Abstract
Eagle syndrome is a rare aggregate of symptoms caused by an elongated styloid process. We present the unique case of bilateral vascular Eagle syndrome in a patient who experienced a unilateral acute swelling due to bleeding at the level of the right internal carotid artery. This complication has never been described before. (Level of Difficulty: Advanced.)
Key Words: carotid bleeding, cervical hematoma, eagle syndrome, elongated styloid process, internal carotid artery
Abbreviations and Acronyms: CT, computed tomography
Graphical abstract
Eagle syndrome is a rare aggregate of symptoms causes by an elongated styloid process. This paper presents the unique case of bilateral vascular Eagle…
Presentation
A 64-year-old man presented to the emergency ward because of a sudden swelling in the right cervical region with hemoptysis after coughing. He had difficulty swallowing and talking was painful. A painful palpable right cervical mass was seen on clinical examination. There was no stridor or dyspnea, but his voice was hoarse. Neurological examination findings were normal.
Learning Objectives
-
•
Eagle syndrome should be considered as a differential diagnosis in carotid bleeding.
-
•
A surgical technique should be advanced to treat Eagle syndrome.
Differential diagnosis
Differentials included head and neck neoplasm, temporomandibular joint disorder, sinusitis, tonsillitis, lymphoma, esophageal diverticula, and carotid artery aneurysm.
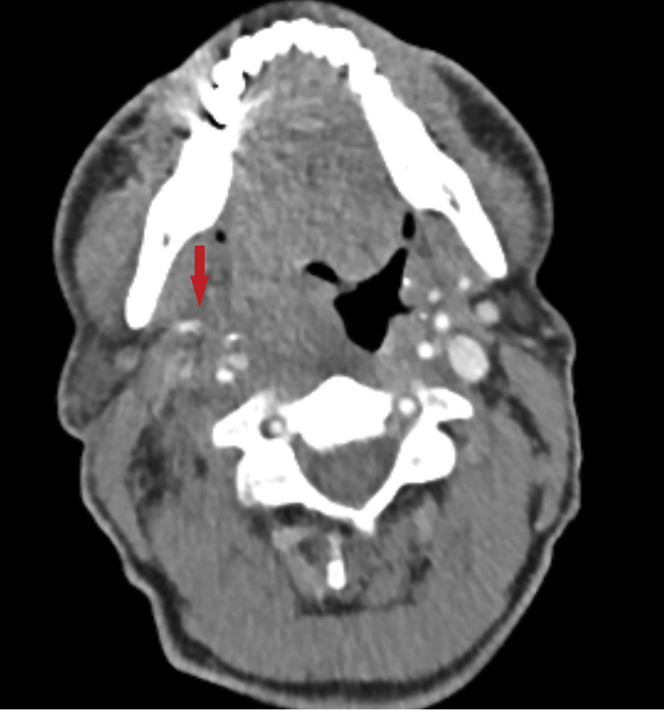
Investigations
Laboratory results were normal. Chest radiography did not show any abnormalities. Flexible laryngoscopy showed a bulging hematoma in the right lateral cervical region. A computed tomography (CT) angiography with 3-mm slices was performed in order to assess the neck and head region. It showed an arterial blush ventrally of the internal carotid artery, 3.5 cm above the carotid bifurcation on the right side without an adventitial hematoma or dissection (Figure 1).
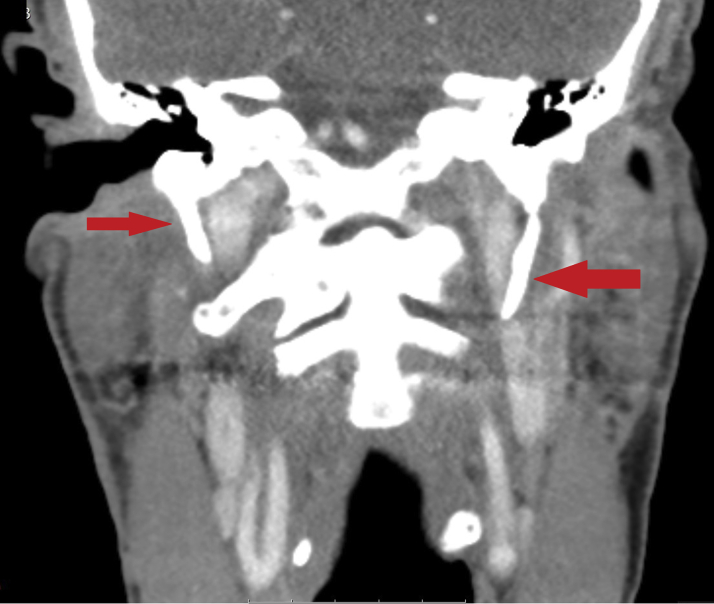
Figure 1.
Pre-Operative Computed Tomography Angiography With the Axial Plane Image of the Contrast Blush on the Right Side
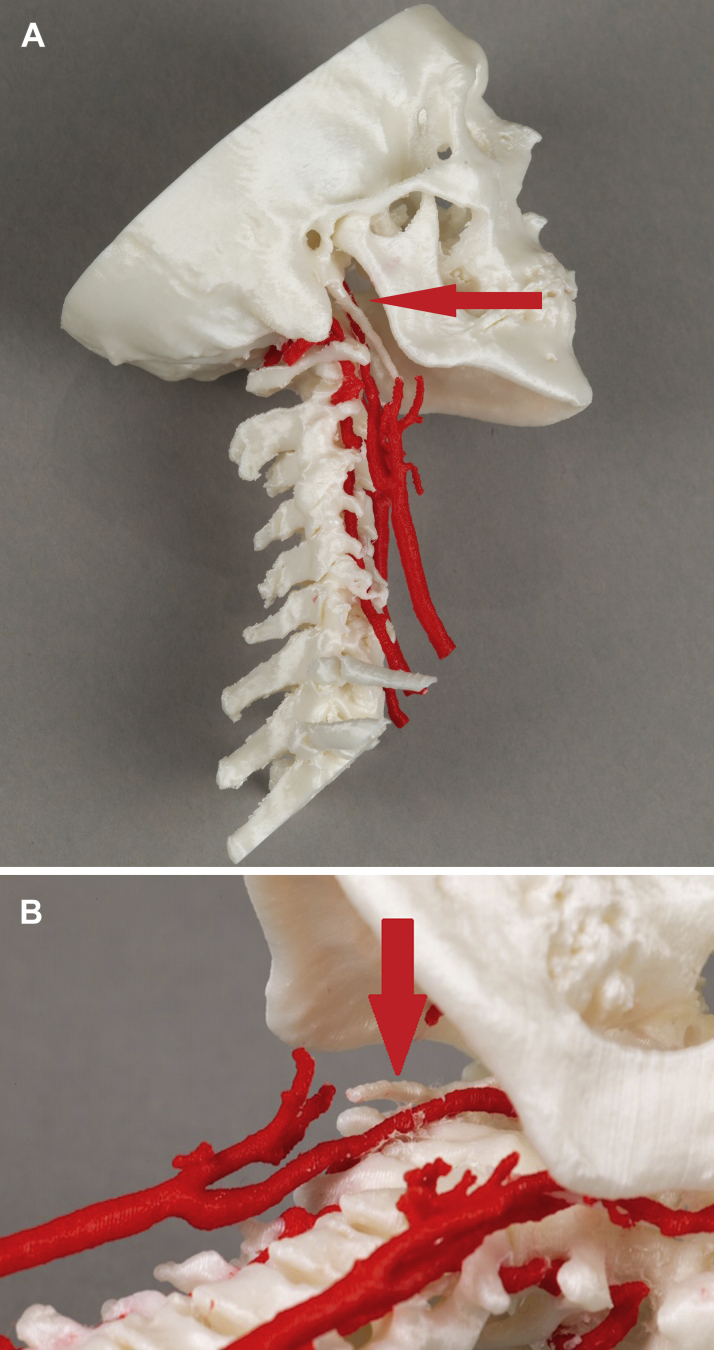
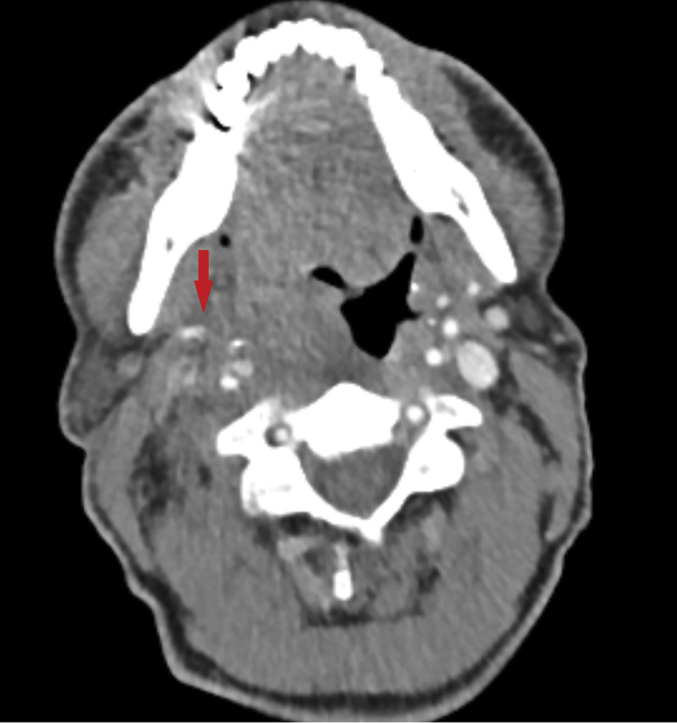
Both styloid processes were found to be longer than normal when bone structures were examined: 46 mm on the right, 50 mm on the left (Figure 2). Also, it was discovered that the right styloid process was adjacent to the internal carotid artery and caused a slight compression of the artery.
Figure 2.
Pre-Operative Computed Tomography Angiography with the Coronal Plane Image of the Bilateral Elongated Styloid Processes
CT angiography was repeated after 8 h and did not reproduce the arterial blush. The images obtained were afterwards reconstructed using a software program to make an in-house printed 3-dimensional replica of the bony and vascular structures, using the Ultimaker (Geldermalsen, the Netherlands) 3D printer (Figures 3A and 3B).
Figures 3.
In-House-Printed 3D Model of the Patient's Carotid Arteries and Bony Structures
(A) Straight lateral view from the right and (B) an oblique caudocranial view from the left. The in-house-printed 3D model of the patient's carotid arteries and bony structures allows a better understanding of the relationship between the internal carotid artery and styloid process on the right side.
Management
Over the first 12 h after admission, the patient was monitored in the intensive care unit. His respiration was stable, and intubation was not necessary because the airway was not threatened. To prevent recurrence, 3 weeks after presentation, a bilateral resection of the styloid processes through a transcervical approach was performed.
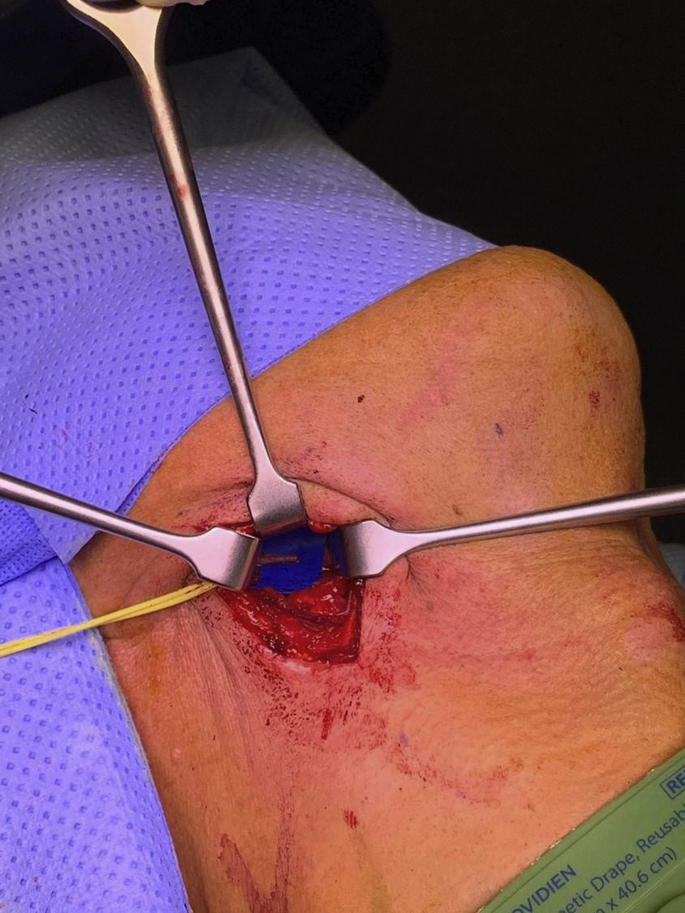
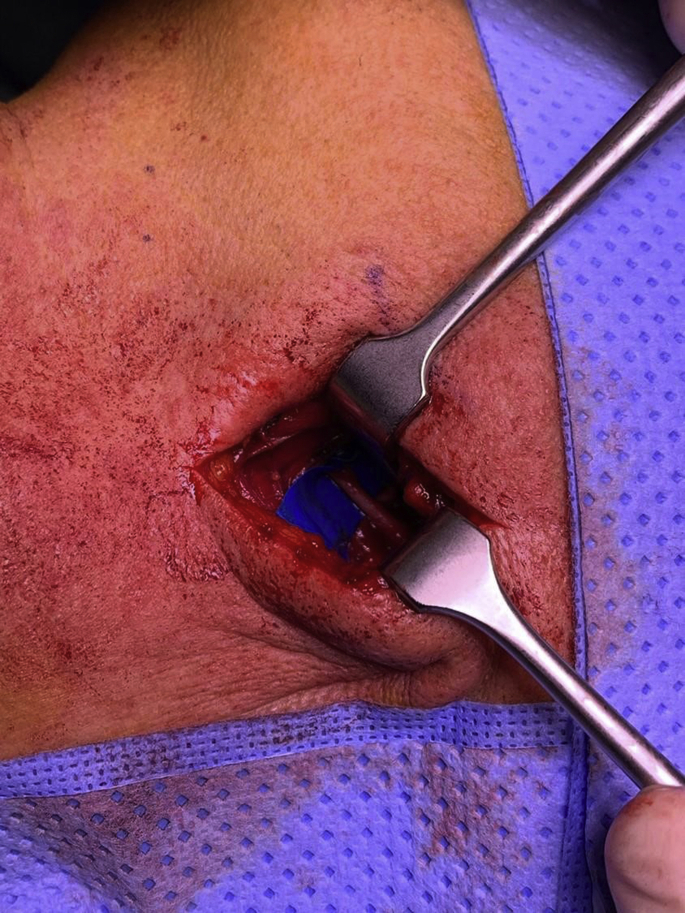
A small skin incision was made at the ventral side of the sternocleidomastoid muscle (Figure 4). The platysma muscle was incised, and the sternocleidomastoid muscle was followed until the level of the digastric muscle, which was cranially retracted to gain good exposure on the internal and external carotid artery. No bruising or other fragility was observed on the carotid arteries. Therefore, additional sutures or intraoperative angiographic images were not considered necessary. A vessel loop was placed around the external carotid artery and lifted laterally. The bony parts of the stylohyoid ligament and styloid process were identified (Figures 5 and 6) and transected as cranially as possible. The remaining proximal part was luxated laterally. The resected styloid processes are depicted in Figure 7. During the procedure, the hypoglossal and glossopharyngeal nerve were identified and spared.
Figure 4.
Incision on the Left Side of the Patient’s Mandibular Edge and Ventral Side of the Sternocleidomastoid Muscle
Full blue line shows the patient's mandibular edge. The dotted blue line shows the ventral side of the sternocleidomastoid muscle.
Figure 5.
Elongated Styloid Process on the Right Side
Figure 6.
Elongated Styloid Process on the Left Side
Figure 7.
Bilateral Resected Styloid Processes
Discussion
The first case of Eagle syndrome was described by W. Eagle in 1937. He described a pain syndrome associated with an elongated styloid process as “stylalgia.” The cartilaginous tip of the styloid process is continued over the lesser cornu of the hyoid bone as a band called the stylohyoid ligament (1). An elongated styloid process or aberrant ossified stylohyoid ligament can cause various symptoms, varying from benign to seriously damaging. In general, literature describes two forms of Eagle syndrome: the classic type with various head-and neck complaints like pain and dysphagia and the vascular type with mainly neurological symptoms (2).
The incidence of this syndrome varies between 1% and 30%, but it is highly variable because of the different thresholds of an abnormal length of the styloid process. Some suggest a length >3 cm is abnormal, but others suggest a length of more than 4 cm is abnormal because the association with symptoms is higher. Most people with an elongated styloid process are asymptomatic, and only approximately 4% are symptomatic (3).
There have been multiple causes presented to explain the finding of an elongated styloid process or ossified stylohyoid ligament, but the exact cause remains unclear. The pathophysiology is better understood: an elongated styloid process or ossified stylohyoid complex leads to compression of surrounding neurovascular structures. In classic Eagle syndrome, nerve compression can lead to craniofacial and cervical pain (2).
In vascular Eagle syndrome, stimulation of the sympathetic plexus around the cervical segment of the internal carotid artery can cause symptoms such as vertigo and syncope. As described in earlier published reports, direct compression of the extracranial internal carotid artery by the styloid process can lead to dissection causing transient ischemic attack or stroke. Also, carotid stent fracture has been reported (2,4). Carotid bleeding as a result of compression and subsequent perforation of the internal carotid artery, as in the present patient, has never been described in a published paper. It seems that, in this case, coughing was the eliciting factor: rotation and/or bending of the neck probably caused the styloid process to make contact with the internal carotid artery leading to laceration. As this is a dynamic component, it is unfortunately not reproduced on the printed 3-dimensional (3D) replicas. Hemoptysis was probably caused by perforation and bleeding of the surrounding cervical soft tissues.
CT angiography is the gold standard for diagnosis and can be aided by 3D reconstructed images (3). Management of Eagle syndrome is divided into conservative methods of medical management and definitive surgical management. Treatment strategy depends on the symptoms. In the vascular type, a surgical resection of the styloid process should be considered because of potential serious complications. A transoral or transcervical approach can be chosen (2,4).
Follow-up
The patient’s post-operative course was uneventful. The symptoms resolved, and the patient was still doing well after 5 months. Control CT angiography at that time showed resolution of the hematoma with no further abnormalities (Figure 8). The patient was discharged from further follow-up.
Figure 8.
Image in the Coronal Plane from the Post-Operative Computed Tomography Angiography With the Resected Bilateral Styloid Processes
The red arrows indicate the location of where the, now resected, styloid proccesi used to be.
Conclusions
This unique case report extends the range of possible complications of vascular Eagle syndrome. Besides carotid dissection leading to transient ischemic stroke and stroke, carotid bleeding also can result from an elongated styloid process or ossified stylohyoid complex compressing and perforating the vessel.
When there is evidence of carotid bleeding without an apparent cause, medical practitioners should be aware of vascular Eagle syndrome. Due to the potentially serious complications of this condition, surgical resection of the elongated styloid process should be considered.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, or patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Eagle W. Elongated styloid processes: Report of Two Cases. Arch Otolaryngol Head Neck Surg. 1937;25:584–587. [Google Scholar]
- 2.Badhey A., Jategaonkar A., Kovacs A., Kadakia S. Eagle syndrome: a comprehensive review. Clin Neurol Neurosurg. 2017;159:34–38. doi: 10.1016/j.clineuro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Murtagh R., Caracciolo J., Fernandez G. CT findings associated with Eagle syndrome. Am J Neuroradiol. 2001;22:1401–1402. [PMC free article] [PubMed] [Google Scholar]
- 4.Demirtaş H., Kayan M., Koyuncuoğlu H., Çelik A., Kara M., Şengeze N. Eagle syndrome causing vascular compression with cervical rotation: case report. Pol J Radiol. 2016;81:277–280. doi: 10.12659/PJR.896741. [DOI] [PMC free article] [PubMed] [Google Scholar]