Abstract
Background:
There is a lack of research regarding whether prolonged use of cocaine would lead to increase of coronary plaque burden.
Objectives:
To study the effects of cocaine use on the coronary artery plaque volume. We hypothesize the longer the cocaine use, the greater the plaque burden.
Methods:
We used coronary computed tomography angiography to evaluate plaque volumes. The study included chronic (N = 33 with 27 HIV+) and non-cocaine users (N = 15 with 12 HIV+). Chronic cocaine use was defined as use by any route for at least 6 months, administered at least 4 times/month. The Student’s t-test was used to compare the plaque volumes between chronic and non-cocaine users. Multivariable regression analysis adjusted for age, sex, body mass index, HIV status, cigarette smoking, diabetes, and total cholesterol was performed to determine the relationship between years of cocaine use and plaque volumes.
Results:
The total plaque volumes between groups showed no difference (p = 0.065). However, the total left anterior descending artery (LAD) plaque volume in the chronic cocaine group was significantly higher than that in the non-cocaine group (p = 0.047). For each year increase in cocaine use, total plaque volume and total LAD plaque volume increased by 7.23 mm3 (p = 0.013) and 4.56 mm3 (p = 0.001), respectively. In the multivariable analyses, both total plaque volume and total LAD plaque volume were significantly associated with years of cocaine use (p = 0.039 and 0.013, respectively).
Conclusion:
Prolonged cocaine use accelerates the development of sub-clinical atherosclerosis.
Keywords: Cocaine use, coronary artery plaque, HIV infection
Introduction
Cocaine is an addictive stimulant that is sourced from the Erythroxylon coca plant. It is categorized as a Schedule II drug and can be prescribing for medical purposes such as local anesthesia during surgery (1). The short-term physical effects of cocaine include sensitivity to environmental factors, increased energy, and mental alertness. The effects vary depending on the amount and route of exposure. There is a wide range of physiological effects from increased heart rate to narrowing of blood vessels. Long term use can lead to negative health consequences such as cardiovascular problems, coma, and seizures (2,3). Even though the rates of cocaine use have remained steady over the past decade, cocaine is still a widely used substance in the United States. The National Survey on Drug Use and Health found that 5.5 million people used cocaine in 2018 (4).
The effects of chronic cocaine use on the cardiovascular system have been reported in the literature (5–7). A review found that a single dose of cocaine increases a resting heart rate by 30 beats/minute and raises blood pressure by 20/10 mmHg (8). While these are not significant increases compared with gains from physical activity, cocaine has shown to decrease the diameter of coronary arteries by 5 to 30% (8). Cocaine is also involved in the process of thrombosis and can contribute to atherosclerosis (9). Acute coronary syndrome and acute myocardial infarction are two common cardiovascular issues that arise in cocaine users (6). One study showed that cocaine users had more plaques than non-cocaine users and concluded that cocaine users have greater development of coronary atherosclerosis (10).
Studies have shown that cocaine users are also at risk of acquiring human immunodeficiency virus (HIV). Behavioral factors such as sharing needles and high-risk sexual activities can lead to transmission of HIV through blood and bodily fluids. The Centers for Disease Control and Prevention reports that about 10% of new HIV diagnoses in the United States are due to these methods of transmission (11). HIV patients who are also injection drug users experience challenges with compliance to treatment. Patients tend to continue their drug use and unsafe sexual practices (12). Aside from behavioral factors, there are social barriers hindering injection drug users from seeking care. Substance use is an illegal activity and patients may encounter stigma within the health care system. Additionally, incarceration, homelessness, and access to health insurance and care are challenges for this vulnerable population (11).
While the published literature has demonstrated an association between cocaine use and cardiovascular disease, there is still a lack of research regarding to whether prolonged use of cocaine would lead to conspicuous increase of plaque burden. The present study aimed to determine the relationship between total coronary plaque volume throughout the entire coronary vasculature in relationship to years of cocaine use in asymptomatic individuals with or without HIV.
Material and Methods
Study Design and Population
The data set came from a longitudinal study examining the cardiovascular consequences of HIV infection and chronic cocaine use in a predominantly African American population in Baltimore, MD. Our study included only African Americans. The HIV-infected participants were recruited from the Johns Hopkins HIV clinic. The HIV-uninfected participants were recruited from the eastern part of Baltimore City. The baseline data collected on the participants included demographic data, medical data, use of anti-retroviral therapy (ART), substance use, treatment history, and clinical data such as coinfections and HIV viral load. Participants also provided biological specimen samples, including urine and blood, and contrast-enhanced coronary computed tomography angiography (CCTA) data (13). Chronic cocaine use was defined as administration via any route for a period of 6 months and at least 4 times/month, based on self-report and confirmed by a urine test during initial study visit.
Inclusion criteria were (1) age ≥21 years; (2) HIV-infected and HIV-uninfected. HIV infection, which was determined by ELISA and confirmed by Western blot test (all participants were tested for HIV); and (3) chronic cocaine users and non-cocaine users. Chronic cocaine use was defined as use by any route for at least 6 months, administered at least 4 times/month. Less-frequent users (fewer than 4 times/month, or <6 consecutive months) were excluded from the study (14). Non-cocaine users were defined as never using cocaine or no use in the past 5 years or longer. Cocaine users could also use other drugs such as opiates, benzodiazepines, methamphetamine, or alcohol. Exclusion criteria were (1) any evidence of clinical CAD or any history of or current symptoms or diagnoses related to cardiovascular disease; (2) history of serious physical disease or current physical disease, including chronic obstructive pulmonary disease; (3) pregnancy; (4) chronic kidney disease with an estimated glomerular filtration rate (eGFR) of <60 mL/minute per 1.73 m2; and (5) contraindication to CT scans, including a history of contrast allergy. The protocol was approved by the Committee on Human Research at the Johns Hopkins School of Medicine and written informed consent was obtained. All procedures used in this study were in accordance with institutional guidelines. Although the overall investigation is a cohort study, the data presented herein are cross-sectional (baseline) only.
Data Processing
Coronary plaque analysis was performed using the QAngioCT software (Research Edition, version 2.0.5; Medis Medical Imaging Systems, Leiden, the Netherlands). Blinding was utilized to prevent bias from the patient data. The coronary tree was automatically extracted, and each of the major vessels (i.e. the left anterior descending artery, LAD, the left circumflex artery, LCX, and the right coronary artery, RCA) was individually analyzed from the ostium to the point at which the internal vessel caliber decreased to < 2.0 mm, exclusive of focal stenosis. Segmentation was performed according to American Heart Association (AHA) nomenclature (15). Segments with image artifacts were excluded. Automated longitudinal contouring of the inner lumen and outer wall was performed, and results were manually adjusted where needed. Results of automated contouring of the inner lumen and outer wall were also reviewed on transverse reconstructed cross-sections of the artery on a section-by-section basis at 0.5-mm increments.
Statistical analysis
Statistical analysis was performed using STATA (STATACorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC). Data were stratified by cocaine use status. Statistics for all continuous variables are reported as mean ± standard deviation (sd). Categorical data were presented as frequencies and percentages and were compared by using the Chi-square test. Shapiro-Wilk test was used to test for normality of plaque volumes. In case of non-normal distribution, we evaluated the differences in plaque volume between cocaine users and non-users using the logarithmic transformation of plaque volume + 1 and compared by using the two tailed t-test for independent samples. Simple linear regression was used to examine the correlation between cocaine years use and total plaque volumes. Multivariable linear regression analyses were conducted to examine the association between plaque volumes and years of cocaine use, adjusted for age, sex, BMI, HIV status, cigarette smoking status, diabetes, and total cholesterol. Fifteen patients were randomly selected for inter-reader reproducibility. Comparison was made in three coronary artery territories. Reproducibility was calculated by using intraclass correlation coefficients for interobserver analysis. P < 0.05 was considered to indicate a statistically significant difference.
Results
Overall, 48 individuals were randomly selected and analyzed. A total of 15 were non-cocaine users, and 33 were chronic cocaine users. Thirty-nine (81%) were men and 39 (81%) were HIV positive. The total plaque volume in the chronic cocaine group was 272.0 ± 254.3 mm3 which was not statistically different from the non-cocaine group (160.5 ± 201.9 mm3, p = 0.065). However, total LAD plaque volume in the chronic cocaine group was 154.6 ± 127.7 mm3 which was statistically significant from the non-cocaine group (72.5 ± 70.0 mm3, p = 0.046). Table 1 summarizes the demographics of study participants stratified by cocaine status.
Table 1.
Demographics of study cohort.
| Non-cocaine group (n = 15) | Chronic cocaine group (n = 33) | p-value | |
|---|---|---|---|
| Sex, no. (%) | |||
| Male | 13 (87) | 26 (79) | |
| Female | 2 (13) | 7 (21) | 0.52 |
| Age (years) | 48.9 (5.4) | 48.9 (7.6) | 0.98 |
| BMI (kg/m2) | 25.7 (4.7) | 26.5 (4.1) | 0.58 |
| Cocaine years use | 0 (0) | 19.2 (9.4) | 0.00 |
| HIV positive, no. (%) | 12 (80) | 27 (82) | 0.88 |
| Cigarette smokers, no. (%) | 10 (67) | 31 (94) | 0.013 |
| Diabetes, no. (%) | 2 (13) | 6 (18) | 0.68 |
| ART, no. (%) | 11 (73) | 23 (70) | 0.80 |
| Total Cholesterol (mg/dL) | 175.5 (34.5) | 185 (58.4) | 0.56 |
| Total Plaque Volume (mm3) | 160.5 (201.9) | 272.0 (254.3) | 0.065 |
| LAD | 72.5 (70.0) | 154.6 (127.7) | 0.046 |
| LCX | 16.0 (32.7) | 47.6 (88.8) | 0.995 |
| RCA | 71.5 (119.6) | 66.0 (82.7) | 0.94 |
| Total noncalcified plaque volume (mm3) | 148.2 (180.6) | 207.6 (194.3) | 0.115 |
| Total calcified plaque volume (mm3) | 12.4 (23.3) | 64.3 (131.2) | 0.236 |
Unless otherwise specified, data are means ± standard deviations. BMI: body mass index. ART: anti-retroviral therapy. LAD: left anterior descending artery. LCX: left circumflex artery. RCA: right coronary artery.
Figure 1 demonstrates the correlation between total plaque volume (a) and total LAD plaque volume (b) and cocaine years use presented for illustrative purpose. In the univariate analysis, both total plaque volume (p = 0.013) and total LAD plaque volume (p = 0.001) were significantly associated with cocaine years use. For each year increase in cocaine use, total plaque volume and total LAD plaque volume increased by 7.23 mm3 and 4.56 mm3, respectively. When considered only the chronic cocaine users (N = 33), the unadjusted total plaque volume increase per year of cocaine use was 8.71 mm3 (p = 0.185) and 9.95 mm3 (p = 0.036) in HIV+ (N=27) and HIV− (N=6), respectively. In the multivariable analyses (Table 2), both total plaque volume and total LAD plaque volume were significantly associated with years of cocaine use (p = 0.039 and 0.013, respectively). When included only the chronic cocaine users in Table 2 analysis (N=33), the results remained the same; i.e. cocaine years use was significantly associated with the plaque volume, and HIV status was not significantly associated with the plaque volume. The Bland-Altman plot for inter-reader reproducibility is demonstrated in Figure 2. There was no statistical difference between the two readers in the plaque volume analysis (mean difference, 5.7 ± 19.61 mm3, 95% CI, 0.85–0.93, ICC=0.89).
Figure 1. The Unadjusted Relationships Between plaque volume and cocaine years use.
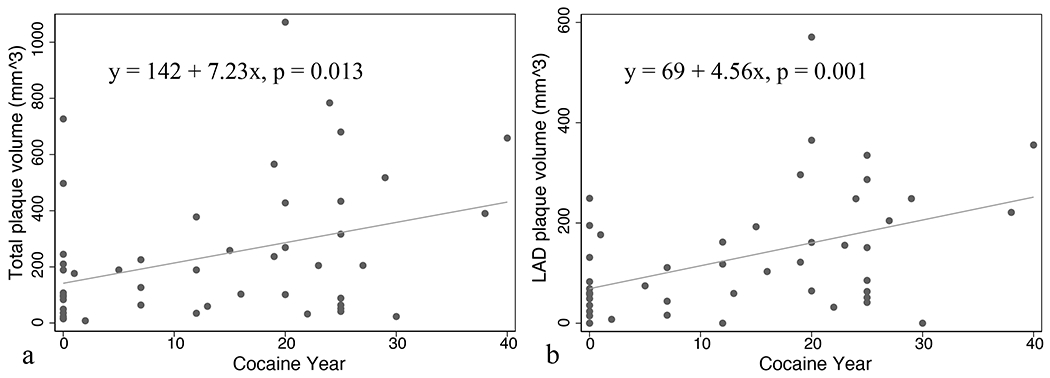
The relationships between total plaque volume (a) and left anterior descending artery (LAD) plaque volume (b) versus cocaine years use in the unadjusted data presented for illustrative purposes. For each year increase in cocaine use, total plaque volume and total LAD plaque volume increased by 7.23 mm3 and 4.56 mm3, respectively. Both associations were significant in the univariate analysis.
Table 2.
Multivariable associations between cardiovascular risk factors and total plaque volume, and LAD plaque volume (N = 48 from the entire cohort)
| Total Plaque Volume (mm3) |
LAD Plaque Volume (mm3) |
|||
|---|---|---|---|---|
| β (95% CI) | p-value | β (95% CI) | p-value | |
| Female sex | 0.145 (−0.199, 0.488) | 0.399 | −0.144 (−0.446, 0.159) | 0.341 |
| Age (years) | 0.039 (0.208, 0.058) | 0.000 | 0.030 (0.014, 0.045) | 0.000 |
| BMI (kg/m2) | 0.029 (−0.001, 0.059) | 0.056 | 0.024 (−0.001, 0.049) | 0.056 |
| Cocaine years use | 0.305 (0.017, 0.592) | 0.039 | 0.309 (0.069, 0.550) | 0.013 |
| HIV positive | −0.240 (−0.587, 0.107) | 0.169 | −0.108 (−0.395, 0.179) | 0.449 |
| Cigarette smoking | −0.164 (−0.553, 0.226) | 0.400 | −0.052 (−0.382, 0.279) | 0.753 |
| Diabetes | 0.333 (−0.014, 0.680) | 0.059 | 0.165 (−0.117, 0.446) | 0.242 |
| Total cholesterol (mg/dL) | 0.000 (−0.003, 0.002) | 0.860 | 0.003 (0.000, 0.005) | 0.070 |
BMI: body mass index. LAD: left anterior descending artery.
Figure 2. Bland-Altman plot of inter-reader reproducibility.
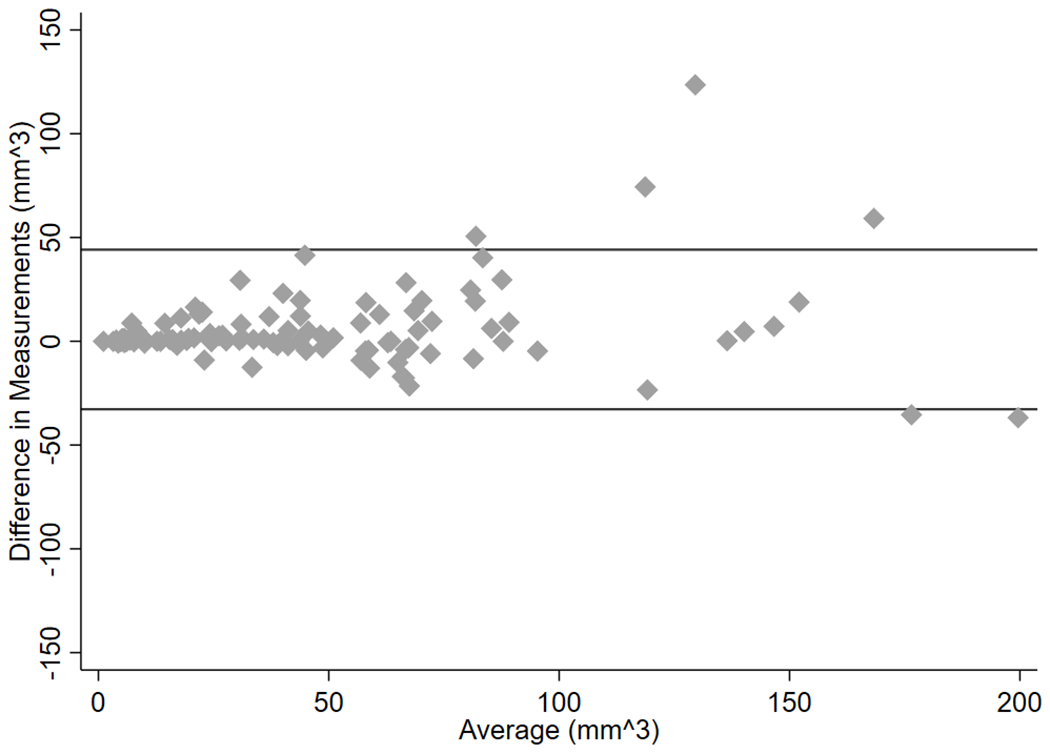
Bland-Altman plot of difference against the mean in two measurements (inter-reader reproducibility). There was no statistical difference between the two readers in the plaque volume analysis (mean difference, 5.7 ± 19.61 mm3, 95% CI, 0.85–0.93, ICC=0.89).The solid lines are the limits of agreement (mean±1.96×SD).
Discussion
The primary goal of the current study was to investigate the effects of cocaine use on the amount of coronary artery plaque volume among a cohort with or without HIV infection. The study groups between chronic cocaine users and non-cocaine users were well-characterized with similar demographics including sex, age, BMI, diabetes, and HIV status with or without ART treatment. Our findings suggest that cocaine use may increase the total plaque burden and prolonged cocaine use accelerates the development of sub-clinical atherosclerosis.
The etiology of atherosclerotic plaque is complex and is likely to be multifactorial. The long-term use of cocaine may provoke endothelial cell dysfunction and stimulate atherosclerosis (7). While direct toxic effects of cocaine on the myocardium have been recognized, findings on the association between cocaine use and sub-clinical atherosclerosis have been controversial. Several animal and autopsy studies have suggested that cocaine administration might accelerate the development of atherosclerosis (16–18). Such a relationship, nonetheless, was not observed in more recent studies based on computed tomography. In a large study which included 3038 young adults (ages 33-45 years, 35% with cocaine exposure), researchers found no evidence of a causal relationship between long-term exposure to cocaine and coronary calcification (19). Chang et al. showed no association between cocaine use and clinically significant coronary stenosis in symptomatic low- to intermediate-risk patients evaluated with CCTA(20). Ebersberger and co-workers reported comparable calcified and non-calcified plaque volume between controls and cocaine users with acute chest pain (10). Contrary to these results, a study with 224 cardiac asymptomatic participants with and without HIV found cocaine use to be independently associated with a higher number of coronary calcifications (21). Divergency of these findings could be partially attributed to the heterogeneity of the study cohorts, number of participants included, as well as the technical approaches. In our study, no significant difference was noted in total plaque volume and calcified or non-calcified plaque between groups. However, if only LAD plaque volume was considered, chronic cocaine users demonstrated significantly greater (p = 0.046) plaque volume than that in non-users. Several studies have demonstrated that left coronary artery appealed to be more susceptible to atherosclerosis compared to right and circumference coronary arteries (22,23). This might be attributed to the intense arterial wall stresses due to the anatomical configuration in LAD (24). Giving the small sample size in our study, further research is needed to confirm whether atherosclerotic plaque is more aggravated in certain coronary territories than in others.
Several studies have shown that persons with HIV infection have an elevated risk of coronary artery disease compared to the general population due to chronic immune activation, inflammation, and ART drug exposure (25–27). Studies also demonstrated higher prevalence of coronary artery calcified and non-calcified plaque in HIV-infected persons compared to HIV-uninfected persons (26,28). However, we did not find any association in plaque volume with HIV status in this investigation. Foldyna et al. revealed significant increased odds of having any subclinical coronary atherosclerotic plaque in men than in women among asymptomatic HIV-infected individuals on ART (29). Our findings also underscored the importance of sex as a determinant of coronary atherosclerosis. While these results could be partly attributed to the small sample size, we believe that years of cocaine use could likely outweigh HIV and sex as a major contributor to more measures of coronary plaque. Rodriguez and colleagues examined the relationship between coronary plaque burden in relationship to cardiovascular risk factors in 199 asymptomatic individuals of age greater than 55 years with low-to-moderate risk (30). Age was a strong predictor of calcified plaque but not of noncalcified plaque. We have also found that age remained to be significantly associated with plaque volume even after adjusting for cocaine years use.
The inclusion criteria for cocaine use varied between studies based on the nature of the research. For example, Pletcher et al. (American heart journal 2005;150:921-6) investigated the cocaine and coronary calcification in young adults (CARDIA study) (19). Cocaine usage was measured by questionnaire and categorized by lifetime exposure and recent exposure. Ebersberger et al. studied atherosclerotic plaque burden in cocaine users with acute chest pain (10). Only patients with a history of non-occasional cocaine use (>3 times/year) were considered. In our study, we focused on the effects of chronic cocaine use on the coronary artery plaque volume. Hence, we felt a strict inclusion criterion should be employed to rule out infrequent users.
We must acknowledge the presence of several limitations in our study. First, this was a study with a limited number of participants and unbalanced data (69% were chronic cocaine users and 81% were men, and 81% were HIV positive). Of note, although the chronic and non-cocaine users in this study were not matched explicitly, the groups were comparable with respect to sex, age, BMI, diabetes, and HIV status. Second, because of the above-mentioned reason and multicollinearity of several factors (age, cocaine years use, HIV infection), it was difficult to identify the synergistic effects of HIV infection and cocaine use on coronary plaque volume. Third, our participants were limited to asymptomatic men and women without overt cardiovascular disease or acute coronary syndrome. Information about coronary plaque volume and cocaine use in symptomatic individuals requires further investigation. Fourth, we could not use DSM-IVR or DSM-5 criteria represented by the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM) for diagnosis of cocaine dependence since those criteria have to be used by physicians. Finally, causal relations cannot be assessed in this cross-sectional study, and generalizability of the results from this study should be evaluated in a large cohort.
Our study demonstrated a strong tendency towards overall more pronounced atherosclerosis in chronic cocaine users and the longer the cocaine use, the greater the plaque burden. Additional research is needed to uncover if plaque progressions among coronary territories were heterogeneous in cocaine users as well as its detrimental health consequences.
Funding
The study was supported by the National Institute on Drug Abuse, National Institutes of Health, US (R01DA12777, R01DA25524, R21DA048780, U01DA040325).
Footnotes
Disclosure of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- 1.Redman M Cocaine: What is the Crack? A Brief History of the Use of Cocaine as an Anesthetic. Anesthesiology and pain medicine 2011;1:95–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstein RA, DesLauriers C, Burda AM. Cocaine: history, social implications, and toxicity--a review. Disease-a-month : DM 2009;55:6–38. [DOI] [PubMed] [Google Scholar]
- 3.Riezzo I, Fiore C, De Carlo D, Pascale N, Neri M, Turillazzi E, Fineschi V. Side effects of cocaine abuse: multiorgan toxicity and pathological consequences. Current medicinal chemistry 2012;19:5624–46. [DOI] [PubMed] [Google Scholar]
- 4.Abuse S Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration; 2019. [Google Scholar]
- 5.Kumar V, Gopalakrishnan L, Singh M, Singh S, Kovacs DF, Benatar D, Gibson CM, Khosla S. Effect of Cocaine on Coronary Microvasculature. Journal of the American College of Cardiology 2018;71:954–955. [DOI] [PubMed] [Google Scholar]
- 6.Rezkalla SH, Kloner RA. Cocaine-induced acute myocardial infarction. Clinical medicine & research 2007;5:172–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talarico GP, Crosta ML, Giannico MB, Summaria F, Calo L, Patrizi R. Cocaine and coronary artery diseases: a systematic review of the literature. Journal of cardiovascular medicine 2017;18:291–294. [DOI] [PubMed] [Google Scholar]
- 8.Benzaquen BS, Cohen V, Eisenberg MJ. Effects of cocaine on the coronary arteries. American heart journal 2001;142:402–10. [DOI] [PubMed] [Google Scholar]
- 9.den Uil CA, Ligthart JMR, Mandigers L, den Dekker WK. Cocaine/amphetamine-induced accelerated atherosclerosis, coronary spasm and thrombosis, and refractory ventricular fibrillation. European heart journal Case reports 2019;3:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ebersberger U, Sudarski S, Schoepf UJ, Bamberg F, Tricarico F, Apfaltrer P, Blanke P, Schindler A, Makowski MR, Headden GF, Leber AW, Hoffmann E, Vliegenthart R. Atherosclerotic plaque burden in cocaine users with acute chest pain: analysis by coronary computed tomography angiography. Atherosclerosis 2013;229:443–8. [DOI] [PubMed] [Google Scholar]
- 11.Hess KL, Johnson SD, Hu X, Li J, Wu B, Yu C, Zhu H, Jin C, Chen M, Gerstle J. Diagnoses of HIV infection in the United States and dependent areas, 2017. 2018. [Google Scholar]
- 12.Khalsa JH, Elkashef A. Interventions for HIV and hepatitis C virus infections in recreational drug users. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2010;50:1505–11. [DOI] [PubMed] [Google Scholar]
- 13.Sandfort V, Bluemke DA, Vargas J, Brinker JA, Gerstenblith G, Kickler T, Zheng G, Li J, Chen S, Lai H, Fishman EK, Lai S. Coronary Plaque Progression and Regression in Asymptomatic African American Chronic Cocaine Users With Obstructive Coronary Stenoses: A Preliminary Study. Journal of addiction medicine 2017;11:126–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai H, Moore R, Celentano DD, Gerstenblith G, Treisman G, Keruly JC, Kickler T, Li J, Chen S, Lai S, Fishman EK. HIV Infection Itself May Not Be Associated With Subclinical Coronary Artery Disease Among African Americans Without Cardiovascular Symptoms. J Am Heart Assoc 2016;5:e002529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS, American Heart Association Writing Group on Myocardial S, Registration for Cardiac I. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539–42. [DOI] [PubMed] [Google Scholar]
- 16.Kloner RA, Hale S, Alker K, Rezkalla S. The effects of acute and chronic cocaine use on the heart. Circulation 1992;85:407–19. [DOI] [PubMed] [Google Scholar]
- 17.Dressler FA, Malekzadeh S, Roberts WC. Quantitative analysis of amounts of coronary arterial narrowing in cocaine addicts. The American journal of cardiology 1990;65:303–8. [DOI] [PubMed] [Google Scholar]
- 18.Karch SB, Green GS, Young S. Myocardial hypertrophy and coronary artery disease in male cocaine users. Journal of forensic sciences 1995;40:591–5. [PubMed] [Google Scholar]
- 19.Pletcher MJ, Kiefe CI, Sidney S, Carr JJ, Lewis CE, Hulley SB. Cocaine and coronary calcification in young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. American heart journal 2005;150:921–6. [DOI] [PubMed] [Google Scholar]
- 20.Chang AM, Walsh KM, Shofer FS, McCusker CM, Litt HI, Hollander JE. Relationship between cocaine use and coronary artery disease in patients with symptoms consistent with an acute coronary syndrome. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 2011;18:1–9. [DOI] [PubMed] [Google Scholar]
- 21.Lai S, Lima JA, Lai H, Vlahov D, Celentano D, Tong W, Bartlett JG, Margolick J, Fishman EK. Human immunodeficiency virus 1 infection, cocaine, and coronary calcification. Archives of internal medicine 2005;165:690–5. [DOI] [PubMed] [Google Scholar]
- 22.Schmermund A, Baumgart D, Mohlenkamp S, Kriener P, Pump H, Gronemeyer D, Seibel R, Erbel R. Natural history and topographic pattern of progression of coronary calcification in symptomatic patients: An electron-beam CT study. Arterioscler Thromb Vasc Biol 2001;21:421–6. [DOI] [PubMed] [Google Scholar]
- 23.Tuzcu EM, Kapadia SR, Tutar E, Ziada KM, Hobbs RE, McCarthy PM, Young JB, Nissen SE. High prevalence of coronary atherosclerosis in asymptomatic teenagers and young adults: evidence from intravascular ultrasound. Circulation 2001;103:2705–10. [DOI] [PubMed] [Google Scholar]
- 24.Chatzizisis YS, Giannoglou GD, Parcharidis GE, Louridas GE. Is left coronary system more susceptible to atherosclerosis than right? A pathophysiological insight. Int J Cardiol 2007;116:7–13. [DOI] [PubMed] [Google Scholar]
- 25.Hakeem A, Bhatti S, Cilingiroglu M. The spectrum of atherosclerotic coronary artery disease in HIV patients. Current atherosclerosis reports 2010;12:119–24. [DOI] [PubMed] [Google Scholar]
- 26.Lai S, Bartlett J, Lai H, Moore R, Cofrancesco J Jr., Pannu H, Tong W, Meng W, Sun H, Fishman EK. Long-term combination antiretroviral therapy is associated with the risk of coronary plaques in African Americans with HIV infection. AIDS patient care and STDs 2009;23:815–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lo J, Abbara S, Shturman L, Soni A, Wei J, Rocha-Filho JA, Nasir K, Grinspoon SK. Increased prevalence of subclinical coronary atherosclerosis detected by coronary computed tomography angiography in HIV-infected men. Aids 2010;24:243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Post WS, Budoff M, Kingsley L, Palella FJ Jr., Witt MD, Li X, George RT, Brown TT, Jacobson LP. Associations between HIV infection and subclinical coronary atherosclerosis. Annals of internal medicine 2014;160:458–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foldyna B, Fourman LT, Lu MT, Mueller ME, Szilveszter B, Neilan TG, Ho JE, Burdo TH, Lau ES, Stone LA, Toribio M, Srinivasa S, Looby SE, Lo J, Fitch KV, Zanni MV. Sex Differences in Subclinical Coronary Atherosclerotic Plaque Among Individuals With HIV on Antiretroviral Therapy. Journal of acquired immune deficiency syndromes 2018;78:421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodriguez K, Kwan AC, Lai S, Lima JA, Vigneault D, Sandfort V, Pattanayak P, Ahlman MA, Mallek M, Sibley CT, Bluemke DA. Coronary Plaque Burden at Coronary CT Angiography in Asymptomatic Men and Women. Radiology 2015;277:73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]


