Abstract
The cervical vertebral maturation (CVM) method is used to determine the craniofacial skeletal maturational stage of an individual at a specific time point during the growth process. This diagnostic approach uses data derived from the second (C2), third (C3), and fourth (C4) cervical vertebrae, as visualized in a two-dimensional lateral cephalogram. Six maturational stages of those three cervical vertebrae can be determined, based on the morphology of their bodies. The first step is to evaluate the inferior border of these vertebral bodies, determining whether they are flat or concave (ie, presence of a visible notch). The second step in the analysis is to evaluate the shape of C3 and C4. These vertebral bodies change in shape in a typical sequence, progressing from trapezoidal to rectangular horizontal, to square, and to rectangular vertical. Typically, cervical stages (CSs) 1 and CS 2 are considered prepubertal, CS 3 and CS 4 circumpubertal, and CS 5 and CS 6 postpubertal. Criticism has been rendered as to the reproducibility of the CVM method. Diminished reliability may be observed at least in part due to the lack of a definitive description of the staging procedure in the literature. Based on the now nearly 20 years of experience in staging cervical vertebrae, this article was prepared as a “user's guide” that describes the CVM stages in detail in attempt to help the reader use this approach in everyday clinical practice.
Keywords: CVM method, Cephalometrics, Maturation, Cervical vertebrae
INTRODUCTION
The level of craniofacial skeletal maturity in a given patient is important in identifying the optimal time to initiate orthodontic/orthopedic treatment of certain craniofacial skeletal imbalances.1–3 In dentofacial orthopedics, the issue of optimal timing is linked intimately to the identification of periods of favorable growth in structures such as the mandibular condyles or the circummaxillary sutures.4–6 Treatment timing during these favorable growth processes can contribute significantly to the efficient and effective improvement of skeletal problems in the individual patient.
Over the years, several types of indicators of individual skeletal maturity have been proposed to define treatment timing in orthodontics. Two of the most frequently used indicators are the chronological age of the patient7 and the stage of dentitional development.8–10 Some investigators have reported that chronological age can be regarded as a reliable predictor of the adolescent growth spurt.11,12 The circumpubertal growth spurt, however, is influenced not only by patient age but also by sex, genetics, ethnicity, nutrition, and socioeconomic status.12–14
Reliable indicators of individual skeletal maturity are three: increase in statural height,9 skeletal maturation of the hand and wrist,15,16 and changes in morphology of the cervical vertebrae.3,6,17 Although several investigations have demonstrated the essential role of treatment timing in the efficacy of different orthopedic approaches,4,5,18 the use of the first two indicators in everyday clinical practice currently is limited.
In contrast, modifications in size and shape of the cervical vertebrae in growing subjects have gained increasing interest during the past few decades as a biological indicator of individual skeletal maturity. Originally described by Lamparski in an unpublished master's thesis in 1972,19,20 the cervical vertebral maturation (CVM) method has become popular because the analysis of cervical vertebrae is performed on the lateral cephalogram, a type of radiograph routinely available for orthodontic diagnosis.
Although the CVM method originally was developed more than 4 decades ago, one obvious limitation so far is that, until now, there have been no published detailed descriptions of the CVM classification system, the stated intention of which is to teach the inexperienced practitioner how to use this staging method. In this paper, a detailed description of our approach to this diagnostic process is presented. The aim of this study, therefore, is to propose user-friendly guidelines to improve intra- and interobserver reliability and to facilitate the applicability of the CVM method to everyday clinical practice.
Guidelines for the Cervical Vertebral Maturation Method
The methodology presented in this paper is based on our experiences analyzing numerous treated18,21–27 and untreated6,28–31 lateral cephalometric samples during the past 2 decades. We also have collaborated with many researchers around the world in perfecting this approach. After having staged thousands of lateral headfilms, it became obvious to us that a more detailed description how to portray each of the six stages of CVM was required.
It should be stressed that, although quantification of skeletal changes of the involved cervical vertebrae is possible—and in fact was described in one of our earlier publications3—CVM staging is still a somewhat imprecise science due to the gradual changes in size and shape that occur over time. A person does not go to bed in the evening at CS 2 and wake up the next morning at CS 3. Obviously, changes in size and shape occur gradually with time. Thus, sometimes an intermediate stage is described (eg, CS 2–3) when characteristics of both stages are present in a single image, an issue that will be discussed later.
There are six stages of cervical maturation in all, as shown diagrammatically in Table 1. In his original presentation of the method in 1972, Lamparski19 described these stages using C2 through C6 in the diagnostic process. In 1995, Hassel and Farman were the first to propose the use of the CVM method based on three vertebrae.32 They stated that these vertebrae were selected because C3 and C4 could be visualized even when a thyroid protective collar was worn during radiation exposure. We also have found it necessary only to analyze the bodies of the second, third, and fourth cervical vertebrae, making the method less complex (Table 1).
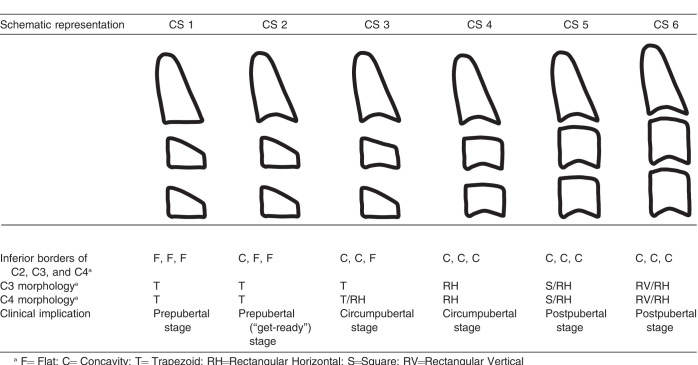
Table 1.
The Six Stages of Cervical Vertebral Maturation
Six maturational stages of the cervical vertebrae can be determined, based on the morphology of C2, 3, and 4. The first step is to evaluate the inferior border of these three vertebral bodies. At CS 1, the inferior surface of all three vertebral bodies is flat. At CS 2, the inferior border of C2 is notched or indented, with the notching of the inferior border becoming more obvious with maturity. At CS 3, similar notches can be observed in C2 and C3. At CS 4, 5, and 6, notching can be seen at the inferior borders of C2, 3, and 4 (Table 1).
The second step in the analysis is to evaluate the shape of C3 and C4. These vertebral bodies change in form in a typical sequence progressing from trapezoidal to rectangular horizontal to square to rectangular vertical. In stages CS 1 to CS 3, most of the cases present a trapezoidal shape of C3 and C4, but in CS 3, one of the vertebral bodies in a limited number of subjects may have a rectangular horizontal shape. C3 and C4 are rectangular horizontal, square in CS 5, and rectangular vertical in CS 6. Typically, CS 1 and CS 2 are considered prepubertal, CS 3 and CS 4 circumpubertal, and CS 5 and CS 6 postpubertal.
We fully realize that comprehending the description of the CVM method in the two paragraphs above can be overwhelming to the uninitiated reader. Describing each stage individually and combining the detailed description with ways of remembering each stage makes the CVM method much easier to use. After gaining some experience, the average user should be able to use the method without having to resort to a photograph or graphic to remember the six stages of CVM. These descriptions are provided below.
Cervical Stage 1
In CS 1, the inferior borders of vertebral bodies C2 to C4 are flat (or sometimes slightly convex; Figure 1). The third and fourth cervical bodies are trapezoidal in morphology, assuming the shape of a wedge of cheese (Figure 2), with the posterior border of the vertebral body taller than the anterior border and the superior surface sloping downward and forward. This stage occurs from approximately the time of eruption of the deciduous dentition until about 2 years before the peak in craniofacial skeletal growth. It should be noted that in some young subjects, C3 and C4 are rectangular and short vertically, reminiscent of the shape of an ice hockey puck in profile (Figure 1A).
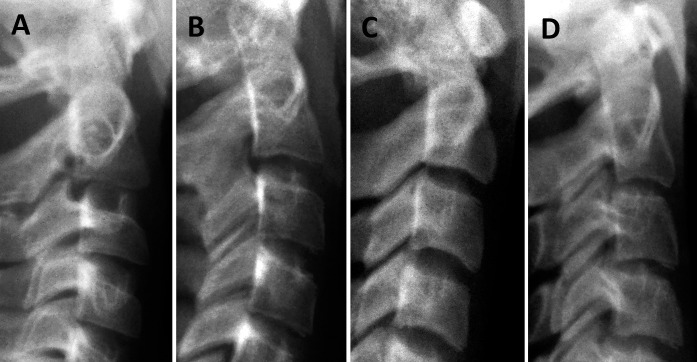
Figure 1.

Four examples of the first CVM stage (CS 1). Note that the inferior borders of the three cervical bodies are not indented but are flat or slightly convex. The uncinate process (uncus) is visible in most images. These processes are situated on either side of the superior face of the vertebral bodies C3 and below. They are bony processes projecting upward that are received by shallow concavities on the lower surface of the adjacent vertebra. The uncinate processes are not considered when in CVM staging.
Figure 2.
In earlier stages, C3 and C4 can have a trapezoidal shape and appear like a wedge of cheese, as shown here. Anterior is to the right. The posterior vertical height is longer than the anterior vertical height.
CS 1 has strong clinical implications. For example, our research4 has shown that the ideal time to intervene with facial mask therapy combined with rapid maxillary expansion (RME) is at CS 1. Maximum skeletal adaptations occur in the midfacial region during this stage as the sutures are more open in the younger patient. Less skeletal and greater dentoalveolar adaptations occur when RME combined with facial mask therapy is used during later stages (eg, CS 3 and CS 4).4
Cervical Stage 2
CS 2 is characterized by a visible notch along the inferior border of the second cervical vertebra (odontoid process). The lower borders of the third and fourth vertebral bodies remain flat (Figure 3). Both C3 and C4 retain a trapezoidal shape (wedge of cheese). CS 2 can be considered the “get-ready” stage because the peak interval of mandibular growth should begin within a year after this stage is evident.
Figure 3.

Four examples of the second CVM stage (CS 2). A notch is present along the inferior border of the odontoid process (C2). The vertebral bodies of C3 and C4 are in the shape of a wedge or trapezoid.
Cervical Stage 3
CS 3 is characterized by visible notching of the inferior borders of C2 and C3; the inferior border of C4 remains flat (Figure 4). Most of the C3 and C4 bodies still retain a trapezoidal shape. In some instances, however, either C3 or C4 has a more rectangular horizontal shape. It must be remembered that the difference between stages is gradual, not abrupt, so that saying that someone is a late CS 3 or an early CS 4 is appropriate, depending on the transitional morphology of the third and fourth vertebrae. At this stage, maximum craniofacial growth velocity is anticipated.
Figure 4.
The third CVM stage (CS 3). Distinct notches are present on the inferior border of C2 and C3. One or both of the third and fourth cervical bodies still have a trapezoidal shape, an easy way to distinguish between CS 3 and CS 4.
Cervical Stage 4
In CS 4, all three bodies have obvious concavities along their inferior surfaces, so the more important factor now is the shape of C3 and C4 (Figure 5). At CS 4, both vertebral bodies have a rectangular horizontal rather than a trapezoidal shape. It is easiest to remember this stage as the “bar of soap” stage because the bodies of both C3 and C4 assume this well-known shape (Figure 6). Alternatively, the familiar rectangular image of a credit card (Figure 7) is another way to visualize this stage. During CS 4, continued accelerated craniofacial growth can be anticipated.
Figure 5.
The fourth CVM stage (CS 4). Distinct notches are present in all vertebrae C2–4. The bodies of C3 and C4 are rectangular horizontal in shape.
Figure 6.

The vertebral bodies of C3 and C4 at CS 4 are shaped like an ordinary bar of soap.
Figure 7.

The vertebral bodies of C3 and C4 at CS 4 are shaped like a credit card, a generic version of which is shown here.
Cervical Stage 5
CS 5 can be differentiated from CS 4 on the basis of the shapes of C3 and C4, with these bodies becoming square (Figure 8). At least one of the bodies of C3 and C4 is square. If not square, the body of the other cervical vertebra is rectangular horizontal. All three cervical bodies have notches, so the presence of notching no longer is important in the differential diagnosis. We have found it easy to remember this stage as the “marshmallow” stage (Figure 9), in that the shape of the vertebral bodies now resemble the soft, white, puffy confection seen so commonly at summer campfires in the United States and elsewhere. When this stage is reached, most substantial craniofacial growth has been achieved.
Figure 8.
The fifth CVM stage (CS 5). The bodies of C3 and C4 are now square, with the posterior height the same as the width.
Figure 9.

C3 and C4 at CS 5 are shaped like a stack of marshmallows.
Cervical Stage 6
It has been our experience that the most difficult stage to determine is CS 6, requiring measurement of the length of the posterior and inferior borders of C3 and C4. At CS 6, at least one of the third and fourth cervical bodies has assumed a rectangular vertical morphology (Figure 10), with the length of the posterior border being longer than the inferior border. If not rectangular vertical, the body of the other cervical vertebra is squared. In addition, the cortical bone appears better delineated in CS 6 than at CS 5. It has been reported that 17% of females never reach CS 6.33 At this stage, a patient can be evaluated for corrective jaw surgery or the placement of endosseous implants in the esthetic region.
Figure 10.
The sixth CVM stage (CS 6). The bodies of C3 and C4 now are rectangular vertical in shape (ie, greater posterior length than inferior length).
It should be noted that even though CVM staging is useful here, it should be reemphasized that the gold standard for determining the continuation or cessation of significant craniofacial growth in all orthodontic patients is the evaluation of two lateral headfilms taken 6–12 months apart. Ideally, if tracings of the two headfilms can be superimposed on one another, then the patient is ready for orthognathic surgery or implant placement in the esthetic zone. An analysis of the Technetium 99m level can also be used to determine whether the mandibular condyles are in an active growth phase.34
DISCUSSION
The CVM method is not a perfect rating system. The method is ordinal in nature in that six distinct stages of cervical maturation are described. The nature of the growth process, however, is not ordinal but continuous. It is obvious that the gradual changes in size and shape occur over time, not overnight. Thus, there is some blending of features in what can be called in-between stages, examples of which are presented in Figure 11.
Figure 11.
(A–D) Four examples of in-between stages in which morphological characteristics of two adjacent CVM stages are observed. (A) CS 2-3. (B) CS 3–4. (C) CS 4–5. (D) CS 5–6.
Figure 11A demonstrates an image of C2, 3, and 4 in which there is a transition from CS 2 to CS 3. Mild notching can be observed at the inferior border of C2 and the beginning of notching at C3. This stage can be described as CS 2–3 or, alternatively, late CS 2.
Figure 11B shows characteristics of both CS 3 and CS 4. The bodies are taller than typical for a CS 3 but C4 still has characteristics of the trapezoid. Minimal notching is observed along the inferior border of C4. This image could be described as late CS 3 or CS 3–4. Similarly, Figure 11C shows C3 with a square shape, but C4 has a rectangular horizontal shape. The staging for this image could be CS 4–5, late C4, or early C5. A similar situation is shown in Figure 11D, with C3 having a rectangular vertical shape and C4 having a square shape, thus another in-between example.
In our long experience with the CVM method, other issues have become obvious; not all cervical vertebrae can be staged in a reproducible manner. We estimate that about 3%–5% of the cervical vertebrae images examined fall into this category for many reasons, some technical and some biological. Inadequate head positioning within the cephalostat can lead to rotational and elevational issues in the headfilm, so that the vertebrae cannot be visualized properly. The image also can be underexposed or overexposed.
One other issue that must be discussed is the occurrence of spikes along the inferior border of the three cervical vertebrae under consideration (Figure 12). These islands of bone can confuse the staging process because they can appear to be extensions of the inferior border, leading to the erroneous appearance of an early concavity or notching. These osseous islands, however, are not connected to the vertebral bodies but rather are isolated areas of bone.
Figure 12.
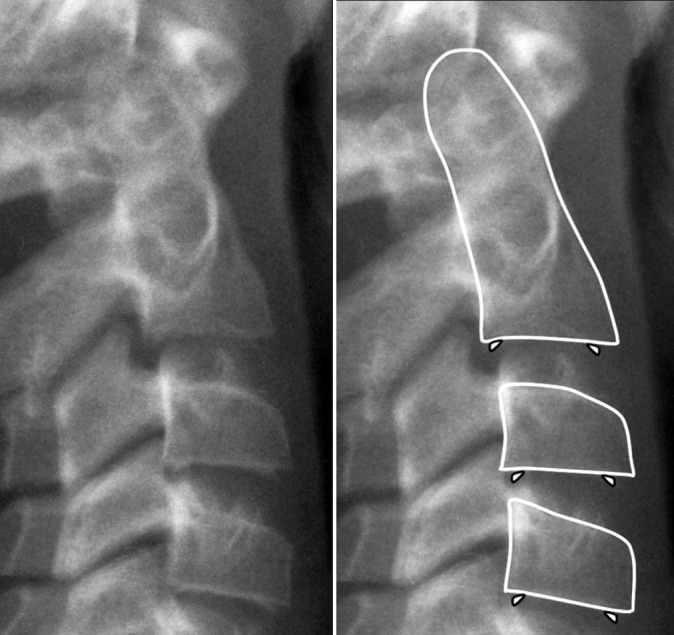
Spikes, or islands of bone, can be observed along the inferior border of the cervical bodies in the anterior and posterior regions. These small osseous structures are not part of the vertebral body but are free-floating. Spikes should be ignored when staging the cervical vertebrae. Left, radiograph alone. Right, same radiograph with C2, 3, and 4 outlined and the location of the spikes indicated.
Several systematic reviews of the CVM method and its reliability have been published previously,35–37 with some investigators questioning the reproducibility of the CVM method. Researchers at the University of Iowa35,38 have reported that the CVM method presents with poor reproducibility among nonexpert examiners. It should be noted, however, that the schematic representation of the CVM method as published in the 2005 article of Baccetti et al.3 that was given to the orthodontists in both Iowa studies was not proposed by those authors as a guideline to implement the CVM method in a clinical setting.
In contrast, Perinetti et al.39 demonstrated that when specific training is provided for the visual assessment of the stages, the CVM method proves to be repeatable to a satisfactory level. Similar positive results were reached by researchers in a recent study at the University of Liverpool. At that institution, Rainey et al.40 investigated the reliability of the CVM method by first contacting one of the developers of the current method (J. Mc.), gaining access to his teaching materials and becoming exposed to his unique method of remembering the morphological characteristics of each of the 6 CVM stages. The Liverpool group found that the intra- and interobserver agreements were substantial, concluding that the current method of CVM classification is reproducible and reliable.
Furthermore, cervical vertebrae do not always “follow the rules” during growth. Such vertebrae occasionally do not develop notching at all or develop notching very late developmentally. In these instances, it is helpful to assess the overall clinical picture, taking into consideration additional developmental factors such as chronological age, stature, and stage of dental development as adjuncts to aid evaluation of the individual's developmental stage. When staging of the CVM is difficult, an alternative for assessment of the individual skeletal maturity is represented by the MP3 method that has shown an overall satisfactorily diagnostic agreement with the CVM method.41
Final Remarks
Estimating the craniofacial maturational level by staging the second through fourth cervical vertebral bodies as seen in the lateral headfilm can give the clinician one additional piece of information that can be used as an adjunct to reach an appropriate diagnosis and make treatment decisions in some clinical cases. CVM staging should be used in concert with a thorough evaluation of the hard and soft tissue during the treatment planning process as well as other maturational indicators and the family history. As with any subjective clinical evaluation, the reliability of the CVM method improves with experience.
Thus, we have written this paper as a “user's guide” to the cervical vertebral maturation method, as originally developed by Lamparski in 1972,19 and as refined during the past 20 years by our group in association with many colleagues, orthodontic residents, and students who have collaborated on numerous research studies using this method of developmental staging. We hope this paper will be used both by those experienced in the CVM method and by the novice who desires to learn the basics of this diagnostic approach.
ACKNOWLEDGMENTS
First, we cite the extraordinary contributions of our close friend Tiziano Baccetti (1966–2011) who was a major driving force behind our efforts to understand and modify the CVM method for use in everyday practice. His many contributions to this effort and to our overall research program were critical; he is sorely missed by all of us.
We thank Don L. Lamparski, who originated the CVM method as part of his master's thesis at the University of Pittsburgh in 1972. We were fortunate to find a copy of his original work in 1998 and were able to understand the value in and nuances of his approach.
We recognize the following individuals for their collaborative efforts in helping us define, refine, and teach the CVM method, applying this approach to a variety of research projects. We thank Fernanda Angelieri, Carlos Flores-Mir, Bernardo Souki, Jared Little, Spencer Crouch, and Sara Hosni for their detailed evaluation of this manuscript prior to submission. We also recognize Marilia Yatabe, Lucia Cevidanes, Giuseppe Perinetti, Antonio Ruelles, Franka Stahl, Billy Jean McKeever, Nicole Pentis, and Robert Schutt for their important contributions to our CVM research effort.
REFERENCES
- 1.McNamara JA, Jr, Bookstein FL, Shaughnessy TG. Skeletal and dental changes following functional regulator therapy on Class II patients. Am J Orthod. 1985;88:91–110. doi: 10.1016/0002-9416(85)90233-7. [DOI] [PubMed] [Google Scholar]
- 2.Franchi L, Baccetti T. New emphasis on the role of mandibular skeletal maturity in dentofacial orthopedics. In: McNamara JA Jr, editor. The Enigma of the Vertical Dimension. Ann Arbor, Mich: Monograph 36, Craniofacial Growth Series, Center for Human Growth and Development, University of Michigan;; 2000. [Google Scholar]
- 3.Baccetti T, Franchi L, McNamara JA., Jr The Cervical Vertebral Maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 4.Franchi L, Baccetti T, McNamara JA., Jr Post-pubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2004;126:555–568. doi: 10.1016/j.ajodo.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 5.Perinetti G, Primožič J, Franchi L, Contardo L. Treatment effects of removable functional appliances in pre-pubertal and pubertal Class II patients: a systematic review and meta-analysis of controlled studies. PLoS One. 2015;10:e0141198. doi: 10.1371/journal.pone.0141198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angelieri F, Franchi L, Cevidanes LHS, McNamara JA., Jr Diagnostic performance of skeletal maturity for the assessment of midpalatal suture maturation. Am J Orthod Dentofacial Orthop. 2015;148:1010–1016. doi: 10.1016/j.ajodo.2015.06.016. [DOI] [PubMed] [Google Scholar]
- 7.Suri S, Prasad C, Tompson B, Lou W. Longitudinal comparison of skeletal age determined by the Greulich and Pyle method and chronologic age in normally growing children, and clinical interpretations for orthodontics. Am J Orthod Dentofacial Orthop. 2013;143:50–60. doi: 10.1016/j.ajodo.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 8.Hellman M. The process of dentition and its effects on occlusion. Dent Cosmos. 1923;65:1329–1344. [Google Scholar]
- 9.Björk A, Helm S. Prediction of the age of maximum pubertal growth in body height. Angle Orthod. 1967;37:134–143. doi: 10.1043/0003-3219(1967)037<0134:POTAOM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Franchi L, Baccetti T, De Toffol L, Polimeni A, Cozza P. Phases of the dentition for the assessment of skeletal maturity: a diagnostic performance study. Am J Orthod Dentofacial Orthop. 2008;133:395–400. doi: 10.1016/j.ajodo.2006.02.040. [DOI] [PubMed] [Google Scholar]
- 11.Mellion ZJ, Behrents RG, Johnston LE., Jr The pattern of facial skeletal growth and its relationship to various common indexes of maturation. Am J Orthod Dentofacial Orthop. 2013;143:845–854. doi: 10.1016/j.ajodo.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 12.Beit P, Peltomäki T, Schätzle M, Signorelli L, Patcas R. Evaluating the agreement of skeletal age assessment based on hand–wrist and cervical vertebrae radiography. Am J Orthod Dentofacial Orthop. 2013;144:838–847. doi: 10.1016/j.ajodo.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Karlberg J. Secular trends in pubertal development. Horm Res. 2002;57(suppl 2):19–36. doi: 10.1159/000058096. [DOI] [PubMed] [Google Scholar]
- 14.Delemarre–van de Waal HA. Secular trend of timing of puberty. Endocr Dev. 2005;8:1–14. doi: 10.1159/000084082. [DOI] [PubMed] [Google Scholar]
- 15.Flores–Mir C, Nebbe B, Major PW. Use of skeletal maturation based on hand-wrist radiographic analysis as a predictor of facial growth: a systematic review. Angle Orthod. 2004;74:118–124. doi: 10.1043/0003-3219(2004)074<0118:UOSMBO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Fishman LS. Radiographic evaluation of skeletal maturation. A clinically oriented method based on hand-wrist films. Angle Orthod. 1982;52:88–112. doi: 10.1043/0003-3219(1982)052<0088:REOSM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Perinetti G, Contardo L, Castaldo A, McNamara JA, Jr, Franchi L. Diagnostic reliability of the cervical vertebral maturation method and standing height in the identification of the mandibular growth spurt. Angle Orthod. 2015;86:599–605. doi: 10.2319/072415-499.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baccetti T, Franchi L, Cameron CA, McNamara JA., Jr Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71:343–350. doi: 10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Lamparski DG. Skeletal Age Assessment Utilizing Cervical Vertebrae [master's thesis] Pittsburgh, Pa: University of Pittsburgh;; 1972. [Google Scholar]
- 20.Lamparski DG, Nanda SK. Skeletal age assessment utilizing cervical vertebrae. In: McNamara JA Jr, Kelly KA, editors. Treatment Timing: Orthodontics in Four Dimensions. Ann Arbor, Mich: Monograph 39, Craniofacial Growth Series, Department of Orthodontics and Pediatric Dentistry and Center for Human Growth and Development, University of Michigan;; 2002. [Google Scholar]
- 21.Franchi L, Baccetti T, McNamara JA., Jr Treatment and post-treatment effects of acrylic splint Herbst appliance therapy. Am J Orthod Dentofac Orthop. 1999;115:429–438. doi: 10.1016/s0889-5406(99)70264-7. [DOI] [PubMed] [Google Scholar]
- 22.Baccetti T, Franchi L, Toth LR, McNamara JA., Jr Treatment timing for twin block therapy. Am J Orthod Dentofac Orthop. 2000;118:159–170. doi: 10.1067/mod.2000.105571. [DOI] [PubMed] [Google Scholar]
- 23.Faltin K, Jr, Faltin RM, Baccetti T, Franchi L, Ghiozzi B, McNamara JA., Jr Long-term effectiveness and treatment timing for Bionator therapy. Angle Orthod. 2003;73:221–230. doi: 10.1043/0003-3219(2003)073<0221:LEATTF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Geran RG, McNamara JA, Jr, Baccetti T, Franchi L, Shapiro LM. A prospective long-term study on the effects of rapid maxillary expansion in the early mixed dentition. Am J Orthod Dentofacial Orthop. 2006;129:631–640. doi: 10.1016/j.ajodo.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 25.Freeman DC, McNamara JA, Jr, Baccetti T, Franchi L. Long-term treatment effects of the FR-2 appliance of Fränkel. Am J Orthod Dentofacial Orthop. 2008;133:513–524. doi: 10.1016/j.ajodo.2007.11.029. [DOI] [PubMed] [Google Scholar]
- 26.Baccetti T, Franchi L, Schulz SO, McNamara JA., Jr Treatment timing for an orthopedic approach to patients with increased vertical dimension. Am J Orthod Dentofacial Orthop. 2008;133:58–64. doi: 10.1016/j.ajodo.2006.01.048. [DOI] [PubMed] [Google Scholar]
- 27.Huanca Ghislanzoni LT, Baccetti T, Cacciatore G, Toll D, McNamara JA, Jr, Franchi L. Treatment timing of MARA and fixed appliance therapy of Class II malocclusion. Eur J Orthod. 2013;35:394–400. doi: 10.1093/ejo/cjs023. [DOI] [PubMed] [Google Scholar]
- 28.Gu Y, McNamara JA., Jr Mandibular growth changes and cervical vertebral maturation: a cephalometric implant study. Angle Orthod. 2007;77:947–953. doi: 10.2319/071006-284.1. [DOI] [PubMed] [Google Scholar]
- 29.Baccetti T, Reyes BC, McNamara JA., Jr Craniofacial changes in Class III malocclusion as related to skeletal and dental maturation. Am J Orthod Dentofacial Orthop. 2007;132:171.e1–171.e12. doi: 10.1016/j.ajodo.2005.07.031. [DOI] [PubMed] [Google Scholar]
- 30.Stahl F, Baccetti T, Franchi L, McNamara JA., Jr Longitudinal growth changes in untreated subjects with Class II division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:125–137. doi: 10.1016/j.ajodo.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 31.Alexander AZ, McNamara JA, Jr, Franchi L, Baccetti T. A mixed longitudinal cephalometric study of craniofacial growth in untreated Class III malocclusion. Am J Orthod Dentofacial Orthop. 2009;135:700.e701–e714. doi: 10.1016/j.ajodo.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 32.Hassel B, Farman AG. Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofacial Orthop. 1995;107:58–66. doi: 10.1016/s0889-5406(95)70157-5. [DOI] [PubMed] [Google Scholar]
- 33.Pasciuti E, Franchi L, Baccetti T, Milani M, Farronato G. Comparison of three methods to assess individual skeletal maturity. J Orofac Orthop. 2013;74:397–408. doi: 10.1007/s00056-013-0164-x. [DOI] [PubMed] [Google Scholar]
- 34.Fahey F, Abramson Z, Padwa B, Zimmerman R, Zurakowski D, Nissenbaum M, et al. Use of 99mTc-MDP SPECT for assessment of mandibular growth: development of normal values. Eur J Nucl Med Mol Imaging. (2010);2010;3737:1002–1010. 1002–1010. doi: 10.1007/s00259-009-1337-0. [DOI] [PubMed] [Google Scholar]
- 35.Gabriel DB, Southard KA, Qian F, Marshall SD, Franciscus RG, Southard TE. Cervical vertebrae maturation method: poor reproducibility. Am J Orthod Dentofacial Orthop. 2009;136:x478.e471–e477. doi: 10.1016/j.ajodo.2007.08.028. [DOI] [PubMed] [Google Scholar]
- 36.Santiago R, Miranda Costa L, Vitral R, Fraga M, Bolognese A, Maia L. Cervical vertebral maturation as a biologic indicator of skeletal maturity: a systematic review. Angle Orthod. 2012;82:1123–1131. doi: 10.2319/103111-673.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao X, Lin J, Jiang J, Wang Q, Hong N. Validity and reliability of a method for assessment of cervical vertebral maturation. Angle Orthod. 2012;82:229–234. doi: 10.2319/051511-333.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nestman T, Marshall S, Qian F, Holton N, Franciscus R, Southard T. Cervical vertebrae maturation method morphologic criteria: poor reproducibility. Am J Orthod Dentofacial Orthop. 2011;140:182–188. doi: 10.1016/j.ajodo.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 39.Perinetti G, Caprioglio A, Contardo L. Visual assessment of the cervical vertebral maturation stages: a study of diagnostic accuracy and repeatability. Angle Orthod. 2014;84:951–956. doi: 10.2319/120913-906.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rainey BJ, Burnside G, Harrison JE. Reliability of cervical vertebra maturation staging. Am J Orthod Dentofacial Orthop. 2016;150:98–104. doi: 10.1016/j.ajodo.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 41.Perinetti G, Perillo L, Franchi L, Di Lenarda R, Contardo L. Maturation of the middle phalanx of the third finger and cervical vertebrae: a comparative and diagnostic agreement study. Orthod Craniofac Res. 2014;17:270–279. doi: 10.1111/ocr.12052. [DOI] [PubMed] [Google Scholar]