to metformin-treated diabetic patients with preexisting diabetic peripheral and/or autonomic neuropathy who may experience an exacerbation of nerve damage as well as a substantial deterioration of neuropathy resulting from the concomitant development of MICD. In light of the highly favorable safety and efficacy profile of metformin as an insulin-sensitizing agent, we certainly recommend against discontinuing this drug in patients with newly diagnosed vitamin B12 deficiency. However, it is prudent to periodically assess vitamin B12 status in metformin-treated patients who could remain at increased risk of vitamin B12 deficiency even after an adequate vitamin B12 supplementation.
ACKNOWLEDGEMENTS
Figure 1 was created with images adapted from Servier Medical Art licensed under a Creative Commons Attribution 3.0 (https://smart.servier.com/).
Footnotes
Conflict-of-interest statement: The authors declare that they have no competing interests.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: American Diabetes Association, No. 548470061.
Peer-review started: January 29, 2021
First decision: March 16, 2021
Article in press: April 29, 2021
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wu WJ, Xu J S-Editor: Gao CC L-Editor: Filipodia P-Editor: Ma YJ
Contributor Information
Marco Infante, UniCamillus, Saint Camillus International University of Health Sciences, Rome 00131, Italy; Diabetes Research Institute Federation (DRIF), Division of Endocrinology and Diabetes, CTO Alesini Hospital, Department of Systems Medicine, University of Rome Tor Vergata, Rome 00145, Italy; Network of Immunity in Infection, Malignancy and Autoimmunity (NIIMA), Universal Scientific Education and Research Network (USERN), Rome 00145, Italy. marco.infante@unicamillus.org.
Martina Leoni, Diabetes Research Institute Federation (DRIF), Division of Endocrinology and Diabetes, CTO Alesini Hospital, Department of Systems Medicine, University of Rome Tor Vergata, Rome 00145, Italy.
Massimiliano Caprio, Department of Human Sciences and Promotion of the Quality of Life, San Raffaele Roma Open University, Rome 00166, Italy; Laboratory of Cardiovascular Endocrinology, IRCCS San Raffaele Pisana, Rome 00166, Italy.
Andrea Fabbri, Diabetes Research Institute Federation (DRIF), Division of Endocrinology and Diabetes, CTO Alesini Hospital, Department of Systems Medicine, University of Rome Tor Vergata, Rome 00145, Italy.
References
- 1.Obeid R, Heil SG, Verhoeven MMA, van den Heuvel EGHM, de Groot LCPGM, Eussen SJPM. Vitamin B12 Intake From Animal Foods, Biomarkers, and Health Aspects. Front Nutr. 2019;6:93. doi: 10.3389/fnut.2019.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beedholm-Ebsen R, van de Wetering K, Hardlei T, Nexø E, Borst P, Moestrup SK. Identification of multidrug resistance protein 1 (MRP1/ABCC1) as a molecular gate for cellular export of cobalamin. Blood. 2010;115:1632–1639. doi: 10.1182/blood-2009-07-232587. [DOI] [PubMed] [Google Scholar]
- 3.Seetharam B, Li N. Transcobalamin II and its cell surface receptor. Vitam Horm. 2000;59:337–366. doi: 10.1016/s0083-6729(00)59012-8. [DOI] [PubMed] [Google Scholar]
- 4.Ankar A, Kumar A. Vitamin B12 Deficiency. 2020 Jun 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 . [Google Scholar]
- 5.Green R, Allen LH, Bjørke-Monsen AL, Brito A, Guéant JL, Miller JW, Molloy AM, Nexo E, Stabler S, Toh BH, Ueland PM, Yajnik C. Vitamin B12 deficiency. Nat Rev Dis Primers. 2017;3:17040. doi: 10.1038/nrdp.2017.40. [DOI] [PubMed] [Google Scholar]
- 6.Konda M, Godbole A, Pandey S, Sasapu A. Vitamin B12 deficiency mimicking acute leukemia. Proc (Bayl Univ Med Cent) 2019;32:589–592. doi: 10.1080/08998280.2019.1641045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar N. Neurologic aspects of cobalamin (B12) deficiency. Handb Clin Neurol. 2014;120:915–926. doi: 10.1016/B978-0-7020-4087-0.00060-7. [DOI] [PubMed] [Google Scholar]
- 8.Langan RC, Goodbred AJ. Vitamin B12 Deficiency: Recognition and Management. Am Fam Physician. 2017;96:384–389. [PubMed] [Google Scholar]
- 9.Kibirige D, Mwebaze R. Vitamin B12 deficiency among patients with diabetes mellitus: is routine screening and supplementation justified? J Diabetes Metab Disord. 2013;12:17. doi: 10.1186/2251-6581-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bell DS. Metformin-induced vitamin B12 deficiency presenting as a peripheral neuropathy. South Med J. 2010;103:265–267. doi: 10.1097/SMJ.0b013e3181ce0e4d. [DOI] [PubMed] [Google Scholar]
- 11.Köbe T, Witte AV, Schnelle A, Grittner U, Tesky VA, Pantel J, Schuchardt JP, Hahn A, Bohlken J, Rujescu D, Flöel A. Vitamin B-12 concentration, memory performance, and hippocampal structure in patients with mild cognitive impairment. Am J Clin Nutr. 2016;103:1045–1054. doi: 10.3945/ajcn.115.116970. [DOI] [PubMed] [Google Scholar]
- 12.Hannibal L, Lysne V, Bjørke-Monsen AL, Behringer S, Grünert SC, Spiekerkoetter U, Jacobsen DW, Blom HJ. Biomarkers and Algorithms for the Diagnosis of Vitamin B12 Deficiency. Front Mol Biosci. 2016;3:27. doi: 10.3389/fmolb.2016.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yetley EA, Pfeiffer CM, Phinney KW, Bailey RL, Blackmore S, Bock JL, Brody LC, Carmel R, Curtin LR, Durazo-Arvizu RA, Eckfeldt JH, Green R, Gregory JF 3rd, Hoofnagle AN, Jacobsen DW, Jacques PF, Lacher DA, Molloy AM, Massaro J, Mills JL, Nexo E, Rader JI, Selhub J, Sempos C, Shane B, Stabler S, Stover P, Tamura T, Tedstone A, Thorpe SJ, Coates PM, Johnson CL, Picciano MF. Biomarkers of vitamin B-12 status in NHANES: a roundtable summary. Am J Clin Nutr. 2011;94:313S–321S. doi: 10.3945/ajcn.111.013243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solomon LR. Cobalamin-responsive disorders in the ambulatory care setting: unreliability of cobalamin, methylmalonic acid, and homocysteine testing. Blood. 2005;105:978–85; author reply 1137. doi: 10.1182/blood-2004-04-1641. [DOI] [PubMed] [Google Scholar]
- 15.Other B Vitamins, and Choline. Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes and its Panel on Folate. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B 6, Folate, Vitamin B 12, Pantothenic Acid, Biotin, and Choline. 1998. [PubMed] [Google Scholar]
- 16.Lupoli R, Lembo E, Saldalamacchia G, Avola CK, Angrisani L, Capaldo B. Bariatric surgery and long-term nutritional issues. World J Diabetes. 2017;8:464–474. doi: 10.4239/wjd.v8.i11.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pennypacker LC, Allen RH, Kelly JP, Matthews LM, Grigsby J, Kaye K, Lindenbaum J, Stabler SP. High prevalence of cobalamin deficiency in elderly outpatients. J Am Geriatr Soc. 1992;40:1197–1204. [PubMed] [Google Scholar]
- 18.Baik HW, Russell RM. Vitamin B12 deficiency in the elderly. Annu Rev Nutr. 1999;19:357–377. doi: 10.1146/annurev.nutr.19.1.357. [DOI] [PubMed] [Google Scholar]
- 19.Johnson MA, Hausman DB, Davey A, Poon LW, Allen RH, Stabler SP Georgia Centenarian Study. Vitamin B12 deficiency in African American and white octogenarians and centenarians in Georgia. J Nutr Health Aging. 2010;14:339–345. doi: 10.1007/s12603-010-0077-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murphy MM, Molloy AM, Ueland PM, Fernandez-Ballart JD, Schneede J, Arija V, Scott JM. Longitudinal study of the effect of pregnancy on maternal and fetal cobalamin status in healthy women and their offspring. J Nutr. 2007;137:1863–1867. doi: 10.1093/jn/137.8.1863. [DOI] [PubMed] [Google Scholar]
- 21.Milman N, Byg KE, Bergholt T, Eriksen L, Hvas AM. Cobalamin status during normal pregnancy and postpartum: a longitudinal study comprising 406 Danish women. Eur J Haematol. 2006;76:521–525. doi: 10.1111/j.0902-4441.2006.t01-1-EJH2550.x. [DOI] [PubMed] [Google Scholar]
- 22.Greibe E, Andreasen BH, Lildballe DL, Morkbak AL, Hvas AM, Nexo E. Uptake of cobalamin and markers of cobalamin status: a longitudinal study of healthy pregnant women. Clin Chem Lab Med. 2011;49:1877–1882. doi: 10.1515/CCLM.2011.682. [DOI] [PubMed] [Google Scholar]
- 23.Carmel R, Green R, Jacobsen DW, Rasmussen K, Florea M, Azen C. Serum cobalamin, homocysteine, and methylmalonic acid concentrations in a multiethnic elderly population: ethnic and sex differences in cobalamin and metabolite abnormalities. Am J Clin Nutr. 1999;70:904–910. doi: 10.1093/ajcn/70.5.904. [DOI] [PubMed] [Google Scholar]
- 24.Devi A, Rush E, Harper M, Venn B. Vitamin B12 Status of Various Ethnic Groups Living in New Zealand: An Analysis of the Adult Nutrition Survey 2008/2009. Nutrients. 2018;10 doi: 10.3390/nu10020181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta AK, Damji A, Uppaluri A. Vitamin B12 deficiency. Prevalence among South Asians at a Toronto clinic. Can Fam Physician. 2004;50:743–747. [PMC free article] [PubMed] [Google Scholar]
- 26.Marshall SM. 60 years of metformin use: a glance at the past and a look to the future. Diabetologia. 2017;60:1561–1565. doi: 10.1007/s00125-017-4343-y. [DOI] [PubMed] [Google Scholar]
- 27.Bonnet F, Scheen A. Understanding and overcoming metformin gastrointestinal intolerance. Diabetes Obes Metab. 2017;19:473–481. doi: 10.1111/dom.12854. [DOI] [PubMed] [Google Scholar]
- 28.DeFronzo R, Fleming GA, Chen K, Bicsak TA. Metformin-associated lactic acidosis: Current perspectives on causes and risk. Metabolism. 2016;65:20–29. doi: 10.1016/j.metabol.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 29.Ito H, Ishida H, Takeuchi Y, Antoku S, Abe M, Mifune M, Togane M. Long-term effect of metformin on blood glucose control in non-obese patients with type 2 diabetes mellitus. Nutr Metab (Lond) 2010;7:83. doi: 10.1186/1743-7075-7-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Viollet B, Guigas B, Sanz Garcia N, Leclerc J, Foretz M, Andreelli F. Cellular and molecular mechanisms of metformin: an overview. Clin Sci (Lond) 2012;122:253–270. doi: 10.1042/CS20110386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chapman LE, Darling AL, Brown JE. Association between metformin and vitamin B12 deficiency in patients with type 2 diabetes: A systematic review and meta-analysis. Diabetes Metab. 2016;42:316–327. doi: 10.1016/j.diabet.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 32.Aroda VR, Edelstein SL, Goldberg RB, Knowler WC, Marcovina SM, Orchard TJ, Bray GA, Schade DS, Temprosa MG, White NH, Crandall JP Diabetes Prevention Program Research Group. Long-term Metformin Use and Vitamin B12 Deficiency in the Diabetes Prevention Program Outcomes Study. J Clin Endocrinol Metab. 2016;101:1754–1761. doi: 10.1210/jc.2015-3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim J, Ahn CW, Fang S, Lee HS, Park JS. Association between metformin dose and vitamin B12 deficiency in patients with type 2 diabetes. Medicine (Baltimore) 2019;98:e17918. doi: 10.1097/MD.0000000000017918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kancherla V, Elliott JL Jr, Patel BB, Holland NW, Johnson TM 2nd, Khakharia A, Phillips LS, Oakley GP Jr, Vaughan CP. Long-term Metformin Therapy and Monitoring for Vitamin B12 Deficiency Among Older Veterans. J Am Geriatr Soc. 2017;65:1061–1066. doi: 10.1111/jgs.14761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Niafar M, Hai F, Porhomayon J, Nader ND. The role of metformin on vitamin B12 deficiency: a meta-analysis review. Intern Emerg Med. 2015;10:93–102. doi: 10.1007/s11739-014-1157-5. [DOI] [PubMed] [Google Scholar]
- 36.Liu Q, Li S, Quan H, Li J. Vitamin B12 status in metformin treated patients: systematic review. PLoS One. 2014;9:e100379. doi: 10.1371/journal.pone.0100379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mazokopakis EE, Starakis IK. Recommendations for diagnosis and management of metformin-induced vitamin B12 (Cbl) deficiency. Diabetes Res Clin Pract. 2012;97:359–367. doi: 10.1016/j.diabres.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 38.de Groot-Kamphuis DM, van Dijk PR, Groenier KH, Houweling ST, Bilo HJ, Kleefstra N. Vitamin B12 deficiency and the lack of its consequences in type 2 diabetes patients using metformin. Neth J Med. 2013;71:386–390. [PubMed] [Google Scholar]
- 39.Beulens JW, Hart HE, Kuijs R, Kooijman-Buiting AM, Rutten GE. Influence of duration and dose of metformin on cobalamin deficiency in type 2 diabetes patients using metformin. Acta Diabetol. 2015;52:47–53. doi: 10.1007/s00592-014-0597-8. [DOI] [PubMed] [Google Scholar]
- 40.Pflipsen MC, Oh RC, Saguil A, Seehusen DA, Seaquist D, Topolski R. The prevalence of vitamin B(12) deficiency in patients with type 2 diabetes: a cross-sectional study. J Am Board Fam Med. 2009;22:528–534. doi: 10.3122/jabfm.2009.05.090044. [DOI] [PubMed] [Google Scholar]
- 41.Rodríguez-Gutiérrez R, Montes-Villarreal J, Rodríguez-Velver KV, González-Velázquez C, Salcido-Montenegro A, Elizondo-Plazas A, González-González JG. Metformin Use and Vitamin B12 Deficiency: Untangling the Association. Am J Med Sci. 2017;354:165–171. doi: 10.1016/j.amjms.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 42.Berchtold P, Bolli P, Arbenz U, Keiser G. [Disturbance of intestinal absorption following metformin therapy (observations on the mode of action of biguanides] Diabetologia. 1969;5:405–412. doi: 10.1007/BF00427979. [DOI] [PubMed] [Google Scholar]
- 43.Tomkin GH, Hadden DR, Weaver JA, Montgomery DA. Vitamin-B12 status of patients on long-term metformin therapy. Br Med J. 1971;2:685–687. doi: 10.1136/bmj.2.5763.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ting RZ, Szeto CC, Chan MH, Ma KK, Chow KM. Risk factors of vitamin B(12) deficiency in patients receiving metformin. Arch Intern Med. 2006;166:1975–1979. doi: 10.1001/archinte.166.18.1975. [DOI] [PubMed] [Google Scholar]
- 45.Shivaprasad C, Gautham K, Ramdas B, Gopaldatta KS, Nishchitha K. Metformin Usage Index and assessment of vitamin B12 deficiency among metformin and non-metformin users with type 2 diabetes mellitus. Acta Diabetol. 2020;57:1073–1080. doi: 10.1007/s00592-020-01526-4. [DOI] [PubMed] [Google Scholar]
- 46.American Diabetes Association. 3. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44:S34–S39. doi: 10.2337/dc21-S003. [DOI] [PubMed] [Google Scholar]
- 47.Martin D, Thaker J, Shreve M, Lamerato L, Budzynska K. Assessment of vitamin B12 deficiency and B12 screening trends for patients on metformin: a retrospective cohort case review. BMJ Nutr Prevent Health. 2021 doi: 10.1136/bmjnph-2020-000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wile DJ, Toth C. Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care. 2010;33:156–161. doi: 10.2337/dc09-0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Out M, Kooy A, Lehert P, Schalkwijk CA, Stehouwer CDA. Long-term treatment with metformin in type 2 diabetes and methylmalonic acid: Post hoc analysis of a randomized controlled 4.3year trial. J Diabetes Complications. 2018;32:171–178. doi: 10.1016/j.jdiacomp.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 50.Carmel R. Current concepts in cobalamin deficiency. Annu Rev Med. 2000;51:357–375. doi: 10.1146/annurev.med.51.1.357. [DOI] [PubMed] [Google Scholar]
- 51.Stover PJ. Vitamin B12 and older adults. Curr Opin Clin Nutr Metab Care. 2010;13:24–27. doi: 10.1097/MCO.0b013e328333d157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Leung S, Mattman A, Snyder F, Kassam R, Meneilly G, Nexo E. Metformin induces reductions in plasma cobalamin and haptocorrin bound cobalamin levels in elderly diabetic patients. Clin Biochem. 2010;43:759–760. doi: 10.1016/j.clinbiochem.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 53.Wakeman M, Archer DT. Metformin and Micronutrient Status in Type 2 Diabetes: Does Polypharmacy Involving Acid-Suppressing Medications Affect Vitamin B12 Levels? Diabetes Metab Syndr Obes. 2020;13:2093–2108. doi: 10.2147/DMSO.S237454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Long AN, Atwell CL, Yoo W, Solomon SS. Vitamin B(12) deficiency associated with concomitant metformin and proton pump inhibitor use. Diabetes Care. 2012;35:e84. doi: 10.2337/dc12-0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hashem MM, Esmael A, Nassar AK, El-Sherif M. The relationship between exacerbated diabetic peripheral neuropathy and metformin treatment in type 2 diabetes mellitus. Sci Rep. 2021;11:1940. doi: 10.1038/s41598-021-81631-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Didangelos T, Karlafti E, Kotzakioulafi E, Margariti E, Giannoulaki P, Batanis G, Tesfaye S, Kantartzis K. Vitamin B12 Supplementation in Diabetic Neuropathy: A 1-Year, Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients. 2021;13 doi: 10.3390/nu13020395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Greibe E, Miller JW, Foutouhi SH, Green R, Nexo E. Metformin increases liver accumulation of vitamin B12 - an experimental study in rats. Biochimie. 2013;95:1062–1065. doi: 10.1016/j.biochi.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 58.Adams JF, Clark JS, Ireland JT, Kesson CM, Watson WS. Malabsorption of vitamin B12 and intrinsic factor secretion during biguanide therapy. Diabetologia. 1983;24:16–18. doi: 10.1007/BF00275941. [DOI] [PubMed] [Google Scholar]
- 59.Caspary WF, Zavada I, Reimold W, Deuticke U, Emrich D, Willms B. Alteration of bile acid metabolism and vitamin-B12-absorption in diabetics on biguanides. Diabetologia. 1977;13:187–193. doi: 10.1007/BF01219698. [DOI] [PubMed] [Google Scholar]
- 60.Andrès E, Noel E, Goichot B. Metformin-associated vitamin B12 deficiency. Arch Intern Med. 2002;162:2251–2252. doi: 10.1001/archinte.162.19.2251-a. [DOI] [PubMed] [Google Scholar]
- 61.Bauman WA, Shaw S, Jayatilleke E, Spungen AM, Herbert V. Increased intake of calcium reverses vitamin B12 malabsorption induced by metformin. Diabetes Care. 2000;23:1227–1231. doi: 10.2337/diacare.23.9.1227. [DOI] [PubMed] [Google Scholar]
- 62.Devalia V, Hamilton MS, Molloy AM British Committee for Standards in Haematology. Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol. 2014;166:496–513. doi: 10.1111/bjh.12959. [DOI] [PubMed] [Google Scholar]
- 63.Nederstigt C, Uitbeijerse BS, Janssen LGM, Corssmit EPM, de Koning EJP, Dekkers OM. Associated auto-immune disease in type 1 diabetes patients: a systematic review and meta-analysis. Eur J Endocrinol. 2019;180:135–144. doi: 10.1530/EJE-18-0515. [DOI] [PubMed] [Google Scholar]
- 64.Perros P, Singh RK, Ludlam CA, Frier BM. Prevalence of pernicious anaemia in patients with Type 1 diabetes mellitus and autoimmune thyroid disease. Diabet Med. 2000;17:749–751. doi: 10.1046/j.1464-5491.2000.00373.x. [DOI] [PubMed] [Google Scholar]
- 65.Bor MV, von Castel-Roberts KM, Kauwell GP, Stabler SP, Allen RH, Maneval DR, Bailey LB, Nexo E. Daily intake of 4 to 7 microg dietary vitamin B-12 is associated with steady concentrations of vitamin B-12-related biomarkers in a healthy young population. Am J Clin Nutr. 2010;91:571–577. doi: 10.3945/ajcn.2009.28082. [DOI] [PubMed] [Google Scholar]
- 66.Tucker KL, Rich S, Rosenberg I, Jacques P, Dallal G, Wilson PW, Selhub J. Plasma vitamin B-12 concentrations relate to intake source in the Framingham Offspring study. Am J Clin Nutr. 2000;71:514–522. doi: 10.1093/ajcn/71.2.514. [DOI] [PubMed] [Google Scholar]
- 67.Paul C, Brady DM. Comparative Bioavailability and Utilization of Particular Forms of B12 Supplements With Potential to Mitigate B12-related Genetic Polymorphisms. Integr Med (Encinitas) 2017;16:42–49. [PMC free article] [PubMed] [Google Scholar]
- 68.Estourgie-van Burk GF, van der Kuy PHM, de Meij TG, Benninga MA, Kneepkens CMF. Intranasal treatment of vitamin B12 deficiency in children. Eur J Pediatr. 2020;179:349–352. doi: 10.1007/s00431-019-03519-0. [DOI] [PubMed] [Google Scholar]
- 69.Del Bo' C, Riso P, Gardana C, Brusamolino A, Battezzati A, Ciappellano S. Effect of two different sublingual dosages of vitamin B12 on cobalamin nutritional status in vegans and vegetarians with a marginal deficiency: A randomized controlled trial. Clin Nutr. 2019;38:575–583. doi: 10.1016/j.clnu.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 70.Berlin H, Berlin R, Brante G. Oral treatment of pernicious anemia with high doses of vitamin B12 without intrinsic factor. Acta Med Scand. 1968;184:247–258. doi: 10.1111/j.0954-6820.1968.tb02452.x. [DOI] [PubMed] [Google Scholar]
- 71.Hunt A, Harrington D, Robinson S. Vitamin B12 deficiency. BMJ. 2014;349:g5226. doi: 10.1136/bmj.g5226. [DOI] [PubMed] [Google Scholar]
- 72.Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi: 10.1016/j.diabres.2019.107843. [DOI] [PubMed] [Google Scholar]