ABSTRACT
Diplopia or double vision has various aetiologies and often presents to the ophthalmologist. The purpose of our study was to study in detail the aetiology, progression, and outcome in patients of diplopia presenting to the ophthalmology department of a tertiary care centre. In a prospective observational study, all patients presenting to the emergency services and the outpatient department of a tertiary care centre over a period of 1 year were recruited. One hundred and sixty patients who presented with diplopia with a mean age of 40 (range 7–76) years were included. There were 112 (70%) males and 48 (30%) females. The most common cause for binocular diplopia was vasculopathy in 43 (28.66%) followed by trauma in 37 (24.66%). In those less than 20 years decompensating heterophorias were most common and had the best prognosis. Traumatic causes were common in the age group 20–40 years and vascular in the >40 years age group. For all other aetiologies, elderly patients had more resolution than young patients (p = .04). Larger deviation at presentation, younger age group, and a history of trauma were associated with late recovery (p = .03. p = .04 and p = .04, respectively).
KEYWORDS: Diplopia, ophthalmology, nerve palsy, double vision
Introduction
Diplopia or double vision is the presenting feature of a wide variety of neurological and ocular conditions.1–3 When identical objects are imaged on disparate retinal areas, they are seen in different visual directions, i.e. they are perceived as double images. Patients with double vision often present first to an ophthalmologist, who can help guide the management of the patient. A careful history and clinical examination can give us a clue to the aetiology; thus, a treatment plan can be formulated.4
Despite its clinical importance, not many studies have focused on the incidence, different causes, and natural history of diplopia. Published literature views such cases mainly from a neurologist’s perspective or on a specific group of aetiologies, a specific age group, or only specific nerve palsies. With the advent of newer imaging algorithms, we may need to re-define certain protocols in the work-up of patients with diplopia. The purpose of our study was to study in detail the distribution, clinical features, aetiology, progression, and outcome in patients with diplopia presenting to the ophthalmology department of a tertiary care centre.
Methods
This was a prospective observational study. We included all the patients with diplopia who presented to the Eye Centre at the Postgraduate Institute of Medical Education and Research, Chandigarh over a period of 1 year. After obtaining informed consent, data were collected from patient files regarding the age at presentation, mode of onset, type of diplopia, inciting cause, history of any treatment, examination findings, and the course of the disease. All patients underwent a complete ophthalmological examination.
A detailed history was taken from each patient including age at diagnosis, laterality, any trauma, ocular surgery, diabetes mellitus, hypertension, hypercholesteraemia, cardiovascular diseases, and history of smoking. Patients who presented with a short history of sudden and recent onset (few days to weeks) were identified as acute/subacute and those who presented after 1 month of onset as chronic. The examination included a recording of visual acuity by Snellen charts, slit lamp examination for anterior segment evaluation as well as posterior segment examination by slit-lamp biomicroscopy. Squint examination included evaluation of the ocular movements, measurement of ocular deviation by the prism bar cover test and Krimsky test when there was no central fixation. Diplopia charting was done with red-green glasses at 1 m. Patients with long-standing phorias or latent strabismus sometimes present with diplopia due to decompensation of their phorias due to fever, trauma, and advancing age. Thorough ophthalmological evaluation and management by a strabismologist was performed in such cases and systemic investigations avoided. These conditions were labelled as decompensating heterotopias. Systemic examination was performed and appropriate investigations were ordered in all other cases. A record was made of the investigations ordered. These were principally, full blood count, blood sugar testing, blood pressure monitoring, lipid profile, chest radiograph, C-reactive protein, antinuclear antibody, anti-neutrophil cytoplasmic antibody, and any imaging of the brain with computed tomography (CT) or magnetic resonance imaging (MRI).
A neurologically isolated palsy was defined as a limitation of ocular movement in the absence of other signs and symptoms. Cases with neurological involvement were examined by a neurologist and investigated accordingly. A CT scan was the investigation of choice in patients with a history of trauma. MRI brain was done as the first line in almost all non-trauma cases and coupled with contrast where a lesion was suspected (inflammatory/tumour) and angiography in cases of isolated third nerve palsy or where a vascular lesion was suspected. If the patient had previous imaging from another centre and the result was felt to be ambiguous MRI was repeated in our centre.
The aetiology was classified as vascular for hypertensive and diabetic patients. A presumed microvascular cause was assigned in those patients for whom the MRI scan and clinical testing did not reveal any abnormality.
At each visit, a note was kept of the outcome in terms of whether the diplopia had resolved or not and whether the ocular movements had recovered or not. Length of follow-up and status at last follow-up was noted. Examination was conducted on the day of the presentation, at 6 weeks, and at 3 months.
Statistical analysis
Descriptive analysis of all the data was done using SPSS for Windows (version 17.0; SPSS Inc., Chicago, IL, USA). Analysis of the epidemiological profile of patients was also performed. Chi-square and ANOVA testing were used to find the statistical correlation between the various variables in our study and resolution of diplopia.
Results
One hundred and sixty patients who presented with diplopia were enrolled in our study between June 2013 to May 2014. There were 112 (70%) males and 48 (30%) females. The mean age at presentation was 40.34 (standard deviation [SD] 16.98, range 7–76) years. The largest group of patients (37%) were in the 20–40 years old age group.
The duration of diplopia at presentation ranged from 1 day to 10 years. Eighty patients (53.33%) presented within 30 days of onset of diplopia and 70 (46.66%) patients presented after 30 days of onset of diplopia. Thirty-nine patients had a duration of diplopia of more than 6 months at presentation. The mean duration of diplopia in these patients was 2.87 SD 1.2 (range 0.5–10) years.
There were 150 patients who presented with binocular diplopia (93.75%) and 10 patients (6.25%) with monocular diplopia.
Aetiology
Table 1 depicts the various causes of diplopia according to the clinical features and systemic associations. The most common cause for binocular diplopia was vasculopathy in 43 (28.66%) of cases, followed by trauma in 37 (24.66%), decompensating heterophorias in 18 (11.25%), intracranial tumours (meningiomas, brainstem gliomas, and pontine tumours) in seven (4.4%), and underlying inflammatory causes in 7 (4.3%). We could not find an inciting cause in 16 (10%) patients at presentation to us.
Table 1.
Aetiology of diplopia
| Monocular diplopia (n = 10) | n(%) |
|---|---|
| Cataract | 2 (20%) |
| Central serous chorioretinopathy | 1 (10%) |
| Migraine | 1 (10%) |
| Adenoviral conjunctivitis | 1 (10%) |
| Incorrect refraction | 1 (10%) |
| Unknown |
4 (40%) |
|
Binocular diplopia (n = 150) |
|
| Vasculopathic (DM, HTN, migraine) | 43 (29%) |
| Trauma | 37 (25%) |
| Decompensating heterophorias | 18 (12%) |
| Inflammatory | 7 (5%) |
| Tumours | 7 (5%) |
| Thyroid eye disease | 6 (4%) |
| Previous ophthalmological surgery | 5 (3%) |
| Ear, nose and throat procedure | 1 (0.6%) |
| Others^ | 10 (6%) |
| Unknown | 16 (10%) |
^Other causes include idiopathic intracranial hypertension, double elevator palsy, myasthenia gravis, gaze palsies and infectious causes.
DM = diabetes mellitus; HTN = hypertension.
Age-wise stratification of the factors leading to diplopia showed that decompensating heterophorias were most common in less than 20 years, traumatic causes in the 20–40 years age group and vascular causes in the greater than 40 years age group.
We also analysed the age-wise distribution of the clinical diagnosis made (Table 2). The single largest cause for diplopia was cranial nerve palsies, which accounted for 113 (70.7%) of all cases. Sixty (53.09%) patients had sixth nerve palsy, 28 (24.77%) had fourth nerve palsy, 19 (16.81%) patients had third nerve palsy, and 6 (5.30%) patients had multiple cranial nerve palsies. In patients presenting with cranial nerve palsies, the most common cause was vasculopathy (diabetes mellitus, hypertension, and migraine) in 43 (36.28%) patients followed by trauma in 35 (29.20%) patients and tumour in seven (6.19%) patients. In patients with vasculopathic causes, nine had diabetes mellitus, five had hypertension, 27 had both diabetes mellitus and hypertension, and two had migraine.
Table 2.
Age-wise stratification of clinical diagnosis in our patients
| Diagnosis | ≤20 years | 20–40 years | 40–60 years | ≥60 years | Total |
|---|---|---|---|---|---|
| Sixth nerve palsy | 9 | 18 | 23 | 10 | 60 |
| Fourth nerve palsy | 2 | 11 | 12 | 3 | 28 |
| Third nerve palsy | 1 | 10 | 6 | 2 | 19 |
| Decompensating phorias | 9 | 3 | 4 | 2 | 18 |
| Monocular diplopia | 2 | 2 | 3 | 3 | 10 |
| Thyroid eye disease | 0 | 3 | 3 | 0 | 6 |
| Multiple cranial nerve palsies | 0 | 3 | 3 | 0 | 6 |
| Post-operative diplopia | 2 | 1 | 2 | 0 | 5 |
| Supranuclear gaze palsy | 0 | 1 | 1 | 0 | 2 |
| Others (DEP, MG, IIH) | 2 | 2 | 2 | 0 | 6 |
| Total | 160 |
DEP = double elevator palsy; MG = myasthenia gravis; IIH = idiopathic intracranial hypertension.
Analysing the nerve palsies and their aetiologies separately, the most common cause of sixth nerve palsy was vascular due to diabetes mellitus, hypertension, or migraine in 42% of patients followed by trauma in 27% of patients. Inflammatory causes included Tolosa-Hunt syndrome and orbital apex syndrome. The most common cause of fourth nerve palsy was vasculopathy in 36% of cases and in third nerve palsy trauma accounted for 47.37% of cases.
Thirty-seven patients (24.6%) had binocular diplopia due to causes other than cranial nerve palsies. Decompensating heterophorias accounted for diplopia in 18 patients (11 patients had esophorias and seven patients had exophorias). Six patients had thyroid-associated ophthalmopathy, five patients had diplopia following ophthalmological surgery, two patients each had supranuclear causes and myasthenia gravis and one each had double elevator palsy and an inflammatory cause. The rest of the patients had trauma as the cause of the diplopia.
Ocular examination
Some form of refractive error was present in 130 patients while 30 patients were emmetropic. One hundred and fifty patients were phakic, nine were pseudophakic, and one was aphakic. Pupillary reactions were abnormal in seven patients. A relative afferent pupillary defect was present in two patients, one of whom had orbital apex syndrome and one had involvement of the inferior division of the third cranial nerve. A mid-dilated pupil was observed in five patients, all of whom had third nerve palsy. Anisocoria was present in four patients, three of whom had third nerve palsy and one had cranial nerve palsy. The rest of patients had normal pupillary reactions.
Imaging
Imaging was available in 80 out of the 160 patients. Forty-nine patients had some form of imaging done from outside when they presented and 31 had imaging at our centre. Imaging was abnormal in 24 patients (30%). Table 3 shows an indication for imaging in our patients with specific findings.
Table 3.
Indications and pathologies on imaging
| No. of patients where imaging was ordered | Indication for imaging | No. of patients with abnormal imaging | Pathology detected | |
|---|---|---|---|---|
| Sixth nerve palsy | 16 | Trauma, neurological symptoms, non resolution | 13 | Orbital fractures – 8 Pontine tumour – 2 Suprasellar mass – 3 |
| Fourth nerve palsy | 4 | Trauma, ordered by neurologist | 3 | Meningioma – 1 Cerebral infarcts – 2 |
| Third nerve palsy | 5 | Trauma, ordered by neurologist | 4 | Muscle entrapment – 4 |
| Multiple cranial nerve palsies | 6 | Multiple cranial nerve involvement | 4 | Orbital apex syndrome – 1 Tolosa-Hunt syndrome – 2 Giant cell arteritis – 1 |
Follow-up
Of the 160 patients included in the study, nine patients were lost to follow up at 6 weeks and a total of 10 patients were lost to follow up at 3 months. Hence, 150 patients completed the study.
Outcomes
In our study cohort, out of 160 patients, 153 patients were managed medically (95.6%) and seven (4.3%) patients had surgical intervention. Medical management included counselling, fogged glasses, multi-vitamin tablets, and oral and intravenous corticosteroids. Corticosteroids were administered in patients with giant cell arteritis and orbital apex syndrome. Four patients were managed with prism correction and one patient was advised to use an aphakic contact lens for correction of diplopia. Corrective surgery in the form of anterior transposition of the inferior oblique muscle was performed in four patients (all diagnosed with superior oblique palsy), Knapp’s procedure was done in one patient and two patients underwent orbital floor repair. In patients who underwent corrective surgery, diplopia resolved in three but remained after surgery in four.
Resolution of diplopia
We analysed the outcomes after 3 months of follow-up (Table 4). Decompensating heterophorias resolved in 82.3% of cases and sixth nerve palsies resolved in 41.5% of cases. Multiple cranial nerve palsies, fourth nerve palsies and supranuclear palsies did not tend to improve significantly. Out of all diagnoses, third nerve palsy showed the least recovery (p = .04).
Table 4.
Resolution of symptoms according to the clinical diagnosis at 3 months
| Total | Resolved | Still improving | No change from presentation | Mean improvement in grade of limitation | P value | |
|---|---|---|---|---|---|---|
| Monocular | 9 | 7 | 1 | 1 | - | 0.07 |
| Sixth nerve palsy | 53 | 22 | 10 | 21 | Abduction 1.85 ± 0.30 | 0.04 |
| Third nerve palsy | 18 | 5 | 4 | 9 | Adduction 0.50 ± 0.20 | 0.23 |
| Fourth nerve palsy | 28 | 11 | 8 | 9 | Abduction 0.83 ± 0.38 | 0.66 |
| Infraduction 0.85 ± 0.31 | ||||||
| Multiple cranial nerve palsies | 6 | 3 | 1 | 2 | - | 0.72 |
| Thyroid eye disease | 6 | 2 | 2 | 2 | Abduction 0.27 ± 0.21 | 0.63 |
| Adduction 0.44 ± 0.30 | ||||||
| Decompensating phorias | 17 | 14 | 2 | 1 | - | 0.0001 |
| Myasthenia gravis | 2 | 0 | 1 | 1 | Abduction 0.25 ± 0.10 | |
| Post-surgery | 5 | 0 | 1 | 4 | Abduction 0.65 ± 0.45 | 0.019 |
| Adduction 0.73 ± 0.56 | ||||||
| Supranuclear causes | 2 | 0 | 1 | 1 | - | |
| Double elevator palsy | 1 | 0 | 0 | 1 | - |
Multivariate statistical analysis showed a positive correlation between the resolution of symptoms and the age of the patients. When we excluded decompensating phorias, elderly patients had more resolution than young patients (p = .04). As the age of the patients increased, chances of recovery of diplopia increased. Larger deviation at presentation as well as the history of trauma was associated with late recovery (p = .03 and 0.04, respectively). The time for recovery of diplopia was not affected by the age of the patient (p = .06), gender of the patient (p = .73), or grade of limitation of movements (p = .73).
Discussion
Diplopia is a disabling condition which causes discomfort and anxiety in patients. Our study has described the aetiology, presenting features and resolution in 160 cases of diplopia presenting over a 1-year period.
There have been studies in the past on the epidemiology, causes, outcomes of diplopia only in selected patient populations and without studying all of the outcomes.2–6 To the best of our knowledge, this study reports the largest series of patients presenting with diplopia prospectively. It helps us in determining the myriad of aetiologies encountered in the Indian sub-continent as well as establishes the natural course of diplopia-related events.
It is extremely important to establish the aetiology of diplopia in any patient presenting to an ophthalmologist. The causes can vary from an undiagnosed refractive error to life-threatening aneurysms. While we should never miss underlying intracranial disease in a patient of diplopia, on the other hand, every case of binocular diplopia does not indicate a sinister pathology. It is necessary to establish the acuteness of diplopia along with an orthoptic examination, which will differentiate cranial nerve palsies from decompensating heterophorias in most cases.
Our study has shown that lenticular abnormalities, refractive errors, macular pathologies like central serous chorioretinopathy and surface abnormalities like conjunctivitis should not be overlooked as a contributing cause for monocular diplopia. Early and careful detailed examination in these patients can obviate the need for unnecessary investigations.
Prior studies have reported the incidence of binocular diplopia to be 74.9%-88.5%, which is less than reported in our study (94%).1,3,4,7 This might be because being a tertiary referral centre, binocular diplopia is more commonly seen. The most common causes of binocular diplopia in our series were vasculopathy and trauma. Our definitions of aetiology were broad, in order to understand the distribution of diplopia. A significant proportion of patients (12.0%) also had diplopia due to decompensating phorias. These three aetiologies constitute the majority of diplopia cases. Vascular risk factors like diabetes, hypertension and hyperlipidaemia have been well documented as the most common aetiology of diplopia in previous studies.3,8 Since decompensated strabismus is a very important cause of diplopia, any diplopia presenting to a neurologist should be clinically examined by an ophthalmologist as well and as soon as possible, before ordering imaging.
Cranial nerve palsies accounted for most of the cases in our study, which is in accordance with previous studies.3,5,7 As far as the distribution of cranial nerve palsies is concerned in our study, sixth nerve involvement (53.09%) was the most common followed by the fourth nerve (25%), third nerve (17%), and multiple nerve palsies (5%). In any age group, sixth nerve palsy was the most common cause of diplopia in our study, a finding well reported in the literature.9–11 Isolated reports also show fourth nerve palsy12 or third nerve palsy13 as the most common causes.
The combination of diabetes mellitus and hypertension in our study was associated with most of the cases of sixth nerve palsy. Patel et al. concluded that hypertension alone should not be considered the sole cause of neurologically isolated sixth nerve palsy.14 However, in our clinical practice, many cases are attributed to hypertension alone. Moreover, 70% of the patients who had neuro-imaging in our study had no reported abnormality. The debate is whether we should order expensive tests in all cases to reassure the patient and safeguard us medico-legally or not when the likelihood is that they will be normal. In one of the largest study of its kind, it was shown that 16.5% patients had an identifiable cause other than microvascular to cause nerve palsies; hence, the authors advocated early imaging in all cases of cranial nerve palsy causing diplopia.15 Perhaps in a setting where the specialist expertise is available, we should rely on our clinical suspicion and deal with every case with a customised approach. Hypertension is known to worsen the effect of diabetes mellitus in microvascular nerve palsies and may not be an isolated factor per se. These patients can generally be followed up without any intervention. If on sequential examinations, these patients develop other neurological symptoms or signs, or the palsy seems to progress, neurological examination with imaging is indicated.
Third nerve palsy was mostly commonly traumatic in origin in our cohort and recovered the least in contrast to fourth and sixth nerve palsies, which were mostly vasculopathic in origin. The proportion who recover following sixth nerve palsy has been reported to be 12–60% with lower rates of recovery in cases due to trauma.16 Previous reports have also shown poor spontaneous recovery rates in patients with all kinds of traumatic cranial nerve palsies.8,17 There is no clear-cut explanation as to why traumatic palsies show poor recovery, although the severity of trauma has been reported to affect the degree of recovery.18 However, we did not grade the severity of trauma in our patients. Perhaps grading the severity of trauma in further studies and correlating it with the recovery of palsy would show us which traumatic palsy will recover earlier.
With the advent of newer and faster diagnostic tests, recent aetiologies like ocular myasthenia gravis are more specific and concrete as compared to the older literature where only cranial nerve palsies were discussed as causes of diplopia.19
Conclusion
The major conclusion from our study is that patients with clinically isolated single cranial nerve palsies associated with diabetes mellitus or hypertension are likely to recover spontaneously and initially require observation only. Neuroimaging should not always be done on the first visit in these patients. Diplopia in a majority of younger patients is due to decompensating phorias which have maximum chances of spontaneous early recovery. Gender and duration of symptoms do not influence the outcome of the resolution of diplopia. In cases besides decompensating phorias, young patients show less resolution than elderly patients, perhaps due to sinister pathologies. We propose a protocol for advising neuro-imaging in a patient with diplopia, based on the results of our study (Figure 1). Neuro-imaging is indicated in patients with multiple cranial nerve palsies, patients in whom nerve palsies fail to recover and those who show progression of diplopia.
Figure 1.
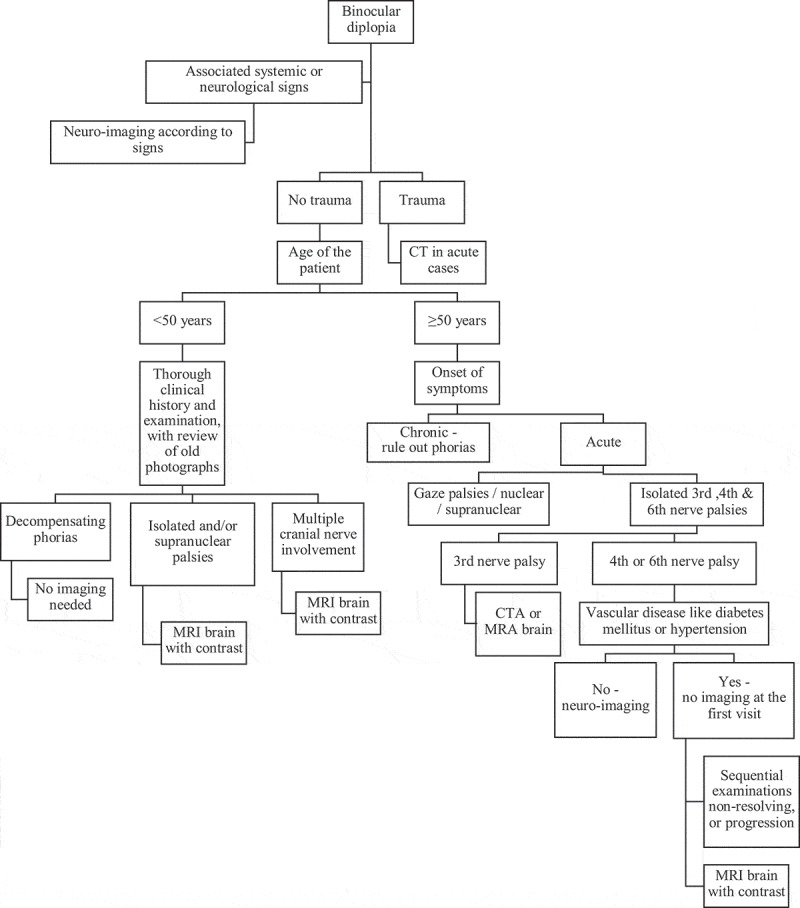
Flow chart describing the approach to a patient with diplopia. It enlists the sequence to be followed before imaging is ordered and in what cases imaging should be ordered acutely
CT = computed tomography; CTA = computed tomography angiography; MRA = magnetic resonance angiography; MRI = magnetic resonance imaging.
The shortcoming of our study is its short duration of follow up along with a selection bias being a hospital-based study. Our study provides insight into the patients who require neuro-imaging and gives a broader picture into the management of patients with diplopia.
Declaration of interest statement
There is no conflict of interest. The authors have no financial interest in any part of this article.
References
- 1.Comer RM, Dawson E, Plant G, Acheson JF, Lee JP.. Causes and outcomes for patients presenting with diplopia to an eye casualty department. Eye. 2007;21:413–418. doi: 10.1038/sj.eye.6702415. [DOI] [PubMed] [Google Scholar]
- 2.Danchaivijitr C, Kennard C. Diplopia and eye movement disorders. J Neurol Neurosurg Psychiatry. 2004;75(Suppl 4):iv24–iv31. doi: 10.1136/jnnp.2004.053413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nolan J. Diplopia. Br J Ophthalmol. 1968;52:166–171. doi: 10.1136/bjo.52.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Colmain U, Gilmour C, Macewen CJ. Acute-onset diplopia. Acta Ophthalmol. 2014;92:382–386. doi: 10.1111/aos.12062. [DOI] [PubMed] [Google Scholar]
- 5.Trimble R. Diplopia as a presenting sign of neoplasia. Trans Ophthalmol Soc UK. 1980;100:498–500. [PubMed] [Google Scholar]
- 6.Yapp JMS. Diplopia as a presenting symptom. Br Orthod J. 1973;30:52–65. [Google Scholar]
- 7.Morris RJ. Double vision as a presenting symptom in an ophthalmic casualty department. Eye. 1991;5:124–125. doi: 10.1038/eye.1991.23. [DOI] [PubMed] [Google Scholar]
- 8.Richards BW, Jones FR and Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992;113:489–496. [DOI] [PubMed] [Google Scholar]
- 9.Rush JA, Younge BR. Paralysis of cranial nerves III, IV and VI. Causes and prognosis in 1000 cases. Arch Ophthalmol. 1981;99:76–79. doi: 10.1001/archopht.1981.03930010078006. [DOI] [PubMed] [Google Scholar]
- 10.Rucker CW. Paralysis of the third, fourth, and sixth cranial nerves. Am J Ophthalmol. 1958;46:787–794. doi: 10.1016/0002-9394(58)90989-9. [DOI] [PubMed] [Google Scholar]
- 11.Tiffin PAC, Mecewen CJ, Craig EA, Clayton G. Acquired palsy of the oculomotor, trochlear and abducens nerves. Eye. 1996;10:377–384. doi: 10.1038/eye.1996.77. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Ophthalmology . Basic and Clinical Science Course: Pediatric Ophthalmology and Strabismus. San Francisco: The Academy; 2007–2008:158. [Google Scholar]
- 13.Berlit P. Isolated and combined pareses of cranial nerves 3rd, 4th and 6th. A retrospective study of 412 patients. Neurol Sci. 1991;103:10–15. doi: 10.1016/0022-510X(91)90276-D. [DOI] [PubMed] [Google Scholar]
- 14.Patel SV, Holmes JM, Hodge DO, Burke JP. Diabetes and hypertension in isolated sixth nerve palsy: a population-based study. Ophthalmology. 2005;112:760–763. doi: 10.1016/j.ophtha.2004.11.057. [DOI] [PubMed] [Google Scholar]
- 15.Tamhankar MA, Biousse V, Ying GS, et al. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology. 2013;120:2264–2269. doi: 10.1016/j.ophtha.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mutyala S, Holmes JM, Hodge DO, Younge BR. Spontaneous recovery rate in traumatic sixth-nerve palsy. Am J Ophthalmol. 1996;122:898–899. doi: 10.1016/S0002-9394(14)70394-0. [DOI] [PubMed] [Google Scholar]
- 17.Holmes JM, Droste PJ, Beck RW. The natural history of acute traumatic sixth nerve palsy or paresis. JAAPOS. 1998;2:265–268. [DOI] [PubMed] [Google Scholar]
- 18.Dhaliwal A, West AL, Trobe JD, Musch DC. Third, fourth, and sixth cranial nerve palsies following closed head injury. J Neuroophthalmol. 2006;26:4–10. doi: 10.1097/01.wno.0000204661.48806.1d. [DOI] [PubMed] [Google Scholar]
- 19.Kumar S. Acute onset binocular diplopia: a retrospective observational study of 100 consecutive cases managed at a tertiary eye centre in Saudi Arabia. Eye (Lond). 2020;34:1608–1613. doi: 10.1038/s41433-019-0705-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


