Abstract
Iron deficiency anemia (IDA) can cause left ventricular (LV) dysfunction, causing heart failure. A 48-year-old woman with severe IDA developed congestive heart failure that was properly diagnosed, managed, and followed with multiple imaging modalities to explore potential mechanisms, highlighting the reversibility of LV function in unique cardiomyopathy. (Level of Difficulty: Intermediate.)
Key Words: cardiac magnetic resonance, cardiomyopathy, iron deficiency anemia, positron emission tomography
Abbreviations and Acronyms: 18F-FDG, 18F-fluorodeoxyglucose; CMR, cardiac magnetic resonance; HF, heart failure; IDA, iron deficiency anemia; LV, left ventricular; NT-proBNP, N-terminal pro–B-type natriuretic peptide; PET/CT, positron emission tomography/computed tomography
Graphical abstract
Iron deficiency anemia (IDA) can cause left ventricular (LV) dysfunction, causing heart failure. A 48-year-old woman with severe IDA developed congestive…
Severe iron deficiency anemia (IDA) has been reported to play a pivotal role in the development of heart failure (HF) through left ventricular (LV) dysfunction and myocardial damage, and substantial clinical benefits have been found as a result of iron deficiency treatment even without anemia (1). A remarkable feature of IDA-induced HF may be the reversibility of LV dysfunction with appropriate treatment. However, the pathogenesis of cardiomyopathy associated with IDA is unknown due to the limited number of affected patients. Here, we report an impressive case with severe IDA causing LV dysfunction and congestive HF, which was appropriately diagnosed and managed. The patient was followed up with multiple imaging modalities exploring the potential mechanisms of IDA-induced HF in terms of myocardial tissue characteristics and myocardial blood flow.
Learning Objectives
-
•
IDA-induced cardiomyopathy can be characterized by severe chronic anemia, significant microvascular dysfunction, and high-output HF, which is reversible if treated properly.
-
•
Multi-imaging modalities such as transthoracic echocardiography, CMR, coronary angiography with hemodynamics measurements, and cardiac positron emission tomography can improve accurate diagnosis and appropriate management.
History of Presentation
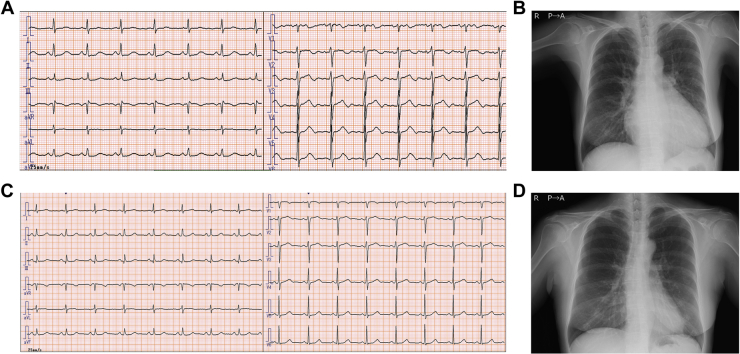
A 48-year-old woman presented with chronic leg edema and worsening exertional dyspnea. She also complained of menorrhagia with irregular periods more than 6 months ago. Vital sign measurements showed blood pressure of 107/48 mm Hg, heart rate of 81 beats/min, SpO2 of 94% (room), and temperature of 36.9°C. Physical examination revealed marked pallor of the skin and conjunctiva, jugular vein distention, crackles in both lungs, rapid regular heart rhythm without any murmur, palpable spleen, and pitting edema of both lower extremities. Electrocardiogram showed normal sinus rhythm with horizontal ST depression in the limb leads (Figure 1A). Chest radiography revealed marked cardiomegaly and mild pulmonary congestion (Figure 1B). The initial hemoglobin level was 1.7 g/l, hematocrit level was 7.2%, and mean corpuscular volume was 55 fl. Iron parameters suggested severe IDA with an iron level of 8 μg/dl, total iron-binding capacity of 468 μg/dl, and ferritin level of 2 ng/ml. The rest of the blood test results and coagulation times, along with other laboratory tests, including clinical chemistry, renal, liver, and thyroid function, were normal except for an elevated level of N-terminal pro–B-type natriuretic peptide (NT-proBNP) (1,547 pg/ml). Stool guaiac tests were negative. The patient received three units of packed red blood cells in 4 days and was admitted for evaluation and treatment of severe IDA and HF.
Figure 1.
Electrocardiogram and Chest X-Ray on Admission and at 4-Month Follow-Up
Electrocardiogram on admission (A) and at the 4-month follow-up (C). Initial (B) and 4-month follow-up (D) chest x-rays.
Past Medical History
The patient’s medical history was unremarkable except for that she regularly smoked tobacco and consumed alcohol.
Differential Diagnoses
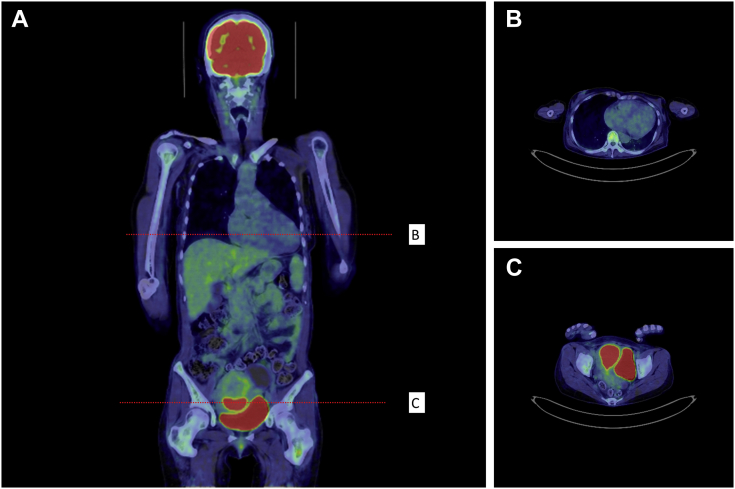
The patient showed high-output HF with a high cardiac index and low systemic vascular resistance. Chronic high-output HF was explained by severe anemia after excluding other common causes, such as obesity, thyroid disease, arteriovenous shunts, and lung and liver diseases. By characterizing myocardial tissue, cardiac magnetic resonance (CMR) helped to distinguish secondary etiologies, such as myocarditis, amyloidosis, sarcoidosis, noncompaction cardiomyopathy, and dilated phase hypertrophic cardiomyopathy. 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) was useful in excluding myocarditis and sarcoidosis. Last, her benign clinical course, which was shortly controlled with iron replacement and transfusion of packed red blood cells, was more suggestive of HF due to severe IDA.
Investigations
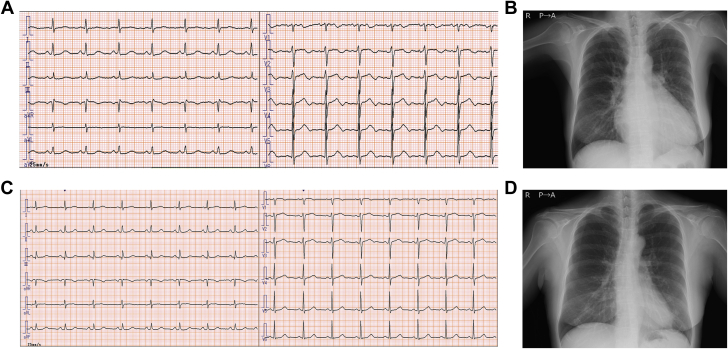
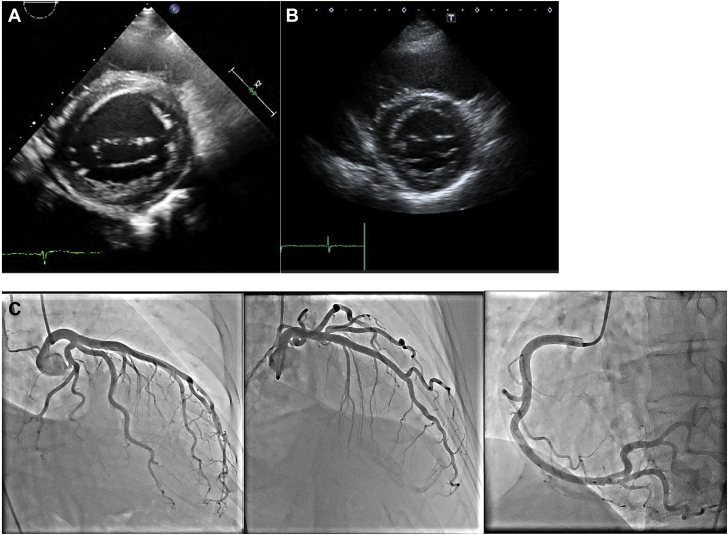
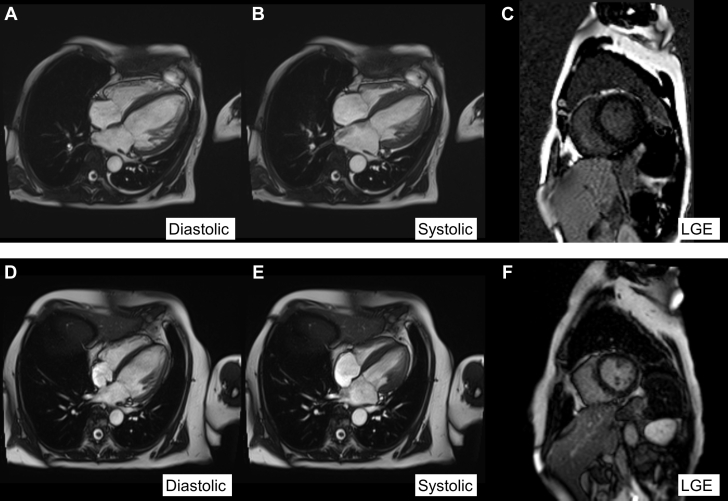
Initial transthoracic echocardiography showed a massively dilated LV chamber and left atrium with eccentric LV hypertrophy and trivial pericardial effusion (Figures 2A and 2B). On the seventh hospital day, coronary angiography (Figure 2C) revealed nonobstructive coronary arteries, and pressure studies were performed to assess LV end-diastolic pressure (9 mm Hg) and mean pulmonary capillary wedge pressures (9 mm Hg) with increased cardiac output at 9.0 l/min and systemic vascular resistance at 691 dynes/s/cm−5. Endomyocardial biopsy was avoided to prevent bleeding complications. CMR demonstrated biventricular dilatation and diffusely reduced LV wall motion with preserved wall thickness and absence of late gadolinium enhancement (Figures 3A to 3C). On day 12, PET/CT with 13N-ammonia (Figures 4A to 4C) demonstrated that ATP-induced stress myocardial blood flow was globally low with a considerable drop in the global coronary flow reserve to 1.70. Moreover, 18F-FDG-PET/CT detected abnormally high 18F-FDG uptake in the uterus with no metastases (Figure 5). Finally, the patient was referred to our obstetrics and gynecology department where the solid mass in her uterus was diagnosed as endometrioid cancer on histology.
Figure 2.
Initial and Follow-Up TTE and Coronary Angiography
Initial transthoracic echocardiogram (TTE) (A) exhibiting biventricular dilatation with preserved left ventricular (LV) wall thickness on a short-axis view compared with the 4-month follow-up TTE (B), which displayed a significant reduction in LV size and an improvement in LV contractility. LV end-diastolic diameter, LV ejection fraction, and stroke volume measured using Doppler ultrasound changed from 72 mm, 50%, and 103 ml, respectively, to 53 mm, 68%, and 67 ml, respectively, over 4 months. Coronary angiography (C) revealed no obstructive coronary disease.
Figure 3.
Cine-CMR Images in Long- and Short-Axis Views
Cine-cardiac magnetic resonance (CMR) images in long-axis ([A] diastolic and [B] systolic phases) and short-axis views with late gadolinium enhancement imaging (C). CMR studies at the 4-month visit were repeated with the corresponding images (D to F). Concentric left ventricular (LV) hypertrophy and biventricular enlargement were visible with a reduced LV ejection fraction of 32%, which improved to 47% over 4 months with a significant drop in the LV end-diastolic volume from 184 to 96 ml. Late gadolinium enhancement was not present over the entire myocardium at both the acute (C) and follow-up phases (F).
Figure 4.
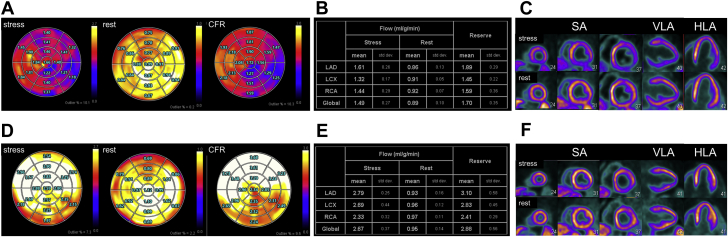
Perfusion Imaging and Myocardial Blood Flow Quantifications Using 13N-Ammonia PET in Acute Phase and at 4-Month Follow-Up
ATP-induced stress/rest 13N-ammonia positron emission tomography (PET) quantified the rest/stress myocardial blood flow (MBF) and coronary flow reserve (CFR) (A) with coronary territories (B) and myocardial perfusion imaging (MPI). (C) Both stress MBF and CFR were globally reduced at baseline and improved dramatically over the next 4 months to within normal ranges with the global CFR increasing from 1.70 to 2.88 (D and E). The MPI study demonstrated the involvement of the anterolateral and inferior walls with reversible myocardial ischemia, which significantly declined in size at follow-up (F). HLA = horizontal long-axis; LAD = left anterior descending; LCX = left circumflex; RCA = right coronary artery; SA = short-axis; VLA = vertical long-axis.
Figure 5.
Whole Body FDG-PET/CT Images
Fluorodeoxyglucose (FDG)-positron emission tomography (PET) (A) dedicated cardiac and whole-body imaging with a high-fat, low-carbohydrate, protein-preferred diet in the fasting state revealed no focal FDG uptake in the myocardium (B). Abnormally high FDG uptake was detected in the uterus with no metastatic sites (C).
Management
Frusemide and enalapril were commenced, and the patient was gradually weaned from supplemental oxygen. After the blood transfusion, she was treated with 7-day intravenous saccharated ferric oxide, followed by oral sulfate. At 3 weeks after discharge, she underwent a total hysterectomy with bilateral salpingo-oophorectomy at a university hospital; endometrial carcinoma was confirmed on pathological examination. At the 4-month follow-up visit, she was free of symptoms, where ST changes on electrocardiogram were normal with a normal cardiac silhouette on the chest radiograph (Figures 1C and 1D). Her LV ejection fraction improved to 69%, and LV diastolic dimension was still enlarged (54 mm) with a mildly elevated LV mass index of 111 g/m2 (Figure 2B). Serum hemoglobin, iron, ferritin, and NT-proBNP levels were within the normal range. Repeated CMR demonstrated that biventricular dilatation improved along with global LV wall motion, and late gadolinium enhancement was absent throughout the entire myocardium (Figures 3D to 3F). Perfusion PET/CT revealed a total recovery of global coronary flow reserve from 1.70 to 2.88 (Figures 4D to 4F).
Discussion
We report a case of a middle-aged woman with chronic severe anemia and iron deficiency. We utilized novel imaging modalities to elucidate the potential mechanisms causing unique HF. Not only can progressive HF cause iron deficiency, but the converse can also occur. Iron deficiency can promote the remodeling of cardiomyocytes (2). Iron has roles beyond oxygen transport, including in the normal activity of key enzymes of the citric acid cycle and reactive oxygen species scavenging enzymes. Decreased levels of reactive oxygen species scavenging enzymes in myocardial iron deficiency may intensify local oxidative stress, causing myocardial damage (3). As noted earlier, compromised oxygen delivery capacity may cause chronic tissue hypoxemia, which can lead to cardiomyocyte dysfunction. In our case, the initial perfusion PET/CT revealed significant microvascular dysfunction that may reflect global myocyte dysfunction. Moreover, IDA-induced cardiomyopathy had no association with myocardial inflammation, as shown by 18F-FDG-PET/CT.
A further remarkable aspect of the present case is the reversibility of IDA-induced cardiomyopathy confirmed with several imaging modalities. At the 4-month follow-up, when the patient was asymptomatic and her hemoglobin, iron, and NT-proBNP levels were normalized, we found remarkable improvements in cardiac function parameters assessed by transthoracic echocardiography, CMR, and perfusion PET/CT. This strongly suggests that IDA-induced cardiomyopathy may be almost completely reversible. However, it remains unclear whether complete normalization of LV function occurs in severe cases. Our present case showed that the LV remained slightly dilated after HF improvement, and these findings were in line with cardiac indexes measured by CMR imaging. Close observation to evaluate longer-term cardiac function and prognosis is warranted.
Follow-Up
The patient continues to take enalapril. LV function by follow-up echocardiography and hemoglobin level are within normal ranges 12 months after hospitalization.
Conclusions
To our knowledge, this is the first case of severe IDA leading to LV dysfunction and congestive HF that was properly diagnosed, managed, and followed with multiple imaging modalities to explore the potential mechanisms. This case supports the reversibility of IDA-induced cardiomyopathy if treated properly, but further research is required to determine the level of improvement.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Grote Beverborg N., van Veldhuisen D.J., van der Meer P. Anemia in heart failure: still relevant? J Am Coll Cardiol HF. 2018;6:201–208. doi: 10.1016/j.jchf.2017.08.023. [DOI] [PubMed] [Google Scholar]
- 2.Jankowska E.A., Ponikowski P. Molecular changes in myocardium in the course of anemia or iron deficiency. Heart Fail Clin. 2010;6:295–304. doi: 10.1016/j.hfc.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Dai D.F., Johnson S.C., Villarin J.J. Mitochondrial oxidative stress mediates angiotensin II-induced cardiac hypertrophy and Galphaq overexpression-induced heart failure. Circ Res. 2011;108:837–846. doi: 10.1161/CIRCRESAHA.110.232306. [DOI] [PMC free article] [PubMed] [Google Scholar]