Abstract
Background:
Coronavirus disease is a highly transmittable and pathogenic viral infection caused by severe acute respiratory syndrome coronavirus 2, which poses therapeutic dilemmas. Some suggestions for drug treatment seem problematic. Beliefs about the causes of health problems are determinants of treatment seeking decisions. Hence, one of the alternatives for the solution of health problems is employing traditional medicine to prevent coronavirus disease 19.
Objective:
To assess the knowledge, attitude, and utilization of drugs toward the coronavirus disease 19 pandemic among Bale zone residents.
Methods:
Community-based cross-sectional study was conducted among the Bale Zone population from May 30 to June 30, 2020. Eight hundred fifty-four participants were selected using a single population formula, and a multistage sampling technique was employed. Data were analyzed using SPSS version 25.0. Descriptive and binary logistic regression was used to analyze the outcomes. A p value ⩽ 0.05 was considered statistically significant.
Results:
Out of the total 854 respondents, about 534 (62.5%) got information about coronavirus disease 19 from TV/radio. More than two-thirds (71.9%) of the respondents have known that severe acute respiratory syndrome coronavirus 2 has no curative drugs, and 65.4% had a more appropriate attitude toward overall drug use in coronavirus disease 19. Level of education and, attitude towards drug use were singnificantly associated with knowledge of drugs, source of information about coronavirus disease 19 and having good practice were significantly associated with atittude toward drug utilization.
Conclusion:
One out of two study participants have good knowledge regarding drugs to the coronavirus disease 19 pandemic. Illiterate people in the community were identified to have poor knowledge about drugs, hence community educuation program is important to improve the knowledge about drugs towards the coronavirus disease 19 pandemic.
Keywords: COVID-19, drugs, modern medicine, traditional medicine, Bale zone
Introduction
Coronavirus disease 19 (COVID-19) is a highly transmittable and pathogenic viral infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 was first reported in Wuhan, the capital of Hubei, China. The etiological agent of COVID-19 has been confirmed as a novel coronavirus, now known as SARS-CoV-2. Within a few months of the first report, COVID-19 had spread across China and worldwide, reaching a pandemic level.1,2
The World Health Organization (WHO) also declared a global emergency on January 31, 2019, due to increasing concerns over its fast spread, and on 11 March, the disease was recognized as a pandemic. Since the base for the pathogenesis of this virus and its proliferation are unclear, there is still no definitive treatment against the virus. Thus, the medications used against SARS-CoV-2 are mainly based on their effectiveness against earlier strains of coronavirus, SARS-CoV, and Middle East respiratory syndrome coronavirus (MERS-CoV). 3
Many medicinal plants were in use as early as 5000–4000 BC in China, and 1600 BC by Syrians, Babylonians, Hebrews, and Egyptians.4,5 Studies indicate that 25% of modern medicines are derived from the extracts of medicinal plants. 6 About 80% of Ethiopian people rely on traditional medicine to meet their healthcare needs which could be attributed to cultural acceptability, perceived efficacy against certain types of diseases, physical accessibility, and affordability compared to modern medicine. 7
The COVID 19 pandemic is causing substantial stress on the health care system of all countries in the world. It is observed that early interventions with optimal political commitment and community mobilization help to flatten the curve averting the occurrence of many cases and deaths.8,9
According to the WHO report, around 176,113,245 confirmed cases and 3,802,238 confirmed deaths occur worldwide. 10 Ethiopia is one of those countries which face the disease burden, up to date, 273,678 confirmed cases and 4231 deaths. 9 COVID-19, which is caused by the single-stranded RNA coronavirus SARS-CoV-2, poses therapeutic dilemmas. They include various antiviral drugs, some of which have primary targets that are DNA viruses, not RNA; immunomodulatory drugs, which may suppress potentially protective acute inflammatory responses and do not specifically, target the virus. 11
The antimalarial drugs chloroquine (CQ) and hydroxychloroquine (HCQ), which have some antiviral activity in vitro but no evidence of clinical benefit in human viral infections and corticosteroids, which may be harmful when used to treat infection related to SARS-CoV-1. 12 Currently, the US Food and Drug Administration (FDA) declares the toxicities associated with these drugs.
The high mortality rate, economic and social crisis, and lack of definitive treatment for the COVID-19 management navigate the community to use different informally heard modern medications by themselves. The use of complementary and alternative medicines, as well as social drug practices like drinking alcohol, is exercised by the community.
Therefore, this study is conducted in communities living at the bottom and around of the National Park of Bale Mountain, in which many medicinal plants and known traditional healers are found around. Thus, society may easily exercise crude traditional medicines for COVID-19. As much as our knowledge is concerned, there is no community-based survey conducted in the country regarding the knowledge, attitude, and utilization of drugs toward the COVID-19 pandemic. Therefore, this study is important to assess the knowledge, attitude, and utilization of modern medications, traditional medicine, and social drugs in the community with the COVID-19 pandemic.
Methods and materials
Study area and period
This study was conducted in two Bale zones, Southeast Ethiopia. These zones are found at 430 km far away from Addis Ababa, the capital city of Ethiopia. The topography is composed of 14.92% highland, 21.53% midland, and 63.55% lowland with an altitude of 300–4377 m and annual rainfall of 900–1400 mm. The main sources of food include cereal crops, fruit, vegetable, and animal products. According to the 2018 zonal report, they have a total population of around 1.9 million. There are 398,240 households. Regarding health facilities, there are 6 hospitals, 90 health centers, and 323 health posts. The study was conducted from 30 May 2020 to 30 June 2020.
Study design and population
A community-based cross-sectional study was carried out. All adult populations living in randomly selected kebeles during the study period and who were eligible for the study were included.
Inclusion criteria
Individuals who were considered eligible for participation were those who have provided written consent and age greater than or equal to 18 years old. Those who are critically ill and psychiatric participants were excluded.
Sample size determination and procedure
The sample size was calculated by employing a single population proportion formula for sample size determination by taking a 50% proportion of people with high-risk perception against COVID-19, assuming a 95% confidence level, 5% margin of error, 10% non-respondents, and a design effect of two. This gives the final sample size of 854 individuals.
The sample size was determined by the formula:
where n is the sample size, p = 50%, d is the marginal error = 5%, and z = at 95% confidence interval = 1.96.
Therefore, n = z2 (1–p)(p)/d2 = (1.96)2(0.5)(.5)/ (0.05)2 n = 768.
After adding 10% of the non-respondent rate, the overall sample size was 854. A multistage sampling technique was employed. First, woredas were grouped based on climate characteristics. Five woredas and one administrative town from each group of woredas by climatic conditions and one administrative town were selected randomly. Then 22 kebeles were selected randomly from selected administrative towns and woredas. Following this, households were selected systematically after marking houses. One participant from each selected household was selected randomly.
Study variables
Knowledge, attitude, and utilization were dependent variables, whereas socio-demographic characteristics like age, sex, residence, monthly income, history of smoking, chewing khat, and alcohol consumption.
Operational definitions
Knowledge scores were calculated by asking seven different questions on knowledge and by coding the response as 1 for a correct answer and 0 for an incorrect answer. Then by summing the entire values, the respondent who scored mean and above the mean was labeled as having good knowledge.
Utilization (practice): respondents who scored points at mean and above for utilization questions were labeled as good practice.
Attitude: respondents who scored points at mean and above for attitude questions were labeled as positive attitude, otherwise negative attitude.
Drugs: any chemical substance which includes modern medicines, traditional medicine, and social substances used for the prevention and or treatment of COVID-19.
Traditional medicines: alternative medicines or any herbal medicine used by the community for the prophylaxis or treatment of COVID-19.
Modern medicine: any drug/group of drugs scientifically studied and used for COVID-19.
Data collection instruments and quality control
Based on the related literature search, the structured study questionnaire was adapted from validated surveys that were previously used and tailored to suit the local population and the pandemic nature of the disease.5,7,13,14 To assure its applicability, the features and content validity of the adapted questionnaire were established by researchers.
Data were collected by three BSc research assistants supervised by the principal investigator.
The questionnaire comprised four sections: socio-demographic characteristics of respondents and sections on each of the knowledge, attitudes, and utilization of drugs related to COVID-19. Knowledge correlated with 7, yes, no, and do not know questions toward the drug used during the COVID-19 pandemic. Attitude-related 6 Likert-type scale questions (strongly disagree = 1, strongly agree = 5) toward drugs used during the COVID-19 pandemic. About the utilization of drugs during the COVID-19 pandemic period, standardized 7 Yes–No questions were developed (suplimentary file).
The questionnaire was prepared in English and then translated into local languages. Translation back to English was done to check for consistency by language experts. Before the actual data collection, questionnaires were pretested on 5% of the original sample size subjects who were not included in the study before actual data collection. The questionnaire was modified based on pretest results. The collected data were first being checked and cleaned for completeness.
Statistical analysis
Manual checkup of the data was performed for its completeness as well as its clarity, coding, and entry into Epi Data version 3.1 and statistical package for the social sciences (SPSS) version 25.0 for Windows. For the analysis of logistic regression, “I do not know” and “no” responses of knowledge were combined and considered as poor knowledge. The Likert-type scale was used to measure attitude. Questions for which the respondents gave correct responses were counted and scored. Then this score was pooled together, and the mean score was computed to determine the overall attitude of the respondents; respondents who were scored greater than or equal to the mean value were grouped as having a positive attitude and those who scored less than the mean value was considered to have a negative attitude. Results were presented using simple frequencies with percentages in appropriate tables to display the descriptive part of the result. Logistic regression analysis was conducted to identify demographic factors associated with knowledge and attitudes. Finally, frequencies, percentages, and tables were used to summarize the characteristics of the study participants. P value less than 0.05% and 95% confidence interval was taken as statistically significant.
Result
Socio-demographic characteristics of study participants
Of 854 respondents participated in this study, yielding a 100% response rate. Out of the total 854 respondents, 547 (64.1%) were male and 845 (98.9%) were Oromo, with 611 (71.5%) living in rural. Accordingly, 499 (58.4%) were farmers, 660 (77.3%) were fathers/mothers, and about 335 (39.2%) have attended primary education. Concerning their marital and monthly income status, 645 (75.5%) were married, earning a median monthly income of 1675.27 ETB. Around two-thirds of the respondents, 534 (62.5%) got information about COVID-19 from TV/radio, 591 (69.2%) of them live near to a health facility and 265 (30.8%) have a history of substance use mostly khat 228 (26.7%) and 100 (11.7%) have a history of chronic illness. Finally, more than two-thirds of the total participants 604 (70.7%) live in their own house (Table 1).
Table 1.
Socio-demographic characteristics of study participants in Bale zones communities, Southeast Ethiopia (n = 854).
| Variables | Frequency (n) | Proportion (%) |
|---|---|---|
| Gender Male | 547 | 64.1 |
| Female | 307 | 35.9 |
| Age in years Mean | 34.12 | |
| Standard deviation | 13.29 | |
| Minimum | 18 | |
| Maximum | 90 | |
| Ethnicity Oromo | 845 | 98.9 |
| Amhara | 4 | 0.5 |
| Tigre | 3 | 0.4 |
| Others | 2 | 0.2 |
| Residence Rural | 611 | 71.5 |
| Urban | 243 | 28.5 |
| Occupation Government workers | 113 | 13.2 |
| NGO employee | 7 | 0.8 |
| Private workers | 161 | 18.9 |
| Farmers | 499 | 58.4 |
| Others | 74 | 8.7 |
| Role in family Father/mother | 660 | 77.3 |
| Son | 143 | 16.7 |
| Daughter | 51 | 6 |
| Level of education No formal education | 213 | 24.9 |
| Primary education (1–8) | 335 | 39.2 |
| Secondary education (9–12) | 178 | 20.8 |
| College and above (12 +) | 128 | 15 |
| Marital status Married | 645 | 75.5 |
| Single | 183 | 21.4 |
| Divorced | 24 | 2.8 |
| Others | 2 | 0.2 |
| Monthly income ETB Median | 1675.27 | |
| Minimum | 10 | |
| Maximum | 50,000 | |
| Source of information religious leaders | 157 | 18.4 |
| TV/radio | 534 | 62.5 |
| Social media | 285 | 33.4 |
| Health workers | 55 | 6.4 |
| Gov’t announcements | 74 | 8.7 |
| Other source (like telecom) | 1 | 0.1 |
| Distance from health facility | ||
| Near health facility | 591 | 69.2 |
| Long distance > 1 h | 256 | 30 |
| Don’t know | 7 | 0.8 |
| Substance use No | 589 | 69 |
| Yes | 265 | 31 |
| Types of substance used Khat | 228 | 26.7 |
| Cigarettes smoking | 33 | 3.9 |
| Alcohol drinking | 28 | 3.3 |
| Other substance | 1 | 0.1 |
| History of chronic illness No | 754 | 88.3 |
| Yes | 100 | 11.7 |
| House ownership No | 250 | 29.3 |
| Yes | 604 | 70.7 |
Knowledge, attitude, and utilization of drugs toward COVID-19
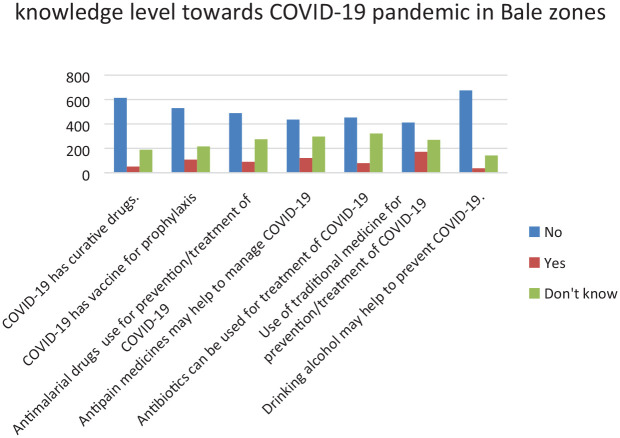
In general, about half (50.6%) of the respondents have good knowledge regarding the overall drug usage in COVID-19. More than two-thirds (71.9%) of the respondents have known that the coronavirus has no curative drugs. Nearly two-thirds (62.1%) of the respondents realize that SARS-COV-2 has no vaccine. Regarding the antimalarial drugs, more than half of the respondents (57.3%) have appropriately responded that antimalarial drugs are not used for prevention or curative treatment of SARS-COV-2. Nearly half of this survey participant responded that antibiotics usage does not have a protective or treatment effect for COVID-19. About half of the respondents (51.8%) had negative responses to the benefit of traditional medicine for the prevention and treatment of SARS-COV-2. Most respondents (71%) have responded that drinking alcohol is not beneficial for the prevention or treatment of SARS-COV-2 (Figure 1).
Figure 1.
Response to questions related to knowledge level toward COVID-19 pandemic in Bale zones, southeast Ethiopia (n = 854).
Out of 854 study participants, 65.4% had a more appropriate attitude toward overall drug use in COVID-19. About 76.5% respondents believed that antibiotics are not used for the prevention and cure of SARS-COV-2. Most of the respondents (86.2%) were believed that taking antiretroviral drugs for the prevention or treatment of SARS-COV-2. The attitude toward the use of analgesics regarding COVID-19 was positive for most of the respondents (81.8%). According to this study, about three-fourths (74.5%) of the respondents believed that the traditional medicine used is not helpful in the prevention or management of SARS-COV-2. Out of 854 study participants, 92% (786) of them agreed that alcohol drink has no benefit for the prevention or treatment of SARS-COV-2. In this study, most of the respondents (86.1%) disagreed with the use of antimalarial drugs for the prevention or treatment of SARS-COV-2 (Table 2).
Table 2.
Response to questions related to attitude level toward COVID-19 pandemic in Bale zones, Southeast Ethiopia (n = 854).
| List of variables | Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
|---|---|---|---|---|---|
| Antibiotics can be used for prevention or treatments of COVID-19 | 183 (21.4) | 471 (55.2) | 80 (9.4) | 99 (11.6) | 21 (2.5) |
| ART can be used for prevention or treatments of COVID-19 | 245 (28.7) | 491 (57.5) | 58 (6.8) | 48 (5.6) | 12 (1.4) |
| Antipain can be used for prevention or treatments of COVID-19 | 191 (22.4) | 507 (59.4) | 55 (6.4) | 83 (9.7) | 18 (2.1) |
| Traditional medicine can be used for prevention or treatments of COVID-19 | 188 (22.0) | 448 (52.5) | 58 (6.8) | 149 (17.4) | 11 (1.3) |
| Alcohol can be used for prevention or treatments of COVID-19 | 336 (39.3) | 450 (52.7) | 33 (3.9) | 28 (3.3) | 7 (0.8) |
| Antimalarial can be used for prevention or treatments of COVID-19 | 256 (30.0) | 479 (56.1) | 63 (7.4) | 49 (5.7) | 7 (0.8) |
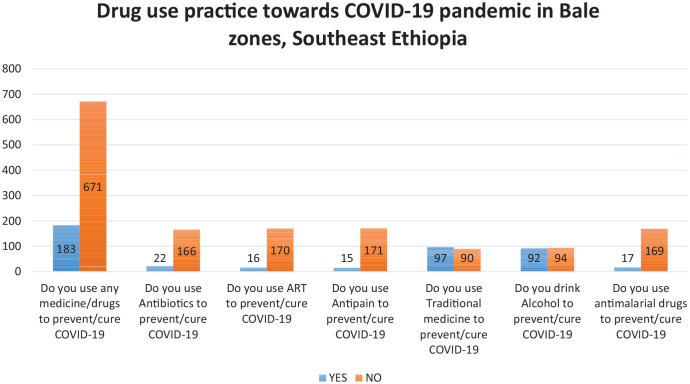
Concerning practices, the overall response of the participants regarding drugs or medicine used in association with COVID-19 was 183 (21.4%), which is regarded as inappropriate in principle. Among the respondents who reported using drugs, a larger number of participants 97 (11.4%) were using traditional medicines, followed by alcohol drink 92 (10.8%) (Figure 2).
Figure 2.
Response to questions related to drug use practice toward COVID-19 pandemic in Bale zones, Southeast Ethiopia (n = 854).
Factors associated with knowledge and attitude
Study participants with the level of education of primary school were 2.7 times more likely to have good knowledge (adjusted odds ratio (AOR) = 2.734, 95% confidence interval (CI) = (1.847–4.409)), whereas those in secondary schools were 5.467 times more likely to have good knowledge when compared to those with no formal education (AOR = 5.050, 95% CI = (3.116–8.186)). Similarly, study participants with a positive attitude about drugs toward COVID-19 were about 2.9 times more likely to have good knowledge about drugs toward COVID-19 (AOR = 2.879, 95% CI = (2.108–3.931)) (Table 3). Concerning attitude, study participants, those who got information from religious leaders and information from TV/Radio were almost four times and three times more likely to have positive attitude (AOR = 4.316, 95% CI = (1.992–9.350)) and (AOR = 2.894, 95% CI = (1.564–5.354)), respectively. Similarly, study participants with drug use practice toward COVID-19 were four times more likely to have an attitude toward drugs than their counterparts (AOR = 4.189, 95% CI = (2.061–8.516))(Table 4).
Table 3.
Multiple logistic regression analysis of the association between independent variables and knowledge toward COVID-19 pandemic in Bale zones, Southeast Ethiopia (n = 854).
| Variables | COR (95% CI) | P value | AOR (95% CI) | P value |
|---|---|---|---|---|
| Categorized age | ||||
| <25 | .002 | .634 | ||
| 25–34 | .629 (.413–.958) | .031 | .762 (.479–1.212) | .251 |
| 35–45 | .533 (.328–.866) | .011 | .903 (.519–1.572) | .718 |
| >45 | .376 (.228–.622) | .001* | .805 (.449–1.443) | .466 |
| Monthly income | ||||
| <500 | .019 | .070 | ||
| 500–1500 | .701 (.476–1.033) | .072 | .678 (.444–1.034) | .071 |
| 1500–250 | 1.136 (.742–1.738) | .558 | 1.029 (.645–1.641) | .905 |
| >2500 | 1.206 (.836–1.740) | .316 | 1.120 (.735–1.706) | .599 |
| Level of education | ||||
| No formal education | 1 | |||
| Primary school (1–8) | .208 (.130–.333) | .001* | 2.734 (1.847–4.049) | .001** |
| Secondary school (9–12) | .572 (.375–.872) | .009* | 5.050 (3.116–8.186) | .001** |
| Collage and above (12+) | 1.066 (.661–1.719) | .792 | 4.761 (2.773–8.172) | .001** |
| History of chronic illnesses | ||||
| No | ||||
| Yes | .741 (.487–1.128) | .162 | .942 (.593–1.495) | .800 |
| Place of Residence | ||||
| Rural | ||||
| Urban | .006 (1.520–1.126) | 2.052 | 1.294 (.928–1.806) | .129 |
| Attitude toward COVID-19 | ||||
| Negative attitude | ||||
| positive attitude | .000 (2.789–2.079) | 3.741 | 2.879 (2.108–3.931) | .001** |
| Constant | .229 | .001** | ||
AOR: adjusted odds ratio; CI: confidence interval; COR: crude odds ratio.
statistically significant in bivariate; **statistically significant in multivariate.
Table 4.
Multiple logistic regression analysis of the association between independent variables and attitudes toward COVID-19 pandemic in Bale zones, southeast Ethiopia (n = 854).
| Variables | COR (95% CI) | P value | AOR (95% CI) | P value |
|---|---|---|---|---|
| Information from religious leader No | ||||
| Yes | 2.166 (1.438–3.262) | .001* | 4.239 (1.963–9.154) | .001** |
| Information from radio/TV No | ||||
| Yes | 1.258 (.942–1.680) | .120 | 3.139 (1.728–5.702) | .001* |
| Alcohol drinking No | ||||
| Yes | .566 (.258–1.242) | .156 | .420 (.161–1.094) | .079 |
| Knowledge toward COVID-19 | ||||
| Poor knowledge | ||||
| Good knowledge | 2.789 (2.079–3.741) | .001* | 3.798 (2.088–6.908) | .001** |
| Drug use practice | ||||
| Poor practice | ||||
| Good practice | 2.856 (2.043–3.993) | .001* | 4.230 (2.086–8.580) | .001** |
| Constant | .121 | .001 |
AOR: adjusted odds ratio; CI: confidence interval; COR: crude odds ratio.
statistically significant in bivariate; **statistically significant in multivariate.
Discussion
In Ethiopia, this is the first study conducted to identify drug-related knowledge, attitudes, and practices of the general population toward the COVID-19 pandemic. Based on findings of this study, nearly half (50.6%) of the study participants have good knowledge toward overall drug use in COVID-19 and 65.4% had a positive attitude toward overall drug use in COVID-19. Hence, the finding of this study is in line with the study conducted in Nepal, in which about 57.9% of the study subjects were identified to have good knowledge. 15 However, it is lower than the finding of the studies conducted in China, Saudi Arabia, and Tanzania, which have identified good knowledge in 90%, 93%, and 84.4% of study participants, respectively.16–18 The variation in results can be due to the difference in study participants. Studies conducted in China involved college students, while two studies conducted in Saudi Arabia and Tanzania used an online survey that shows a difference in awareness level.
About 78.6% of the study respondents responded as the use of drugs or medicine for COVID-19 is beneficial. Similarly, 48.2% of the study subjects had positive responses to the benefits of traditional medicine for the prevention and treatment of COVID-19. The above positive responses about the importance of traditional medicine are supported by a study conducted in China during the SARS epidemic of 2003. 19 During the treatment period of COVID-19, more than 3100 medical staff of traditional Chinese medicine (TCM) were dispatched to Hubei province, and the TCM scheme was included in the guideline on the treatment of COVID-19. 20 In addition, a study conducted in Turkey revealed that the majority of participants (24%) turned to alternative therapies indicated that they got negative and wrong information about the drugs. 21 Furthermore, in China, a study conducted on herbal medicine revealed that none of the study participants who took the preventive herbal medicine had contracted SARS, and information on the safety of the herbal medicines was also not reported. 22 Based on findings of the study done in Southeast Ethiopia, traditional healers of the study area use medicinal products for the treatment of different diseases that range from painkillers to malaria and cancer. 23 From the result of our study, compared to modern and social medicine, the study participants practiced the use of traditional medicines for the prevention of COVID-19. Some of the commonly used traditional drugs and food items are listed in the table below (Table 5).
Table 5.
Traditional medicines used by the community in two Bale zones.
| Local name | Scientific name | Part used | Dosage form |
|---|---|---|---|
| Zingibilaa | Zingiber officinale | Rhizome | Solid |
| Xoosinyii | Satureja punctate | Leaf | Liquid |
| Teena Addam | Ruta chalepensis | Leaf | Liquid |
| Sinaificaa | Brassica nigra | Seed | Solid |
| Qulubbi Addi | Allium sativum | Bulb | Solid |
| Loomi | Citrus aurantifolia | Fruit | Liquid |
| Feexoo | Lepidium sativum | Seed | Solid |
| Baargamoo | Eucalpytus globulus | Leaf | Gaseous |
| Abusuudaa gurraacha | Ribes nigrum | Seed | Solid |
| Burtukaana | Citrus sinensis | Fruit | Liquid |
| Abaaboo suufii | Helianthus annus | Seed | Liquid |
| Bursaa/bursa | |||
| Habukurtoo | Persea Americana | Fruit | Liquid |
| Qaaraa | Piper nigrum | Seed | Solid |
| Damma | Honey |
Study participants who attended primary and secondary school were three to five times more likely to have good knowledge when compared to those who did not attend school (AOR = 2.734, 95% CI (1.847–4.409)), AOR = 5.050, 95% CI (3.116–8.186), respectively. Within the community, having formal education may help study participants to learn and search for information about COVID-19 by themselves.
One of the limitations of this study was the application of self-reporting methods of data collection through interviews; it is possible that respondents may over-report socially desirable behaviors or underreport socially undesirable behaviors. A further limitation is being cross-sectional nature of the data that represented one point in time and, therefore, do not reflect any changes in respondents’ knowledge, attitude, and utilization during the COVID-19 pandemic.
Conclusion
This study showed that one out of two study participants have good knowledge regarding drugs to the COVID-19 pandemic. Hence, the good knowledge they had about drugs to the COVID-19, made the study participants have positive attitudes and good practices toward drugs during the COVID-19 pandemic. Our findings suggest the need for effective and tailored community education programs aimed at improving further knowledge regarding different types of drug utilization toward the COVID-19 pandemic, thereby leading to more positive attitudes and safe drug utilization.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211034384 for Knowledge, attitude, and utilization of drugs toward COVID-19 pandemic among Bale Zone residents, Southeast Ethiopia by Ayele Mamo, Mesud M Hassen, Ahmednur Adem, Zinash Teferu, Musa Kumbi, Abduljewad Husen, Damtew Solomon, Abate Lette, Sintayew Hailu, Edao Sinba, Abdushakur M Abduletif, Jeylan Kassim, Gashaw Walle and Daniel Atlaw in SAGE Open Medicine
Acknowledgments
The authors want to express their great thanks to Madda Walabu University, Goba Referral Hospital, school of Medicine & Health Science for their support. They would like to extend their appreciation for people working with us.
Footnotes
Authors’ contributions: A.M. and M.M. were involved in developing the proposal and design of the study. A.M., M.M., A.A., Z.T., M.K., A.H., D.S., A.L., E.S., S.H., J.K., G.W., and D.A. conducted the actual study and statistical analysis and contributed to writing of the manuscript. All authors gave the final approval of the version to be published and agreed to be accountable for all aspects of the work.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The study received ethical approval from the MWU Ethical review Committee (da 22/1-27/1468/1-17)
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The data collectors and study supervisor fee were covered by Madda Walabu University.
Informed consent: Written informed consent from each participant
ORCID iDs: Ahmednur Adem  https://orcid.org/0000-0001-9087-5393
https://orcid.org/0000-0001-9087-5393
Damtew Solomon  https://orcid.org/0000-0003-4831-4992
https://orcid.org/0000-0003-4831-4992
Daniel Atlaw  https://orcid.org/0000-0002-2968-4958
https://orcid.org/0000-0002-2968-4958
Availability of data and materials: The data sets used and analyzed during this study are available from the corresponding author on reasonable request.
Supplementary file: Supplementary file for this article is available online.
References
- 1. Ahn DG, Shin HJ, Kim MH, et al. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19). J Microbiol Biotech 2020; 30(3): 313–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shereen MA, Khan S, Kazmi A, et al. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res 2020; 24: 91–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rismanbaf A. Potential treatments for COVID-19; a narrative literature review. Arch Acad Emerg Med 2020; 8(1): e29. [PMC free article] [PubMed] [Google Scholar]
- 4. Du HZ, Hou XY, Miao YH, et al. Traditional Chinese Medicine: an effective treatment for 2019 novel coronavirus pneumonia (NCP). Chin J Nat Med 2020; 18(3): 206–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berhane T, Vijaibasker G. Assessment of traditional home remedy usage among people in Harar, Ethiopia. Int J Pharmaceut Sci Res 2015; 6(6): 2451. [Google Scholar]
- 6. Tirfessa K, Belude T, Denu D. Ethnobotanical study of medicinal plants in Akaki district, East Shewa Zone, Oromia regional state, Ethiopia. J Med Plant 2017; 5(2): 353–360. [Google Scholar]
- 7. Aragaw TJ, Afework DT, Getahun KA. Assessment of knowledge, attitude, and utilization of traditional medicine among the communities of Debre Tabor Town, Amhara Regional State, North Central Ethiopia: a cross-sectional study. Evid Based Complement Alternat Med 2020; 2020: 6565131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Han SS. Where on earth is the World Heath Organization? 2020, https://works.bepress.com/sung_soo_han/100/
- 9. FMOH. National comprhensive Covid19 management hand book. In: FMOH (ed.) National Comprhensive Covid19 Management Hand Book. 1st ed. Addis Ababa, Ethiopia: Ethiopian Public Health Institute, 2020. [Google Scholar]
- 10. who.int. World Health Organisarion emergency update covid-19, 2020, https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 11. Tufan A, Avanoğlu Güler A, Matucci-Cerinic M. COVID-19, immune system response, hyperinflammation and repurposing antirheumatic drugs. Turkish J Med Sci 2020; 50(SI-1): 620–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aronson JK, Ferner RE. Drugs and the renin-angiotensin system in covid-19. BMJ 2020; 369: m1313. [DOI] [PubMed] [Google Scholar]
- 13. Nepal Anant DH, Suzanne Robinson Linda A. Knowledge, attitudes and practices relating to antibiotic use among community members of the Rupandehi District in Nepal. BMC Public Health 2019; 19: 1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rabby MII. Current drugs with potential for treatment of COVID-19: a literature review. J Pharm Pharm Sci 2020; 23(1): 58–64. [DOI] [PubMed] [Google Scholar]
- 15. Sarraf DP, Keshwar GP. Public’s knowledge and beliefs towards universal safety precautions during COVID-19 pandemic in Nepal: a web-based cross-sectional study. J Drug Deliver Therapeutic 2020; 10(3-s): 133–141. [Google Scholar]
- 16. Zhong BLLW, Luo W, Li HM, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 2020; 16(10): 1745–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Al-Hanawi MKAK, Alshareef N, Qattan AMN, et al. Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Front Public Health 2020; 8: 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rugarabamu SIM, Byanaku A. Knowledge, attitudes, and practices (KAP) towards COVID-19: a quick online cross-sectional survey among Tanzanian residents. medRxiv Preprint, 2020, https://www.medrxiv.org/content/10.1101/2020.04.26.20080820v2
- 19. Ren JL, Zhang AH, Wang XJ. Traditional Chinese medicine for COVID-19 treatment. Pharmacol Res 2020; 155: 104743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ang L, Lee HW, Choi JY, et al. Herbal medicine and pattern identification for treating COVID-19: a rapid review of guidelines. Integr Med Res 2020; 9(2): 100407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yakut S, Karagülle B, Atçalı T, et al. Knowledge, attitudes, practices and some characteristic features of people recovered from COVID-19 in Turkey. Medicina 2021; 57: 431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wabe N, Mohammed MA, Raju NJ. An ethnobotanical survey of medicinal plants in the Southeast Ethiopia used in traditional medicine. Spatula DD 2011; 1(3): 153–158. [Google Scholar]
- 23. Clay JM, Parker MO. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis. Lancet Public Health 2020; 5: e259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211034384 for Knowledge, attitude, and utilization of drugs toward COVID-19 pandemic among Bale Zone residents, Southeast Ethiopia by Ayele Mamo, Mesud M Hassen, Ahmednur Adem, Zinash Teferu, Musa Kumbi, Abduljewad Husen, Damtew Solomon, Abate Lette, Sintayew Hailu, Edao Sinba, Abdushakur M Abduletif, Jeylan Kassim, Gashaw Walle and Daniel Atlaw in SAGE Open Medicine