Abstract
Background:
The incidence of concomitant injuries, including meniscal and cartilage injuries, has not been adequately reported in previous studies on multiligament knee injury (MLKI) because their primary focal points have been the degree of ligament injury, treatment strategy, involvement of other soft tissues, and neurovascular injury.
Purpose:
To analyze the incidence of associated lesions in MLKIs, including medial and lateral meniscal injuries, cartilage lesions, and complications.
Study Design:
Systemic review; Level of evidence, 4.
Methods:
The PubMed, Embase, Cochrane Library, CINAHL, and Scopus databases were searched between inception and April 30, 2020. Studies were included if they reported the incidence rates of medial and/or lateral meniscal tears and cartilage injuries in cases of MLKIs. For the meta-analysis, data were extracted on clinical outcomes measured according to the number of medial and/or lateral meniscal tears, cartilage injuries, and complications.
Results:
A total of 45 studies were included in the MLKI analysis (3391 patients). The pooled rate of medial meniscal tears was 30.4% (95% CI, 24.1%-37.1%; P < .0001; I 2 = 85.8%). The pooled rate of lateral meniscal tears was 27.5% (95% CI, 20.3%-35.3%; P < .0001; I 2 = 89.6%). The pooled rate of cartilage injuries was 27.5% (95% CI, 22.1%-33.3%; P < .0001; I 2 = 86.8%). The pooled rates of peroneal nerve injuries, vascular injuries, and arthrofibrosis were 19.2% (95% CI, 14.2%-24.7%; P < .001; I 2 = 81.3%), 18.4% (95% CI, 13.2%-24.3%; P < .0001; I 2 = 81.0%), and 11.2% (95% CI, 8.1%-14.7%; P = .0018; I 2 = 54.0%), respectively.
Conclusion:
The pooled rates of meniscal tears and cartilage injuries concomitant with MLKIs were high, ranging from 27% to 30%, and the pooled rates of peroneal nerve injury, vascular injury, and arthrofibrosis were considerable, ranging from 11% to 19%. The influence of these associated lesions on clinical results should be evaluated in future clinical studies.
Keywords: multiligament knee injury, anterior cruciate ligament, meta-analysis, outcomes, meniscus, cartilage
Multiligament knee injuries (MLKIs) are rare; nevertheless, they are potentially limb-threatening injuries given the possibility of concomitant severe soft tissue injuries. 18,19,21,58 The classification of injuries, techniques and timing of surgical interventions, postoperative rehabilitation, and reporting of surgical outcomes vary widely among previously published case series in the literature. 19,21,45,58,62 Moreover, evidence on the treatment and incidence of concomitant injuries is sparse owing to the lack of high-level studies or meta-analyses involving this patient population because previous studies have primarily focused on the timing of surgery, rehabilitation, or treatment techniques. 33,45,58
The incidence rates of concomitant injuries, including meniscal and cartilage injuries, have not been adequately reported in studies on MLKIs because their primary foci have been the degree of ligament injury, treatment strategy, involvement of other soft tissues, and neurovascular injury. 19,45,58,62 While concomitant injuries have not been explored in detail in cases of MLKI, 11,21,42,51,59,74,78,80 they are considered important in cases of anterior cruciate ligament (ACL) injury for achieving favorable clinical outcomes. 1,49,54,60,64 According to registry studies, 49,50 23% to 31% of MLKIs involved meniscal injuries, and 16% involved cartilage injuries. In contrast, 46% of isolated ACL injuries involved meniscal injuries, and 61% involved cartilage injuries. 50 However, no meta-analysis has focused on the incidence of concomitant lesions in MLKIs.
This meta-analysis aimed to analyze the pooled incidence of commonly occurring lesions in MLKIs (ie, medial and lateral meniscal tears, cartilage lesions, and other complications). We hypothesized that MLKIs would demonstrate a high incidence of concomitant injuries, similar to that of isolated ACL injuries.
Methods
Study Protocol and Registration
The systematic review and meta-analysis were performed according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. 48 The systematic review protocol was registered in PROSPERO international prospective register of systematic reviews 8 and is accessible online (CRD42020145204).
Search Strategy
The PubMed, EMBASE, Cochrane Library, CINAHL, and Scopus databases were searched. All publications up to April 30, 2020, were included (the literature search was performed on May 28, 2020). The following search specifics and keywords were used:
(Multiligament[All Fields] OR ((“multiple chronic conditions”[Medical Subject Headings (MeSH) Terms] OR (“multiple”[All Fields] AND “chronic”[All Fields] AND “conditions”[All Fields] AND “acute”[All Fields]) OR “multiple chronic conditions”[All Fields] OR “multi”[All Fields]) AND (“ligaments”[MeSH Terms] OR “ligaments”[All Fields] OR “ligament”[All Fields]))) AND ((“meniscus”[MeSH Terms] OR “meniscus”[All Fields]) OR (“cartilage”[MeSH Terms] OR “cartilage”[All Fields])) AND (“knee”[MeSH Terms] OR “knee”[All Fields] OR “knee joint”[MeSH Terms] OR (“knee”[All Fields] AND “joint”[All Fields]) OR “knee joint”[All Fields]).
The search criteria were kept intentionally broad to capture all potentially relevant articles, but only those published in English were included.
Two authors (S.H.K. and Y.-B.P.) independently screened the titles and abstracts of the retrieved studies for eligibility and assessed the agreement using κ statistics. The full texts of the selected studies were reviewed to assess whether they met the inclusion criteria. All citations within the selected studies were screened for relevant studies in case these were missed in the initial search. Disagreements were resolved via discussion between the authors or via consultation with a third author (N.P.).
Eligibility Criteria
The eligibility criteria for systematic reviews and meta-analyses were as follows: published in the English language between January 1980 and April 2020, level of evidence 1 to 4, number of concomitant injuries explicitly reported, and “multiligament” injury defined as the disruption of at least 2 of the 4 major knee ligaments. The concomitant injuries were recorded as follows: number of medial meniscal tears; number of lateral meniscal tears; number of cartilage injuries; and number of complications, such as peroneal nerve injury, vascular injury, and arthrofibrosis. The locations and types of meniscal tears and cartilage injuries were not considered owing to heterogeneity. The numbers of injuries in the studies were obtained regardless of diagnostic methods, such as arthroscopy or magnetic resonance imaging. The number of combined medial and lateral meniscal tears was added to the number of meniscal tears (medial or lateral).
Studies were excluded if they were not published in English or were case reports, clinical opinions and technical notes, or discussions of emergency treatment for MLKI (eg, timing of external fixator application, incidence of concomitant injuries of internal organs, and multiple fractures other than knee fractures).
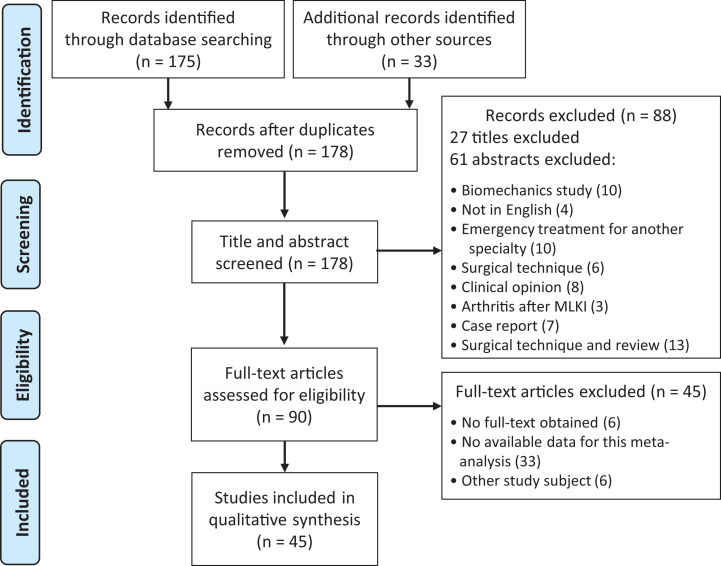
A total of 45 studies (3391 patients) reported the results of concomitant injuries with MLKIs. A flow diagram illustrating the selection process for study inclusion is shown in Figure 1.
Figure 1.
Flow diagram of the article selection process using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. MLKI, multiligament knee injury.
Data Extraction and Collection
Data extraction was performed using the checklist developed by Spindler et al, 69 which was based on the consensus of authors on variables that should be reported. Data on the following variables were extracted: study type, level of evidence, number of cases, number of combined ligament injuries, number of medial and lateral meniscal injuries, number of cartilage injuries, number of complications, and follow-up duration. The extracted data were also cross-checked for accuracy; disagreements were resolved via discussion between the reviewing authors or via consultation with the same third author.
Assessment of Methodological Quality
Two investigators independently assessed the methodological quality of each study using the Downs and Black quality assessment tool, 14 which was developed for use for systemic reviews of randomized and nonrandomized studies. This tool consists of 27 questions that assess the criteria for reporting and external and internal validity (measurement and confounding biases); the highest possible score is 32. Disagreements were resolved via discussion and assessed according to the κ value. The possibility of publication bias was examined using funnel plots and the Egger test. 15
Statistical Analysis
Data analyses were performed using the R program (Version 3.5.3; R Foundation for Statistical Computing) with the “meta” and “metafor” packages. Estimates of the incidence of concomitant injuries among the eligible studies were transformed using the Freeman-Tukey double arcsine method 25 and analyzed using a random-effects proportion meta-analysis (weighted for individual study size). Statistical heterogeneity was assessed using the I 2 statistic and defined as follows: I 2 > 50%, substantial heterogeneity; 20% < I 2 ≤ 50%, moderate; and I 2 < 20%, low. A random-effects model was used to analyze the most robust results. Pooled estimates were summarized using forest plots for the total study population.
Interrater reliability was assessed using the κ statistic to determine the degree of agreement between study selection and risk assessment. Agreement was defined as fair (κ = 0.21-0.40), moderate (κ = 0.41-0.60), substantial (κ = 0.61-0.80), or almost perfect (κ = 0.81-1.00). In all analyses, a 2-sided P value <.05 was considered statistically significant.
Results
Study Characteristics
A summary of the studies in this review is shown in Appendix Table A1.
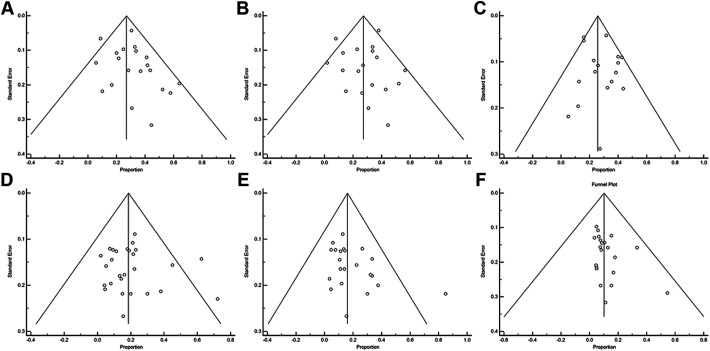
Assessment of Methodological Quality and Grade of Evidence Quality for Each Outcome
The results of the literature review and quality assessment of the studies are summarized in Appendix Table A2 (κ = 0.71 [substantial agreement]). The funnel plots showed no publication bias in the reporting of medial meniscal tears (P = .062), lateral meniscal tears (P = .103), cartilage injuries (P = .198), peroneal nerve injuries (P = .371), vascular injuries (P = .069), and arthrofibrosis (P = .073) (Appendix Figure A1).
Risk of Concomitant Medial Meniscal Tears
The number of medial meniscal tears was reported in 20 studies (1663 patients) on MLKIs. ∥ There were 461 medial meniscal tears in the MLKI group. The overall pooled rate of medial meniscal tears in the MLKI group was 30.4% (95% CI, 24.1%-37.1%; P < .0001); substantial heterogeneity was noted (I 2 = 85.8%; 95% CI, 79.5%-90.2%) (Figure 2).
Figure 2.
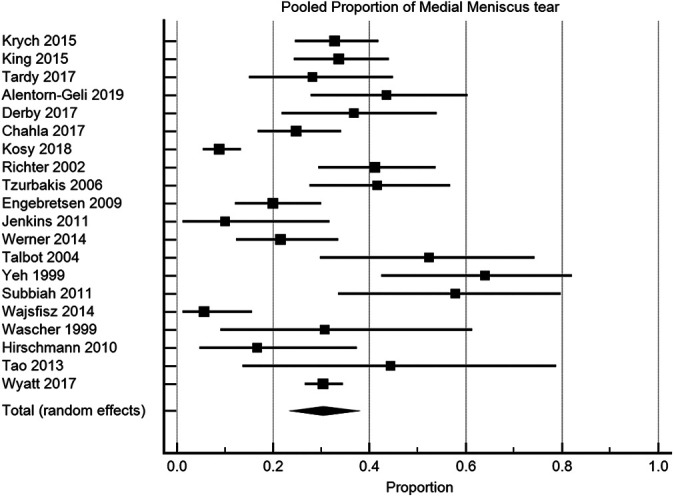
Proportional forest plot with 95% CIs for medial meniscal tears in multiligament knee injuries. The squares represent the results of each study. The ends of the horizontal bars represent 95% CIs. The diamond denotes the overall pooled proportion from all studies. The pooled proportion was 30.4% with substantial heterogeneity (95% CI, 24.1%-37.1%; P < .0001; I 2 = 85.8%).
Risk of Concomitant Lateral Meniscal Tears
The number of lateral meniscal tears was reported in 19 studies (1598 patients) on MLKIs. ¶ There were 455 lateral meniscal tears in the MLKI group. The overall pooled rate of lateral meniscal tears in the MLKI group was 27.5% (95% CI, 20.3%-35.3%; P < .0001); substantial heterogeneity was noted (I 2 = 89.6%; 95% CI, 85.2%-92.7%) (Figure 3).
Figure 3.
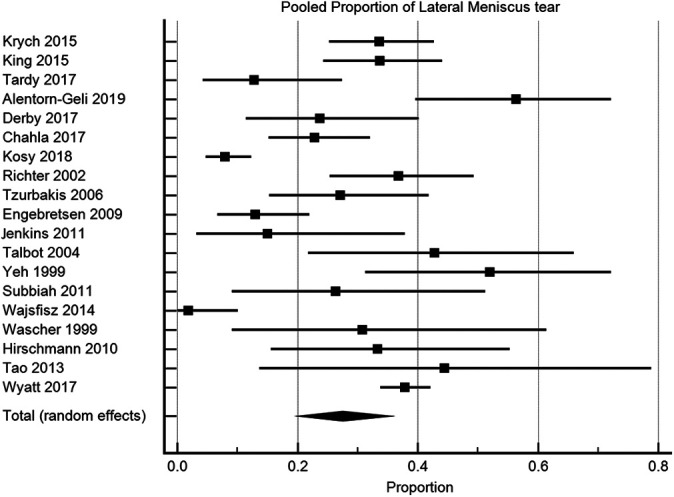
Proportional forest plot with 95% CIs for lateral meniscal tears in multiligament knee injuries. The squares represent the results of each study. The diamond denotes the overall pooled proportion from all studies. The pooled proportion was 27.5% with substantial heterogeneity (95% CI, 20.3%-35.3%; P < .0001; I 2 = 89.6).
Risk of Concomitant Cartilage Injury
The incidence of cartilage injury was reported in 17 studies (2245 patients) on MLKIs. # There were 589 cartilage injuries in the MLKI group. The overall pooled cartilage injury rate in the MLKI group was 27.5% (95% CI, 22.1%-33.3%; P < .0001); substantial heterogeneity was noted (I 2 = 86.8%; 95% CI, 80.3%-91.1%) (Figure 4).
Figure 4.
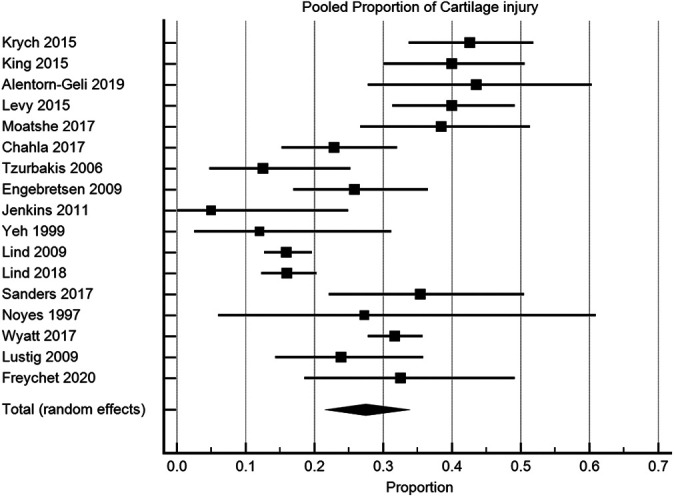
Proportional forest plot with 95% CIs for concomitant cartilage injury in multiligament knee injuries. The squares represent the results of each study. The diamond denotes the overall pooled proportion from all studies. The pooled proportion was 27.5% with substantial heterogeneity (95% CI, 22.1%-33.3%; P < .0001; I 2 = 86.8%).
Risk of Concomitant Complications in MLKIs
The number of peroneal nerve injures in MLKIs was reported in 27 studies (231/1191 patients). ** The pooled rate of peroneal nerve injury in MLKIs was 19.2% (95% CI, 14.2%-24.7%; P < .001); substantial heterogeneity was noted (I 2 = 81.3%; 95% CI, 73.7%-86.8%) (Figure 5). The number of vascular injuries concomitant with MLKIs was reported in 22 studies (170/1020 patients). †† The pooled rate of vascular injuries was 18.4% (95% CI, 13.2%-24.3%; P < .0001); substantial heterogeneity was noted (I 2 = 81.0%; 95% CI, 72.1%-87.1%) (Figure 6).
Figure 5.
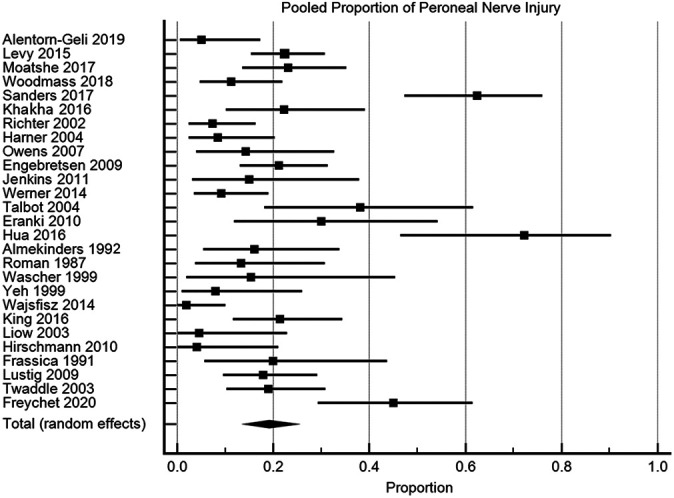
Proportional forest plot with 95% CIs for peroneal nerve injury in multiligament knee injuries. The squares represent the results of each study. The diamond denotes the overall pooled proportion from all studies. The pooled proportion was 19.2% with substantial heterogeneity (95% CI, 14.2%-24.7%; P < .001; I 2 = 81.3%).
Figure 6.
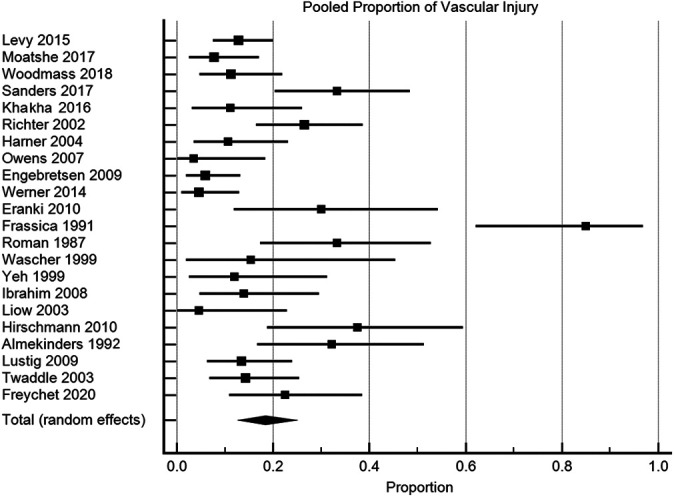
Proportional forest plot with 95% CIs for vascular injuries concomitant with multiligament knee injuries. The squares represent the results of each study. The diamond denotes the overall pooled proportion from all studies. The pooled proportion was 18.4% with substantial heterogeneity (95% CI, 13.2%-24.3%; P < .0001; I 2 = 81.0%).
Arthrofibrosis in MLKI cases was reported in 21 studies (84/833 patients). ‡‡ The pooled rate of arthrofibrosis in MLKI was 11.2% (95% CI, 8.1%-14.7%; P = .0018); substantial heterogeneity was noted (I 2 = 54.0%; 95% CI, 24.6%-71.9%) (Figure 7).
Figure 7.
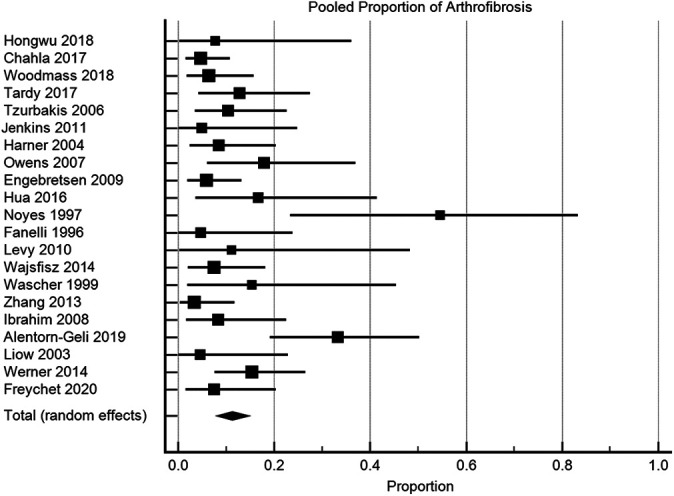
Proportional forest plot with 95% CIs for arthrofibrosis in multiligament knee injuries. The squares represent the results of each study. The diamond denotes the overall pooled proportion from all studies. The pooled proportion was 11.2% with substantial heterogeneity (95% CI, 8.1%-14.7%; P = .0018; I 2 = 54.0%).
Discussion
The primary finding of the present meta-analysis was that the pooled incidence of injuries concomitant with MLKIs was 30.4% for medial meniscal tears, 27.5% for lateral meniscal tears, and 27.5% for cartilage injuries. Although study heterogeneity was substantial, the pooled rates of injuries concomitant with MLKIs in this proportional meta-analysis were lower than were those concomitant with isolated ACL injuries in previous studies. 23,50,53,72 Moreover, the pooled rates for peroneal nerve injuries, vascular injuries, and arthrofibrosis ranged from 11% to 19%. As such, careful examination should be performed during the assessment of combined injuries.
Controversy persists in orthopaedic reports regarding the treatment for or incidence of injuries concomitant with MLKIs owing to the paucity of high-level studies, rarity of MLKIs, and heterogeneity in patients and involved structures. 33,45,58 The incidence of meniscal and cartilage injuries concomitant with MLKIs has not been previously examined because clinical outcomes, such as postoperative stiffness, stability, and timing of surgery, are usually highlighted in systematic reviews and meta-analyses. 5,21,33,45,58 Thus, it is necessary to evaluate the incidence rates of concomitant meniscal tears, cartilage injuries, and complications, especially using pooled proportional meta-analysis methods.
The pooled results of concomitant medial meniscal tears showed that 30.4% of MLKIs involved medial meniscal tears. In the MLKI group, Yeh et al 83 cited the highest incidence of medial meniscal tears (64.0% [16/25]) in a small series, whereas Kosy et al 42 noted the lowest incidence (8.8% [20/226]) in a large cohort. As Kosy et al evaluated the incidence of root tears of the meniscus in patients with MLKIs, the incidence may have been lower than that in other studies. In a study by Wyatt et al, 82 30.4% of medial meniscal tears were in cases of MLKIs, similar to our pooled result, and the incidence rate was 39.5% in patients with isolated ACL injuries. According to the results of Wyatt et al, in the largest comparative study on MLKIs and isolated ACL injuries, lower likelihood rates for all meniscal injuries (odds ratio, 0.56; 95% CI, 0.47-0.67; P < .001) and medial meniscal injuries (odds ratio, 0.053; 95% CI, 0.44-0.65; P < .001) were found after multivariable adjustment in the MLKI group versus the isolated ACL injury group. Meanwhile, among previous studies on isolated ACL injuries reporting the results of combined lesions, Cipolla et al 12 cited a high incidence of medial meniscal tears in patients with isolated ACL injuries (61.7% [475/770]); in contrast, Herbst et al 31 indicated a rate of only 16.0% (33/206). In the largest cohort study by Magnussen et al, 53 33.3% (1643/4928) of medial meniscal tears were found in cases of an isolated ACL injury, and interestingly, the incidence of medial meniscal tears in the Multicenter Orthopaedic Outcomes Network prospective cohort was higher than that in the Norwegian National Knee Ligament Registry. 22,53 In the study by Mehl et al, 56 52.1% of isolated ACL injuries involved medial meniscal tears: 41.2% occurred <6 months after ACL injury, and 63.9% occurred >6 months after ACL injury. In brief, the pooled incidence of medial meniscal tears in the MLKI group was approximately 30%, similar to that in the isolated ACL injury group of Magnussen et al but lower than that in the isolated ACL injury group of Wyatt et al. As such, these lesions should be carefully evaluated during surgery to determine whether the meniscus needs to be treated.
The pooled results for concomitant lateral meniscal tears showed that 27.5% of MLKIs involved lateral meniscal tears. In contrast, the incidence of lateral meniscal tears in MLKIs varied across studies, ranging from 1.8% to 56.4% 3,77 ; however, the overall pooled rate of lateral meniscal tears in the MLKI group was 26.5%, similar to that reported by Magnussen et al. 53 However, Wyatt et al 82 indicated a higher incidence of lateral meniscal tears in the MLKI group (37.9%) than in this study. The incidence rate of lateral meniscal tears in isolated ACL injuries ranged from 48.7% (73/150) 23 to 13.2% (31/235) in previous studies. 64 In the study by Magnussen et al, the rate of lateral meniscal tears in patients with isolated ACL injuries was 25.1%, as opposed to 37.4% from Wyatt et al. However, the pooled incidence of lateral meniscal tears in patients with MLKIs in this study seemed to be lower than that in previous studies on isolated ACL injuries. 23,82
The pooled rate of cartilage injuries was 27.5% in the MLKI group. A cohort study by Lind et al 50 showed that the rate of cartilage injuries was 63.0% in the isolated ACL injury group but only 16% in the MLKI group. In the study by Wyatt et al, 82 the rate of cartilage injuries in the isolated ACL group was 26.4%, but a higher incidence (31.7%) was found in the MLKI group, although these differences were not significant after multivariate adjustment. In brief, the incidence rates of cartilage injuries concomitant with MLKIs or isolated ACL injuries also varied across studies, ranging from 11.2% to 76.6% for isolated ACLs injuries 23,72 and from 5% to 43.6% for MLKIs. 3,37 The pooled incidence of cartilage injuries in the MLKI group in this study was lower than that in the isolated ACL injury group in other large cohort series. 50,56,82
In this study, high incidence rates of medial and lateral meniscal tears were found in the MLKI group; the incidence rates were similar to or lower than those in the isolated ACL injury groups in previous studies 50,56,82 (Appendix Table A1). Deficiency in the ACL increases the contact and hoop forces of the menisci and cartilage, especially in response to rotatory loading, as shown in biomechanical and clinical studies. 2,28,29,55,84 Thus, the twisting mechanism (ie, the combined force of hyperextension and rotational direction, as well as valgus/varus compression forces) would increase the risk of meniscal and cartilage injuries. 9,44 However, if cruciate deficiency is combined with a deficiency in the collateral ligaments in the case of high-energy direct trauma, the twist loading on the knee joint could be lower than that on intact collateral models owing to loss of the knee hinge, 6,39,44,67,68 which might be a reason for the relatively lower incidence of meniscal injury in MLKIs than in isolated ACL injuries. However, in this study, the mechanism of MLKIs was not identified; thus, it is difficult to conclude how the mechanism of injury or differences in load distribution might affect the ligament, cartilage, or meniscal tear patterns.
In terms of complications in the MLKI group, the pooled rate of vascular injuries was 18.4%. However, the incidence of vascular injuries in the present study was lower than that in previous studies, ranging from 21% to 50%. 7,24,27,65 The popliteal artery is an “end-to-end artery” to the leg, with minimal collateral circulation; thus, injury to this artery is considered an emergency situation. When the pooled results were calculated, studies on emergency treatment for vascular and nerve injury were excluded; therefore, the rate may be lower than those in other previous studies. The pooled rate of peroneal nerve injuries was 19.2%. This result was similar to those in some previous studies 21,37,79 ; however, other studies have reported higher incidence rates. 7,40,47
There are many other complications in MLKIs, and a careful evaluation is therefore essential. Alentorn-Geli et al 3 observed osteoarthritis development (33% [13/39]) after a mean 27 months of follow-up in MLKI injuries. Roman et al 65 and Richter et al 63 examined tibial nerve injury (9.2% [11/119]), and Richter et al and Engebretsen et al 16 investigated combined patellar tendon injuries (7.5% [11/147]) and patellar dislocations (5.9% [5/85]) with MLKI, respectively. Engebrestsen et al and Jenkins et al 37 focused on combined deep vein thrombosis after treatment of MLKI (5.3% [5/95]), and Eranki et al 17 studied compartment syndrome of the limb (5% [1/20]).
There are several limitations to the present study. First, the lack of randomization, low methodological quality, and heterogeneity of the studies may have reduced the external validity of the studies and this meta-analysis. The lack of a large number of studies might be the reason for the nonsignificant results of the metaregression analysis. Second, the pooled rates of concomitant injuries could not be directly compared with the rates associated with isolated ACL injuries, which were not pooled. Moreover, clinical outcomes and objective measurements, such as stress radiography findings, could not be pooled for studies on MLKIs because of heterogeneity or missing data. Third, the timing of surgery, mechanism of injury, and ligament injuries in the MLKI group were not classified. There might have been differences in the number of combined ligament injuries, such as ACL and/or posterior cruciate ligament injuries with collateral ligament injuries. Moreover, there may have been outcome differences in early versus delayed surgery for MLKIs. As such, there may have been differences in concomitant injuries according to these factors.
The strengths of this meta-analysis were its systematic approach and the pooling of data from studies that reported on injuries concomitant with MLKIs. Studies on MLKIs are inconsistent and uncommon, with many potential confounding factors and sources of heterogeneity; therefore, manually counting and pooling the numbers of combined injuries in each study might be possible in a proportional meta-analysis. To our knowledge, this is the first study to focus on the pooled rates of meniscal tears, cartilage injuries, and complications in MLKIs and compare them with the respective rates associated with isolated ACL injuries. The results of this study suggest that the incidence rates of concomitant meniscal tears and cartilage injuries are high in cases of MLKIs and are comparable with the rates in cases of isolated ACL injuries; thus, these injuries should be carefully diagnosed, and ligament surgery should be planned accordingly.
Conclusion
The pooled rates of concomitant meniscal tears and cartilage injuries in MLKIs were high, ranging from 27% to 30%, and the complications of peroneal nerve injury, vascular injury, and arthrofibrosis were considerable, with pooled rates ranging from 11% to 19%. The influence of these associated lesions on clinical results should be evaluated in future clinical studies.
Appendix
TABLE A1.
Results From Studies on Multiligament Knee Injury a
| Combined Injuries, No. (%) | Mean ± SD (Range) | ||||||
|---|---|---|---|---|---|---|---|
| Lead Author (Year) | No. of Patients | Ligament | Meniscal | Cartilage | No. of Complications | Time From Trauma to Surgery | Follow-up |
| Krych (2015) 43 | 122 | Multiligament | MM tear: 40 LM tear: 41 |
52 | 62 early (<3 mo) 40 delayed (3-12 mo) 20 chronic (>12 mo) |
||
| Lind (2009) 49 | 457 | Multiligament | 73 (16) | 21.9% early (<0.5 y)53.4% delayed (0.5-5 y)24.7% chronic (>5 y) | 2 y after surgery | ||
| King (2015) 41 | 95 | Multiligament (knees with only ACL-MCL or ACL-PLC injuries excluded) | MM tear: 32 LM tear: 32 |
38 | Mean 8 mo | 6 y (2-20 y) | |
| King (2016) 40 | 56 | Multiligament (ACL-PCL-MCL and ACL-PCL-LCL) | Peroneal nerve injury: 12 | ACL-PCL-MCL: 9.8 ± 23.3 mo ACL-PCL-LCL: 7.2 ± 15.0 mo |
ACL-PCL-MCL: 78.3 ± 60.4 mo ACL-PCL-LCL: 76.1 ± 58.9 mo |
||
| Tardy (2017) 74 | 39 | Multiligament, PMC vs PLC, combined ACL or PCL injury | MM tear: 11 LM tear: 5 |
Arthrofibrosis: 5 | 28 acute (<3 wk)11 chronic (>3 wk) | Median, 57 mo (12-129 mo) | |
| Alentorn-Geli (2019) 3 | 39 | Multiligament | MM tear: 17 LM tear: 22 |
17 | Peroneal nerve injury: 2 Arthrofibrosis: 13 |
36 acute (8 ± 5.3 wk) 3 chronic (124 ± 87 mo) |
Median, 27 mo (12-84 mo) |
| Levy (2015) 47 | 125 | Multiligament | Total: 73 | 50 | Peroneal nerve injury: 28 Vascular injury: 16 |
Median, 5 y (2-22 y) | |
| Derby (2017) 13 | 38 | Multiligament | MM tear: 14 LM tear: 9 c |
26 acute (<3 mo) 7 chronic (>3 mo) 5 unknown |
|||
| Moatshe (2017) 57 | 65 | ACL-PCL rupture with/without collateral ligament injury | Total: 25 | 25 | Peroneal nerve injury: 15 Vascular injury: 5 |
33 acute (<21 d) 32 chronic (>21 d) |
13.1 y (10-18.8 y) |
| Lind (2018) 50 | 344 | Multiligament injury | Total: 79 (23) | 55 (16) | 5.7 ± 2.9 y | ||
| Woodmass (2018) 81 | 62 | Multiligament injury including fracture | Peroneal nerve injury: 7 Vascular injury: 7 Arthrofibrosis: 4 |
10 acute (<3 wk) 52 delayed (>3 wk) |
67 mo (24-220 mo) | ||
| Hongwu (2018) 34 | 13 | Multiligament injury | Arthrofibrosis: 1 | 1.84 d (1-3 d) | 32.6 mo (24-46 mo) | ||
| Chahla (2017) 10 | 105 | Multiligament injury | MM tear: 26 LM tear: 24 |
24 | Arthrofibrosis: 5 | 72 acute (<6 wk) 33 chronic (>6 wk to 6 mo) |
3.0 y (2.0-4.7 y) |
| Yeh (1999) 83 | 25 | Multiligament injury | MM tear: 16 LM tear: 13 |
3 | Peroneal nerve injury: 2 Vascular injury: 3 |
11.1 ± 5 d (5-25 d) | 27.2 ± 7.86 mo |
| Levy (2010) 46 | 9 | Multiligament injury | Arthrofibrosis: 1 | 75 d (21-171 d) 5 acute (<6 wk) 4 chronic (>6 wk) |
4 mo (13-32 mo) | ||
| Liow (2003) 51 | 22 | Multiligament injury including fracture | Peroneal nerve injury: 1 Vascular injury: 1 Arthrofibrosis (stiffness): 1 |
8 acute (<2 wk) 14 chronic (>6 mo) |
32 mo (11-77 mo) | ||
| Sanders (2017) 66 | 48 | Multiligament injury including fracture | Total: 30 | 17 | Peroneal nerve injury: 30 Vascular injury: 16 |
13 acute (<3 wk) 35 chronic (>3 wk) |
8.3 ± 5.0 y (2.1-21.8 y) |
| Subbiah (2011) 70 | 19 | Multiligament injury | MM tear: 11 LM tear: 5 |
11 acute (<3 wk) 8 chronic (>3 wk) |
22 mo (14-33 mo) | ||
| Tao (2013) 73 | 9 | Multiligament injury | MM tear: 4 LM tear: 4 |
Acute (<3 wk): 11.4 ± 4.8 d | 30 mo (18-46 mo) | ||
| Zhang (2013) 85 | 59 | Multiligament injury including fractures | Arthrofibrosis: 2 | 48 acute (<3 wk): 7.3 d (1-13 d) 11 chronic (>3 wk): 3.8 mo (1-9 mo) |
2.5 y (1.75-3.75 y) | ||
| Kosy (2018) 42 | 226 | Multiligament injury including fractures | MM root tear: 20 LM root tear: 18 |
All within 2 wk of trauma | |||
| Khakha (2016) 38 | 36 | Multiligament injury | Peroneal nerve injury: 8 Vascular injury: 4 |
All within 3 wk after trauma | 10.1 y (7-19 y) | ||
| Richter (2002) 63 | 68 | Multiligament | MM tear: 28 LM tear: 25 |
Peroneal nerve injury: 5 Vascular injury: 18 |
10.6 ± 26.6 d (0-140 d) | 8.2 y (2-25 y) | |
| Tzurbakis (2006) 76 | 48 | ACL + medial side: 12 (25) Cruciate + PLC: 11 (22.9) Bicruciate + collateral: 25 (52.1) |
MM tear: 20 LM tear: 13 |
6 | Arthrofibrosis: 5 | 38 acute (<3 wk): 7.47 ± 5.82 d 10 chronic (>3 wk): 204.7 ± 138.1 d |
51.3 ± 28.9 mo (24-96 mo) |
| Noyes (1997) 59 | 11 | Multiligament including fracture | Total: 5 | 3 | Arthrofibrosis: 6 | 7 acute (<2 wk) 4 chronic (>2 wk) |
4.5 y (2.5-6.9 y) |
| Harner (2004) 30 | 47 b | Multiligament | Peroneal nerve injury: 4 Vascular injury: 5 Arthrofibrosis: 4 |
19 acute (<3 wk) 12 chronic (>3 wk) |
44 mo (2-6 y) | ||
| Owens (2007) 61 | 28 | Multiligament | Total: 14 | Peroneal nerve injury: 4 Vascular injury: 1 Arthrofibrosis: 5 |
All within 2 wk of trauma (17 d [1-101 d]) | 48 mo (13-82 mo) | |
| Engebretsen (2009) 16 | 85 | Multiligament including fracture | MM tear: 17 LM tear: 11 |
22 | Peroneal nerve injury: 18 Vascular injury: 5 Arthrofibrosis: 5 |
50 acute (<2 wk) 35 chronic (>2 wk) |
5.3 ± 1.9 y |
| Jenkins (2011) 37 | 20 | ACL-MCL: 1 (5); ACL-PCL: 3 (15); ACL-PLC: 4 (20); PCL-PLC: 2 (10); ACL-PCL-PLC: 8 (40); ACL-MCL-PCL: 2 (10) | MM tear: 2 LM tear: 3 |
1 | Peroneal nerve injury: 3 Arthrofibrosis: 1 |
6 acute (<3 wk): 3.3 d (1-7 d) 14 chronic (>3 wk): 13 mo (1-64 mo) |
2 y |
| Werner (2014) 79 | 65 | KD 3 M: 32 (49.2); KD 4: 33 (50.8) | MM tear: 14 | Peroneal nerve injury: 6 Vascular injury: 3 Arthrofibrosis: 10 |
All within 3 wk | 6.2 y (1.1-11.6 y) | |
| Talbot (2004) 71 | 21 | KD 2: 1 (4.8); KD 3 M: 9 (42.9); KD 3 L: 10 (47.6); KD 4: 1 (4.8) | MM tear: 11 LM tear: 9 |
Peroneal nerve injury: 8 | All within 3 wk | 27.4 mo | |
| Eranki (2010) 17 | 20 | Multiligament including fracture (ACL-PCL-MCL most common, PCL-LCL-PLC second, ACL-PCL-MCL-LCL-PLC third) | Peroneal nerve injury: 6 Vascular injury: 6 |
All within 14 d | 24 mo | ||
| Hua (2016) 35 | 18 | Multiligament including fracture | Peroneal nerve injury: 13 Arthrofibrosis: 3 |
All within 2 wk (5-10 d after injury) | 4.8 ± 1.3 y | ||
| Almekinders (1992) 4 | 31 | Multiligament | Peroneal nerve injury: 5 Vascular injury: 10 |
40 mo | |||
| Roman (1987) 65 | 30 | Multiligament | Peroneal nerve injury: 4 Vascular injury: 10 |
||||
| Wascher (1999) 78 | 13 | ACL-PCL-MCL: 7 (53.8); ACL-PCL-PLC: 6 (46.2) | MM tear: 4 LM tear: 4 |
Peroneal nerve injury: 2 Vascular injury: 2 Arthrofibrosis: 2 |
9 acute (<3 wk) 4 chronic (>6 wk) |
38.4 mo | |
| Fanelli (1996) 20 | 21 | All were PCL-PLC injuries | Arthrofibrosis: 1 | 10 acute 11 chronic |
24 mo (24-54 mo) | ||
| Frassica (1991) 24 | 20 | Multiligament including fracture | Vascular injury: 17 Peroneal nerve injury: 4 |
12 within 5 d | 57 mo (22-96 mo) | ||
| Hirschmann (2010) 32 | 24 | KD 3 M: 12 (50); KD 3 L: 8 (33); KD 4: 4 (17) | MM tear: 4 LM tear: 8 |
Peroneal nerve injury: 1 Vascular injury: 9 |
12 within 1 wk 5 within 2-3 wk 7 after 3 wk |
8 y (1-23 y) | |
| Ibrahim (2008) 36 | 36 | ACL-PCL-MCL: 15 (75); ACL-PCL-PLC: 5 (25); others excluded | Vascular injury: 5 Arthrofibrosis: 3 |
2-3 wk after injury | 43 mo | ||
| Wajsfisz (2014) 77 | 53 | Multiligament | MM tear: 3 LM tear: 1 |
Peroneal nerve injury: 1 Arthrofibrosis: 4 |
10 early (<3 wk) 43 delayed (>3 wk) |
49 mo (12-146 mo) | |
| Wyatt (2017) 82 | 549 | Multiligament | MM tear: 167 LM tear: 208 |
174 | |||
| Lustig (2009) 52 | 67 | Multiligament | 16 | Peroneal nerve injury: 12 Vascular injury: 9 |
|||
| Twaddle (2003) 75 | 63 | Multiligament | Peroneal nerve injury: 12 Vascular injury: 9 |
||||
| Freychet (2020) 26 | 40 | Multiligament | Total: 22 | 13 | Peroneal nerve injury: 18 Vascular injury: 9 Arthrofibrosis: 3 |
20 single-stage surgery 20 staged surgery |
≥2 y |
a Blank cells indicate not reported. ACL, anterior cruciate ligament; KD, knee dislocation classification; L, lateral; LCL, lateral collateral ligament; LM, lateral meniscus; M, medial; MCL, medial collateral ligament; MM, medial meniscus; PCL, posterior cruciate ligament; PLC, posterolateral corner; PMC, posteromedial corner.
b Included in clinical analysis: n = 31.
c Confirmed using arthroscopy.
TABLE A2.
Quality Assessment of the Included Studies
| Internal Validity | ||||||||
|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | Study Design (Level of Evidence) | No. of Patients | Reporting | External Validity | Bias | Confounding (Selection Bias) | Power | Total |
| Krych (2015) 43 | Retrospective (3) | 122 | 3 | 1 | 3 | 3 | 5 | 15 |
| King (2015) 41 | Retrospective (3) | 95 | 5 | 1 | 3 | 3 | 4 | 16 |
| King (2016) 40 | Retrospective comparative (3) | 56 | 5 | 1 | 2 | 2 | 3 | 13 |
| Tardy (2017) 74 | Retrospective (3) | 39 | 4 | 1 | 3 | 3 | 2 | 13 |
| Alentorn-Geli (2019) 3 | Retrospective cross-sectional comparative (3) | 39 | 5 | 1 | 3 | 3 | 2 | 14 |
| Levy (2015) 47 | Retrospective (3) | 125 | 4 | 1 | 3 | 3 | 5 | 16 |
| Derby (2017) 13 | Retrospective diagnostic (2) | 38 | 6 | 1 | 3 | 2 | 2 | 14 |
| Moatshe (2017) 57 | Retrospective cohort (3) | 65 | 9 | 1 | 4 | 3 | 4 | 21 |
| Hongwu (2018) 34 | Retrospective cohort (4) | 13 | 4 | 1 | 3 | 3 | 0 | 11 |
| Woodmass (2018) 81 | Retrospective cohort (3) | 62 | 9 | 1 | 3 | 3 | 4 | 20 |
| Chahla (2017) 10 | Retrospective cohort (3) | 105 | 9 | 1 | 5 | 3 | 5 | 23 |
| Yeh (1999) 83 | Retrospective cohort (4) | 25 | 4 | 1 | 3 | 3 | 1 | 12 |
| Levy (2010) 46 | Retrospective cohort (4) | 9 | 5 | 1 | 3 | 3 | 0 | 12 |
| Liow (2003) 51 | Retrospective cohort (4) | 22 | 5 | 1 | 3 | 3 | 1 | 13 |
| Subbiah (2011) 70 | Retrospective cohort (4) | 19 | 7 | 1 | 3 | 2 | 0 | 13 |
| Tao (2013) 73 | Retrospective cohort (4) | 9 | 8 | 1 | 3 | 2 | 0 | 14 |
| Zhang (2013) 85 | Retrospective cohort (3) | 59 | 7 | 1 | 3 | 2 | 3 | 16 |
| Sanders (2017) 66 | Retrospective cohort (3) | 48 | 7 | 1 | 4 | 2 | 3 | 17 |
| Richter (2002) 63 | Retrospective case-control (3) | 68 | 5 | 1 | 3 | 3 | 4 | 16 |
| Kosy (2018) 42 | Retrospective cohort (3) | 226 | 5 | 1 | 2 | 0 | 5 | 13 |
| Khakha (2016) 38 | Prospective cohort (2b) | 36 | 6 | 1 | 3 | 2 | 2 | 14 |
| Tzurbakis (2006) 76 | Retrospective cohort (3) | 48 | 5 | 1 | 2 | 0 | 3 | 11 |
| Noyes (1997) 59 | Retrospective cohort (4) | 11 | 3 | 1 | 2 | 0 | 0 | 6 |
| Harner (2004) 30 | Retrospective cohort (3) | 47 | 9 | 1 | 3 | 3 | 2 | 18 |
| Owens (2007) 61 | Retrospective cohort (4) | 28 | 4 | 1 | 2 | 0 | 1 | 8 |
| Engebretsen (2009) 16 | Prospective cohort (2) | 85 | 8 | 1 | 3 | 2 | 4 | 18 |
| Jenkins (2011) 37 | Retrospective cohort (4) | 20 | 6 | 1 | 3 | 0 | 1 | 10 |
| Werner (2014) 79 | Retrospective cohort (3) | 65 | 4 | 1 | 3 | 2 | 4 | 14 |
| Talbot (2004) 71 | Retrospective cohort (4) | 21 | 4 | 1 | 2 | 0 | 1 | 8 |
| Eranki (2010) 17 | Retrospective cohort (4) | 20 | 5 | 1 | 2 | 0 | 1 | 9 |
| Hua (2016) 35 | Retrospective cohort (4) | 18 | 6 | 0 | 2 | 0 | 0 | 8 |
| Almekinders (1992) 4 | Retrospective cohort (3) | 31 | 5 | 1 | 3 | 2 | 0 | 11 |
| Roman (1987) 65 | Retrospective cohort (3) | 30 | 2 | 1 | 2 | 0 | 2 | 7 |
| Wascher (1999) 78 | Retrospective cohort (4) | 13 | 5 | 1 | 2 | 0 | 0 | 8 |
| Fanelli (1996) 20 | Retrospective cohort (4) | 21 | 3 | 0 | 1 | 0 | 1 | 5 |
| Frassica (1991) 24 | Retrospective cohort (4) | 17 | 3 | 0 | 1 | 0 | 1 | 5 |
| Hirschmann (2010) 32 | Retrospective cohort (4) | 24 | 3 | 1 | 1 | 0 | 1 | 6 |
| Ibrahim (2008) 36 | Retrospective cohort (3) | 36 | 4 | 1 | 2 | 0 | 1 | 8 |
| Wajsfisz (2014) 77 | Retrospective cohort (3) | 53 | 6 | 1 | 3 | 2 | 3 | 15 |
| Lind (2018) 50 | Prospective cohort (registry data) (3) | 344 | 10 | 2 | 4 | 3 | 5 | 24 |
| Lind (2009) 49 | Prospective cohort (registry data) (3) | 457 | 10 | 2 | 4 | 3 | 5 | 24 |
| Wyatt (2017) 82 | Prospective cohort (2) | 549 | 10 | 2 | 4 | 3 | 5 | 24 |
| Lustig (2009) 52 | Prospective cohort (2) | 67 | 9 | 1 | 3 | 3 | 4 | 20 |
| Twaddle (2003) 75 | Prospective cohort (2) | 63 | 9 | 1 | 3 | 3 | 4 | 20 |
| Freychet (2020) 26 | Retrospective cohort (3) | 40 | 9 | 1 | 2 | 2 | 3 | 17 |
Figure A1.
Funnel plots for publication bias in the studies on multiligament knee injury (MLKI). No evidence of asymmetry was found: (A) medial meniscal injury (P = .062), (B) lateral meniscal injury (P = .103), (C) cartilage injury (P = .198), (D) peroneal nerve injury in MLKI group (P = .371), (E) vascular injury in MLKI group (P = .069), and (F) arthrofibrosis (P = .073).
Footnotes
Final revision submitted December 5, 2020; accepted January 5, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was supported by a research grant from Chung-Ang University (2019). N.P. has received educational consulting fees from Smith & Nephew, LimaCorporate, Stryker, and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ahlén M, Lidén M. A comparison of the clinical outcome after anterior cruciate ligament reconstruction using a hamstring tendon autograft with special emphasis on the timing of the reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19(3):488–494. [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament–deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39(10):2187–2193. [DOI] [PubMed] [Google Scholar]
- 3. Alentorn-Geli E, Lazarides AL, Utturkar GM, et al. Factors predictive of poorer outcomes in the surgical repair of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):445–459. [DOI] [PubMed] [Google Scholar]
- 4. Almekinders LC, Logan TC. Results following treatment of traumatic dislocations of the knee joint. Clin Orthop Relat Res. 1992;284:203–207. [PubMed] [Google Scholar]
- 5. Barfield WR, Holmes RE, Slone H, Walton ZJ, Hartsock LA. Acute versus staged surgical intervention in multiligamentous knee injuries: a review of the literature since 2009. Curr Orthop Pract. 2015;26(5):530–535. [Google Scholar]
- 6. Bates NA, Schilaty ND, Nagelli CV, Krych AJ, Hewett TE. Multiplanar loading of the knee and its influence on anterior cruciate ligament and medial collateral ligament strain during simulated landings and noncontact tears. Am J Sports Med. 2019;47(8):1844–1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Becker EH, Watson JD, Dreese JC. Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J Orthop Trauma. 2013;27(4):226–231. [DOI] [PubMed] [Google Scholar]
- 8. Booth A, Clarke M, Dooley G, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brophy RH, Zeltser D, Wright RW, Flanigan D. Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. Arthroscopy. 2010;26(1):112–120. [DOI] [PubMed] [Google Scholar]
- 10. Chahla J, Dean CS, Matheny LM, Mitchell JJ, Cinque ME, LaPrade RF. Outcomes of inside-out meniscal repair in the setting of multiligament reconstruction in the knee. Am J Sports Med. 2017;45(9):2098–2104. [DOI] [PubMed] [Google Scholar]
- 11. Chahla J, Murray IR, Robinson J, et al. Posterolateral corner of the knee: an expert consensus statement on diagnosis, classification, treatment, and rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2018;27(8):2520–2529. [DOI] [PubMed] [Google Scholar]
- 12. Cipolla M, Scala A, Gianni E, Puddu G. Different patterns of meniscal tears in acute anterior cruciate ligament (ACL) ruptures and in chronic ACL-deficient knees: classification, staging and timing of treatment. Knee Surg Sports Traumatol Arthrosc. 1995;3(3):130–134. [DOI] [PubMed] [Google Scholar]
- 13. Derby E, Imrecke J, Henckel J, Hirschmann A, Amsler F, Hirschmann MT. How sensitive and specific is 1.5 Tesla MRI for diagnosing injuries in patients with knee dislocation? Knee Surg Sports Traumatol Arthrosc. 2017;25(2):517–523. [DOI] [PubMed] [Google Scholar]
- 14. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocations: a 2-9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1013–1026. [DOI] [PubMed] [Google Scholar]
- 17. Eranki V, Begg C, Wallace B. Outcomes of operatively treated acute knee dislocations. Open Orthop J. 2010;4:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fanelli GC. Evaluation and treatment of the multiple ligament injured knee. Arthroscopy. 2003;19(suppl 1):30–37. [DOI] [PubMed] [Google Scholar]
- 19. Fanelli GC. Multiple ligament injured knee: initial assessment and treatment. Clin Sports Med. 2019;38(2):193–198. [DOI] [PubMed] [Google Scholar]
- 20. Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy. 1996;12(5):521–530. [DOI] [PubMed] [Google Scholar]
- 21. Fanelli GC, Orcutt DR, Edson CJ. The multiple-ligament injured knee: evaluation, treatment, and results. Arthroscopy. 2005;21(4):471–486. [DOI] [PubMed] [Google Scholar]
- 22. Fetzer GB, Spindler KP, Amendola A, et al. Potential market for new meniscus repair strategies: evaluation of the MOON cohort. J Knee Surg. 2009;22(3):180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fok AW, Yau WP. Delay in ACL reconstruction is associated with more severe and painful meniscal and chondral injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):928–933. [DOI] [PubMed] [Google Scholar]
- 24. Frassica FJ, Sim FH, Staeheli JW, Pairolero PC. Dislocation of the knee. Clin Orthop Relat Res. 1991;263:200–205. [PubMed] [Google Scholar]
- 25. Freeman M, Tukey J. Transformations related to the angular and the square root. Ann Math Stats. 1950;21(4):607–611. [Google Scholar]
- 26. Freychet B, Kennedy NI, Sanders TL, et al. No difference between single and staged posterolateral corner surgical procedures in the multiligament injured/dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2170–2176. [DOI] [PubMed] [Google Scholar]
- 27. Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59(2):236–239. [PubMed] [Google Scholar]
- 28. Guess TM, Razu S. Loading of the medial meniscus in the ACL deficient knee: a multibody computational study. Med Eng Phys. 2017;41:26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Guess TM, Razu SS, Kuroki K, Cook JL. Function of the anterior intermeniscal ligament. J Knee Surg. 2018;31(1):68–74. [DOI] [PubMed] [Google Scholar]
- 30. Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86(2):262–273. [DOI] [PubMed] [Google Scholar]
- 31. Herbst E, Hoser C, Gföller P, et al. Impact of surgical timing on the outcome of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;25(2):569–577. [DOI] [PubMed] [Google Scholar]
- 32. Hirschmann MT, Iranpour F, Muller W, Friederich NF. Surgical treatment of complex bicruciate knee ligament injuries in elite athletes: what long-term outcome can we expect? Am J Sports Med. 2010;38(6):1103–1109. [DOI] [PubMed] [Google Scholar]
- 33. Hohmann E, Glatt V, Tetsworth K. Early or delayed reconstruction in multi-ligament knee injuries: a systematic review and meta-analysis. Knee. 2017;24(5):909–916. [DOI] [PubMed] [Google Scholar]
- 34. Hongwu Z, Li J. One-stage arthroscopic reduction combined with multiligament reconstruction or repair for irreducible posterolateral knee dislocation: a retrospective case series with minimum 2-year follow-up. J Knee Surg. 2018;31(10):1015–1021. [DOI] [PubMed] [Google Scholar]
- 35. Hua X, Tao H, Fang W, Tang J. Single-stage in situ suture repair of multiple-ligament knee injury: a retrospective study of 17 patients (18 knees). BMC Musculoskelet Disord. 2016;17:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ibrahim SA, Ahmad FH, Salah M, Al Misfer AR, Ghaffer SA, Khirat S. Surgical management of traumatic knee dislocation. Arthroscopy. 2008;24(2):178–187. [DOI] [PubMed] [Google Scholar]
- 37. Jenkins PJ, Clifton R, Gillespie GN, Will EM, Keating JF. Strength and function recovery after multiple-ligament reconstruction of the knee. Injury. 2011;42(12):1426–1429. [DOI] [PubMed] [Google Scholar]
- 38. Khakha RS, Day AC, Gibbs J, et al. Acute surgical management of traumatic knee dislocations—average follow-up of 10 years. Knee. 2016;23(2):267–275. [DOI] [PubMed] [Google Scholar]
- 39. Kiapour AM, Demetropoulos CK, Kiapour A, et al. Strain response of the anterior cruciate ligament to uniplanar and multiplanar loads during simulated landings: implications for injury mechanism. Am J Sports Med. 2016;44(8):2087–2096. [DOI] [PubMed] [Google Scholar]
- 40. King AH, Krych AJ, Prince MR, Pareek A, Stuart MJ, Levy BA. Surgical outcomes of medial versus lateral multiligament-injured, dislocated knees. Arthroscopy. 2016;32(9):1814–1819. [DOI] [PubMed] [Google Scholar]
- 41. King AH, Krych AJ, Prince MR, Sousa PL, Stuart MJ, Levy BA. Are meniscal tears and articular cartilage injury predictive of inferior patient outcome after surgical reconstruction for the dislocated knee? Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3008–3011. [DOI] [PubMed] [Google Scholar]
- 42. Kosy JD, Matteliano L, Rastogi A, Pearce D, Whelan DB. Meniscal root tears occur frequently in multi-ligament knee injury and can be predicted by associated MRI injury patterns. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3731–3737. [DOI] [PubMed] [Google Scholar]
- 43. Krych AJ, Sousa PL, King AH, Engasser WM, Stuart MJ, Levy BA. Meniscal tears and articular cartilage damage in the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3019–3025. [DOI] [PubMed] [Google Scholar]
- 44. Levine JW, Kiapour AM, Quatman CE, et al. Clinically relevant injury patterns after an anterior cruciate ligament injury provide insight into injury mechanisms. Am J Sports Med. 2013;41(2):385–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430–438. [DOI] [PubMed] [Google Scholar]
- 46. Levy BA, Krych AJ, Shah JP, Morgan JA, Stuart MJ. Staged protocol for initial management of the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2010;18(12):1630–1637. [DOI] [PubMed] [Google Scholar]
- 47. Levy NM, Krych AJ, Hevesi M, et al. Does age predict outcome after multiligament knee reconstruction for the dislocated knee? 2- to 22-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3003–3007. [DOI] [PubMed] [Google Scholar]
- 48. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):117–124. [DOI] [PubMed] [Google Scholar]
- 50. Lind M, Nielsen TG, Behrndtz K. Both isolated and multi-ligament posterior cruciate ligament reconstruction results in improved subjective outcome: results from the Danish Knee Ligament Reconstruction Registry. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1190–1196. [DOI] [PubMed] [Google Scholar]
- 51. Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85(6):845–851. [PubMed] [Google Scholar]
- 52. Lustig S, Leray E, Boisrenoult P, et al. Dislocation and bicruciate lesions of the knee: epidemiology and acute stage assessment in a prospective series. Orthop Traumatol Surg Res. 2009;95(8):614–620. [DOI] [PubMed] [Google Scholar]
- 53. Magnussen RA, Granan LP, Dunn WR, et al. Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 55. McDonald LS, Boorman-Padgett J, Kent R, et al. ACL deficiency increases forces on the medial femoral condyle and the lateral meniscus with applied rotatory loads. J Bone Joint Surg Am. 2016;98(20):1713–1721. [DOI] [PubMed] [Google Scholar]
- 56. Mehl J, Otto A, Baldino JB, et al. The ACL-deficient knee and the prevalence of meniscus and cartilage lesions: a systematic review and meta-analysis (CRD42017076897). Arch Orthop Trauma Surg. 2019;139(6):819–841. [DOI] [PubMed] [Google Scholar]
- 57. Moatshe G, Dornan GJ, Ludvigsen T, Loken S, LaPrade RF, Engebretsen L. High prevalence of knee osteoarthritis at a minimum 10-year follow-up after knee dislocation surgery. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3914–3922. [DOI] [PubMed] [Google Scholar]
- 58. Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91(12):2946–2957. [DOI] [PubMed] [Google Scholar]
- 59. Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med. 1997;25(6):769–778. [DOI] [PubMed] [Google Scholar]
- 60. Noyes FR, Barber-Westin SD. Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy. 2012;28(1):123–130. [DOI] [PubMed] [Google Scholar]
- 61. Owens BD, Neault M, Benson E, Busconi BD. Primary repair of knee dislocations: results in 25 patients (28 knees) at a mean follow-up of four years. J Orthop Trauma. 2007;21(2):92–96. [DOI] [PubMed] [Google Scholar]
- 62. Peskun CJ, Levy BA, Fanelli GC, et al. Diagnosis and management of knee dislocations. Phys Sportsmed. 2010;38(4):101–111. [DOI] [PubMed] [Google Scholar]
- 63. Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30(5):718–727. [DOI] [PubMed] [Google Scholar]
- 64. Rochcongar G, Cucurulo T, Ameline T, et al. Meniscal survival rate after anterior cruciate ligament reconstruction. Orthop Traumatol Surg Res. 2015;101(8):S323–S326. [DOI] [PubMed] [Google Scholar]
- 65. Roman PD, Hopson CN, Zenni EJ, Jr. Traumatic dislocation of the knee: a report of 30 cases and literature review. Orthop Rev. 1987;16(12):917–924. [PubMed] [Google Scholar]
- 66. Sanders TL, Johnson NR, Levy NM, et al. Effect of vascular injury on functional outcome in knees with multi-ligament injury: a matched-cohort analysis. J Bone Joint Surg Am. 2017;99(18):1565–1571. [DOI] [PubMed] [Google Scholar]
- 67. Schilaty ND, Bates NA, Krych AJ, Hewett TE. Frontal plane loading characteristics of medial collateral ligament strain concurrent with anterior cruciate ligament failure. Am J Sports Med. 2019;47(9):2143–2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Skendzel JG, Sekiya JK, Wojtys EM. Diagnosis and management of the multiligament-injured knee. J Orthop Sports Phys Ther. 2012;42(3):234–242. [DOI] [PubMed] [Google Scholar]
- 69. Spindler KP, Kuhn JE, Dunn W, Matthews CE, Harrell FE, Jr, Dittus RS. Reading and reviewing the orthopaedic literature: a systematic, evidence-based medicine approach. J Am Acad Orthop Surg. 2005;13(4):220–229. [DOI] [PubMed] [Google Scholar]
- 70. Subbiah M, Pandey V, Rao SK, Rao S. Staged arthroscopic reconstructive surgery for multiple ligament injuries of the knee. J Orthop Surg (Hong Kong). 2011;19(3):297–302. [DOI] [PubMed] [Google Scholar]
- 71. Talbot M, Berry G, Fernandes J, Ranger P. Knee dislocations: experience at the Hopital du Sacre-Coeur de Montreal. Can J Surg. 2004;47(1):20–24. [PMC free article] [PubMed] [Google Scholar]
- 72. Tandogan RN, Taşer Ö, Kayaalp A, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2003;12(4):262–270. [DOI] [PubMed] [Google Scholar]
- 73. Tao J, Li X, Zhou Z, Zhu Z. Acute single-stage reconstruction of multiligament knee injuries using the ligament advanced reinforcement system. Med Princ Pract. 2013;22(4):373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Tardy N, Boisrenoult P, Teissier P, Steltzlen C, Beaufils P, Pujol N. Clinical outcomes after multiligament injured knees: medial versus lateral reconstructions. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):524–531. [DOI] [PubMed] [Google Scholar]
- 75. Twaddle BC, Bidwell TA, Chapman JR. Knee dislocations: where are the lesions? A prospective evaluation of surgical findings in 63 cases. J Orthop Trauma. 2003;17(3):198–202. [DOI] [PubMed] [Google Scholar]
- 76. Tzurbakis M, Diamantopoulos A, Xenakis T, Georgoulis A. Surgical treatment of multiple knee ligament injuries in 44 patients: 2-8 years follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):739–749. [DOI] [PubMed] [Google Scholar]
- 77. Wajsfisz A, Bajard X, Plaweski S, et al. Surgical management of combined anterior or posterior cruciate ligament and posterolateral corner tears: for what functional results? Orthop Traumatol Surg Res. 2014;100(8):S379–S383. [DOI] [PubMed] [Google Scholar]
- 78. Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27(2):189–196. [DOI] [PubMed] [Google Scholar]
- 79. Werner BC, Hadeed MM, Gwathmey FW, Jr, Gaskin CM, Hart JM, Miller MD. Medial injury in knee dislocations: what are the common injury patterns and surgical outcomes? Clin Orthop Relat Res. 2014;472(9):2658–2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Wilson SM, Mehta N, Do HT, Ghomrawi H, Lyman S, Marx RG. Epidemiology of multiligament knee reconstruction. Clin Orthop Relat Res. 2014;472(9):2603–2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Woodmass JM, Johnson NR, Mohan R, Krych AJ, Levy BA, Stuart MJ. Poly-traumatic multi-ligament knee injuries: is the knee the limiting factor? Knee Surg Sports Traumatol Arthrosc. 2018;26(9):2865–2871. [DOI] [PubMed] [Google Scholar]
- 82. Wyatt RWB, Inacio MCS, Bellevue KD, Schepps AL, Maletis GB. Isolated ACL versus multiple knee ligament injury: associations with patient characteristics, cartilage status, and meniscal tears identified during ACL reconstruction. Phys Sportsmed. 2017;45(3):323–328. [DOI] [PubMed] [Google Scholar]
- 83. Yeh WL, Tu YK, Su JY, Hsu RW. Knee dislocation: treatment of high-velocity knee dislocation. J Trauma. 1999;46(4):693–701. [DOI] [PubMed] [Google Scholar]
- 84. Zhang K, Li L, Yang L, et al. The biomechanical changes of load distribution with longitudinal tears of meniscal horns on knee joint: a finite element analysis. J Orthop Surg Res. 2019;14(1):237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Zhang Y, Zhang X, Hao Y, Zhang YM, Wang M, Zhou Y. Surgical management of the multiple-ligament injured knee: a case series from Chongqing, China and review of published reports. Orthop Surg. 2013;5(4):239–249. [DOI] [PMC free article] [PubMed] [Google Scholar]