Abstract
Background
A positive relationship between flat feet and low back pain (LBP) has not gained consensus in literature. The aim of this study was to determine the prevalence and factors associated with low back pain (acute and chronic) among individuals with flat feet.
Methods
In 2018, a cross-sectional study was conducted at a national festival in Saudi Arabia, and 1798 adult visitors were invited to participate in face-to-face interviews. Participants’ characteristics were stratified by the type of foot and they were questioned on acute low back pain (ALBP) or chronic low back pain (CLBP). The odds ratio (OR) were presented as a measure of this association, followed by a multivariate analysis.
Results
The prevalence of LBP among participants with flat feet was 65.9%, among whom 51.6% suffered ALBP and 48.4% suffered from CLBP. Flat feet increased the chances of having ALBP by 3.28 times and CLBP by 4.5 times. After stratification, ALBP and CLBP were both significantly higher among all participants with flat feet in comparison with their counter groups. Multivariate analyses showed that females were more likely to complain of ALBP. Participants who did no physical activity were more likely to complain of ALBP. Female participants and older participants were more likely to complain of ALBP and CLBP.
Conclusion
Flat feet are associated with both ALBP and CLBP. Significant factors of low back pain also included sex, age, occupation, and physical activity.
Keywords: flat feet, back pain, odds ratio, acute, chronic
Background
Low back pain (LBP) is a worldwide health concern. As per the Global Burden of Disease study, LBP is one of the top ten diseases and injuries that people face daily.1 The predicted lifetime prevalence of LBP ranges from 60–70% in developed countries, and on an annual basis, 15–45% of adults develop LBP.2 This prevalence is in particular higher among those between 35 and 55 years old, and it will increase substantially with age due to traumas, stress or intervertebral disc conditions.2 LBP significantly disturbs people’s health and quality of life; to a degree, it might even incapacitate their daily performance and activities.3 Absenteeism from work and even early job retirement have been associated with LBP.4 It was reported that the combined direct and indirect estimated annual medical costs associated with LBP in the United States is in the range of $19.6–118.8 billion.5
LBP is manifested by pain, muscle tension, or stiffness between the lower costal margin and above the inferior gluteal folds that might or might not radiate to the lower extremities. LBP can be diagnosed as either specific LBP, caused by a specific pathophysiological mechanism (herniated disc, infection, osteoporosis etc.), or nonspecific LBP caused by an unknown reason.6 Acute low back pain (ALBP) is a self-limited condition and usually resolves without medical treatment in less than four weeks.7 On the other hand, chronic low back pain (CLBP) is a persistent form of LBP that is of moderate intensity, lasts for more than 3 months, and results in substantial limitations in activity.7
Flat feet or pes planus is an abnormality characterized by excessive pronation of the foot that leads to an internal rotation of the tibia and femur, as well as an anterior pelvic tilt.8 This disorder disturbs the kinematics of lower extremities, the ground reaction forces, the muscle movement and overall gait.8 Flat feet can be classified into either flexible or rigid arch that may or may not reform in non-weight bearing postures.9 The features of flat feet are an extremely low arch that increases the risk of hallux valgus, hammer toes, patellofemoral pain, and other musculoskeletal complications including low back pain.10 The five-year prevalence of flat feet among visitors to an Italian orthopedic ambulatory unit was 3.96%, among whom women were predominant.11 Flat feet has been associated with body mass index, foot size, type of population, family history, and usage of footwear during infancy.12
A review of published studies that investigated the relationship between flat feet and LBP between 2006 and 2017 revealed a lack of consensus and further gaps in knowledge. For instance, one study conducted among children (8–15 years) confirmed that a flatter foot posture was associated with pain/discomfort at the knee, hip and back.13 Among women, one study stated that pronated foot function (flat feet) contributed to lower back symptoms,14 while another female-based study claimed that LBP showed no significant relationship with foot arch indices.15 Even among pregnant women, the foot arch heights did not show any relationship with LBP.16 Two studies conducted in both genders reported that decreased ankle dorsiflexion was a factor in CLBP17 and that moderate to severe pes planus doubled the rate of intermittent LBP.18 However, a single-blind pilot study stated that flat feet did not appear to be a risk factor in subjects with LBP.19 A systematic review on this aspect found that there is indeed a limited research regarding foot deviations and their connection to LBP, but that foot deviations may be potentially associated with LBP.20
Though a number of confirmed confounders might distort the relationship between flat feet and LBP, no studies have stratified their subgroups by the type of foot nor did they investigate this relationship regarding both ALBP and CLBP. Since studies with larger sample sizes and matched-paired groups have been recommended on this matter,10 this study evaluated the factors associated with ALBP and CLBP among individuals complaining of flat feet. The strength of this association was quantified and visually illustrated in a figure to display the impact of flat feet on the acute and chronic types of LBP across various subgroups.
Materials and Methods
During the month of February 2018, a cross-sectional study was conducted at Al-Janadriyah national festival for culture and heritage (32nd version) situated in Riyadh, central Saudi Arabia. This annual event is a major attraction to the Saudi public population who visit it for tourism and shopping, held over the course of three weeks. The estimated number of Al-Janadriyah visitors exceeds 1.2 million. As per the general authority for statistics, the Saudi Arabian population census in 2016 was over 30 million, with equal gender distribution and a median age of 30.2 years.
A team of well-trained 5th year medical students volunteered to do this public survey. The data collection team was oriented on the study objectives, trained on recruiting study participants and obtaining the data. Two licensed clinical research coordinators supervised the medical students at the targeted site. A minimum sample size of 1000 was projected based on the previously reported point prevalence of flat feet (18%)14 and the prevalence of LBP (53–79%),21 a confidence level of 95%, and a margin of error 3%. However, a much larger sample beyond 1200 was needed so that stratification and control of confounders could be conducted without weakening the statistical power of the sample.
A number of data collection booths were distributed at various points of the targeted setting, mainly on pedestrian routes. These booths were organized and equipped for interviews and body measurements (height and weight). By convenience, visitors who randomly passed-by the data collection booths were invited to enroll in this study. Eligible participants were adults (>18 years) who were free of any abnormal spinal curvature or deviation due to previous traumas, aging process, hereditary or congenital reasons. Those who complained of flat feet due to tendon injuries or tears were also excluded. Pregnant women were not included, as were those with lower extremity fractures in the past two years.
Data were obtained via face-to-face interviews. The obtained data were electronically entered into portable assistant devices, and uploaded to a local institutional server at the end of each day. The data collection tool comprised the participants’ characteristics and the outcomes’ characteristics. The participants’ gender, age (young adults ≤25 vs older adults >25 years), level of education (school vs university), financial status (participants were asked whether they are financially comfortable or stressed), marital status (single vs married), occupation (unemployed/student vs employed), physical activity (participants were asked about their physical activities per week), and smoking status were collected. Body mass index was collected based on calculating the measured height (m) and weight (kg) using the same brand of equipment (Secca). Participants were requested to stand straight, shoes/heavy coats taken off and head tilted forward. The scale was quality checked daily for battery life and calibrated by zeroing prior to start. A ±1 kilogram for weight and ±2 centimeter variability was foreseen during body measurements due to participants’ clothing and shoes.
The study outcomes were low back pain and flat feet. Low back pain was explained to the participants as a complaint of pain, numbness, tingling, stiffness, aching, burning in the past 12 months. If the pain was self-limited and resolved within one month then it was counted as an ALBP. If the pain was daily for at least 3 months then it was counted as a CLBP.7 Participants were asked whether they have flat feet or not, an illustrative figure for flat feet was presented to the participants to confirm the presence of flat feet.
Data were analyzed using SPSS version 25 (NY, US). Categorical variables were presented in frequency and percentage. Univariate analyses tested the associations between flat feet and the individual types of LBP after stratifying by gender, age, occupation, BMI category, physical activity and smoking status. The odds ratio (OR) was presented as a measure of the strength of this association. Multivariate analysis was conducted through two binary logistic regression models. The adjusted OR and its 95% confidence interval [95% CI] were presented with a P-value statistically significant at <0.05.
Results
Participants’ and Outcomes’ Characteristics
A total of 1798 participants were enrolled in this study who visited the targeted setting from various geographical regions, central (1211; 67.4%), Western (206; 11.4%), Eastern (144; 8.0%), Southern (128; 7.1%) and Northern (109; 6.1%). The majority were Saudi nationals (1699; 94.5%), while the others were expatriates. Study investigators throughout data collection maintained equal gender distribution. The mean±standard deviation of age was 27.3±8.8 years, with 55.1% of participants. Almost half (54.2%) had a university level of education, while one third were married (35.5%). Half of participants (52%) were unemployed/students and 72.8% reported being comfortable financially. Participants with normal weight were 43.0%, while 28.7% and 21.4% were either overweight or obese. Almost 48% of study participants did not engage in physical activity, and 20.9% reported being regular smokers (Table 1).
Table 1.
Sample Characteristics
| n (%) | |
|---|---|
| Gender | |
| Male | 844 (46.9) |
| Female | 954 (53.1) |
| Age category (years) | |
| ≤25 | 990 (55.1) |
| >25 | 808 (44.9) |
| Mean±standard deviation | 27.3±8.8 |
| Education | |
| School | 824 (45.8) |
| University | 947 (54.2) |
| Financial status | |
| Comfortable | 1309 (72.8) |
| Uncomfortable | 489 (27.2) |
| Marital status | |
| Single | 1159 (64.5) |
| Married | 639 (35.5) |
| Occupation | |
| No/student | 938 (52.2) |
| Yes | 860 (47.8) |
| BMI category | |
| Underweight | 113 (6.9) |
| Normal | 707 (43.0) |
| Overweight | 472 (28.7) |
| Obese | 354 (21.4) |
| Physical activity | |
| None | 866 (48.2) |
| Yes | 948 (51.8) |
| Strenuous | 263 (27.7%) |
| Light | 685 (72.3%) |
| Smoker | |
| Yes | 376 (20.9) |
| No | 1422 (79.1) |
Abbreviations: n, frequency; %, percentage.
A total of 381 participants reported ALBP, while 255 participants reported CLBP. Flat feet were observed among 138 participants, while those with regular feet numbered 1660 participants. The prevalence of LBP among participants with flat feet was 91/138 (65.9%), among whom 47 (51.6%) suffered ALBP and 44 (48.4%) suffered from CLBP. The prevalence of LBP among participants with regular feet was 545/1660 (32.8%), among whom 334 (61.2%) suffered ALBP and 211 (38.7%) suffered CLBP.
Factors Associated with Acute and Chronic Low Back Pain
Acute and chronic low back pain were significantly higher among all participants with flat feet in comparison to those with normal feet after stratifying by gender, age category, occupation, BMI, physical activity and smoking status (Table 2). Having acute and chronic low back pain (55.7% and 54.2%, respectively) was higher in females with flat feet compared with males with flat feet (39.4% and 37.5%, respectively). Older participants with flat feet also reported higher rates of ALBP (60.9%) and higher rates of CLBP (64%), in comparison with younger adults with flat feet (39.6% and 29.3%, respectively). Other associated factors are listed in Table 2.
Table 2.
Odds of Acute and Chronic Low Back Pain in Association with Flat Feet Among Subgroups
| Foot type | Acute Low Back Pain | Chronic Low Back Pain | |||||
|---|---|---|---|---|---|---|---|
| n (%) | OR [95% CI] | χ2; P-value | n (%) | OR [95% CI] | χ2; P-value | ||
| Gender | |||||||
| Male | Regular | 142 (20.3%) | 1 | χ2=6.873 | 100 (15.2%) | 1 | χ2=11.126 |
| Flat | 13 (39.4%) | 2.6 [1.2–5.2] | P=0.009* | 12 (37.5%) | 3.3 [1.6–7.0] | P=0.001* | |
| Female | Regular | 192 (25.6%) | 1 | χ2=25.490 | 111 (16.6%) | 1 | χ2=48.679 |
| Flat | 34 (55.7%) | 3.7 [2.2–6.2] | P<0.001* | 32 (54.2%) | 5.9 [3.4–10.3] | P<0.001* | |
| Age category | |||||||
| ≤25 | Regular | 189 (22.6%) | 1 | χ2=7.270 | 94 (12.7%) | 1 | χ2=9.117 |
| Flat | 19 (39.6%) | 2.2 [1.2–4.1] | P=0.007* | 12 (29.3%) | 2.8 [1.4–5.7] | P=0.003* | |
| >25 | Regular | 145 (23.7%) | 1 | χ2=30.610 | 117 (20.0%) | 1 | χ2=46.657 |
| Flat | 28 (60.9%) | 5.0 [2.7–9.4] | P<0.001* | 32 (64.0%) | 7.1 [3.8–13.1] | P<0.001* | |
| Occupation | |||||||
| No | Regular | 177 (22.5%) | 1 | χ2=15.051 | 88 (12.6%) | 1 | χ2=21.194 |
| Flat | 23 (46.9%) | 3.0 [1.7–5.5] | P=0.001* | 16 (38.1%) | 4.3 [2.2–8.2] | P=0.001* | |
| Yes | Regular | 157 (23.6%) | 1 | χ2=19.539 | 123 (19.5%) | 1 | χ2=37.206 |
| Flat | 24 (53.3%) | 3.7 [2.0–6.8] | P<0.001* | 28 (57.1%) | 5.5 [3.0–10.0] | P<0.001* | |
| BMI category | |||||||
| Underweight/Normal | Regular | 150 (22.0%) | 1 | χ2=15.664 | 83 (13.5%) | 1 | χ2=32.858 |
| Flat | 19 (50.0%) | 3.5 [1.8–6.8] | P=0.001* | 18 (48.6%) | 6.1 [3.1–12.0] | P=0.001* | |
| Overweight/Obese | Regular | 156 (23.9%) | 1 | χ2=17.012 | 103 (17.1%) | 1 | χ2=27.045 |
| Flat | 24 (51.1%) | 3.3 [1.8–6.0] | P<0.001* | 22 (48.9) | 4.6 [2.5–8.6] | P<0.001* | |
| Physical activity | |||||||
| None | Regular | 185 (26.6%) | 1 | χ2=8.225 | 107 (17.3%) | 1 | χ2=34.228 |
| Flat | 19 (47.5%) | 2.5 [1.3–4.7] | P=0.004* | 24 (53.3%) | 5.4 [2.9–10.1] | P=0.001* | |
| Yes | Regular | 149 (19.8%) | 1 | χ2=30.334 | 104 (14.7%) | 1 | χ2=26.120 |
| Flat | 28 (51.9%) | 4.4 [2.5–7.8] | P<0.001* | 20 (43.5%) | 4.5 [2.4–8.3] | P<0.001* | |
| Smoker | |||||||
| No | Regular | 266 (23.1%) | 1 | χ2=29.842 | 158 (15.1%) | 1 | χ2=59.937 |
| Flat | 38 (51.4%) | 3.5 [2.2–5.6] | P<0.001* | 37 (50.7%) | 5.7 [3.5–9.4] | P<0.001* | |
| Yes | Regular | 68 (23.0%) | 1 | χ2=4.932 | 53 (18.9%) | 1 | χ2=4.230 |
| Flat | 9 (45.0%) | 2.7 [1.1–6.7] | P=0.026* | 7 (38.9%) | 2.7 [1.1–7.4] | P=0.040* | |
Note: *P-value statistically significant at <0.05.
Abbreviations: n, frequency; %, percentage; χ2, Pearson Chi-square test; df, degree of freedom; OR, odds ratio; [95%], 95% confidence interval; P, P-value.
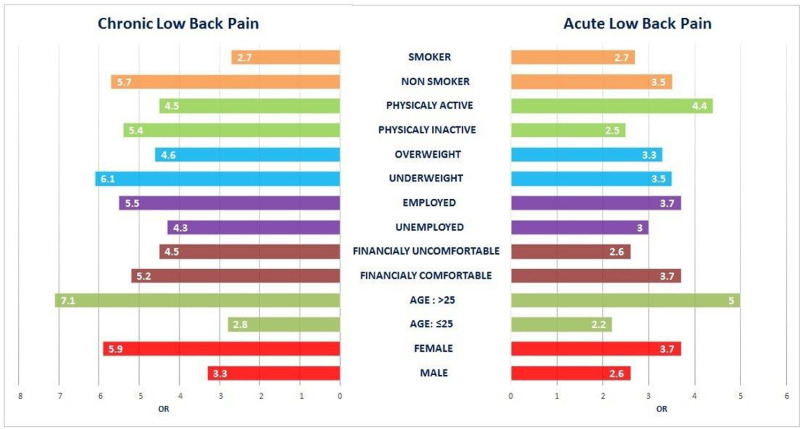
After stratification, the odds of being flat footed and developing ALBP were the highest among older participants (>25) (OR [95%] = 5.0 [2.7–0.9.4]) compared with younger participants with flat feet. This was followed by participants who had flat feet and engaged in physical activity (OR [95%] = 4.4 [2.5–7.8]) compared with participants with normal feet who engaged in physical activity. Similarly, the odds of reporting chronic low pain was the highest among older participants with flat feet (OR [95%] = 7.1 [3.8–13.1]) in comparison with older participants with normal feet. Participants with under/normal weight and flat feet were also (OR [95%] = 6.1 [3.1–12.0]) more likely to endure CLBP compared with their counter group with regular feet. Other odds ratios are illustrated in Figure 1.
Figure 1.
Odds of having low back pain among participants with flat and normal feet.
After conducting multivariate analyses of various exposures including flat foot, females were 1.62 [1.2–2.2] times more likely to complain of ALBP compared with males, adj.P = 0.001. Participants who did no physical activity were 1.43 [1.1–1.8] times more likely to complain of aALBP compared with others, adj.P = 0.005. Female participants and older participants were 1.7 [1.2–2.4] and 1.2 [1.1–1.2] times more likely to complain of acute and chronic low back pain compared with males, adj.P = 0.003 and adj.P<0.001, respectively. Participants who had a job were 1.6 [1.1–2.2] times more likely to complain of CLBP compared with those who were unemployed or students, adj.P = 0.008. Having flat feet increased the chances of having ALBP by 3.28 [2.1–5.2] times and the chances of having CLBP by 4.5 [2.8–7.2] times compared with participants with normal feet, adj.P<0.001 each (Table 3).
Table 3.
Significant Risk Factors Associated with Acute and Chronic Low Back Pain
| Acute Low Back Pain | Chronic Low Back Pain | |||
|---|---|---|---|---|
| Adj.OR [95% CI] | Adj.P-value | Adj.OR [95% CI] | Adj.P-value | |
| Gender (Female vs male) | 1.62 [1.2–2.2] | 0.001* | 1.7 [1.2–2.4] | 0.003* |
| Age (years) | 1.01 [1.0–1.03] | 0.268 | 1.2 [1.1–1.2] | <0.001* |
| Occupation (Yes vs no) | 1.22 [0.9–1.6] | 0.160 | 1.6 [1.1–2.2] | 0.008* |
| BMI (Higher vs Lower) | 1.04 [0.8–1.3] | 0.773 | 1.2 [0.9–1.7] | 0.154 |
| Physical activity (Inactive vs active) | 1.43 [1.1–1.8] | 0.005* | 1.2 [0.9–1.7] | 0.190 |
| Smoking (Yes vs no) | 1.02 [0.7–1.4] | 0.926 | 1.2 [0.8–1.8] | 0.364 |
| Flat feet (Yes vs no) | 3.28 [2.1–5.2] | <0.001* | 4.5 [2.8–7.2] | <0.001* |
Note: *Statistically significant at <0.05.
Abbreviations: BMI, body mass index; Adj, adjusted; OR, odds ratio; Adj, adjusted; CI, confidence interval.
Discussion
This is a public survey on flat feet to determine the nature of its association with ALBP and CLBP. The strength of this study lies in its large sample size and the stratification that described the level of association across various subgroups. Flat feet has been found to be a significant contributor to both types of LBP across all groups. The authors believe that the illustrated figure of odds ratio will present a visual comparison and a clarification of the true impact of flat feet on LBP, so that individuals with flat feet can take precautionary measures.
The prevalence of LBP among participants with flat feet was 65.9%, compared with 32.8% prevalence of LBP among those with regular feet. One study noted that pronated foot function was associated with female gender even after adjusting for age, weight, smoking and depression.14,22 This study acknowledged these previous findings. However, this study showed that the presence of flat feet in both genders was significantly associated with both ALBP and CLBP, and the odds of LBP was higher among females with flat feet compared with males with flat feet. Sex remains a major confounder for both flat feet and low back pain. Females generally differ from males in terms of body alignment, range of motion and spinal joints.14,22 Women with flat feet have been reported to exhibit a greater static anterior pelvic tilt and dorsal inclination of the spine.14,23 Moreover, females tend to have greater internal hip rotation and trunk extension compared with males, all of which are accounted as kinematic changes influenced by flat feet.14
Age is another major contributing factor of LBP, and with the presence of flat feet, LBP is expected to be higher. Participants above 25 years of age who had flat feet were almost seven times more likely to develop CLBP, compared with those of same age category and regular feet. Flat feet usually disappear by the age of six when the feet become less flexible and the arches develop.24 The rates of flat feet are often higher in children due to ligament laxity, but this then declines with age.25 However, some studies have stated that older adults have a more pronated foot posture than younger adults.26 Studies have noted that the highest incidence of LBP occurs in the third decade of life and the overall prevalence increases until age 60–65 years.7 Therefore, the age factor has contributed negatively in the prevalence of LBP in combination with the presence of flat foot. Regardless of any weight category, flat feet were significantly associated with ALBP and CLBP. Flat feet were significantly associated with LBP even after adjusting for weight as reported in literature.14
Occupation increased the chances of developing both ALBP and CLBP among participants with flat feet. Authors believe that this variable is hard to evaluate, as careers vary in the degree of physical stress that participants are exposed to. For instance, some jobs require longer times of standing, lifting heavy objects, while others require operating on chairs behind desks. Even participants who spend more time sitting may or may not follow healthy ergonometric postures. From a statistical point of view, workers with flat feet endured higher rates of LBP with no affirmation that the career itself played a minor or a major contribution. It has been reported that even those who were unsatisfied with their work situation and its physical demand were at a higher risk of developing LBP.27 Moreover, in military careers, applicants with flat feet have been historically rejected due to risk of developing foot and back pain.28 The National Health Interview Survey confirmed that white-collar workers (professional, managerial, or administrative work) with flat feet were significantly more prone to pain.29 Accordingly, these participants need to be vigilant about healthy body mechanics and postures during their working hours.
Obesity has been reported to be strongly related with ankle and foot pain.30 Weight reduction has been proven by one randomized control trial to reduce the dynamic plantar pressure in obese adults.31 Whether weight had a mediating effect or a direct effect, participants with flat feet were at higher risk to develop LBP and excess body weight can only elevate this risk. In a previous study, flat feet was also positively correlated with increased lumbar curvature and back pain.15
Engaging in physical activity is crucial in controlling the body weight and strengthening the lower back muscles. The prevalence of CLBP in this study was higher among participants with flat feet who did not perform physical activity in comparison with those with flat feet who engaged in physical activities. One study concluded that an Increase in physical activity aided in the improvement of foot structure and the function among obese persons.30 Compliance with healthy dietary habits and engagement in regular physical activity makes the feet thinner, the arches higher/stiffer and ankle muscle stronger.30 Accordingly, the authors believe that participants with flat feet are advised to adopt a healthier lifestyle.
Numerous studies have related former or current smoking to LBP.32 Some studies considered that smoking and pain fall under a dose-response relationship, in a sense nicotine alters the perception and threshold for pain.33 Therefore, it was suggested that exposure to smoking could be associated with a higher prevalence of LBP.33 Smokers might increase in the level of circulating pro-inflammatory cytokines, which also amplifies pain.33 Moreover, smoking might have increased inflammation, and thus delayed the healing of LBP.33 In this setting, smokers with flat feet had higher prevalence of LBP compared with smokers with regular feet. This entails that smoking behavior did not enhance the prevalence of LBP.
Limitations
This study encountered some limitations. Due to the busy and crowded nature of the event held at this setting, some participants might have been rushed to provide answers or distracted by their companions, though study investigators made an effort to insure participants were interviewed in a private and calm area. Variations in the shape and weight of clothing worn by visitors might have altered the accuracy of the height and weight measurements, and a certain degree of variability was anticipated. However, upon converting these body measurements to BMI categories and considering the large sample size, authors believe that such errors are less likely to jeopardize the accuracy of this variable. Moreover, a certain degree of recall bias from the participants’ side is expected due to the retrospective nature of the study design. Lack of physical examination is considered one of the major limitations in this study (except for height and weight) as the presence of flat feet was self-reported by participants due to lack of privacy in the study setting. Majority of the study participants (festival visitors who agreed to participate) are fairly young, therefore including different age groups is of significance. Therefore the study findings cannot be generalized for all age groups. Low back pain might have been induced by numerous factors such as trauma, ergonometric factors, sleep hygiene and so on. The authors tried their best to control for these confounders by limiting the eligibility criteria to health participants, yet other confounders might have been present and not controlled.
Conclusions
Flat foot is a deformity that accompanies the individual since early childhood. Persons with flat feet suffer from the implications of this issue, mainly low back pain. This study showed that regardless of age, gender, BMI, occupation, being a non-smoker or physically active, flat feet was a significant factor associated with both types of low back pain. The odds ratio, being the highest among certain subgroups, is an alert to these individuals to be extra vigilant about their selection of shoes and safe lifestyle measures. Although physical activity and weight control measures are known to lower the chance of low back pain, individuals with flat feet still reported low back pain.
Acknowledgment
This study was approved and supported by King Abdullah International Medical Research Center, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
Abbreviations
LBP, Low back pain; ALBP, Acute low back pain; CLBP, Chronic low back pain; OR, Odds ratio.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The Institutional Review Board at the Saudi Ministry of National Guard Health Affairs has approved this study (RC17/127). A self-explanatory letter of invitation to participate was handed to each of the participants. Those who agreed to participate were interviewed. This observational study posed no potential risks and lacked any intervention or any usage of new equipment.
Disclosure
The authors declare no conflicts of interest for this work.
References
- 1.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Priority diseases and reasons for inclusion: low back pain Chapter 6. WHO; 2013. Available from: https://www.who.int/medicines/areas/priority_medicines/Ch6_24LBP.pdf.
- 3.Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457. doi: 10.2147/JPR.S105892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palmer KT, Goodson N. Ageing, musculoskeletal health and work. Best Pract Res Clin Rheumatol. 2015;29(3):391–404. doi: 10.1016/j.berh.2015.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi: 10.1016/j.spinee.2007.10.005 [DOI] [PubMed] [Google Scholar]
- 6.Koes B, Van Tulder M, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332(7555):1430–1434. doi: 10.1136/bmj.332.7555.1430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patrick N, Emanski E, Knaub MA. Acute and chronic low back pain. Med Clin N Am. 2014;98(4):777–789. doi: 10.1016/j.mcna.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 8.Farahpour N, Jafarnezhad A, Damavandi M, Bakhtiari A, Allard P. Gait ground reaction force characteristics of low back pain patients with pronated foot and able-bodied individuals with and without foot pronation. J Biomech. 2016;49(9):1705–1710. doi: 10.1016/j.jbiomech.2016.03.056 [DOI] [PubMed] [Google Scholar]
- 9.Dars S, Uden H, Banwell HA, Kumar S. The effectiveness of non-surgical intervention (Foot Orthoses) for paediatric flexible pes planus: a systematic review: update. PLoS One. 2018;13(2):e0193060. doi: 10.1371/journal.pone.0193060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.López-López D, Vilar-Fernández J, Barros-García G, et al. Foot arch height and quality of life in adults: a strobe observational study. Int J Environ Res Public Health. 2018;15(7):1555. doi: 10.3390/ijerph15071555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Troiano G, Nante N, Citarelli GL. Pes planus and pes cavus in Southern Italy: a 5 years study. Ann Ist Super Sanità. 2017;53(2):142–145. doi: 10.4415/ANN_17_02_10 [DOI] [PubMed] [Google Scholar]
- 12.Pita-Fernandez S, Gonzalez-Martin C, Alonso-Tajes F, et al. Flat foot in a random population and its impact on quality of life and functionality. J Clin Diagn Res. 2017;11(4):LC22. doi: 10.7860/JCDR/2017/24362.9697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kothari A, Dixon P, Stebbins J, Zavatsky A, Theologis T. Are flexible flat feet associated with proximal joint problems in children? Gait Posture. 2016;45:204–210. doi: 10.1016/j.gaitpost.2016.02.008 [DOI] [PubMed] [Google Scholar]
- 14.Menz HB, Dufour AB, Riskowski JL, Hillstrom HJ, Hannan MT. Foot posture, foot function and low back pain: the Framingham Foot Study. Rheumatology. 2013;52(12):2275–2282. doi: 10.1093/rheumatology/ket298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borges CDS, Fernandes LFRM, Bertoncello D. Relationship between lumbar changes and modifications in the plantar arch in women with low back pain. Acta Ortop Bras. 2013;21(3):135–138. doi: 10.1590/S1413-78522013000300001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ojukwu CP, Anyanwu EG, Nwafor GG. Correlation between Foot arch index and the intensity of foot, knee, and lower back pain among pregnant women in a South-Eastern Nigerian Community. Med Princ Pract. 2017;26(5):480–484. doi: 10.1159/000481622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brantingham JW, Gilbert JL, Shaik J, Globe G. Sagittal plane blockage of the foot, ankle and hallux and foot alignment-prevalence and association with low back pain. J Chiropr Med. 2006;5(4):123–127. doi: 10.1016/S0899-3467(07)60144-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kosashvili Y, Fridman T, Backstein D, Safir O, Ziv YB. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008;29(9):910–913. doi: 10.3113/FAI.2008.0910 [DOI] [PubMed] [Google Scholar]
- 19.Brantingham JW, Adams KJ, Cooley JR, Globe D, Globe G. A single-blind pilot study to determine risk and association between navicular drop, calcaneal eversion, and low back pain. J Manipulative Physiol Ther. 2007;30(5):380–385. doi: 10.1016/j.jmpt.2007.04.004 [DOI] [PubMed] [Google Scholar]
- 20.O’Leary CB, Cahill CR, Robinson AW, Barnes MJ, Hong J. A systematic review: the effects of podiatrical deviations on nonspecific chronic low back pain. J Back Musculoskelet Rehabil. 2013;26(2):117–123. doi: 10.3233/BMR-130367 [DOI] [PubMed] [Google Scholar]
- 21.Awaji M. Epidemiology of low back pain in Saudi Arabia. J Adv Med Pharm Sci. 2016;6(4):1–9. [Google Scholar]
- 22.Nguyen A-D, Shultz SJ. Sex differences in clinical measures of lower extremity alignment. J Orthop Sports Phys Ther. 2007;37(7):389–398. doi: 10.2519/jospt.2007.2487 [DOI] [PubMed] [Google Scholar]
- 23.Janssen MM, Drevelle X, Humbert L, Skalli W, Castelein RM. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine. 2009;34(23):E826–E32. doi: 10.1097/BRS.0b013e3181a9fd85 [DOI] [PubMed] [Google Scholar]
- 24.Raj MA, Bhimji SS. Pes Planus. StatPearls [Internet]. StatPearls Publishing; 2018. [PubMed] [Google Scholar]
- 25.Aenumulapalli A, Kulkarni MM, Gandotra AR. Prevalence of flexible flat foot in adults: a cross-sectional study. J Clin Diagn Res. 2017;11(6):AC17. doi: 10.7860/JCDR/2017/26566.10059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Redmond AC, Crane YZ, Menz HB. Normative values for the foot posture index. J Foot Ankle Res. 2008;1(1):6. doi: 10.1186/1757-1146-1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matsudaira K, Konishi H, Miyoshi K, Isomura T, Inuzuka K. Potential risk factors of persistent low back pain developing from mild low back pain in urban Japanese workers. PLoS One. 2014;9(4):e93924. doi: 10.1371/journal.pone.0093924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Menz HB, Dufour AB, Riskowski JL, Hillstrom HJ, Hannan MT. Association of planus foot posture and pronated foot function with foot pain: the Framingham foot study. Arthritis Care Res. 2013;65(12):1991–1999. doi: 10.1002/acr.22079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shibuya N, Jupiter DC, Ciliberti LJ, VanBuren V, La Fontaine J. Characteristics of adult flatfoot in the United States. J Foot Ankle Surg. 2010;49(4):363–368. doi: 10.1053/j.jfas.2010.04.001 [DOI] [PubMed] [Google Scholar]
- 30.Zhao X, Tsujimoto T, Kim B, et al. Effects of increasing physical activity on foot structure and ankle muscle strength in adults with obesity. J Phys Ther Sci. 2016;28(8):2332–2336. doi: 10.1589/jpts.28.2332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Song J, Kane R, Tango DN, et al. Effects of weight loss on foot structure and function in obese adults: a pilot randomized controlled trial. Gait Posture. 2015;41(1):86–92. doi: 10.1016/j.gaitpost.2014.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between smoking and low back pain: a meta-analysis. Am J Med. 2010;123(1):87. e7–e35. doi: 10.1016/j.amjmed.2009.05.028 [DOI] [PubMed] [Google Scholar]
- 33.Green BN, Johnson CD, Snodgrass J, Smith M, Dunn AS. Association between smoking and back pain in a cross-section of adult Americans. Cureus. 2016;8(9). doi: 10.7759/cureus.806 [DOI] [PMC free article] [PubMed] [Google Scholar]