Abstract
Background
Stress is a dynamic construct that predicts a range of health behaviors and conditions, including binge eating and excess weight. Thus far, there have been limited and inconsistent findings regarding stress responses in binge-eating disorder (BED) and insufficient consideration of temporal patterns of stress responses across the weight spectrum.
Purpose
The present study used ecological momentary assessment (EMA) to examine stress reactivity (i.e., the magnitude of the initial stress response), recovery (i.e., how long the stress response lasts before returning to baseline), and pileup (i.e., accumulation of repeated experiences of stressors and responses over time) as predictors of binge-eating symptoms (BES) and food craving in BED.
Methods
Adults with BED (N = 115) completed a 7 day EMA protocol assessing stressful events, perceived stress, binge eating, and food craving prior to being randomized to a behavioral intervention.
Results
Generalized estimating equations indicated that moments of greater stress pileup predicted greater subsequent BES (within-person effect). Participants with higher perceived stress and pileup reported greater overall BES and craving, and those with better recovery reported higher overall craving (between-person effects).
Conclusions
Findings highlight the importance of considering the dynamic nature of stress responses and, particularly, that the accumulation of stress over the day is an important trigger for BES.
Keywords: Stress, Ecological momentary assessment, Binge-eating disorder, Obesity
Using real-time data collection methods in a sample of adults with binge eating disorder, the cumulative pileup of stress over the last 12 hours was more predictive of momentary binge eating compared to more recent ratings of stress.
Binge-eating disorder (BED) is characterized by recurrent binge eating (i.e., consumption of a large amount of food while feeling a loss of control over eating) in the absence of regular compensatory behaviors, such as purging, fasting, or exercise [1]. BED is associated with a range of negative outcomes, including psychosocial impairment, reduced quality of life, and a high degree of comorbidity with other psychiatric and medical conditions, particularly obesity [2–4]. Together, this constellation poses serious problems to the overall health and well-being of individuals with BED. Despite these health risks, the effectiveness of treatment for BED is suboptimal, as only approximately 50% of those who receive treatment achieve abstinence from binge eating [5]. As such, there is a critical need to identify and target the momentary processes contributing to the maintenance of binge eating and associated symptomatology.
Stress is a multifaceted, dynamic construct that is thought to be centrally important to binge eating and weight regulation [6, 7]. Stress has been defined as a negative emotional experience that is associated with biochemical, physiological, cognitive, and behavioral changes, which are directed toward altering the stressor or accommodating to its effects [8]. Stress has, therefore, been conceptualized as a key “upstream” factor that influences the development and maintenance of dysregulated eating and obesity through multiple interrelated pathways, including alterations related to cognitive functioning, physiology, and biochemistry [6, 7].
Consistent with this conceptualization of stress and affect regulation models of eating disorder behaviors, binge-eating symptoms (BES; i.e., overeating and loss of control eating) often occur in response to stress and negative emotional states [9]. This is further supported by research demonstrating relationships between heightened cortisol reactivity and eating behavior [10, 11]. These relationships may result in part from the effects of stress on reward processes, as acute stress can increase craving and preference for palatable energy-dense foods, possibly via links between cortisol release and appetite-related hormones and neuropeptides (i.e., ghrelin, neuropeptide Y, and leptin) [6, 12]. Given the relevance of stress for binge eating and weight management, identifying the momentary mechanisms by which stress predicts eating-related motivation and behaviors is important to develop more effective, targeted interventions.
Momentary Stress in BED
With respect to prior research on acute stress in BED, a recent review identified 14 laboratory studies assessing physiological and behavioral responses to experimentally induced stress in BED [7]. However, stress-induced eating was examined in only a limited number of studies (k = 4), indicating a clear need for future study in this area given that physiological and psychological stress can independently and interactively contribute to eating behaviors [7]. In addition, despite the methodological rigor of laboratory studies, such paradigms may also fail to capture the nature of psychological stressors occurring in daily life that are most relevant to eating behavior. Evaluating how momentary stress influences eating behaviors as they occur in the natural environment could lend more nuanced, ecologically valid insights into the microtemporal (e.g., moment-to-moment) processes underlying associations between psychological stress and eating.
To this end, ecological momentary assessment (EMA) research has been useful to elucidate such relationships. EMA involves repeated assessments of experiences in the natural environment, which allows for the examination of microtemporal relationships between variables and limits retrospective recall biases [13]. Earlier EMA work demonstrated relationships between momentary self-reported perceived stress and binge eating in anorexia nervosa [14] and bulimia nervosa [15–18], although no relationship was found between the occurrence of momentary stressors and binge eating among individuals with obesity [19]. Furthermore, no EMA studies have examined momentary responses to stressors in BED or obesity in naturalistic settings.
Dynamic Stress Responses
The inconsistent findings from prior experimental and EMA work could be due in part to a lack of consideration of the temporal patterning of stress responses. Recent research suggests that momentary stress responses are highly dynamic and can be delineated into three distinct components: (a) reactivity—that is, the magnitude of the initial stress response/change in affect; (b) recovery—that is, how long the stress response lasts before returning to baseline; and (c) pileup—that is, the accumulation of repeated experiences of stressors and responses over time [20]. Prior EMA work has shown that these stress response components demonstrate unique relationships with other health-related behaviors. For example, research in adults showed that the effects of stress reactivity, recovery, and pileup on physical activity levels differed from the effects of current perceived stress and negative affect; in addition, stress pileup over the previous 12 hr was more predictive of subsequent physical activity compared to stress reactivity and recovery [21]. However, dynamic stress responses have not been examined in relation to binge eating or in the context of BED or obesity. Examining momentary stress domains and momentary eating-related motivation and behaviors will provide a more temporally precise understanding of the moments at which individuals with BED are at elevated risk for engaging in maladaptive eating behaviors.
Stress, Body Weight, and BED
It is also important to note that the relative influences of overweight/obesity versus BED diagnostic status on stress response remain unclear given their common co-occurrence [7]. While stress is independently linked to excess weight [6], some research has also suggested that stress-induced eating in BED may be more strongly linked to psychological factors (e.g., anxiety) compared to physiological hunger, independent of weight status [22]. This is generally consistent with other findings demonstrating that individuals with binge eating report higher craving, emotional eating, and reward-related eating compared to weight-matched counterparts [23]. Furthermore, considerable research has suggested that BED in the context of obesity is a distinct phenotype of obesity such that negative affect is more strongly associated with dysregulated eating among those with BED and obesity compared to those with obesity without BED and binge eating in the context of obesity is associated with increased comorbidities, emotion regulation problems, and distress [4, 24, 25]. As such, it is important to adjust for weight status when examining stress in relation to eating behaviors.
Present Study
In light of the current gaps and limitations in the literature, the present study aimed to (a) assess the degree to which dynamic stress response components (i.e., reactivity, recovery, and pileup) are related to desire to eat and dysregulated eating behavior (i.e., craving and BES) measured via EMA among a treatment-seeking sample of adults with BED and (b) examine whether dynamic stress response components demonstrate unique explanatory power compared to single self-report assessments of perceived stress and after controlling for body mass index (BMI). It was hypothesized that greater stress reactivity and pileup, and poorer recovery, would be associated with increased craving and BES beyond the effects of self-reported perceived stress.
Method
Participants and Procedure
Participants were drawn from an initial sample of 115 adults who completed pretreatment assessments as part of a two-site treatment trial assessing the efficacy of two psychosocial treatments for BED (integrative cognitive-affective therapy [ICAT-BED] and cognitive behavior therapy guided self-help [CBTgsh]) [26–28]. This randomized controlled trial was registered with clinicaltrials.gov (NCT02043496). Participants were recruited from eating disorder clinics, community advertisements, and social media postings at two sites in the midwest USA. Exclusion criteria for the study included severe comorbid psychopathology (i.e., lifetime history of psychotic symptoms or bipolar disorder and substance use disorder within 6 months of enrollment), medical or psychiatric instability (e.g., active suicidality), clinically significant purging behavior, eating or weight loss treatment, or a medical condition affecting eating or weight. Institutional review board approval for the study was obtained at each site. Informed consent was obtained from all individual participants included in the study.
After an initial eligibility screening, participants completed a baseline study visit that included semistructured clinical interviews assessing eating disorder symptoms and comorbid psychopathology, followed by a 7 day EMA protocol to assess symptoms in the natural environment. EMA was completed using the ReTAINE (Real-Time Assessment in the Natural Environment; see ReTAINE.org) system administered by smartphone. Participants were then randomized to ICAT-BED or CBTgsh. Participants returned for outcome assessments at the end of treatment and 6 month follow-up. Each wave of assessment included a 7 day EMA protocol; however, the present study only utilized the pretreatment EMA data. Participants received $150 for assessments following study completion.
Measures
Diagnostic interviews
The Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Version [29] was used to assess DSM-IV Axis I disorders to examine exclusion criteria and for descriptive purposes. The Eating Disorder Examination (EDE) version 16.0 [30] was administered by trained assessors to establish DSM-5 BED diagnoses and for descriptive purposes.
Anthropometric assessments
Height and weight were measured with a stadiometer and scale and used to calculate BMI (kilograms per square meter).
EMA measures
The EMA protocol utilized both signal- and interval-contingent recordings. Signal-contingent recordings are completed at variable time intervals; for these recordings, participants were prompted to complete assessments throughout the day in response to five semirandom signals evenly distributed around five anchor points between 8 am and 10 pm. Interval-contingent recordings are made at fixed times; for these recordings, participants completed a final assessment at the end of the day (i.e., bedtime). At each recording, participants were asked to rate their current mood, stress level, occurrence of stressors, and craving and to report any eating behaviors that had not yet been recorded. If a participant reported an eating episode, he/she was prompted to complete items assessing binge eating. Participants indicated the timing of reported eating episodes in order to locate that eating behavior in time and establish temporality. This EMA schedule resulted in a maximum of 42 possible recordings per person during the study (i.e., [5 semirandom signals/day + 1 end of day signal] × 7 days).
Binge eating
Overeating and loss of control eating were measured at all eating episodes. Overeating was assessed with two items: (a) “To what extent to do you feel that you overate?” and (b) “To what extent do you feel that you ate an excessive amount of food?” Loss of control eating was assessed with four items: (a) “While you were eating, to what extent did you feel a sense of loss of control?” (b) “While you were eating, to what extent did you feel that you could not resist eating?” (c) “While you were eating, to what extent did you feel that you could not stop eating once you had started?” and (d) “While you were eating, to what extent did you feel driven or compelled to eat?” Items were rated on a scale from 1 (not at all) to 5 (extremely). Loss of control and overeating items were first averaged to create two composite scores (α = .83 and .93, respectively); then a dimensional rating of BES was calculated at each eating episode by summing the loss of control and overeating composite scores.
Craving
Participants indicated their current level of craving for food by rating the item “I am craving food” on a scale from 1 (not at all) to 5 (completely), with higher ratings indicating greater momentary craving.
Stressors and perceived stress level
Participants rated their current level of stress on a visual analog scale from 1 (none) to 100 (extreme). Participants also indicated whether any stressful events had occurred since the last EMA signal that was related to the following domains: family concerns, personal relationships, financial problems, work-related problems, school-related problems, or other problems. For descriptive purposes, family concerns and personal relationships were categorized as “interpersonal,” and work- and school-related problems were categorized as “work/school-related.” If any stressor was reported, the timepoint was coded as a stressor moment.
Statistical Analyses
Stress response components
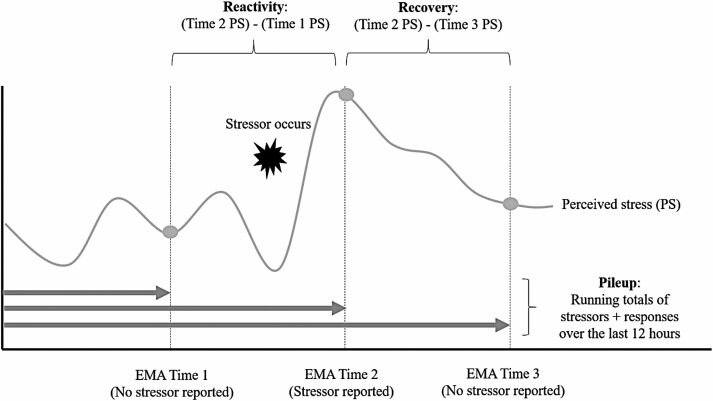
Calculation of stress reactivity, recovery, and pileup was calculated based on the procedures outlined in Almeida et al. [21]. Figure 1 presents a conceptual depiction of reactivity, recovery, and pileup across EMA signals.
Fig. 1.
Conceptual depiction of dynamic stress response components (reactivity, recovery, and pileup) across ecological momentary assessment (EMA) signals.
Stress reactivity
This calculation used EMA recordings when a stressor was reported following a nonstressor EMA signal. The perceived stress score from the nonstressor moment at the last EMA signal (t − 1) was subtracted from the perceived stress score when the recent stressor was reported at time t. Higher scores reflect greater increases in perceived stress following a stressor, indicating greater reactivity.
Stress recovery
The level of perceived stress on a nonstressor moment that was reported following a stressor (t + 1) was subtracted from the level of perceived stress reported at a prior stressor moment (t). Higher scores indicate a greater decline in perceived stress after a stressor, thereby reflecting better stress recovery.
Stress pileup
The accumulation of stress was defined as the combination of stressors and stress responses over the previous 12 hr. First, EMA recordings were categorized based on the endorsement of a stressor since the last EMA signal (coded 0 or 1) and whether the perceived stress level was at least 1.5 standard deviations [SDs] above the participant’s own baseline perceived stress (coded 0 or 1). Each participant’s baseline perceived stress was calculated as the mean of perceived stress ratings occurring (a) on days when no stressors were reported and (b) at EMA signals prior to the first stressor of the day on days when stressors were reported; this approach was taken to minimize the impact of prior stressors on perceived stress ratings reported at nonstressor moments. Next, the total number of EMA signals coded as both a stressor occurrence and stress response (i.e., occurrence of a stressor accompanied by a perceived stress score that was ≥1.5 SDs above one’s baseline perceived stress level) over the prior 12 hr were summed over a moving 12 hr window ending at the current EMA signal.
Hypothesis testing
To evaluate Aim 1, separate generalized estimating equations (GEEs) with AR1 covariance structures were conducted to examine the association between each dynamic stress index (i.e., stress reactivity, stress recovery, and pileup) and two dependent variables (i.e., craving and BES). GEEs are an extension of the generalized linear model that apply a semiparametric approach to longitudinal analysis. GEEs use one clustering variable and estimate parameters across clusters to yield population-level inferences [31]. Two separate GEEs examined perceived stress ratings as independent variables in order to compare the effects of dynamic and static stress measures (Aim 2). Gamma link functions were used to account for nonnormal distributions. Each GEE included between-person (i.e., grand-mean centered) and within-person effects (i.e., person-mean centered) of independent variables. That is, between-person effects indicate the degree to which individuals who are higher or lower on a variable (relative to the sample mean) generally report higher or lower levels of a dependent variable, aggregating across EMA measurements. For instance, individuals who report higher overall stress, relative to individuals with lower overall stress, may experience more severe binge eating during the EMA monitoring period. Within-person effects indicate the degree to which momentary fluctuations in a variable (relative to the person’s own average level) are related to levels of an outcome variable measured at a single EMA measurement. For instance, when an individual experiences an increase in stress that is higher than his/her usual baseline level of stress, he/she may be at greater risk to engage in binge eating. Within-person perceived stress was lagged from the prior EMA signal (t − 1) in models to establish temporal order of this effect. All analyses controlled for BMI, age (grand-mean centered), and gender. Analyses were based on all available data without imputation; GEEs were based on full information maximum likelihood methods. Alpha was set at .05; adjustments were not made for multiple comparisons. Analyses were conducted using SPSS 25 and SAS 9.4.
Results
Descriptive statistics are presented for the full sample (N = 115) in Table 1. At baseline, the mean age of the sample was 39.9 years (SD = 13.2), and the mean BMI was 35.2 kg/m2 (SD = 8.6; range: 21.4–62.0); 20.0% of the sample had a BMI in the overweight range (25 ≤ BMI < 30 kg/m2), and 67.0% had a BMI in the obese range (BMI ≥ 30 kg/m2). The majority of the sample was female (82.3%) and Caucasian (92.9%). The observed time intervals between consecutive EMA assessments within a day ranged from 1.2 to 4.7 hr, with an average of 3.1 hr (SD = 0.88). The nature of missing data was explored by examining associations between the number of completed EMA signals per person and demographic (i.e., age, BMI, and gender) and clinical characteristics (i.e., severity of binge-eating psychopathology, as measured by EDE binge episode frequency). The number of completed EMA signals was not significantly related to participants’ age (r = 0.12, p = .197), BMI (r = −0.03, p = .759) or binge frequency (Spearman ρ = 0.05, p = .578), nor did it differ between men and women (t[111] = −1.78, p = .08).
Table 1.
Descriptive statistics
| n | Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|---|
| Number of EMA days completed | 115 | 6.51 | 1.56 | 1.00 | 8.00 |
| Number of EMA signals completed | 115 | 27.34 | 10.63 | 1.00 | 43.00 |
| Number of eating episodes reported | 115 | 18.97 | 8.00 | 0.00 | 33.00 |
| Age | 112 | 39.93 | 13.22 | 18.00 | 64.00 |
| BMI | 115 | 35.15 | 8.60 | 21.41 | 62.03 |
| Craving mean | 115 | 2.39 | 0.78 | 1.00 | 5.00 |
| Binge-eating mean | 114 | 5.01 | 1.51 | 2.13 | 9.35 |
| LOC-eating mean | 114 | 2.67 | 0.84 | 1.13 | 4.55 |
| Overeating mean | 114 | 2.34 | 0.77 | 1.00 | 4.80 |
| Perceived stress mean | 115 | 28.39 | 18.79 | 0.40 | 94.77 |
| Reactivity mean | 82 | 15.23 | 14.39 | −5.00 | 81.00 |
| Recovery mean | 87 | 15.18 | 11.11 | −1.50 | 53.00 |
| Pileup mean | 115 | 1.32 | 0.82 | 0.00 | 3.50 |
| Total interpersonal stressors reported | 115 | 6.97 | 6.56 | 0.00 | 37.00 |
| Total work/school stressors reported | 115 | 7.43 | 6.89 | 0.00 | 27.00 |
| Total financial stressors reported | 115 | 4.09 | 7.51 | 0.00 | 37.00 |
| Total other stressors reported | 115 | 6.50 | 7.55 | 0.00 | 34.00 |
| Total stressors reported | 113 | 25.42 | 17.94 | 2.00 | 82.00 |
EMA-measured variables were aggregated within person (i.e., mean or total scores across the EMA protocol).
BMI body mass index; EMA ecological momentary assessment; LOC loss of control; SD standard deviation.
Stressors were reported at 62.2% of the 3,144 completed EMA signals. Participants reported an average of 1.47 ± 0.72 (range: 1–4) types of stressors at each EMA signal. Over the course of EMA, work-/school-related stressors were the most commonly reported type of stressor, followed by interpersonal and financial stressors. Table 2 displays Spearman rank correlations. While mean stress reactivity and recovery were moderately correlated (ρ = .52), they were less strongly related to pileup (ρ = .23). Moderate to strong associations were observed between mean perceived stress and dynamic stress responses (ρ = .36–.59). Table 3 displays GEE results. The available sample size and observations were lower for GEEs examining reactivity (ns = 71–79; observations: 169–226) and recovery (ns = 72–84; observations: 203–321) compared to GEEs examining perceived stress (n = 109; observations: 1,617–2,354) and pileup (n = 111; observations: 2,129–3,062). This was due to the fact that there were fewer available intervals possible to test reactivity and recovery because they require the sequential order of stressor and eating episode.
Table 2.
Spearman correlations (EMA variables are aggregated within person)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | 0.11 | −0.21* | −0.05 | −0.06 | −0.04 | −0.26** | −0.03 | −0.06 | −0.07 | 0.10 | −0.19* | −0.09 | 0.02 | −0.02 |
| 2. BMI | – | 0.19* | 0.19* | 0.13 | 0.25** | 0.04 | 0.01 | 0.16 | 0.10 | 0.07 | 0.09 | −0.09 | 0.06 | 0.08 | |
| 3. Craving mean | – | 0.37** | 0.43** | 0.26** | 0.23* | 0.06 | 0.21 | 0.28** | 0.14 | 0.17 | 0.12 | 0.07 | 0.23* | ||
| 4. Binge-eating mean | – | 0.94** | 0.92** | 0.30** | 0.01 | 0.15 | 0.24* | 0.17 | 0.17 | 0.07 | 0.03 | 0.17 | |||
| 5. LOC-eating mean | – | 0.74** | 0.29** | −0.03 | 0.10 | 0.25** | 0.20* | 0.15 | 0.08 | 0.06 | 0.18 | ||||
| 6. Overeating mean | – | 0.27** | 0.01 | 0.14 | 0.19* | 0.15 | 0.14 | 0.04 | 0.03 | 0.15 | |||||
| 7. Perceived stress mean | – | 0.37** | 0.36** | 0.59** | 0.32** | 0.34** | 0.24* | 0.14 | 0.34** | ||||||
| 8. Reactivity mean | – | 0.52** | 0.23* | 0.22 | 0.16 | 0.05 | 0.13 | 0.24* | |||||||
| 9. Recovery mean | – | 0.23* | 0.06 | 0.16 | 0.03 | −0.02 | 0.09 | ||||||||
| 10. Pileup mean | – | 0.49** | 0.30** | 0.38** | 0.21* | 0.58** | |||||||||
| 11.Total interpersonal stressors | – | 0.46** | 0.32** | 0.20* | 0.68** | ||||||||||
| 12. Total work/school stressors | – | 0.41** | 0.10 | 0.63** | |||||||||||
| 13. Total financial stressors | – | 0.12 | 0.65** | ||||||||||||
| 14. Total other stressors | – | 0.50** | |||||||||||||
| 15. Total stressors | – |
BMI body mass index; EMA ecological momentary assessment; LOC loss of control.
*p < .05.
**p < .01.
Table 3.
Generalized estimating equation results
| Binge eating | Craving | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Perceived stress | B | SE | Lower CI | Upper CI | Wald χ 2 | p | B | SE | Lower CI | Upper CI | Wald χ 2 | p |
| Intercept | 1.53 | 0.07 | 1.40 | 1.66 | 522.55 | <.001 | 0.82 | 0.05 | 0.72 | 0.93 | 244.70 | <.001 |
| Gender | 0.09 | 0.07 | −0.05 | 0.23 | 1.59 | .208 | 0.06 | 0.06 | −0.06 | 0.18 | 0.81 | .367 |
| Age | <−0.01 | <0.01 | −0.01 | <0.01 | 1.28 | .258 | −0.01 | <0.01 | −0.01 | <0.01 | 7.06 | .008 |
| BMI | 0.01 | <0.01 | <0.01 | 0.01 | 6.85 | .009 | 0.01 | <0.01 | <0.01 | 0.01 | 5.22 | .022 |
| Perceived stress (between) | 0.01 | <0.01 | <0.01 | 0.01 | 25.16 | <.001 | 0.01 | <0.01 | <0.01 | 0.01 | 7.91 | .005 |
| Perceived stress (within) | <0.01 | <0.01 | <−0.01 | <0.01 | 0.02 | .895 | <0.01 | <0.01 | <0.01 | <0.01 | 2.41 | .120 |
| n = 109; observations = 1,617 | n = 109; observations = 2,354 | |||||||||||
| Reactivity | B | SE | Lower CI | Upper CI | Wald χ 2 | p | B | SE | Lower CI | Upper CI | Wald χ 2 | p |
| Intercept | 1.72 | 0.14 | 1.45 | 1.99 | 154.39 | <.001 | 0.86 | 0.11 | 0.64 | 1.07 | 61.25 | <.001 |
| Gender | −0.07 | 0.15 | −0.36 | 0.22 | 0.21 | .649 | 0.01 | 0.12 | −0.23 | 0.25 | 0.01 | .943 |
| Age | −0.01 | <0.01 | −0.01 | <0.01 | 2.99 | .084 | −0.01 | <0.01 | −0.02 | <0.01 | 7.37 | .007 |
| BMI | 0.01 | 0.01 | <−0.01 | 0.02 | 2.04 | .153 | 0.01 | 0.01 | <0.01 | 0.02 | 4.33 | .037 |
| Reactivity (between) | <0.01 | <0.01 | <−0.01 | 0.01 | 2.51 | .113 | <0.01 | <0.01 | <−0.01 | 0.01 | 0.55 | .456 |
| Reactivity (within) | <0.01 | <0.01 | <−0.01 | 0.01 | 0.13 | .717 | <0.01 | <0.01 | <−0.01 | 0.01 | 0.35 | .552 |
| n = 71; observations = 169 | n = 79; observations = 226 | |||||||||||
| Recovery | B | SE | Lower CI | Upper CI | Wald χ 2 | P | B | SE | Lower CI | Upper CI | Wald χ 2 | p |
| Intercept | 1.46 | 0.15 | 1.17 | 1.74 | 100.01 | <.001 | 0.62 | 0.12 | 0.39 | 0.84 | 28.10 | <.001 |
| Gender | 0.12 | 0.16 | −0.18 | 0.43 | 0.63 | .427 | 0.22 | 0.12 | −0.02 | 0.47 | 3.21 | .073 |
| Age | <−0.01 | <0.01 | −0.01 | <0.01 | 0.61 | .436 | <−0.01 | <0.01 | −0.01 | <0.01 | 1.49 | .221 |
| BMI | 0.02 | <0.01 | 0.01 | 0.03 | 16.58 | <.001 | 0.01 | <0.01 | <0.01 | 0.02 | 5.73 | .017 |
| Recovery (between) | <−0.01 | <0.01 | −0.01 | <0.01 | 1.07 | .302 | 0.01 | <0.01 | <0.01 | 0.01 | 4.31 | .038 |
| Recovery (within) | <0.01 | <0.01 | <−0.01 | 0.01 | 0.50 | .481 | <0.01 | <0.01 | <−0.01 | <0.01 | 0.02 | .886 |
| n = 72; observations = 203 | n = 84; observations = 321 | |||||||||||
| Pileup | B | SE | Lower CI | Upper CI | Wald χ 2 | p | B | SE | Lower CI | Upper CI | Wald χ 2 | p |
| Intercept | 1.54 | 0.08 | 1.38 | 1.70 | 366.63 | <.001 | 0.79 | 0.05 | 0.69 | 0.89 | 222.90 | <.001 |
| Gender | 0.05 | 0.08 | −0.12 | 0.22 | 0.34 | .558 | 0.08 | 0.06 | −0.04 | 0.20 | 1.61 | .204 |
| Pileup | B | SE | Lower CI | Upper CI | Wald χ 2 | p | B | SE | Lower CI | Upper CI | Wald χ 2 | p |
| Age | <−0.01 | <0.01 | −0.01 | <0.01 | 2.44 | .118 | −0.01 | <0.01 | −0.01 | <−0.01 | 9.17 | .002 |
| BMI | 0.01 | <0.01 | <0.01 | 0.01 | 6.47 | .011 | 0.01 | <0.01 | <0.01 | 0.01 | 5.98 | .014 |
| Pileup (between) | 0.13 | 0.04 | 0.06 | 0.20 | 13.01 | <.001 | 0.13 | 0.03 | 0.06 | 0.19 | 14.50 | <.001 |
| Pileup (within) | 0.06 | 0.01 | 0.04 | 0.08 | 29.26 | <.001 | −0.01 | 0.01 | −0.03 | 0.01 | 1.09 | .296 |
| n = 111; observations = 2,129 | n = 111; observations = 3,062 |
Within-person perceived stress was lagged from the prior EMA signal (t − 1). Gender was coded such that men were the reference category. Bolded effects are significant at p < .05, adjusted for gender, age, and BMI. Between = grand-mean-centered variable (reflecting individual differences); within = person-mean-centered variable (reflecting fluctuations relative to an individual’s own average level of a variable).
BMI body mass index; CI 95% confidence interval; EMA ecological momentary assessment; SE standard error.
Perceived Stress
There were main effects of between-person perceived stress predicting BES and craving such that individuals with greater overall perceived stress reported more BES and craving during the EMA protocol. There were no significant effects of within-person perceived stress. In other words, when individuals reported greater perceived stress relative to their usual levels, they were not more likely to report subsequent increases in BES or craving.
Stress Reactivity
The GEE examining reactivity as a predictor of BES and craving revealed no significant effects of between- or within-person stress reactivity. That is, individuals who had greater stress reactivity did not report more BES or craving than individuals with less stress reactivity and, at moments when individuals reported greater stress reactivity relative to their usual levels, they were not more likely to report subsequent increases in BES or craving.
Stress Recovery
Similarly, stress recovery was not related to BES at the between- or within-person level. However, there was a significant effect of between-person stress recovery predicting craving such that participants with higher (i.e., better) recovery reported more craving across the EMA protocol. There was no significant effect of within-person recovery predicting craving. That is, while individuals with better stress recovery experienced more craving on average, at moments when individuals had better or worse stress recovery compared to their usual level, they were not more likely to report increases in craving.
Stress Pileup
With respect to stress pileup, there were significant between- and within-person main effects predicting binge eating. That is, participants with greater overall stress pileup reported more BES over the course of EMA (between-person effect). In addition, at moments when participants had experienced greater pileup over the last 12 hr (i.e., a greater number of stressors associated with heightened negative affect), relative to their own average level of pileup, they reported greater subsequent BES at the next EMA signal (within-person effect). For craving, there was also a significant main effect of between-person pileup such that individuals with higher pileup reported higher craving on average. There was not a significant effect of within-person pileup on craving.
Discussion
The present study sought to examine dynamic stress response components (i.e., reactivity, recovery, and pileup) in relationship to food craving and BES in BED, after adjusting for weight status. Hypotheses were partially supported in that stress pileup was the dynamic stress index that contributed to both food craving and BES. However, no hypothesized effects were supported for stress reactivity or recovery and, contrary to hypotheses, better stress recovery was associated with higher overall craving. There were also similarities and differences across static (i.e., derived from single timepoint assessments) and dynamic stress measures. At the individual level (i.e., between-person effects), both perceived stress and pileup were associated with greater BES and craving. These similarities are consistent with correlations that showed moderate to strong correlations between perceived stress and the dynamic stress indices at the individual level (rs = 0.36–0.59), suggesting at least some overlap in these constructs. However, differences between static and dynamic measures also emerged. At the momentary (i.e., within person) level, individuals were more likely to report BES at moments when they had higher stress pileup, though momentary stress reactivity, recovery, and perceived stress were not related to subsequent BES or craving.
The observed individual-level effects regarding BES and craving are largely consistent with the broader literature suggesting that stress is related to dysregulated eating [8]. Findings from the current study lend a more nuanced understanding of these associations in BED and are not attributable to the effects of co-occurring obesity alone. These findings are also supported by literature showing distinctions between acute and chronic stress responses (i.e., high allostatic load) [32]. That is, allostatic load refers to the cumulative effects of activated physiological (neuroendocrine, autonomic, and metabolic) responses to stressful experiences, with allostatic overload being associated with numerous negative health consequences [33]. In the present sample, it is possible that the result of chronic stress or allostatic overload was manifested by the trait-level (i.e., between person) effects of perceived stress and stress pileup on BES and craving. However, contrary to hypotheses, individuals with better stress recovery also reported higher food craving. One possibility is that the tendency to experience greater relief from stressors may activate hedonic appetite and trigger an increased desire to eat when in a good or significantly improved mood—that is, eating for reward enhancement [34].
Despite these effects, individual differences in stress reactivity and recovery were not associated with BES, and neither momentary reactivity nor recovery predicted subsequent BES or craving levels the next EMA signal. It is important to note that these models were based on a smaller number of observations, which may have impacted the ability to detect effects. Given that the average interval between EMA recordings was approximately 3 hr, it is also possible that the EMA prompts were too infrequent to capture the dynamic process of recovery and reactivity. Thus, the potential nature and timescale of these associations are yet unclear. In addition, these stress indices were based on self-reports over 1 week, and future research is warranted to assess the degree to which these indices also converge with self-report and physiological measures of chronic stress over longer time periods.
It is also significant that only stress pileup was related to subsequent BES at the momentary level (i.e., within-person effect) and that only average levels but not momentary fluctuations in perceived stress were predictive of BES. This finding aligns with the results of Almeida et al., who found that stress pileup was more strongly associated with physical activity compared to reactivity and recovery [21]. In other words, compared to other within-person stress indices that focus on relatively short-term fluctuations (i.e., moments of increased perceived stress, stress reactivity, and stress recovery), the cumulative buildup of stress over recent hours appears to be more salient in predicting the moments at which individuals with BED are likely to engage in binge eating. It may be that temporary fluctuations in stress are not unequivocally linked to subsequent maladaptive eating behavior. Rather, the progressive buildup of stress is likely to lead to dysregulated eating among individuals who have difficulties with consistently implementing adaptive emotion regulation strategies over the course of the day, such as those with BED [25].
Limitations
There are also several limitations to acknowledge the present study. Only signal- and interval-contingent EMA recordings were used in this study, which may have failed to capture all eating episodes; however, this was done to minimize participant burden associated with event-contingent recordings (i.e., completing assessments immediately after behaviors of interest). The sample was limited to primarily Caucasian women, which limits the generalizability of findings to other demographic groups. While EMA and interview-based measures of binge eating have shown moderate convergence [35], it is unclear the extent to which self-reported overeating corresponded to objective amounts of food consumed. As previously noted, stress indices relied on self-report, and it is was not possible to determine how these measures correspond to objective physiological markers of stress responses (e.g., cortisol). In addition, there were less data points to derive reactivity and recovery indices, which may attenuate the reliability of these stress indices; thus, EMA monitoring periods longer than 7 days would be advantageous to address this concern. Lastly, all participants were diagnosed with BED, most of whom had overweight/obesity. Given that stress can lead to both overeating and undereating [12], it would be informative for future research to explore how these results may differ in other eating disorders and groups without overweight/obesity.
Conclusions and Future Directions
Collectively, these results highlight the importance of considering temporal patterning of stress responses in relation to eating-related motivation and behavior in BED, independent of weight status. Based on the present study, the cumulative buildup of stress appears most relevant when predicting episodes of binge eating, which has direct implications for the development of tailored momentary interventions (i.e., just-in-time adaptive interventions) that could be harnessed to target these times of risk with stress management or emotion regulation strategies [36]. The current findings imply that it is necessary for such interventions to take into account not only individuals’ current states but also how they have experienced and responded to prior stressors that day. Future research is also needed to determine what threshold of stress pileup has to be reached before a given individual will engage in binge eating. In addition, trait-level (i.e., between person) relationships indicate that chronic stress is nevertheless a relevant clinical target, and additional work is needed to examine how longer-term stress management and emotion regulation interventions may alter dynamic stress responses and associated biomarkers in BED. Ultimately, identifying and targeting acute and chronic stress may serve to enhance the efficacy of BED treatments and mitigate the associated psychological and physical health consequences of this disorder.
Funding: This research was supported by the National Institute of Mental Health (grant numbers R34 MH099040-01A1, R34MH098995, and T32 MH082761).
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors declare that they have no conflict of interest.
Authors’ Contributions K.E.S.: Conceptualization, Methodology, Formal analysis, Writing- Original draft preparation, Review & Editing; T.B.M.: Writing- Original draft preparation, Review, & Editing; L.M.S.: Writing- Original draft preparation, Review & Editing; L.M.A.: Writing- Original draft preparation, Review & Editing; K.C.: Writing- Original draft preparation; R.D.C.: Funding acquisition, Investigation, Methodology, Project administration, Supervision, Formal analysis, Writing- Review & Editing; Writing- Review, & Editing; S.G.E.: Funding acquisition, Investigation, Methodology, Project administration, Writing- Review & Editing; S.J.C.: Funding acquisition, Investigation, Methodology, Project administration, Writing- Review & Editing; S.A.W.: Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing- Review & Editing; C.B.P.: Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing- Review & Editing.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association, 2013. [Google Scholar]
- 2.Udo T, Grilo CM. Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. adults. Biol Psychiatry. 2018;84:345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duncan AE, Ziobrowski HN, Nicol G. The prevalence of past 12-month and lifetime DSM-IV eating disorders by BMI category in US men and women. Eur Eat Disord Rev. 2017;25:165–171. [DOI] [PubMed] [Google Scholar]
- 4.Wassenaar E, Friedman J, Mehler PS. Medical complications of binge eating disorder. Psychiatr Clin North Am. 2019;42:275–286. [DOI] [PubMed] [Google Scholar]
- 5.Linardon J. Rates of abstinence following psychological or behavioral treatments for binge-eating disorder: Meta-analysis. Int J Eat Disord. 2018;51:785–797. [DOI] [PubMed] [Google Scholar]
- 6.Tomiyama AJ. Stress and obesity. Annu Rev Psychol. 2019;70:703–718. [DOI] [PubMed] [Google Scholar]
- 7.Naish KR, Laliberte M, MacKillop J, Balodis IM. Systematic review of the effects of acute stress in binge eating disorder. Eur J Neurosci. 2019;50:2415–2429. [DOI] [PubMed] [Google Scholar]
- 8.Baum A. Stress, intrusive imagery, and chronic distress. Health Psychol. 1990;6:221–234. [DOI] [PubMed] [Google Scholar]
- 9.Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychol Bull. 2011;137:660–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91:449–458. [DOI] [PubMed] [Google Scholar]
- 11.Newman E, O’Connor DB, Conner M. Daily hassles and eating behaviour: The role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32:125–132. [DOI] [PubMed] [Google Scholar]
- 12.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23:887–894. [DOI] [PubMed] [Google Scholar]
- 13.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. [DOI] [PubMed] [Google Scholar]
- 14.Mason TB, Lavender JM, Wonderlich SA, et al. Examining a momentary mediation model of appearance-related stress, anxiety, and eating disorder behaviors in adult anorexia nervosa. Eat Weight Disord. 2018;23:637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smyth JM, Wonderlich SA, Sliwinski MJ, et al. Ecological momentary assessment of affect, stress, and binge-purge behaviors: Day of week and time of day effects in the natural environment. Int J Eat Disord. 2009;42:429–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smyth JM, Wonderlich SA, Heron KE, et al. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. 2007;75:629–638. [DOI] [PubMed] [Google Scholar]
- 17.Fischer S, Breithaupt L, Wonderlich J, et al. Impact of the neural correlates of stress and cue reactivity on stress related binge eating in the natural environment. J Psychiatr Res. 2017;92:15–23. [DOI] [PubMed] [Google Scholar]
- 18.Goldschmidt AB, Wonderlich SA, Crosby RD, et al. Ecological momentary assessment of stressful events and negative affect in bulimia nervosa. J Consult Clin Psychol. 2014;82:30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldschmidt AB, Crosby RD, Cao L, et al. Ecological momentary assessment of eating episodes in obese adults. Psychosom Med. 2014;76:747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smyth JM, Sliwinski MJ, Zawadzki MJ, et al. Everyday stress response targets in the science of behavior change. Behav Res Ther. 2018;101:20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Almeida DM, Marcusson-Clavertz D, Conroy DE, et al. Everyday stress components and physical activity: Examining reactivity, recovery and pileup. J Behav Med. 2020;43:108–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klatzkin RR, Gaffney S, Cyrus K, Bigus E, Brownley KA. Stress-induced eating in women with binge-eating disorder and obesity. Biol Psychol. 2018;131:96–106. [DOI] [PubMed] [Google Scholar]
- 23.Leslie M, Turton R, Burgess E, Nazar BP, Treasure J. Testing the addictive appetite model of binge eating: The importance of craving, coping, and reward enhancement. Eur Eat Disord Rev. 2018;26:541–550. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell JE. Medical comorbidity and medical complications associated with binge-eating disorder. Int J Eat Disord. 2016;49:319–323. [DOI] [PubMed] [Google Scholar]
- 25.Leehr EJ, Krohmer K, Schag K, et al. Emotion regulation model in binge eating disorder and obesity—A systematic review. Neurosci Biobehav Rev. 2015;49:125–134. [DOI] [PubMed] [Google Scholar]
- 26.Wonderlich SA, Peterson CB, Smith TL.. Integrative Cognitive—Affective Therapy for Bulimia Nervosa: A Treatment Manual. Guilford Publications. New York, NY: Guilford Publications; 2015. [Google Scholar]
- 27.Fairburn CG.Overcoming Binge Eating. New York, NY: Guilford Press; 2013. [Google Scholar]
- 28.Peterson CB, Engel SG, Crosby RD, et al. Comparing integrative cognitive-affective therapy and guided self-help cognitive-behavioral therapy to treat binge-eating disorder using standard and naturalistic momentary outcome measures: A randomized controlled trial. Int J Eat Disord. 2020. doi: 10.1002/eat.23324 [DOI] [PubMed] [Google Scholar]
- 29.First MB, Spitzer RL, Gibbon M, Williams J.. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P). New York, NY: Biometrics Research Development, New York State Psychiatric Institute; 1996. [Google Scholar]
- 30.Fairburn CG, Beglin SJ. Eating disorder examination questionnaire (6.0). In: Fairburn CG, ed. Cognitive Behavior Therapy and Eating Disorders. New York, NY: Guilford Press; 2008. [Google Scholar]
- 31.Hu FB, Goldberg J, Hedeker D, Flay BR, Pentz MA. Comparison of population-averaged and subject-specific approaches for analyzing repeated binary outcomes. Am J Epidemiol. 1998;147:694–703. [DOI] [PubMed] [Google Scholar]
- 32.McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann NY Acad Sci. 1998;840:33–44. [DOI] [PubMed] [Google Scholar]
- 33.Peters A, McEwen BS. Stress habituation, body shape and cardiovascular mortality. Neurosci Biobehav Rev. 2015;56:139–150. [DOI] [PubMed] [Google Scholar]
- 34.Burgess EE, Turan B, Lokken KL, Morse A, Boggiano MM. Profiling motives behind hedonic eating. Preliminary validation of the Palatable Eating Motives Scale. Appetite. 2014;72:66–72. [DOI] [PubMed] [Google Scholar]
- 35.Wonderlich JA, Lavender JM, Wonderlich SA, et al. Examining convergence of retrospective and ecological momentary assessment measures of negative affect and eating disorder behaviors. Int J Eat Disord. 2015;48:305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nahum-Shani I, Hekler EB, Spruijt-Metz D. Building health behavior models to guide the development of just-in-time adaptive interventions: A pragmatic framework. Health Psychol. 2015;34S:1209–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]