Abstract
Nurses provide the majority of health care in sub-Saharan Africa, which has high rates of Hepatitis B Virus (HBV) and human immunodeficiency virus (HIV). This systematic review used PRISMA methodology to synthesize the literature published between January 2008 and December 2018 examining the occupational health of nurses practicing in the Economic Community of West African States (ECOWAS). The United States’ National Institute for Occupational Safety and Health’s Hierarchy of Controls is used to frame the findings. This research was mostly conducted in Nigeria and Ghana and focused on administrative controls. Nurses practicing in ECOWAS are at high risk of acquiring a bloodborne illness due to inadequate engineering and administrative controls, as well as limited access to personal protective equipment (PPE). These findings indicate interventions to improve these controls would likely lower the occupational risks faced by nurses practicing in ECOWAS. Research in more countries in ECOWAS would likely find differences in occupational health practices in Nigeria and Ghana, which are relatively wealthy, and other countries in the region. This literature showed nurses practicing in ECOWAS did not have adequate protection from biological hazards. Regional health groups, such as the West African Health Organization, should commit to improving occupational health practice. Needle recapping and double gloving must be discontinued, and PPE must be made more widely available in ECOWAS. Occupational health professionals in the region should advocate for better distribution of PPE and consider offering trainings on these behaviors.
Keywords: global occupational health, national institute of occupational safety and health (NIOSH), government regulation, immunizations, occupational hazards, occupational injuries, built environment
Background and Significance
Nurses are the largest cadre of health care workers (HCWs) in the world and provide the majority of care in sub-Saharan Africa (Goosby and von Zinkernagel, 2014). Of the approximately one billion people who live in sub-Saharan Africa, about 360 million live within the Economic Community of West African States (ECOWAS, 2016), a West African regional group of 15 member states. ECOWAS was founded in 1975 to promote economic cooperation within the West African region, and oversees the West African Health Organization (WAHO). Two member states of ECOWAS, Ghana and Guinea, have signed the Nursing Personnel Convention of 1977 (International Labor Organization, 1979), which commits member states to “employment and working conditions,” which are likely to attract and retain nurses (United Nations, International Labor Organization, 1979).
Sub-Saharan Africa has a high burden of bloodborne pathogens, such as Hepatitis B Virus (HBV) and Hepatitis C, relative to other parts of the world (Barth, Huijgen, Taljaard, & Hoepelman, 2010). Approximately 4.5 million people in the ECOWAS region are infected with human immunodeficiency virus (HIV), and fewer than half of those infected are taking antiretroviral medications (WAHO, 2016). One estimate of the 12-month prevalence of blood and body fluid exposure among HCWs in the West African region was 47.9% (Auta et al., 2017). Thus, nurses working in ECOWAS are at significant risk of contracting a bloodborne illness. The issue of nurses’ occupational health is especially pressing in West Africa as the region seeks to develop its human resources for health (WAHO, 2016). The purpose of this work was to review and synthesize the literature on the occupational health of nurses in the ECOWAS region with particular attention to the risk they face of acquiring bloodborne illnesses.
Theoretical Framework
This review used the theoretical framework of the United States’ National Institute for Occupational Safety and Health’s (NIOSH, 2016) Hierarchy of Controls to organize its results and identify gaps in the literature (Figure 1). The hierarchy ranks five approaches to hazard control in descending order of effectiveness: elimination, substitution, engineering, administrative controls, and personal protective equipment (PPE). This order also applies to the cost of these different approaches over time: while engineering controls may be more expensive to implement initially than changes in behavior or the provision of PPE, over time, up-front costs are amortized patient by patient, such that in long run less money is spent by health care organizations (NIOSH, 2016).
Figure 1. NIOSH’s hierarchy of controls.
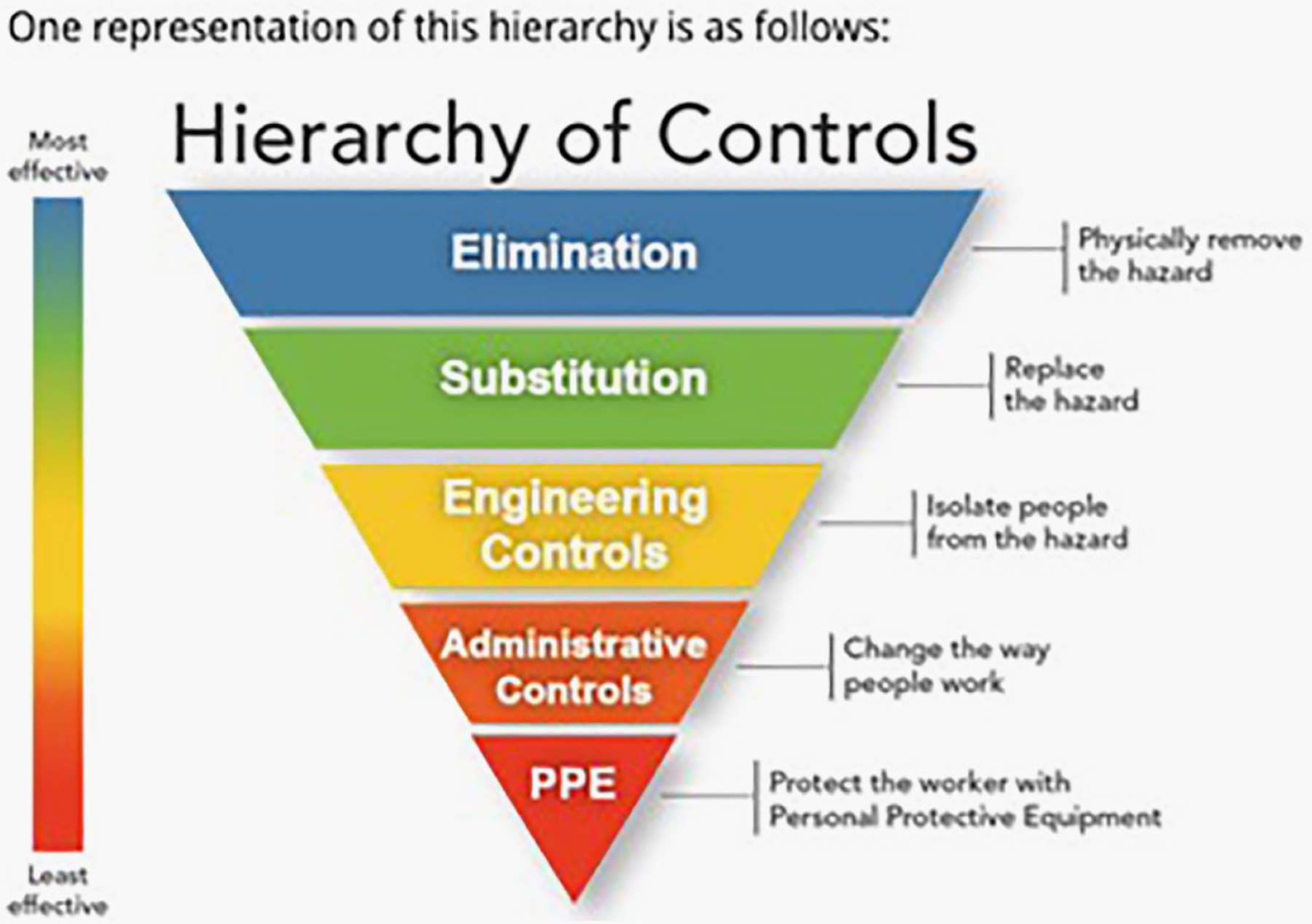
Source. NIOSH, Centers for Disease Control and Prevention, 2019.
Note. NIOSH = National Institute for Occupational Safety and Health.
In health care, exposure prevention typically relies on elimination, engineering controls, administrative controls, and PPE (Centers for Disease Control [CDC], 2010). Administrative controls affect the way a worker behaves around a hazard, and can also include trainings and workplace protocols (NIOSH, 2017). The Hierarchy of Controls does not address risk mitigation after exposure has taken place, but we reviewed that issue, as well.
Method
Four databases were searched from October to December 2018: PubMed, CINAHL, EMBASE, and PsychInfo. Search terms used included Africa, nus*, nurses, occupational health, needle stick, needle stick injuries, universal precautions, and sharps. A reference librarian with expertise in biomedical research was consulted in conducting the search. Fives articles had been identified previously via hand searching. Inclusion criteria included that the paper was published on or after January 2008, it was written in English, it addressed at least one element of the Hierarchy of Controls, it pertained to licensed nurses currently working in a health care setting, and it appeared in a peer-reviewed journal. Exclusion criteria were that the paper pertained to an African country outside of ECOWAS, that it focused on psychosocial or ergonomic hazards, and that it did not report results specific to licensed nurses. Single case studies were also excluded, as were articles specific to the Ebola epidemic of 2014–2015, because that epidemic had unique circumstances and dynamics. As we wanted a search as comprehensive as possible, no quality assessment of the articles was completed. Once the searches were completed, a PRISMA (Figure 2) approach was employed to identity articles for final inclusion.
Figure 2.
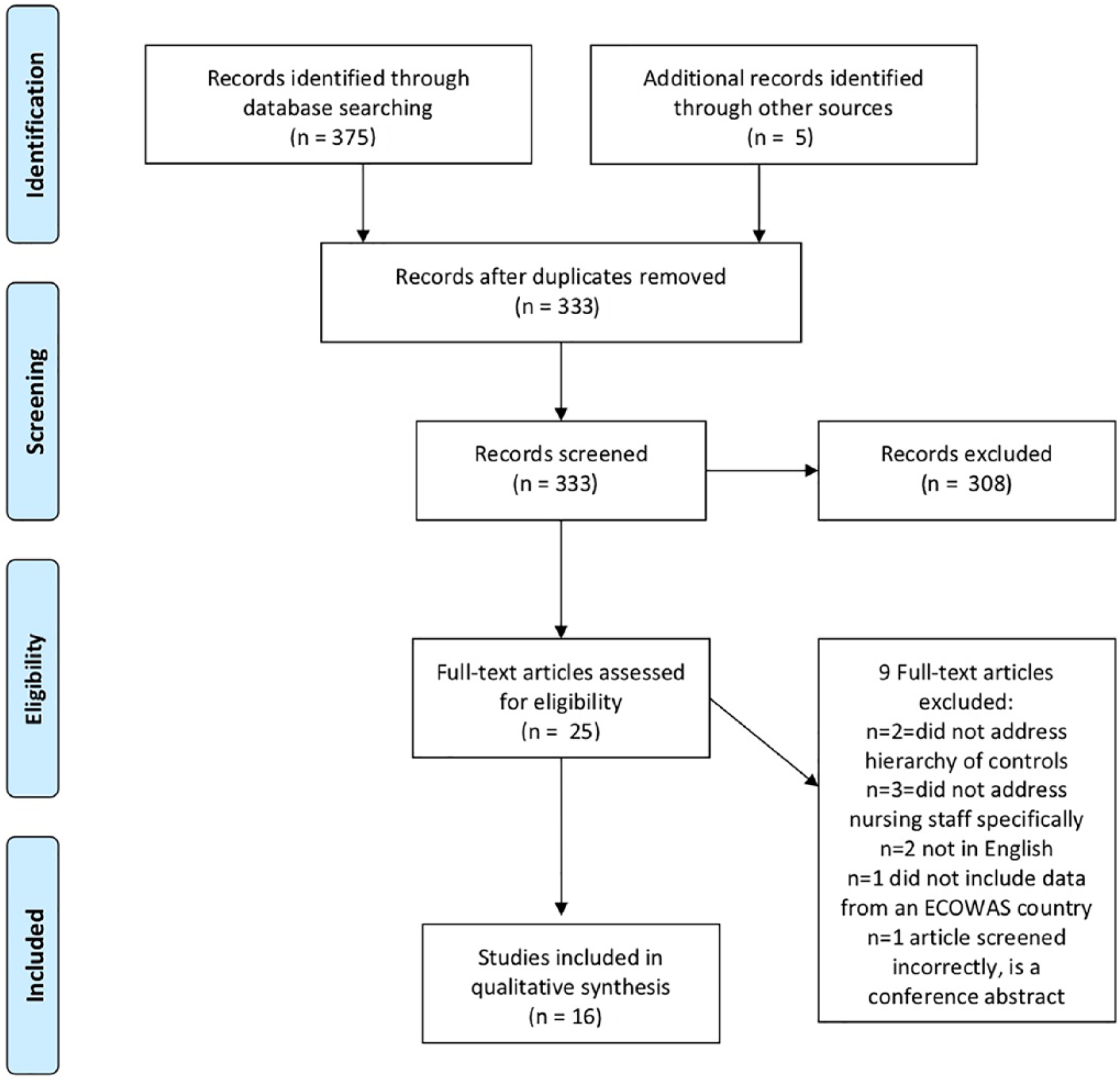
PRISMA flow diagram of studies pertaining to the occupational health of nurses in Economic Community of West African States.
Results
Sixteen papers were included in the final review (Table 1). Twelve papers examined nurses’ occupational health in Nigeria (Abiola et al., 2016; Adinma, Ezeama, Adinma, & Asuzu, 2009; Amira & Awobusuyi, 2014; Arinze-Onyia, Ndu, Aguwa, Modebe, & Nwamoh, 2018; Egwuenu & Okanlawon, 2014; Enwere & Diwe, 2014; Iliyasu et al., 2016; Isara & Ofili, 2010; Ogoina et al., 2014; Olatunji, Adejumo, & Adejumo, 2009; Omorogbe, Omuemu, & Isara, 2012; Onadeko, Balogun, Onigbogi, & Omokhodion, 2017). Of the remaining four studies, three were from Ghana (Konlan, Aarah-Bapuah, Kombat, & Wuffele, 2017; Lori, McCullagh, Krueger, & Oteng, 2016; Yawson & Hesse, 2013) and one was from Sierra Leone (Kingham, Kamara, Daoh, Kabbia, & Kushner, 2009).
Table 1.
Included Studies Addressing Nurses’ Occupational Health With a Focus on Exposure to Bloodborne Illnesses in the Economic Community of West African States
| Author/year | Country | Method | Sample size | Element of hierarchy of controls | Key findings |
|---|---|---|---|---|---|
| Abiola et al., 2016 | Nigeria | Cross-sectional survey, self-administered | 134 HCWs | Administrative |
|
| Adinma, Ezeama, Adinma, & Asuza, 2009 | Nigeria | Cross-sectional survey, self-administered | 178 HCWs; 112 nurses | Engineering, administrative, PPE |
|
| Amira & Awobusuyi, 2014 | Nigeria | Cross-sectional survey, self-administered | 102 HCWs; 42 nurses | Administrative |
|
| Arinze-Onyia, Ndu, Aguwa, Modebe, & Mwamoh, 2018 | Nigeria | Cross-sectional survey, self-administered | 629 HCWs; 290 nurses | Administrative, PPE |
|
| Egwuenu & Okanlawon, 2014 | Nigeria | Cross-sectional survey, self-administered | 231 nurses | Administrative |
|
| Enwere & Diwe, 2014 | Nigeria | Cross-sectional survey, self-administered | 156 HCWs; 98 nurses | Engineering, administrative |
|
| Iliyasu et al., 2016 | Nigeria | Cross-sectional survey, self-administered | 200 HCWs; 152 nurses | Administrative |
|
| Isara & Ofili, 2010 | Nigeria | Cross-sectional survey, self-administered | 167 HCWs; 100 nurses | Administrative |
|
| Kingham, Kamara, Daoh, Kabbia, & Kushner, 2009 | Sierra Leone | Cross-sectional survey of equipment | 10 facilities | Engineering, PPE |
|
| Konlan, Aarah- Bapuah, Kombat, & Wuffele, 2017 | Ghana | Cross-sectional survey, self-administered | 108 nurses | Administrative, PPE |
|
| Lori, McCullagh, Krueger, & Oteng, 2016 | Ghana | Mixed methods, including key informant interviews, self-administered survey, and document review | 45 nurses | Administrative |
|
| Ogoina et al., 2014 | Nigeria | Cross-sectional survey, self-administered | 381 HCWs; 220 nurses | Administrative |
|
| Olatunji, Adejumo, & Adejumo, 2009 | Nigeria | Cross-sectional survey, self-administered | 275 nurses | Administrative |
|
| Omorogbe, Omuemu, & Isara, 2012 | Nigeria | Cross-sectional survey, interview administered | 122 nurses | Administrative |
|
| Onadeko, Balogun, Onigbogi, & Omokhodian, 2017 | Nigeria | Cross-sectional survey, self-administered | 977 HCWs; 405 nurses | Administrative |
|
| Yawson & Hesse, 2013 | Ghana | Cross-sectional survey via direct observation | 15 facilities | Engineering, Administrative |
|
Note. PPE = personal protective equipment; PEP = postexposure prophylaxis; OR = odds ratio; HCW = health care worker; HIV = human immunodeficiency virus; HBV = hepatitis B virus; NSI = needle stick injury; BBP = bloodborne pathogen.
All but two of the studies used a cross-sectional survey design in which health care providers answered questionnaires about knowledge, attitudes, or practices germane to occupational health. Of these 14, three studies focused on knowledge, attitudes, or practices pertinent to HBV vaccination (Abiola et al., 2016; Konlan et al., 2017; Ogoina et al., 2014). Six studies focused on knowledge, attitudes, or practices pertinent to universal or standard precautions (Adinma et al., 2009; Arinze-Onyia et al., 2018; Egwuenu & Okanlawon, 2014; Iliyasu et al., 2016; Isara & Ofili, 2010; Olatunji et al., 2009). Four studies focused on knowledge, attitudes, or practices pertinent to injection safety (Amira & Awobusuyi, 2014; Enwere & Diwe, 2014; Lori et al., 2016; Omorogbe et al., 2012). One examined a variety of behaviors of health care providers specifically in the context of caring for patients with HIV (Onadeko et al., 2017). All but one survey used self-administered questionnaires: Omorogbe et al. (2012) used an interviewer-administered questionnaire as well as an observational checklist. Lori et al. (2016) conducted a mixed-methods study in which key informant interviews and document review were included in addition to the survey.
The remaining two studies were also cross-sectional in design. Kingham et al. (2009) conducted a survey of the equipment available at 10 hospitals in Sierra Leone using the World Health Organization’s Tool for Situational Analysis to Assess Emergency and Essential Surgical Care. Yawson and Hesse (2013) used direct observation to examine hand-washing practices at a teaching hospital in Ghana.
Elimination, substitution, and engineering controls
None of the 16 studies examined elimination or substitution (e.g., substituting an oral medication for an intravenous medication to reduce the risk of exposure via needlestick) as a way of managing exposure to biological hazards. Four examined facilities’ engineering-based controls (Adinma et al., 2009; Enwere & Diwe, 2014; Kingham et al., 2009; Yawson & Hesse, 2013). Two of these examined the infrastructure needed for proper hand hygiene. Yawson and Hesse’s (2013) survey of hand hygiene practices found that of the 15 Ghanaian units surveyed, all had running water, although other controls, such as alcohol gel and single-use towels, were frequently missing (Yawson and Hesse, 2013). By contrast, Adinma et al. (2009) in Nigeria found that 46.4% of nurses reported that insufficient water supply was a factor affecting their use of universal precautions.
Two other studies examined engineering controls outside the context of hand hygiene. Enwere and Diwe (2014) noted that although the teaching hospital they were studying had color-coded bins for needle disposal, only 54% of nurses were aware of them. Kingham et al.’s (2009) survey reviewed the availability of equipment needed for safe surgery in Sierra Leone. It found that only 50% of government hospitals had functioning sterilizers and sharps containers available for use. By contrast, all of the faith-based and nongovernmental hospitals previously surveyed had these controls available (Kingham et al., 2009).
Administrative controls
Administrative, or behavioral, controls was the topic examined most often in this literature. Fifteen of the 16 papers addressed these controls, with the only exception being Kingham et al. (2009). The most common topics were vaccination, universal or standard precautions, and injection safety. Although each paper had an overarching research topic (e.g., universal precautions, injection safety), they often explored more than one occupational health behavior.
HBV vaccination was the focus of in three studies (Abiola et al., 2016; Konlan et al., 2017; Ogoina et al., 2014). Two of these were conducted in Nigeria (Abiola et al., 2016; Ogoina et al., 2014) one in Ghana (Konlan et al., 2017). All identified serious gaps in knowledge, attitudes, or practice pertinent to HBV vaccination. All three found low rates of HBV vaccination: Abiola et al. (2016) reported the highest rate of vaccination at 48.5% of HCWs receiving the necessary three doses; Konlan et al. (2017) found the lowest at 33.3%. Ogoina et al. (2014), who found 36.2% of HCWs had received three doses, also reported that 32.5% of HCWs had received zero doses. Abiola et al. (2016) found a statistically significant relationship between professional cohort and HBV vaccine practice; nurses were more likely to have good vaccine practice than physicians (p = .05). By contrast, Ogoina et al., (2014) found that while nurses were more likely to be vaccinated than house officers, there was no statistically significant difference between nurses’ vaccination rates and those of resident or consulting physicians. Abiola et al. (2016) found only 56.3% of nurses had good knowledge of HBV infection and appropriate vaccination practices, although the exact knowledge tested was not clear. Konlan et al. (2017), in Ghana, found that only 12.1% of nurses had adequate knowledge of postexposure prophylaxis (PEP) for HBV.
Six studies focused explicitly on knowledge, attitudes, or practices pertinent to universal or standard precautions (Adinma et al., 2009; Arinze-Onyia et al., 2018; Egwuenu & Okanlawon, 2014; Iliyasu et al., 2016; Isara & Ofili, 2010; Olatunji et al., 2009). All were conducted in Nigeria. The term “standard precautions” covers a wide range of behaviors (CDC, 2011); these studies tended to focus on four topics: hand washing, use of protective barriers, and safe use and disposal of sharps. High levels of awareness of standard precautions were reported consistently, with a range of 94.4% (Arinze-Onyia et al., 2018) to 82% (Isara & Ofili, 2010) of HCWs reporting they had ever heard of standard precautions. Isara and Ofili (2010) reported no statistically significant difference in knowledge of standard precautions between different health professions (p = .129); Adinma et al. (2009) found that both 97% of physicians and 92% of nurses had a high level of awareness of standard precautions and did not test to see if the difference was statistically significant. Iliyasu et al. (2016), by contrast, reported that nurses were significantly more likely to have good knowledge of infection transmission than physicians (p = .001). Only one study (Arinze-Onyia et al., 2018) surveyed attitudes to standard precautions, and found them to be generally positive: 94.5% of HCWs either agreed or strongly agreed that standard precautions were useful for protecting against hazards.
Measures of the practice of standard precautions varied across studies. Adinma et al. (2009) found that 66.1% of nurses practiced standard precautions always. Reported rates of hand washing varied. Egwuenu and Okanlawon (2014) found that 80% of nurses reported consistently washing hands after patient care, whereas Isara and Ofili (2010) found 97%. Iliyasu et al. (2016) found that nurses were significantly more likely to wash their hands between patients than physicians (p = .02). Yawson and Hesse (2013), who directly observed nurses, found they washed their hands 60%–87% of the time after touching a patient, depending on the patient care setting. The survey also noted that nurses almost never adhered to the 40–60 second, recommended time frame for hand washing despite having access to most of the needed equipment (Yawson & Hesse, 2013).
The use of gloves was surprising: Isara and Ofili (2010) found that only 75% of nurses wear gloves when assisting with a birth, a finding consistent with Egwuenu and Okanlawon’s (2014) that only 45.9% of nurses wear gloves when they expect to come in contact with blood or body fluids. Olatunji et al. (2009), by contrast, found that 94.2% of nurses always used a protective barrier when providing care, but the difference can perhaps be explained by the fact that Olatunji et al. (2009) focused specifically on nurses providing care to people living with HIV. Isara and Ofili (2010) also reported 62% of nurses used double gloves at least some of the time. Omorogbe el al. (2012) also found that only 3.3% of nurses use gloves regularly when administering an injection; 68.9% do so sometimes.
Four studies focused on knowledge, attitudes, or practices pertinent to injection safety (Amira & Awobusuyi, 2014; Enwere & Diwe, 2014; Lori et al., 2016; Omorogbe et al., 2012); all but Lori et al. (2016) were conducted in Nigeria. These studies examined the frequency of needle stick injuries among HCWs in the past 12 months with very similar findings: 24.5% (Amira & Awobusuyi, 2014), 24.6% (Omorogbe et al., 2012), and 28.9% (Lori et al., 2016). Lori et al. (2016) also found that 36.3% of the nurses who experienced a needle stick injury in the past 12 months had experienced four or more such injuries in that period. Needle recapping, a fairly common behavior, had reported rates between 44.8% (Enwere & Diwe, 2014) and 75% (Arinze-Onyia et al., 2018). Amira and Awobusuyi (2014) found that needle recapping was the behavior leading to 45% of needle stick injuries.
PPE
Four studies discussed the amount of PPE available to HCWs by their employers and whether or not it was adequate for care (Adinma et al., 2009; Arinze-Onyia et al., 2018; Kingham et al., 2009; Konlan et al., 2017). All found a dearth of PPE supplies in practice settings. Konlan et al. (2017) found that only half of nurses (51.9%) described the glove supply as adequate; similarly, 57.7% of HCWs surveyed by Arinze-Onyia et al. (2018) reported that they did not have regular access to PPE. Similarly, Adinma et al. (2009) reported that 82.1% of nurses cited a lack of PPE supplies as a reason they sometimes did not follow standard precaution guidelines.
Kingham et al. (2009) examined the issue quantitatively in Sierra Leone by surveying government hospitals, where the majority of care is provided in that country, to assess for the presence or absence of needed surgical equipment. Only one in five of the government facilities surveyed had access to eye protection and sterile gloves, while other surveys had shown that the faith-based and nongovernmental hospitals were fully stocked (Kingham et al., 2009).
Postexposure Prophylaxis (PEP)
Nine studies examined how HCWs responded after an exposure to biological hazards (Amira & Awobusuyi, 2014; Enwere & Diwe, 2014; Iliyasu et al., 2016; Konlan et al., 2017; Lori et al., 2016; Olatunji et al., 2009; Omorogbe et al., 2012; Onadeko et al., 2017; Yawson & Hesse, 2013). Olatunji et al. (2009) examined PEP specifically in the context of caring for patients with HIV. Ways to mitigate risk, which were examined in this literature, were washing the exposed area, reporting the exposure to a supervisor, and, when possible and appropriate, accessing PEP.
Washing the exposed area was a surprisingly infrequent behavior: between 16.2% of nurses practicing in the surgical ward and 29.8% in the NICU washed their hands after a blood or body fluid exposure (Yawson & Hesse, 2013). Amira and Awobusuyi (2014) found that only 37% of HCWs reported their needle stick injuries to a supervisor; Konlan et al. (2017) found that 64.8% of nurses reported. Lori et al. (2016) found that while their facility protocol recommended testing nurses for HIV postexposure, the protocol did not mention HBV testing. Reported knowledge rates of PEP were low, and ranged from 58% of nurses reporting that PEP must begin with 72 hours (Iliyasu et al., 2016) to 69.4% of nurses reporting that PEP should be taken as early as possible to maximize effectiveness (Konlan et al., 2017).
Reported rates of HCWs actually obtaining PEP were all fairly low: Enwere and Diwe (2014) found that 25.6% of HCWs with a history of needle stick injury had obtained PEP (for which illness was not specified), Amira and Awobusuyi (2014) found that only 7.3% of HCWs received PEP for HIV, and 2.4% for HBV; Omorogbe et al. (2012) found the rate was only 0.6% (again, for which illness was not specified). 58.5% of nurses taking care of HIV-positive patients reported they never obtained PEP after a needlestick or sharps injury (Olatunji et al., 2009).
Use of theory
This is a largely atheoretical body of literature. Some internationally recognized tools pertaining to occupational health are used, such as the World Health Organization (WHO) Hand Hygiene Observation Method and WHO Hand Hygiene Technical Reference Manual (Yawson & Hesse, 2013), and the Occupational Safety and Health Administration’s (OSHA) bloodborne exposure standards (Lori et al., 2016).
Discussion
This literature review synthesized the literature of the last 11 years on the occupational health of nurses in the ECOWAS region, with particular attention to the literature pertinent to nurses’ risk of exposure to bloodborne illnesses. Taken together, this literature suggests there are serious threats to the occupational health of nurses in the ECOWAS region.
Except for Kingham et al.’s (2009) survey in Sierra Leone, all of these studies were conducted in either Nigeria or Ghana. Although those two countries are populated by about 209 million of ECOWAS’ 360 million people, this is nevertheless disproportionate and likely due to those countries’ relative prosperity. It seems probable that nurses in other, less wealthy ECOWAS countries, such as Liberia and Niger, face even larger obstacles to occupational health.
Three of the five levels of controls were examined in depth: engineering, administrative, and PPE. At each level, major gaps were found. At the engineering level, hand-washing stations were found to be lacking either running water or other important components such as towels. Moreover, sharps disposal containers were either absent or unknown to nursing staff (Enwere & Diwe, 2014; Kingham et al., 2009).
Administrative controls were also found to be limited. The high rate of needle stick injuries, found to have occurred between 24.5% (Amira & Awobusuyi, 2014) and 28.9% (Lori et al., 2016) of nurses in the past year, is consistent across these studies. It is also roughly consistent with the pooled rate of blood and body fluid exposures in West Africa of 47.9% reported by Auta et al (2017), when one considers that the Auta et al. (2017) estimate includes all exposures to blood and body fluids, not just needle stick injuries. Auta et al.’s (2017) inclusion of mucous membrane exposure, bites, and nonintact skin exposure highlights the fact these types of exposure do not appear in this literature despite their relevance to HIV and HBV transmission. As this rate of exposure is occurring in a region in which there is a high prevalence of bloodborne illnesses, including HIV and HBV, there is reason to consider the nurses practicing in ECOWAS highly vulnerable.
PPE was consistently found to be inadequate and its absence regularly impacted nurses’ ability to adhere to standard precautions. These findings are consistent with those from other studies conducted in sub-Saharan Africa that report that facilities have trouble obtaining PPE (Tudor, Van der Walt, Hill, & Farley, 2013) or that PPE is frequently reused during a shift because of inadequate supplies (Nderitu, Mill, & Richter, 2015). This is, of course, a threat to patients’ safety as well as to nurses.
Implications for Occupational Health Nursing Practice
Policy
The current WAHO strategic plan states a clear goal to develop human resources for health, but the plan does not mention supporting the occupational health of HCWs in the region (WAHO, 2016). This review of the literature makes it clear these HCWs are highly vulnerable and that future plans should include goals for minimizing occupational health risk. The United Nations placed the issue of occupational health at the center of the effort to recruit and retain more nurses in 1979 (United Nations, International Labor Organization, 1979) and affirmed in 2017 that poor working conditions contribute to a shortage of HCWs (World Health Organization, 2017). Thus, improving working conditions for HCWs within ECOWAS is an integral part of meeting WAHO’s strategic goals.
To improve the occupational health of nurses, policy changes should take place at the regional, or national, level, and at the level of individual facilities. Regionally, those member states of ECOWAS which do not yet have national occupational health regulations should develop and implement them, with special attention paid to HCWs. Policies supporting HCW vaccination, such as the provision of needed vaccines through the public health system and mandatory paid time off to receive vaccination, would also support worker health. Individual facilities should formulate policies mandating regular trainings on occupational health issues (e.g., standard precautions, HBV PEP) and offer those trainings accordingly.
Practice
This review suggests that many of the nurses practicing in ECOWAS do not have adequate protection from biological hazards. For the nurses themselves, simply demanding better conditions, such as more accessible PPE, is unlikely to be fruitful, as their governments are frequently highly constrained by limited budgets. It does seem, however, that certain trainings could improve occupational health by assisting nurses in using the resources that are already available to them. These trainings might include: safer handling of sharps, proper hand washing, or orienting nurses better to the engineering controls available in their facilities.
Another approach might be to partner with local or national nursing boards to develop facilities specifically meant to improve the occupational health of nurses, as has been seen in Swaziland and Lesotho (Carrier-Walker, 2011). This has the potential to be a highly efficient use of funds as such a center could serve several facilities at once and potentially make PEP, currently utilized by a small number of nurses, more broadly accessible.
Research
Based on the studies reviewed, there are four major avenues for occupational health research on nursing in the ECOWAS region. First, the topics in this literature (e.g., adherence to standard precautions, injection safety) should be examined in all ECOWAS countries. Except for Kingham et al. (2009), all of the studies included in this review were conducted in either Nigeria or Ghana. Thus, 12 of the 15 members states of ECOWAS are not represented in this literature, but are likely as vulnerable, or more so, to the same challenges. Second, this literature is aging rapidly; of the 16 studies included in this review, four were published in 2009 and 2010.
Third, there should be more research on the elimination and engineering levels of control. These two levels are both the most efficacious and the most cost effective, so they should be of particular interest in resource-constrained settings. However, they have received very little attention to date.
Fourth, this review has shed light on the dearth of research on occupational health interventions. Every study included was a cross-sectional look at current realities, and nearly every study found important gaps. It would be useful and informative for researchers to attempt to address these gaps by offering and evaluating some of the trainings discussed above, or other interventions they design. More interventions at the administrative level in the hierarchy of controls are of particular interest, given the spending constraints facing many of these governments.
Limitations
The studies included in this review had a number of limitations. Most relied on self-report survey methods. The accuracy of surveys is, of course, limited by the accuracy of the participants’ recollection. Asking for HCWs to recall the number of HBV vaccines they have obtained in the past, for example, is likely to result in a number of participants misreporting simply due to an inability to remember. Moreover, most researchers did not have the ability to actually perform follow-up HBV antibody testing to confirm immunity. Furthermore, studies that focus on the implementation of standard precautions are subject to social desirability bias as HCWs are typically aware of the “right” answer. This seems likely to be the case with these studies as surveys, which asked for nurses to self-report hand-washing practices (Egwuenu & Okanlawon, 2014; Isara & Ofili, 2010) found higher rates of hand washing after patient care than Yawson and Hesse (2013), who directly observed nurses. Surveys also cannot offer insight into the quality of adherence to precautions guidelines, such as length of hand washing or if PPE was donned or doffed correctly.
Conclusion
This review integrated the literature about the occupational health of nurses practicing in the ECOWAS region of sub-Saharan Africa since 2008. The articles included were almost entirely cross-sectional studies from three countries in the region. Collectively, they showed that nurses did not have sufficient protection from biological hazards. They demonstrated that though the risks of exposure and rates of exposure were high, there are major gaps throughout the hierarchy of controls, as well as in managing exposures. There is a clearly demonstrated need for regional health groups to focus on the occupational health of nurses, for trainings to be offered to improve current nurse practice, and for more research developing and evaluating interventions to address these gaps.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This publication was supported by Grant Number, T42OH008422, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Author Biographies
Laura Jean Ridge, MS, ANP-BC, AAHIVE, is a PhD candidate at Rory Meyers College of Nursing and a trainee in the NIOSH-funded doctoral training program in Occupation and Environmental Health Nursing. Her research focuses on nurses’ occupational health in lower- and middle-income countries.
Victoria Vaughan Dickson, PhD, RN, FAAN, is an associate professor in the Rory Meyers College of Nursing with extensive clinical and research experience in cardiovascular and occupational health nursing. She is the program director of the NIOSH-funded doctoral training program in occupational and environmental health nursing.
Amy Witkoski Stimpfel, PhD, RN, has been an assistant professor at the Rory Meyers College of Nursing since 2013 and co-directs the NIOSH-funded doctoral training program in Occupation and Environmental Health Nursing. Her research focuses on modifiable risk factors in nurses’ work environment influences and how they influence nurses’ well-being.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abiola A-HO, Agunbiade AB, Badmos KB, Lesi AO, Lawal AO, & Alli QO (2016). Prevalence of HBsAg, knowledge, and vaccination practice against viral hepatitis B infection among doctors and nurses in a secondary health care facility in Lagos state, South-western Nigeria. The Pan African Medical Journal, 23, Article 160. doi: 10.11604/pamj.2016.23.160.8710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adinma ED, Ezeama C, Adinma JIB, & Asuzu MC (2009). Knowledge and practice of universal precautions against blood borne pathogens amongst house officers and nurses in tertiary health institutions in Southeast Nigeria. Nigerian Journal of Clinical Practice, 12, 398–402. [PubMed] [Google Scholar]
- Amira CO, & Awobusuyi JO (2014). Needle-stick injury among health care workers in hemodialysis units in Nigeria: A multi-center study. The International Journal of Occupational and Environmental Medicine, 5(1), 1–8. [PMC free article] [PubMed] [Google Scholar]
- Arinze-Onyia SU, Ndu AC, Aguwa EN, Modebe I, & Nwamoh UN (2018). Knowledge and practice of standard precautions by health-care workers in a tertiary health institution in Enugu, Nigeria. Nigerian Journal of Clinical Practice, 21, 149–155. doi: 10.4103/njcp.njcp_69_17 [DOI] [PubMed] [Google Scholar]
- Auta A, Adewuyi EO, Tor-Anyiin A, Aziz D, Ogbole E, Ogbonna BO, & Adeloye D (2017). Health-care workers’ occupational exposures to body fluids in 21 countries in Africa: Systematic review and meta-analysis. Bulletin of the World Health Organization, 95, 831–841. doi: 10.2471/BLT.17.195735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth RE, Huijgen Q, Taljaard J, & Hoepelman AIM (2010). Hepatitis B/C and HIV in sub-Saharan Africa: An association between highly prevalent infectious diseases. A systematic review and meta-analysis. International Journal of Infectious Diseases: IJID: Official Publication of the International Society for Infectious Diseases, 14(12), e1024–1031. doi: 10.1016/j.ijid.2010.06.013 [DOI] [PubMed] [Google Scholar]
- Carrier-Walker L (2011). Focussing on the wellbeing of health care workers in sub-Saharan Africa. International Nursing Review, 58(3), 273–274. doi: 10.1111/j.1466-7657.2011.00933.x [DOI] [PubMed] [Google Scholar]
- Center for Disease Control. (2010). Interim guidance on infection control measures for 2009 H1N1 influenza in healthcare settings, including protection of healthcare personnel. Retrieved from https://www.cdc.gov/h1n1flu/guidelines_infection_control.htm [PubMed]
- Center for Disease Control. (2011). Basic infection control and prevention plan for outpatient oncology settings. Retrieved from https://www.cdc.gov/hai/pdfs/guidelines/basic-infection-control-prevention-plan-2011.pdf
- Economic Community of West African States. (2016). 2016 Annual report of ECOWAS. Retrieved from http://www.ecowas.int/wp-content/uploads/2017/11/Annual-Report-2016_English-Fina_Final.pdf
- Egwuenu SEO, & Okanlawon FA (2014). Infection control: Nurses’ knowledge and practice of universal precaution in Delta State, Nigeria. African Journal of Medicine and Medical Sciences, 43, 127–134. [PubMed] [Google Scholar]
- Enwere OO, & Diwe KC (2014). Knowledge, perception and practice of injection safety and healthcare waste management among teaching hospital staff in south east Nigeria: An intervention study. The Pan African Medical Journal, 17, Article 218. doi: 10.11604/pamj.2014.17.218.3084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goosby EP, & von Zinkernagel D (2014). The medical and nursing education partnership initiatives. Academic Medicine: Journal of the Association of American Medical Colleges, 89(8. Suppl), S5–S7. doi: 10.1097/ACM.0000000000000346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iliyasu G, Dayyab FM, Habib ZG, Tiamiyu AB, Abubakar S, Mijinyawa MS, & Habib AG (2016). Knowledge and practices of infection control among healthcare workers in a Tertiary Referral Center in North-Western Nigeria. Annals of African Medicine, 15, 34–40. 10.4103/1596-3519.161724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Labor Organization. (1979, July 11). Ratifications of C149—Nursing Personnel Convention, 1977 (No. 149). United Nations. Retrieved from https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:11300:0::NO::P11300_INSTRUMENT_ID:312294 [Google Scholar]
- Isara AR, & Ofili AN (2010). Knowledge and practice of standard precautions among health care workers in the federal medical centre, Asaba, delta state, Nigeria. The Nigerian Postgraduate Medical Journal, 17, 204–209. [PubMed] [Google Scholar]
- Kingham TP, Kamara TB, Daoh KS, Kabbia S, & Kushner AL (2009). Universal precautions and surgery in Sierra Leone: The unprotected workforce. World Journal of Surgery, 33, 1194–1196. doi: 10.1007/s00268-009-0014-6 [DOI] [PubMed] [Google Scholar]
- Konlan KD, Aarah-Bapuah M, Kombat JM, & Wuffele GM (2017). TOPIC: “The level of nurses” knowledge on occupational post exposure to hepatitis B infection in the Tamale metropolis, Ghana. BMC Health Services Research, 17(1), Article 254. doi: 10.1186/s12913-017-2182-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lori JR, McCullagh MC, Krueger A, & Oteng R (2016). Sharps injuries among emergency department nurses in one tertiary care hospital in Ghana. International Emergency Nursing, 28, 14–19. doi: 10.1016/j.ienj.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Institute for Occupational Safety and Health. (2016). Hierarchy of controls. Retrieved from https://www.cdc.gov/niosh/topics/hierarchy/default.html
- Nderitu EW, Mill J, & Richter S (2015). The experience of Ugandan nurses in the practice of universal precautions. The Journal of the Association of Nurses in AIDS Care: JANAC, 26, 625–638. doi: 10.1016/j.jana.2014.10.003 [DOI] [PubMed] [Google Scholar]
- Ogoina D, Pondei K, Adetunji B, Chima G, Isichei C, & Gidado S (2014). Prevalence of hepatitis B vaccination among health care workers in Nigeria in. The International Journal of Occupational and Environmental Medicine, 5, 51–56. [PMC free article] [PubMed] [Google Scholar]
- Olatunji OO, Adejumo PO, & Adejumo AO (2009). Constraints in nurses’ use of HIV protective barriers in the care of PLWHA in the University College Hospital, Ibadan, Nigeria. World Hospitals and Health Services : The Official Journal of the International Hospital Federation, 45(2), 27–30. [PubMed] [Google Scholar]
- Omorogbe VE, Omuemu VO, & Isara AR (2012). Injection safety practices among nursing staff of mission hospitals in Benin City, Nigeria. Annals of African Medicine, 11, 36–41. doi: 10.4103/1596-3519.91020 [DOI] [PubMed] [Google Scholar]
- Onadeko MO, Balogun MO, Onigbogi OO, & Omokhodion FO (2017). Occupational exposure, attitude to HIV-positive patients and uptake of HIV counselling and testing among health care workers in a tertiary hospital in Nigeria. SAHARA J : Journal of Social Aspects of HIV/AIDS Research Alliance, 14, 193–201. doi: 10.1080/17290376.2017.1398104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor C, Van der Walt M, Hill MN, & Farley JE (2013). Occupational health policies and practices related to tuberculosis in health care workers in KwaZulu-Natal, South Africa. Public Health Action, 3, 141–145. doi: 10.5588/pha.12.0098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations, International Labor Organization. (1979, August 11). Nursing Personnel Convention. Retrieved from ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_INSTRUMENT_ID:312294
- West African Health Organization. (2016). West African Health Organization Strategic Plan: 2016–2020. Retrieved from https://nigeriandocuments.blogspot.com/p/west-african-health-organisation-waho.html
- World Health Organization. (2017). Inter-country workshop on occupational safety and health in the preparedness and response to outbreaks and public health emergencies in Africa: Report. Retrieved from https://www.who.int/occupational_health/publications/intercountry_workshop_Africa_EN.pdf?ua=1
- Yawson AE, & Hesse AAJ (2013). Hand hygiene practices and resources in a teaching hospital in Ghana. Journal of Infection in Developing Countries, 7, 338–347. [DOI] [PubMed] [Google Scholar]


