Abstract
Introduction:
On June 24 in the United Kingdom, there were 277,989 cases of COVID-19 and 39,369 deaths recorded. The government enforced a complete lockdown on March 23 that resulted in cessation of all elective admissions on 24th onward, with only acute trauma cases being admitted to hospital. This study aims to characterize the changes in trauma admissions during the first 5-week lockdown period. The hypothesis states that there would be a significant reduction in overall orthopedic trauma admissions, polytrauma, and high-energy outdoor trauma during this COVID-19 period.
Methods:
All trauma admissions over nearly a 5-week period from March 23, 2020, to April 26, 2020, were collated as the “COVID cohort” and compared to the “control” group of patients from the same hospitals 1 year before between March 23, 2019, and April 26, 2019. Spinal admissions and pediatrics were excluded from the study as they were managed in other regional units.
Results:
There was a 56% reduction in trauma admissions during the COVID-19 lockdown (133 vs. 304). A majority of the COVID cohort were admitted with fractures (89 vs. 164, P = 0.017, Chi-square test) from home with low-energy falls. Overall, fewer operations were performed than the year before. However, a greater proportion of admitted patients had a surgical orthopedic intervention rather than admission and nonoperative management.
Conclusions:
There was a reduction in admissions as well as reductions in high energy and occupational injuries. Elderly patients continued to fall at home or in care, sustaining hip fractures. This vulnerable group requires beds, orthogeriatric management followed by surgical intervention and social care. Orthogeriatric services must be maintained to ensure the best clinical outcomes for this group.
Keywords: COVID-19, pandemic, reconfiguration, trauma, trauma and orthopedics
INTRODUCTION
An outbreak of COVID-19 was first reported in China on December 31, 2019.[1,2] As the outbreak spread across the world, it was evident containment was an issue and on the March 11, 2020, the World Health Organization declared the virus had gone from an epidemic to a pandemic.[3] On the March 16, 2020, the government urged that only those in utmost need to attend hospital to avoid overwhelming the National Health Service (NHS).[4] On the March 23, the United Kingdom entered lockdown.[5]
The four Surgical Royal Colleges of the UK and Ireland issued a joint guideline outlining four key priorities for surgical teams during the pandemic: maintain emergency surgical capability, protect and preserve the surgical workforce, and help to fulfill alternative surgical and nonsurgical roles.[6] The British Orthopaedic Association (BOA), Royal Colleges of Surgeons and NHS England issued guidelines on the management of orthopedic trauma during COVID.[7,8] The national guidelines provide an alternative way to manage urgent orthopedic conditions and trauma, both help to minimize patient and staff exposure to COVID-19 while protecting resources of the NHS.[7] Publications from the USA have found reduction in major trauma at level I and II trauma centers ranging from 42.9% to 70%.[9,10,11] One study looking exclusively at orthopedic trauma found an overall reduction in orthopedic trauma of 45.1% at a level II center.[10]
The BOA predicted that there would be a significant reduction in the volume of high-energy injuries with the implementation of the lockdown.[7] It would be prudent that our research highlights and stratifies the types of injury being admitted to hospitals to maintain appropriate surgical capability. The current hypothesis states that there would be a significant reduction in orthopedic trauma during the COVID-19 lockdown.
METHODS
The setup
Our hospital is the highest volume elective orthopedic hospital in the United Kingdom. As a tertiary referral center, it deals with general elective orthopedics, musculoskeletal oncology, elective and trauma spinal surgery, and cold trauma (upper and lower limb). In an effort to reduce bed occupancy and provide support for our neighboring trusts during the pandemic, the services in our hospital were reconfigured to accept orthopedic trauma transfers while completely curtailing our elective activity.[12] This was done with respiratory ventilators/equipment, staff, and bed capacity to allow the two district general hospitals (DGHs) to accept COVID-19 patients. Our hospital commenced accepting trauma transfers from two DGHs on March 23, 2020, this would be equivalent to level II trauma centers in the USA.
Data were collected via a prospectively updated electronic trauma admission database between March 23, 2020, and April 26, 2020, this was to be the COVID-19 cohort. These data were compared with a cohort of patients from the two local DGHs admitted during the same period in 2019, the pre-COVID cohort.
This was a 4-week period during the national enforced lockdown period. Inclusion criteria were for all patients admitted to hospital with trauma-related injury or infection requiring orthopedic input (intravenous antibiotics or surgical debridement), irrespective of treatment received. Exclusion criteria were pediatric patients, who were still being managed at the local DGH, spinal referrals, which were dealt by the spinal unit and are split between three regional units and minor injuries (patients not needing admission to a trauma bed), as these were referred to the fracture clinic.
Demographical data were collated, as was the type of injury, the anatomical region of injury, mechanism of injury, where the injury took place, and type of treatment the patient underwent during their admission.
Statistical analysis
Statistical analysis was performed using the statistical package R (3.4.3, R Core Team, Austria). Data were assessed for normality using frequency histograms where normality was not found, data were presented as median (interquartile range). Numerical data were compared using nonparametric Wilcoxon rank test. Categorical data were compared using the Chi-square test and Fisher's exact test where the expected frequency was <5. P < 0.05 was deemed to be statistically significant.
RESULTS
The COVID cohort there were 133 trauma admissions, compared to 304 across the two DGH, in the control group [Table 1]. There was a 56% reduction in admissions compared to the previous year. There was an increase in the length of stay in the COVID cohort [Figure 1], but this was not statistically significant (P = 0.052, Wilcoxon rank Test).
Table 1.
Baseline characteristics of admitted orthopaedic patients
| COVID | PreCOVID | P | |
|---|---|---|---|
| Admissions | 133 | 304 | |
| Agea (years) | 72.9 (IQR: 43.3) | 68.8 (IQR: 28) | 0.009* |
| Sexb | 82 (62%) | 140 (46%) | 0.004* |
| LoSc (days) | 6 (IQR: 9) | 4 (IQR: 7) | 0.052* |
aMedian value IQR, bFemale sex, cMedian length of stay IQR, *Wilcoxon rank test: α 0.05. IQR Interquartile range
Figure 1.
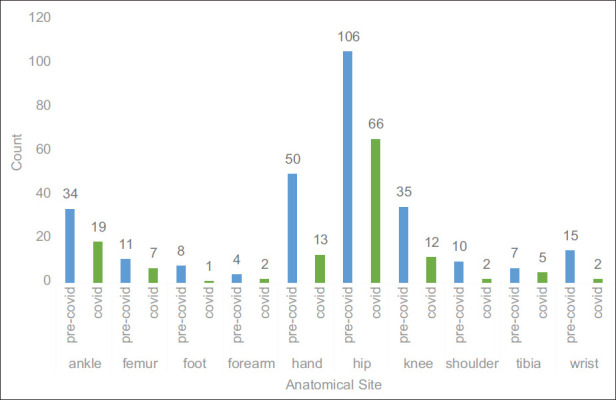
Pre-COVID and COVID admissions by anatomical site
Fractures were the main reason for admission across both groups [Table 2]. However, this was proportionally greater in the COVID cohort making up 67% of total admissions compared to 54% the year prior, which was statistically significant.
Table 2.
Admissions by type
| COVID (n=133), n (%) | Pre-COVID (n=304), n (%) | P | |
|---|---|---|---|
| Fracture | 89 (67) | 164 (54) | 0.019* |
| Soft-tissue injury | 20 (15) | 66 (22) | 0.106* |
| Postoperative complications | 11 (8) | 16 (5) | 0.229* |
| Periprosthetic | 7 (5) | 7 (2) | 0.106* |
| Infection | 5 (4) | 34 (11) | 0.011$ |
| Dislocation | 1 (1) | 17 (6) | 0.017$ |
*Chi-square test, $Fisher’s exact test
Hip fractures continued to provide the bulk of the admissions (49% COVID vs. 35% pre-COVID) and made up a majority of the operative workload (20%) in the COVID group. Hip fractures and management of postoperative complications have remained static, with all other admission types decreasing proportionally.
Types of treatment
There was an increase in the proportion of patients in the COVID cohort who had operative management (106 (80%) vs. 214 (71%)), this was not statistically significant (Chi-square, P = 0.060). Operations for hip fractures were the most common operation performed in both cohorts (COVID 20% vs. pre-COVID 22%). There was only one total hip replacement performed for hip fracture during the COVID period (2 vs. 5), this is in keeping the guidance from NHS England where a preference for hemiarthroplasty should be given over total hip arthroplasty.[13] Comparing COVID against controls, there was a reduction in minor orthopedic procedures such as k-wiring (0 vs. 5), manipulation under anesthesia (1 vs. 16), and open reduction and internal fixation (4 vs. 46) as per the NHS guidance.
Mechanism and place of injury
The national lockdown led to a dramatic increase in indoor and low-energy injuries to (68%) [Table 3]. This is an 18% increase compared to last year. Nineteen percent of patients sustained injuries, while out in the garden during the strict lockdown, compared to only 9% the year prior, there was a reduction in outdoor leisure-related injuries [Table 4].
Table 3.
Mechanism of injury
| COVID (n=133), n (%) | Pre-COVID (n=304), n (%) | P | |
|---|---|---|---|
| Atraumatic | 15 (11) | 62 (20) | 0.021* |
| High-energy blunt | 2 (2) | 19 (6) | 0.048$ |
| High-energy fall | 7 (5) | 20 (7) | 0.599* |
| High-energy penetrating | 1 (1) | 2 (1) | |
| Low-energy blunt | 2 (2) | 9 (3) | |
| Low-energy fall | 90 (68) | 151 (50) | <0.001* |
| Low-energy penetrating | 15 (11) | 38 (13) | 0.719* |
| Other | 1 (1) | 3 (1) |
*Chi-square test, $Fisher’s exact test
Table 4.
Place where injury sustained
| COVID (n=133), n (%) | Pre-COVID (n=304), n (%) | P | |
|---|---|---|---|
| Care home | 11 (8) | 19 (6) | 0.442* |
| Home indoors | 73 (55) | 105 (35) | <0.001* |
| Home outdoors | 25 (19) | 27 (9) | 0.003* |
| Not applicable | 0 | 62 (20) | |
| Outdoor leisure | 17 (13) | 60 (20) | 0.079* |
| Outdoor other | 0 | 18 (6) | |
| Outdoor work | 7 (5) | 13 (4) | 0.649* |
*Chi-square test, $Fisher’s exact test
DISCUSSION
The data set shows a 56% reduction in trauma and orthopedic admissions over the initial 4-week period of lockdown. Two USA studies conducted at a level I trauma centers experienced a 44.9%–70% decline in trauma admissions.[11] One study at a level II trauma center, which is similar to the type of unit we reflect, had a 45.1% decrease in orthopedic trauma encounters. Stoker et al. found a 58.8% decrease in high-severity injuries with a fracture (P = 0.013) and a 42.9% decrease in low-severity injuries (P = 0.0003).[10] This reflects the trend in the reduction of emergency department (ED) attendance over COVID period and the BOA's own prediction. During the month of April 2020, there was 917,000 attendances, NHS England found that this was a 57% reduction compared to the same month last year. This is undoubtedly secondary to the public response to the COVID-19 pandemic, a combination of public avoidance of ED, engaging in less hazardous activity and stricter ED admission criteria.
Injury
Analysis of the data demonstrates that the most common musculoskeletal region injured during lockdown was the hip (49%), followed by the ankle (14%) [Figure 1]. There may be some correlation between increased outdoor-related activity such as government-sanctioned exercise, dog walking, and increased number of ankle fractures. Hand-related admission was the third most common reason for admission in the COVID cohort (10%) and second in the pre-COVID cohort (16%). Pichard et al. found that a greater proportion of patients benefitted from upper limb operations (51% vs. 37%) than their pre-COVID comparison group.[14] It may be that Paris, France, has a different setup to the UK where locally in the UK, it was attempted to manage nonlimb threatening upper limb trauma conservatively or with definitive management in the ED.[7]
Hip fractures accounted for half of all admissions during the lockdown, this has increased compared to the previous year (35%). In total numbers, there was an overall reduction of hip fractures (66 vs. 106), this is an interesting difference, as it would have been expected the numbers to be similar. It may be that COVID has changed the behaviors of the older person meaning less outdoor activity and walks to the shops. Hip fractures are predominantly fragility-related fractures, commonly sustained at home one would not expect the incidence to be affected.[13] Dayananda et al. in Wales also found hip fractures made up the largest cohort of admissions and operations in their cohort of patients.[15] The prevalence of fragility fractures in the elderly commonly sustained at home means that the role of the orthogeriatrician in the management of these patients is key, and therefore, this role should be considered protected from redeployment to other roles during pandemics.[12,13] These trends suggest that fractures commonly associated with occurring at home are likely to be the predominant cause for admission during pandemics.
Operative management
Majority of admissions in the COVID cohort were hip fractures, it follows that the most common operations performed were hemiarthroplasty[14] and dynamic hip screw[10] procedures. It is therefore imperative hospitals that maintain their stock and supply of prosthesis and equipment to enable them to perform these procedures on a regular basis. Our tertiary unit required redeployment of stock from the two DGHs to fulfill this requirement.[12] During the 5 week period, no patients were admitted for antibiotic treatment alone, compared to 7% of patients in the year previously. All five patients admitted during the COVID period with infection required an operative procedure such as washout or debridement.
One institution looking at orthopedic trauma operations during the COVID period found a 23% reduction, this covered the period between March 1 and April 9, only 2 weeks into lockdown.[16] We found a 50% reduction in the total number of operations performed when compared to 2019. There was a reduction in nonoperatively managed patients in the COVID cohort and displays a trend toward only admitting patients requiring definitive operations. By minimizing those that do not require admission, such as those that can be managed with a definitive procedure or treatment plan in the ED, would mean a reduction in admissions and alleviate bed pressures. The COVIDsurg collaborative published a study estimating over 43,000 weekly elective procedures that have been cancelled.[17] The decision to cancel all elective procedures was vital in creating capacity for COVID admissions. If a long-term study shows definitive management in the ED and nonoperative management of certain types of fractures does not significantly cause detriment to the patient, it may lead to a new paradigm in the management of certain orthopedic trauma conditions.
Mechanism and place of injury
There was a significant decrease in volumes of admission and shift in mechanisms of injury during the initial 4 weeks of the lockdown. A reduction was seen in high-energy-related trauma (10 COVID vs.(42) pre-COVID), this included polytrauma and work-related injuries. This was attributed to the reduction of vehicles on the road, as well as closure of many industrial and manual jobs.[18] A large proportion of admissions were due to low-energy falls; these were primarily made up hip fractures occurring at home and care institutions. The second and third biggest groups in the COVID cohort were injuries sustained at home outdoors in the garden (19%) or while those pursuing an outdoor leisure activity (13%) such as dog walking or horse riding [Table 4]. This would be an expected effect of the lockdown and its impact on people lives, injuries sustained at home continue to occur at home despite the pandemic. However, there was an increased number of hand injuries sustained at home outdoors while people made use of the lockdown period to perform home improvements and hobbies [Table 4].
Limitations
This study has the advantage of being a homogeneous group with comparison of trauma admissions from the year prior against the same two local DGHs. The numbers are taken from a regional perspective and may vary from region to region, especially when comparing cities like London. The study covers the first 4 weeks of lockdown, strict lockdown lasted 7 weeks, starting on March 23, and easing on May 13, 2020.[19] During the strict lockdown, we would expect the 4 week sample to give a representative look at the admissions, it is certainly expected that as measures are eased, the level of trauma will steadily increase to pre-COVID levels. Our study is comparable to other studies on the topic, even though they compared multiple hospitals accepting differing types of trauma and therefore do not allow for a true comparison unlike our cohort of patients.[20]
CONCLUSION
COVID-19 has impacted all spheres of life for all people. The elderly continue to fall at home sustaining hip fractures. This vulnerable group requires beds, orthogeriatric management followed by surgical intervention and social care input. Overall, there was a reduction in high-energy-related trauma and injuries sustained outside the home. Greater public health awareness needs to occur around performing home improvements during pandemics as this group tended to be younger, looking to be productive and requiring surgery. The take-home message highlighted by this study states a better reallocation of resources to be to essential services based on admission and surgical rates seen during such pandemics that could be transferred to natural disasters alike.
Research quality and ethics statement
This study was determined to not require the Institutional Review Board / Ethics Committee review, and the corresponding protocol/approval number is not applicable. The authors followed applicable EQUATOR Network (http://www.equator-network.org/) guidelines during the conduct of this research project.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. WHO | Novel Coronavirus – China. World Health Organization. 2020. [Last accessed on 2020 May 26]. Available from: http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO Director-General's Opening Remarks at the Media Briefing on COVID-19. 2020. [Last accessed on 2020 May 26]. Available from: https://www. who.int/dg/speeches/detail/who-director-general-s-opening-remarksat-the-media-briefing-on-covid-19--- 11-march-2020 .
- 4.Vol. 2020. GOV.UK: 2020. Mar 16, [Last accessed on 2020 May 26]. PM Statement on Coronavirus. Available from: https://www.gov.uk/government/speeches/pm-statementon-coronavirus-16-march-2020 . [Google Scholar]
- 5.Vol. 2020. GOV.UK: 2020. Mar 23, [Last accessed on 2020 May 26]. PM Address to the Nation on Coronavirus. Available from: https://www.gov.uk/government/speeches/pmaddress-to-the-nation-on-coronavirus-23-march-2020 . [Google Scholar]
- 6.Royal College of Surgeons England. Guidance for Surgeons Working During the Covid-19 Pandemic. The Surgical Royal Colleges of the United Kingdom and Ireland. 2020. [Last accessed on 2020 May 26]. Available from: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/
- 7.British Orthopaedic Association. BOAST-Management of Patients with Urgent Orthopaedic Conditions and Trauma during the Coronavirus Pandemic. 2020. [Last accessed on 2020 May 26]. Available from: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html .
- 8.NHS England. NHS England: 2020. [Last accessed on 2020 Jun 26]. Clinical guide for the Management of Trauma and Orthopaedic Patients during the Coronavirus Pandemic, Version 2. Available from: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0274-Specialty-guide-Orthopaedic-trauma-v2-14-April.pdf . [Google Scholar]
- 9.Sherman WF, Khadra HS, Kale NN, Wu VJ, Gladden PB, Lee OC. How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? [Last accessed on 2020 Dec 11];Clin Orthop Relat Res. 2021 479:266–75. doi: 10.1097/CORR.0000000000001484. Available from: https://journals.lww.com/clinorthop/Abstract/9000/How_Did_the_Number_and_Type_of_Injuries_in. 97484.aspx . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stoker S, McDaniel D, Crean T, Maddox J, Jawanda G, Krentz N, et al. Effect of shelter-in-place orders and the COVID-19 Pandemic on orthopaedic trauma at a community level II trauma center. J Orthop Trauma. 2020;34:e336. doi: 10.1097/BOT.0000000000001860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DiFazio LT, Curran T, Bilaniuk JW, Adams JM, Durling-Grover R, Kong K, et al. The impact of the COVID-19 pandemic on hospital admissions for trauma and acute care surgery. Am Surg. 2020;86:901–3. doi: 10.1177/0003134820939904. [DOI] [PubMed] [Google Scholar]
- 12.Govilkar S, Dover C, Dass D, Rhind JH, Ramhamadany E, Ford D, et al. From Elective Orthopaedic Centre to a COVID-19 Trauma Unit: Rapid Transformation. 2020. [Last accessed on 2020 May 26]. Available from: https://www.boa.ac.uk/ policy-engagement/journal-of-trauma-orthopaedics/journal-of-traumaorthopaedics-and-coronavirus/from-elective-orthopaedic-centre-to-acovid-19.html .
- 13.NHS England. Clinical Guide for the Perioperative Care of People with Fragility Fractures during the Coronavirus Pandemic. [Last accessed on 2020 May 31];2020 https://www.england.nhs.uk/corohttps://www.england.nhs.uk/coronavirus/wpcontent/uploads/sites/52/2020/03/C0086_Specialty-guide-_Fragility-Fractures-and-Coronavirus-v1-26-March.pdf. [Google Scholar]
- 14.Pichard R, Kopel L, Lejeune Q, Masmoudi R, Masmejean EH. Impact of the Coronavirus Disease 2019 lockdown on hand and upper limb emergencies: experience of a referred university trauma hand centre in Paris, France. Int Orthop. 2020;44:1497–501. doi: 10.1007/s00264-020-04654-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dayananda K, Yasin T, Jemmett P, Trickett R. The Impact and Changes to Trauma Services in Cardiff. [Last accessed on 2020 Jun 05]. Available from: https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/covid-19-the-impactand-changes-to-trauma-services.html .
- 16.Jenkins P. The Early Effect of COVID-19 on Trauma and Elective Orthopaedic Surgery. 2020. [Last accessed on 2020 May 31]. Available from: https://www.boa.ac.uk/ policy-engagement/journal-of-trauma-orthopaedics/journal-of-traumaorthopaedics-and-coronavirus/the-early-effect-of-covid-19-on-traumaand-elect.html .
- 17.Nepogodiev D, Bhangu A. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. [Last accessed 2020 Jun 02];Br J Surg. 2020 107:1440–9. doi: 10.1002/bjs.11746. Available from: https://bjssjournals.onlinelibrary.wiley.com/doi/abs/10.1002/bjs. 11746 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.What Has the Covid-19 Situation Done to Motorway Traffic? 2020. [Last accessed on 2020 Jun 02]. Available from: https://trl.co.uk/news/news/what-has-covid-19-situation-done-motorway-traffic .
- 19.GOV.UK: 2020. May 10, [Last accessed on 2020 May 31]. PM Address to the Nation on Coronavirus. Available from: https://www.gov.uk/government/speeches/pmaddress-to-the-nation-on-coronavirus-10-may-2020 . [Google Scholar]
- 20.Hampton M, Clark M, Baxter I, Stevens R, Flatt E, Murray J, et al. The effects of a UK lockdown on orthopaedic trauma admissions and surgical cases: A multicentre comparative study. Bone Jt Open. 2020;1:137–43. doi: 10.1302/2633-1462.15.BJO-2020-0028.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]


