Abstract
Moderate/severe calcification, present in approximately one-third of culprit lesions in acute coronary syndromes (ACS), portends unfavorable procedural and post-primary percutaneous coronary intervention outcomes. Intravascular lithotripsy is a novel technique using shockwaves to fracture calcific plaques. Presenting a clinical case, we enumerate efficacy and safety parameters in using intravascular lithotripsy in ACS. (Level of Difficulty: Advanced.)
Key Words: acute coronary syndromes, intravascular lithotripsy, percutaneous coronary intervention, plaque calcification
Abbreviations and Acronyms: ACS, acute coronary syndromes; IVL, intravascular lithotripsy; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction
Graphical abstract
Moderate/severe calcification, present in approximately one-third of culprit lesions in acute coronary syndromes (ACS), portends unfavorable…
Moderate/severe calcification, present in approximately 30% of culprit lesions in acute coronary syndromes (ACS) (1), adversely affects safety/efficacy of primary percutaneous coronary intervention (PCI) and portends worse post-PCI outcomes (1). Although atherectomy is contraindicated in thrombotic coronary lesions, intravascular lithotripsy (IVL) may mitigate the adverse consequences of severe calcification (2). IVL, however, has not been tested in ACS and DISRUPT-CADIII trial (Disrupt CAD III With the Shockwave Coronary IVL System; NCT03595176), designed for premarketing approval of coronary IVL, has excluded patients with ACS.
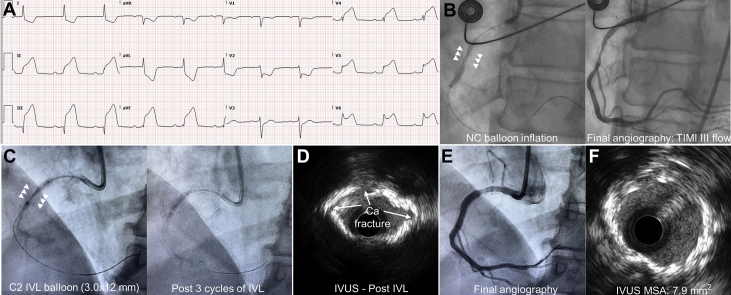
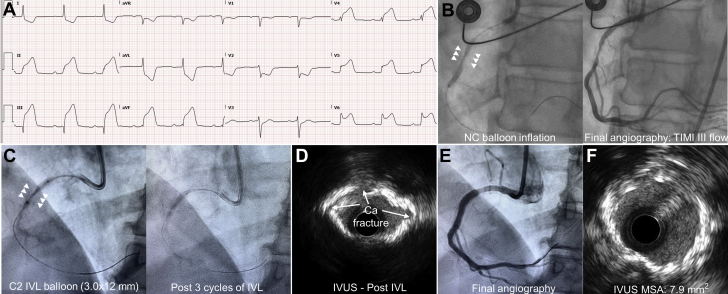
An alternative approach for PCI on severely calcified culprit lesions was undertaken in a 65-year-old woman with inferior ST-segment elevation myocardial infarction (STEMI) (Figure 1). IVL use was approved by the institutional review board at our institution.
Figure 1.
Staged Intravascular Lithotripsy-Facilitated Stent Deployment in STEMI
(A) A 65-year-old woman presented with inferior STEMI. Heart rate = 70 beats/min and blood pressure = 110/60 mm Hg. (B) High-pressure noncompliant balloon inflation failed to dilate the severely calcified culprit lesion (arrowheads). TIMI flow grade 3 was achieved, and stenting was deferred. (C) At a staged procedure, a 3 × 12-mm IVL balloon was inflated (4 atm) and 3 cycles of IVL delivered. Post-IVL, full balloon inflation was noted. (D) Post-IVL IVUS revealed multiple fractures in the concentric calcification (arrows). (E) A 3 × 23-mm drug-eluting stent was implanted and post-dilated with a 3.5 × 20-mm noncompliant balloon (at 22 atm). Final angiography revealed optimal stent expansion and TIMI flow grade 3. (F) IVUS MSA = 7.9 mm2. No slow-flow/no-reflow, arrhythmia, or hemodynamic compromise were noted during the staged procedure. Ca = calcium; IVL = intravascular lithotripsy; IVUS = intravascular ultrasound; MSA = minimal stent area; NC = noncompliant; TIMI = Thrombolysis In Myocardial Infarction.
Safety of IVL in thrombus-laden lesions is unknown. Insonification of platelet/fibrin-rich thrombi by shockwaves may result in thrombus degradation/embolization. Shockwaves can induce myocardial depolarization (2). Although an R-on-T phenomenon inducing tachyarrhythmia has not been substantiated in stable coronary lesions (2), such a risk in electrically excitable myocardium during early reperfusion is unknown. Thus, “off-label” IVL use in acute STEMI is not recommended.
We propose that IVL can be used in staged stenting procedure during which thrombus burden and myocardial electrical instability may be substantially less. This approach is supported by the DEFER-STEMI (Deferred Stent Trial in STEMI), in which deferring stent implantation in STEMI resulted in reduced no-reflow and increased myocardial salvage, with approximately 4% needing urgent PCI before the staged procedure (3).
Footnotes
Dr. Patel has received educational grants from Abbott Vascular and Novartis; and consultancy fees from Abbott Vascular, Novartis, and Aspen. Dr. Madhavan has received an institutional grant from the National Institutes of Health/National Heart, Lung, and Blood Institute to Columbia University Irving Medical Center (T32 HL007854). Dr. Figtree has received consultancy fees from Janssen and CSL. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
References
- 1.Genereux P., Madhavan M.V., Mintz G.S. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI and ACUITY TRIALS. J Am Coll Cardiol. 2014;63:1845–1854. doi: 10.1016/j.jacc.2014.01.034. [DOI] [PubMed] [Google Scholar]
- 2.Karimi Galougahi K., Patel S., Shlofmitz R.A. Calcific plaque modification by acoustic shockwaves: intravascular lithotripsy in coronary interventions. Circ Cardiovasc Interv. 2020 doi: 10.1161/CIRCINTERVENTIONS.120.009354. In press. [DOI] [PubMed] [Google Scholar]
- 3.Carrick D., Oldroyd K.G., McEntegart M. A randomized trial of deferred stenting versus immediate stenting to prevent no- or slow-reflow in acute ST-segment elevation myocardial infarction (DEFER-STEMI) J Am Coll Cardiol. 2014;63:2088–2098. doi: 10.1016/j.jacc.2014.02.530. [DOI] [PMC free article] [PubMed] [Google Scholar]