Abstract
Background:
Graduate school environments are recognized for contributing to elevated stress levels among student populations.
Purpose:
The objective was to test whether a behavioral intervention, delivered through an online course on behavior change, is effective in preventing declining mental health.
Methods:
Data were collected via a quasi-experimental longitudinal study to observe the effect of self-directed behavioral interventions on mental health. Participants included students enrolled in a course on Health Behavior Change at the Yale School of Public Health (n = 45) and a control group (n = 33) of students in the same graduate program. Analyses were conducted to evaluate differences at post-intervention and at a 12-week follow-up assessment in indicators of mental and general health.
Results:
Enrolled students reported significantly improved mental health outcomes as compared to the control students. At follow-up, multiple differences persisted, with participants who had completed the course reporting sustained improvements in general and mental health.
Discussion:
Self-directed behavior change interventions are effective in promoting mental and physical health among graduate student populations.
Translation to Health Education Practice:
This curriculum-based intervention can support student wellbeing in a variety of academic programs.
Background
The World Health Organization defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”1 Implicit in this definition is that mental health is a critical component of overall wellbeing, and that mental illness necessarily undermines overall health. Indeed, mental disorders are now recognized as a significant chronic health issue,2 and promoting mental health is a top health priority for the United States and global health organizations.1 From an epidemiologic perspective, mental illness is a prevalent condition, with nearly half of American adults experiencing a mental disorder at some point in their lifetime.3 Depression and anxiety are especially common,4 and cause significant impairment and disability,5 highlighting the need for effective treatment and prevention programs. Prevention programs for mental health aim to identify and mitigate risk factors.1,6,7
Early adulthood, corresponding developmentally with matriculation in higher education, is a high-risk period for the onset of mental illness.3 Graduate school environments are recognized for contributing to stress among student populations.8,9 Elevated rates of anxiety and depression among graduate students have been well documented.9,10 While studies of educational burnout and mental health frequently focus on medical students,11-15 a growing body of research has focused on students in other graduate and professional programs.16-18 Chronic stress from a combination of academic pressure and non-academic responsibilities cultivate a landscape for poor health outcomes wherein students may engage in maladaptive coping strategies in order to manage stress. These strategies include selfisolation, poor nutrition choices, lack of physical exercise, and substance misuse.19
To address graduate student stress, a range of strategies is likely needed beyond those offered by university health services. Self-stigma regarding mental health, for example, is shown to influence the ways in which individuals seek psychological treatment, with evidence suggesting that self-stigma may prevent people from seeking professional help.20 Self-care interventions might offer a means of reducing stress and mental health stigma, thereby bolstering the odds of formal help-seeking when needed. When implemented routinely, self-care interventions can be an effective strategy for students to manage areas of physical health and wellness including nutrition and physical activity.21,22
Preliminary evidence suggests that self-directed interventions may equip graduate students with tools to individually manage their mental health.21,22 In the first iteration of this research, data were collected from public health graduate students enrolled in a survey course teaching principles of behavior change. Students in the course administered self-care interventions by applying behavior change principles to create goals related to health promotion. The study reported increased engagement in self-care behaviors across multiple domains, which were associated with mental health outcomes. A follow-up study22 examined the effect of the curriculum-based intervention within the context of a distance-learning course and reported similar improvements among enrolled students.
Purpose
The purpose of the current study was to examine the effectiveness and durability of a behavioral self-care intervention delivered in the context of an online course. The course provides a curriculum-based behavioral self-care intervention. Participants were graduate students in the School of Public Health. The methodology implemented was designed to support and extend previous conclusions about the efficacy of self-directed behavioral interventions for health promotion among graduate students. The current study also included a control group of students from the same competitive degree program to examine the saliency of the intervention in influencing self-care behaviors and psychological outcomes. Finally, the study included a follow-up assessment point, occurring 12 weeks following the conclusion of the course, to examine the durability of the intervention.
Methods
Participants
Participants in the intervention were 45 students enrolled in a graduate course, Foundations of Health Behavior Change, through the Yale School of Public Health. Control participants (n = 33) were students enrolled in the same competitive degree program. A chance to win a 200 USD gift card was offered to all students in exchange for their participation.
Procedure
The study was granted an exemption from IRB review under federal regulation 45 CFR 46.101(b)(1) by the Yale University Human Subjects Review Board. After providing informed consent, students completed an anonymous survey during the first week of the semester, again during the last week of the semester (approximately 12 weeks later), and again 12 weeks following the conclusion of the intervention (i.e., the course). Students were enrolled in the online course delivered through Canvas, the university’s online course management platform. Students were required to watch video lectures and to complete assignments weekly throughout the semester. Control participants were sent the links for the online assessment measures at the beginning and end of the semester, and again for the follow-up assessment.
Course description and content
The educational setting was a course, Foundations of Health Behavior Change, offered through the Yale School of Public Health. The course content was delivered online; students were required to log on to the course website at least weekly, and to watch prerecorded video lectures. The curriculum has been described previously.21,22 In brief, students are taught the fundamentals of behavior change theory with a focus on the integration of social, psychological, and behavioral factors in promoting health behaviors. Evidence-based practices are emphasized for implementation of behavior change strategies that students may eventually produce in broader public health settings. The content progresses through four distinct modules, focusing on nutrition, mental health, physical activity, and social support. Each module covers the relevance of health behaviors to chronic disease; e.g., the nutrition unit discusses the role of nutrition in chronic disease and research on clinical treatments and public health interventions for improved nutrition. The mental health unit discusses the epidemiology of mental health disorders, empirically supported treatments for mental health disorders, mental health stigma and other obstacles to treatment, diversity issues and mental health (i.e., structural/systemic factors affecting mental health), and public health interventions for promoting mental wellness. The full course outline appears in the online Supplemental file for this article; assigned readings, slide decks, and assignments are available from the senior author (M.W.) upon request. Assignments focused on testing behavior change strategies with respect to individually selected behavioral goals in each domain. For example, a sample assignment was to apply a behavioral strategy to modify a small measurable goal (e.g., “engage in deep breathing for 5 minutes each day”) within the mental health unit for 5 days. After the 5-day period, students had the option to earn extra credit points for maintaining the behavior change for the duration of the semester. Goal completion was monitored via self-report, collected through Qualtrics surveys distributed weekly. The approach parallels the best practice self-report procedures employed by behavioral health interventions.23
Students adhering to their goals for >90% of the days of the semester were given 10 bonus points to their grade, which amounted to an increase in a full letter grade for the term. Students achieving less were also granted bonus points in a stepped fashion: 80–89% of daily goals resulted in 7 bonus points; 60–79% of daily goals received 5 points; and 30–59% received 3 points. A summary of the most commonly chosen health behaviors and examples of the person-level behavior change strategies appears in Table 1.
Table 1.
Example behavioral goals and behavioral strategies selected by students.
| Nutrition (11 weeks) |
Mental Health (8 weeks) |
Physical Activity (5 weeks) |
Social Support (2 weeks) |
Behavioral Strategy |
|---|---|---|---|---|
| Log all intake (complete food records using an app) | Limit blue light before bed, decrease screen time | Increase aerobic activity (specified time) | Attend religious services | Token economy/reinforcement |
| Drink 64 oz. of water/day | Prayer or gratitude journal | Take stairs instead of elevator | Call family | Prompting |
| Eat mindfully (at table, technology-free) | Deep breathing 4x/day | Stretching | Schedule social activities (non-academic) | Premack principle |
| Eat 1 serving of fresh fruit/day | Pleasure reading | Increase walking (specified steps) | Write letters | Response cost |
| Eliminate soda | Creative activities | Attend exercise class | Acts of kindness |
Behavioral tracking
As is commonly utilized in interventions for health behaviors, students completed monitoring records for all targeted behaviors and submitted these on a weekly basis. Links to the behavioral tracking measure were posted on the course website and students received regular reminder prompts. The behavioral tracking measure required reporting of the specific goal and a daily record of whether or not the goal had been achieved. Final adherence scores were calculated as the percentage of days achieving the goals, with a maximum possible score of 182 daily goals achieved.
Measures
Students completed a self-report questionnaire battery about personal health behaviors and mental health outcomes. The battery included validated measures and key items drawn from national longitudinal health surveys.24-26 The survey took approximately 15 min to complete.
Nutrition
Nutritional variables were derived from large-scale epidemiologic surveys (e.g. the National Health and Nutrition Examination Survey) and focused on the frequency of consuming specific types of foods over the previous week. Questions regarding nutrition addressed the quantity of servings the student consumed of various food types over the course of the previous week, including red meat, processed meats, dairy, fruit, vegetables, sweets/fast food, and whole grains.
Physical activity
The Godin Leisure Time Exercise Questionnaire (GLTEQ) is commonly used to measure levels of physical activity.27,28 Physical activity is measured as frequency of mild, moderate, and strenuous exercise, with respondents asked to provide the number of days per week they engaged with each type of exercise category for >15 minutes. The GLTEQ yields a summary score, which is calculated as the combination of values reported for each type of exercise intensity to yield a metabolic equivalents of task score (METs). METs range from 0 to 119, with higher scores indicating higher levels of engagement with physical activity. A separate indicator for physical activity was the number of times, out of the previous 7 days, participants reported engaging in “rigorous” physical activity for at least 30 minutes.
Mental health
The Depression Anxiety Stress Scale 21-Item version29,30; DASS21 was used to evaluate mental health outcomes. The measure yields three subscale scores (depression, anxiety, and stress/tension) and has been found to be sensitive to clinical change.30 Scores on each subscale range from 0 to 42, with higher scores indicating greater distress. Supplementary mental health and wellness questions were sourced from the Behavioral Risk Factor Surveillance System and the Health Related Quality of Life Assessment.24,25 These questions were, “During the past month, how many days have you felt sad or depressed?” and “During the past month, how many days have you felt worried, tense, or anxious?” Options were presented on an ordinal scale ranging from 0 (no days) to 6 (21–30 days).
Perceived stress
The Perceived Stress Scale – 10 item version31,32 is a reliable and valid measure of psychological stress. Its psychometric properties have been established for use with large-scale community samples33 and university students.34 Items (e.g., “In the past month, how often have you found that you could not cope with all the things you had to do?”) are rated on a 5-point scale ranging from 0 (never) to 4 (very often), yielding total scores ranging from 0 to 40.
General self-rated health
Health perception was evaluated using three items from the National Health and Nutrition Examination Survey.26,35,36 General health perception was evaluated with, “Would you say that in general your health is – ?” ranging from 1 (Poor) to 5 (Excellent). Perceived health change was evaluated with “Compared to a year ago, how has your health changed?” ranging from 1 (Much worse) to 5 (Much better). A third item was, “Compared to others your same age and sex, how would you rate your overall health?” which ranged from 1 (Much worse than average) to 5 (Much better than average).
Secondary outcomes
Self-efficacy
Self-efficacy is defined as one’s optimistic belief that one can perform novel tasks or cope with adversity. In the current study, global self-efficacy was measured with the 10-item General Self-Efficacy Scale,37 which has demonstrated acceptable psychometric properties for use with university students.38 Items (e.g., “I am confident that I could deal with unexpected events”) are rated on a 4-point scale ranging from “not at all true” to “exactly true,” yielding a total score range of 10 to 40.
Mental health stigma
Self-stigma regarding mental health was evaluated with the 10-item Self-Stigma of Seeking Help scale.20,39 Questions from this assessment include “I would feel inadequate if I went to a therapist for psychological help” and “My view of myself would not change just because I made the choice to see a therapist.” Response options range from “Strongly Agree” to “Strongly Disagree.” Scores can range from 10 to 50, with higher scores indicating greater stigma associated with seeking help for mental health treatment.
Social support
Social support was measured with a single item, “How satisfied are you with your social life (relationships with friends and/or partner)?” Responses could range from 1 (not satisfied) to 4 (very satisfied).40
Post-intervention and follow-up behavioral adherence measure
Additional questions evaluated adherence to the individually chosen behavioral goals – e.g., “Considering each of the behavior change goals, on approximately what percentage of days did you achieve your goal?” Thus, there were four separate adherence measures, one for each of the behavior change modules.
Statistical analysis
Data were downloaded directly from the survey collection service (Qualtrics.com) and analyzed with SPSS. Missing data on the anonymous self-report were excluded from analysis. Varying rates of participation at post-intervention and follow-up precluded the ability to use longitudinal data analytic methods (i.e., repeated measures analysis). Analysis of covariance, controlling for baseline values, was used to examine group differences in mental health and general health outcomes at the post-intervention and follow-up assessment points. Correlation (Pearson’s r) was used to test associations among health behaviors and mental health outcomes. Alpha of .05 was used to determine statistical significance.
Results
Behavioral adherence
Behavioral tracking scores
The duration of the behavioral goal setting period was 11 weeks, staggered across each of the behavioral modules. Thus, each student had the opportunity to achieve the nutrition goal on 77 days, mental health on 56 days, physical activity on 35 days, and social support on 14 days, for a total behavioral adherence score of 182. The average number of daily behavioral goals met was 115 (range 0– 182). Proportionally, 31% (n = 15) of the students met their behavioral goals on at least 90% of days (score of 164 or higher). Another 17% (n = 8) met 80–89% of their daily behavioral goals, and 17% of students (n = 8) achieved between 60% and 79% of their daily goals, with 6% (n = 3) reporting 30–59%. Another 30% (n = 14) reported achieving <30% of the daily goals. However, it is possible that these values are underestimates, in that some students opted not to submit weekly tracking.
The majority of students (94%, n = 45) completed the anonymous post-intervention assessment. Measured in the post-intervention retrospective assessment, students reported achieving their behavioral goals for the majority of the semester. The average goal attainment across behavioral domains was: 77% of days for nutrition (range 6–100), 74% (range 5–100) for mental health, 77% (range for physical activity), and 85% (range 7 to 100) for social support. Combined across all four behavioral domains, 40% of students reported achieving at least 90% of their daily behavioral goals, 18% reported meeting between 80% and 89% of the daily goals, and 29% achieved between 60% and 79% of their daily goals. It should be noted that these values were estimates, provided retrospectively via self-report. Figure 1 is a graphic depiction of the retrospective reports as compared to the prospective reports and demonstrates that the retrospective data likely over-estimated the degree of goal attainment. Except for the lowest category, which reflects missing weekly behavioral tracking logs, the retrospective reports aligned with the values provided prospectively over the semester via the behavioral monitoring records.
Figure 1.
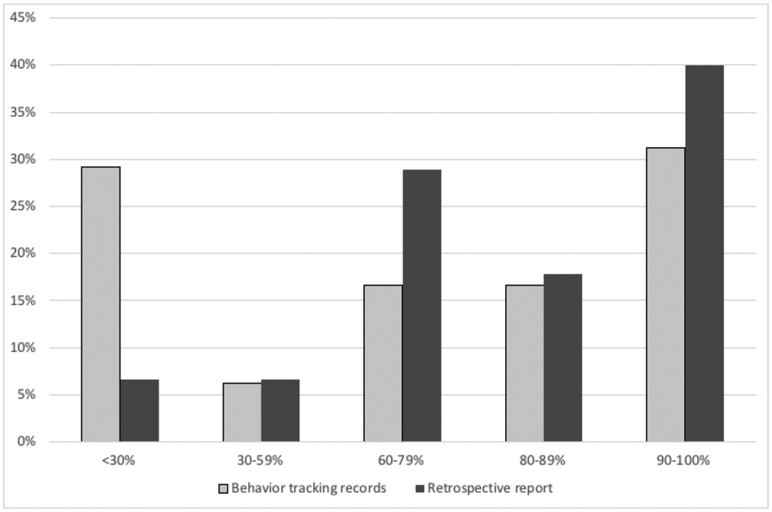
Percent goal attainment, according to behavioral tracking records collected prospectively and retrospective self-report. Goal percentage is based on 182 possible daily goals.
Behavioral goal attainment was also assessed at the 12-week follow-up. Although the course had concluded (and the external incentive had been removed), students reported continued engagement in their behavioral goals. The average daily goal attainment reported was 62% in aggregate, with domain-specific attainment being 64% for nutrition, 50% for mental health, 74% for physical activity, and 62% for social support goals. Although behavioral goal attainment was significantly lower during the follow-up period (t[30] = 5.52, p < .001), there was a significant correlation between goal attainment achieved during the semester and goal attainment in the follow-up period (r(30) = .69, p < .001).
Primary and secondary outcomes
The primary outcomes were scores on the DASS21 anxiety, depression, stress, and total scale scores, as well as the frequency of experiencing depressed and anxious days. The related constructs of mental health stigma and self-efficacy were also tested. Although secondary to our aims to evaluate changes in mental health outcomes, we also included analyses comparing the experimental groups on general health indicators – i.e., general health perception, perceived changes in health as compared to 1 year prior, and perception of health in relation to others of the same age and sex. Baseline, post-intervention, and follow-up scores for the enrolled and control students are presented in Table 2. Analysis of covariance compared groups (enrolled vs. control) on key outcomes, controlling for baseline values.
Table 2.
Health behavior outcomes at baseline, post, and follow up for enrolled and control students.
| Baseline |
Post-Intervention |
Follow-up |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control (n = 36) |
Enrolled (n = 46) |
Control (n = 25) |
Enrolled (n = 45) |
Control (n = 35) |
Enrolled (n = 33) |
|||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Nutrition (# of servings/week) | ||||||||||||
| Vegetable | 10.9 | (7.2) | 9.8 | (7.1) | 12.7 | (7.9) | 13.5 | (8.3) | 11.3 | (6.9) | 11.7 | (7.8) |
| Fruit | 9.2 | (7.3) | 7.8 | (6.1) | 9.0 | (6.9) | 10.3 | (7.5) | 8.9 | (5.9) | 10.8 | (7.6) |
| Dairy | 6.5 | (6.5) | 6.3 | (5.5) | 8.7 | (7.2) | 6.7 | (5.7) | 6.3 | (6.5) | 5.9 | (4.4) |
| Sweets | 3.3 | (2.3) | 5.0 | (5.4) | 5.0 | (4.0) | 5.0 | (4.9) | 4.6 | (3.7) | 5.5 | (5.5) |
| Red meat | 1.2 | (1.3) | 1.0 | (1.1) | 1.0 | (1.4) | 0.9 | (0.7) | 0.9 | (0.8) | 0.8 | (0.5) |
| Processed meat | 0.6 | (0.9) | 0.7 | (0.9) | 0.8 | (1.2) | 0.6 | (0.8) | 0.7 | (1.0) | 0.5 | (1.0) |
| Whole grains | 1.8 | (1.3) | 1.4 | (1.0) | 1.5 | (1.3) | 1.4 | (0.8) | 1.5 | (1.3) | 1.4 | (0.8) |
| Mental Health | ||||||||||||
| Depressed days past month | 5.7 | (5.1) | 3.6 | (2.7) | 6.6 | (6.1) | 4.1 | (3.4) | 5.4 | (4.7) | 5.0 | (5.8) |
| Anxious days past month | 11.4 | (7.8) | 7.9 | (5.6) | 13.3 | (8.1) | 7.7 | (6.2) | 11.4 | (8.0) | 9.1 | (7.6) |
| DASS Stress | 12.4 | (6.8) | 12.2 | (7.2) | 13.8 | (8.9) | 8.0 | (5.4) | 14.6 | (10.4) | 11.4 | (8.3) |
| DASS Anxiety | 7.1 | (6.8) | 6.9 | (5.9) | 6.3 | (6.7) | 4.9 | (4.8) | 8.2 | (9.3) | 5.1 | (5.2) |
| DASS Depression | 8.4 | (6.5) | 8.7 | (8.0) | 8.9 | (8.1) | 5.6 | (5.5) | 10.3 | (8.5) | 7.0 | (7.7) |
| DASS Total | 14.0 | (7.7) | 14.0 | (9.1) | 14.5 | (10.2) | 9.1 | (6.0) | 16.6 | (12.5) | 11.7 | (9.5) |
| Perceived Stress | 18.3 | (4.5) | 16.8 | (5.9) | 19.8 | (6.0) | 17.0 | (5.8) | 19.8 | (5.1) | 15.7 | (7.6) |
| Self Efficacy | 31.8 | (3.4) | 31.8 | (4.6) | 30.2 | (3.9) | 32.0 | (4.2) | 30.5 | (4.5) | 32.2 | (5.3) |
| Stigma | 20.9 | (8.0) | 20.2 | (7.5) | 20.3 | (8.6) | 18.2 | (5.8) | 20.2 | (7.3) | 17.2 | (6.2) |
| Physical Activity | ||||||||||||
| Rigorous activity (past week) | 2.2 | (1.9) | 2.3 | (2.1) | 2.3 | (2.1) | 3.4 | (1.7) | 2.1 | (1.8) | 3.5 | (1.9) |
| Godin (METs) | 43.8 | (26.4) | 44.4 | (30.7) | 37.2 | (31.5) | 53.3 | (27.6) | 43.5 | (31.6) | 57.3 | (30.0) |
| Social | ||||||||||||
| Social life satisfaction | 2.9 | (0.5) | 3.5 | (0.6) | 2.7 | (0.8) | 3.4 | (0.8) | 2.9 | (0.7) | 3.5 | (0.7) |
| Perceived health status | ||||||||||||
| General health perception (1 = poor; 5 = excellent) | 3.7 | (0.8) | 3.7 | (0.8) | 3.6 | (0.8) | 3.7 | (0.7) | 3.6 | (0.8) | 3.9 | (0.5) |
| Change in general health (1 = much worse; 5 = much better) | 3.4 | (0.9) | 3.3 | (1.0) | 3.0 | (0.8) | 3.5 | (1.0) | 3.3 | (0.7) | 4.0 | (1.0) |
| Compared to others same age and sex (1 = much worse; 5 = much better | 3.4 | (0.8) | 3.4 | (0.7) | 3.2 | (0.8) | 3.6 | (0.7) | 3.1 | (0.8) | 3.6 | (0.7) |
Post intervention – mental health outcomes
At the end of the semester, after controlling for baseline values, the enrolled group reported significantly lower scores than the control group on DASS Total score (F(1,62) = 7.27, p = .01), DASS Stress (F(1,64) = 10.91, p = .002), and DASS Depression (F(1, 64) = 4.54, p = .04). Differences approached significance for frequency of depressed days (F(1, 67) = 3.94, p = .05) and frequency of anxious days (F(1, 67) = 3.081, p = .08). The enrolled students reported significantly higher self-efficacy scores at post-intervention, F(1, 64) = 5.93, p = .02. At post-intervention, the groups did not differ on DASS Anxiety, Perceived Stress Scale scores, or mental health stigma. The patterns of improvement in key mental health outcomes, depicted in change scores from baseline values, are presented in Figure 2.
Figure 2.
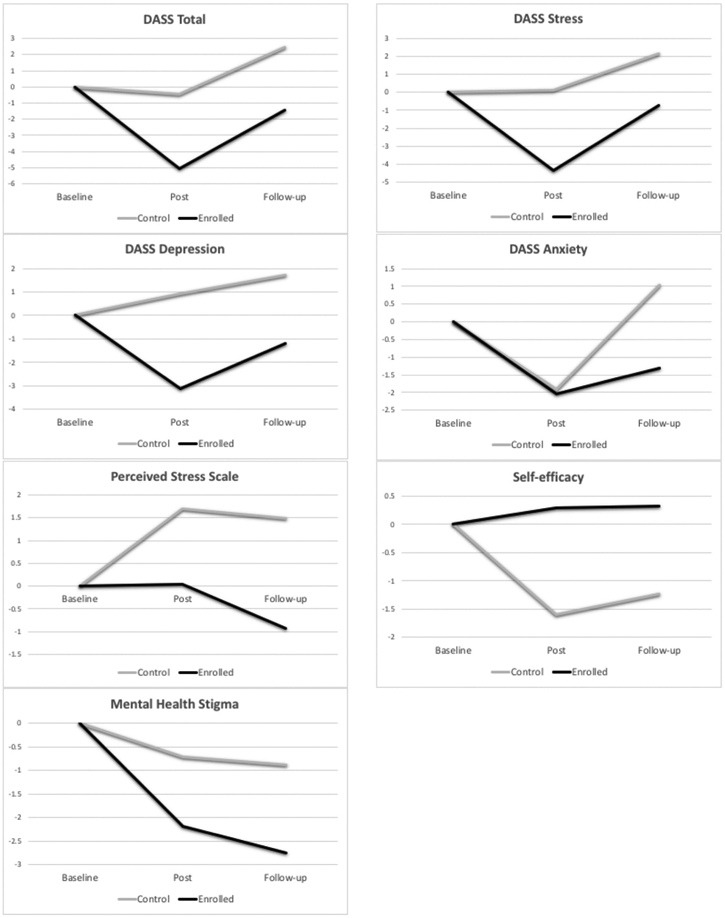
Changes in mental health outcomes.
Post intervention – general health outcomes
After controlling for baseline values, enrolled students reported significantly higher perceived improvement in health as compared to 1 year prior (F(1, 67) = 5.85, p = .02. Group comparisons in perceived health as compared to others of the same age and sex approached significance, F(1, 67) = 3.78, p = .06. The groups did not differ with respect to overall perception of health, F(1, 67) = 0.58, p = .45. The patterns of changes in general health outcomes, depicted as change scores from baseline values, are presented in Figure 3.
Figure 3.
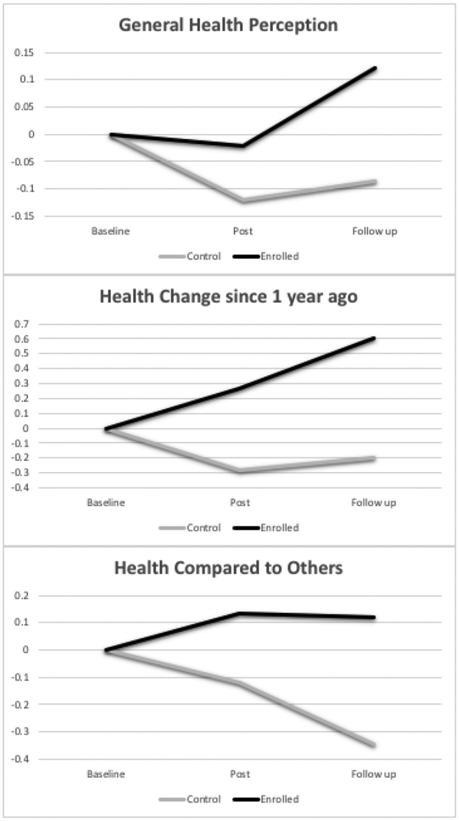
Changes in general health perception.
Follow-up – mental health outcomes
At the 12-week follow-up assessment, after controlling for baseline values, enrolled students reported significantly lower scores on the Perceived Stress Scale (F(1, 61) = 4.71, p = .03) than students in the control group. Group comparisons for other outcomes were marginal or not significant: DASS total (F(1, 63) = 2.97, p = .09), DASS Depression (F(1,64) = 3.14, p = .08), DASS Stress (F(1, 65) = 2.14, p = .15), self-efficacy (F(1, 64) = 2.89, p = .09), and stigma scores (F (1, 65) = 3.66, p = .06).
Follow-up – general health outcomes
At follow-up, the enrolled students reported significant perceived health improvement (F(1, 65) = 14.14, p < .001) and higher ratings of their health as compared to students in the control group (F(1, 65) = 11.15, p < .001). Groups did not differ with respect to general health perception, F(1, 65) = 2.48, p = .12.
Exploratory analyses
To examine potential mechanisms of change among enrolled students, correlation analysis evaluated whether percent goal attainment was significantly associated with mental and general health outcomes. At post-intervention, daily goal achievement was positively correlated with general health perception (r(43) = .54, p < .001) and with perceived improvement in health as compared to 1 year prior (r(43) = .36, p = .01). At follow-up, daily goal achievement was positively associated with general health perception (r(31) = .35, p = .04).
Discussion
The primary goal of this study was to determine if students enrolled in a behavior change course experienced improvements in mental health following engagement in self-directed behavior change practices. Health promotion behaviors were encouraged across multiple domains, including mental health, physical activity, and nutrition to allow for more specific critical analysis. Previous studies evaluating the effectiveness of behavioral self-care interventions found significant improvements in nutrition and physical activity goals.21,22 This study supports these findings and adds to the existing body of research by employing validated measures of mental health, a control group of students from the same competitive program, and a follow-up period.
This study is a notable addition to the existing research as it suggests that self-directed behavior change interventions may improve student mental health. Among the improved outcomes in mental health experienced by enrolled students were lower stress and depression following the intervention, relative to the control group. Significantly lower perceived stress was also observed at the follow-up assessment, suggesting that the intervention had lasting effects into the subsequent academic semester. The inclusion of an equivalent control group was an important addition to this study, particularly when compared to previous iterations of this research.21,22 Results from the exploratory analysis of enrolled students further suggest that instruction in behavior change theory may contribute to greater adherence to behavior change goals that, in turn, may result in more significant rates of health promotion.
As of the findings from this study, three independent cohorts have been evaluated to determine whether self-directed behavioral interventions contribute to health promotion among graduate student populations. Applying identical methods of data collection to different groups of students over time contributes to the validity of existing research and is likely to encourage researchers to continue this work.
There are a few limitations to the study that should be considered. The quasi-experimental design of this study does not allow for randomization, which limits the ability to draw conclusions about causality between the intervention and outcomes measured. For example, it could be that students who enrolled in the course had greater motivation to change their behaviors than those in the control group, which could account in part for differences at post-intervention and follow-up. However, since completion of personal behavior change was not specified in the course directory or syllabus, this bias is minimized. Alternatively, a potential benefit of quasi-experimental design is real-world generalizability. This can be considered a trade-off for the benefits of choosing to conduct a randomized controlled trial (RCT) instead of utilizing a quasi-experimental design. RCTs typically have more complex requirements in terms of implementation and would have presented challenges to data collection for this study.41 It is also possible that the self-report structure of responses to some survey questions resulted in recall bias (for example, asking students to recall the specific number of anxious or depressed days experienced within the last 30 days). However, given that both the control and enrolled students completed identical assessments, this bias is minimized. Finally, the relatively small and homogenous sample size (graduate students enrolled in a public health program at Yale University) may limit the study’s generalizability. Conclusions drawn in this paper might not translate to other student populations given differences between academic programs, their requirements, and students’ lived experiences.
Despite these limitations, the current findings indicate that self-directed behavioral interventions implemented by students enrolled in this course on health behavior change were effective in promoting healthy behaviors at various intervals including post-intervention (the conclusion of the course) and follow-up (12 weeks after the conclusion of the course). Significant findings from the enrolled participants included reductions in measurements of stress and depression, and improvements in general health perception. These findings add to existing evidence from literature regarding the health promotion benefits of self-directed behavioral interventions.
Translation to Health Education Practice
The findings, when combined with results from similar previous studies,21,22 present evidence that self-directed behavioral interventions are effective in promoting healthy behaviors among graduate students. Given what is known about stress and mental health crises among the graduate student population, applying the model used in this health behavior change course to students in other academic programs and at other academic institutions is recommended.
It is additionally worth noting that coursework where students are graded on behavioral performance, as opposed to academic performance, is novel in the context of academics. Requiring a course like the one described herein as part of the curriculum for public health and behavioral science students, for example, could provide students with a stronger foundation to implement behavioral interventions in post-graduate professional settings. A study following students formerly enrolled in the course in their post-graduate careers could evaluate this hypothesis.
Future research could also evaluate the effectiveness of this curriculum-based intervention when applied to a community sample of learners. Since the behavioral intervention described here is now being delivered through a Massive Open Online Course (MOOC), future research is needed to determine whether it generalizes to that platform and could thus serve as a mental health intervention for a global audience of MOOC learners. With increasing preference and/or necessity of distance-learning platforms, implementation of wellness interventions through the media described in this paper may represent an appropriate avenue for improving mental health outcomes.
Areas of responsibility for health education specialists
Planning, Implementing, and Evaluating Health Education/Promotion: Health Educators and Certified Health Education Specialists can use the methods and results of this study in designing and implementing similar interventions in their respective populations of interest. Lecture material, readings, assignments, and assessment tools are available from the senior author (M.W.) upon request. In developing curricula and interventions, Health Educators may also access some of the course content at no charge through Coursera.org, which is currently hosting an abbreviated version of the course.
Adapting intervention for population of interest
While the curriculum and intervention described here were designed for advanced public health students (i.e., graduate students), it is adaptable for beginner or non-academic audiences, independent of educational attainment. Health Educators are encouraged to employ focus groups and to pilot the intervention prior to full delivery to evaluate the appropriateness of the curriculum and intervention for the particular population. Finally, Health Educators are encouraged to evaluate the effectiveness and durability of their interventions, by administering validated assessments of mental and physical wellbeing prior to and following delivery of the intervention.
Supplementary Material
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental data for this article can be accessed on the publisher’s website.
References
- 1.World Health Organization. Prevention of mental disorders. https://www.who.int/mental_health/evidence/en/prevention_of_mental_disorders_sr.pdf. Published 2004. Accessed January 2020
- 2.Eifert EK. Introduction to special issue on mental disorders as a chronic issue. Am J Health Educ. 2019;50(4):207–209. doi: 10.1080/19325037.2019.1621645. [DOI] [Google Scholar]
- 3.Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s world mental health survey initiative. World Psychiatry. 2007;6(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD Disease Injury. Incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saxena S, Jane-Llopis E, Hosman C. Prevention of mental and behavioural disorders: implications for policy and practice. World Psychiatry. 2006;5:5–14. [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Risks to mental health: an overview of vulnerabilities and risk factors. Background paper by WHO secretariat for the development of a comprehensive mental health action plan. https://www.who.int/mental_health/mhgap/risks_to_mental_health_EN_27_08_12.pdf. Published August 2012. Accessed January 2020. [Google Scholar]
- 8.Bullock G, Kraft L, Amsden K, et al. The prevalence and effect of burnout on graduate healthcare students. Canadian Medical Education Journal. 2017;8(3):e90–e108. PMID: 29098051; PMCID: PMC5661741. doi: 10.36834/cmej.36890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oswalt S, Riddock C. What to do about being overwhelmed: graduate students, stress, and university services. Coll Student Affairs J. 2007;27:24–44. [Google Scholar]
- 10.Arnold C Paying graduate school’s mental toll. Science. http://www.sciencemag.org/careers/2014/02/paying-graduate-schools-mental-toll. Published February 4, 2014. Accessed January 2020. [Google Scholar]
- 11.Brazeau CM, Shanafelt T, Durning SJ, et al. Distress among matriculating medical students relative to the general population. Acad Med. 2014;89(11):1520–1525. doi: 10.1097/ACM.0000000000000482. [DOI] [PubMed] [Google Scholar]
- 12.Dyrbye LN, Satele D, Shanafelt TD. Healthy exercise habits are associated with lower risk of burnout and higher quality of life among U.S. medical students. Acad Med. 2017;92(7):1006–1011. doi: 10.1097/ACM.0000000000001540. [DOI] [PubMed] [Google Scholar]
- 13.Dyrbye LN, West CP, Satele D, Boone S, Sloan J, Shanafelt TD. A national study of medical students’ attitudes toward self-prescribing and responsibility to report impaired colleagues. Acad Med. 2015;90(4):485–493. doi: 10.1097/ACM.0000000000000604. [DOI] [PubMed] [Google Scholar]
- 14.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–451. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 15.Jackson ER, Shanafelt TD, Hasan O, Satele DV, Dyrbye LN. Burnout and alcohol abuse/dependence among U.S. medical students. Acad Med. 2016;91 (9):1251–1256. doi: 10.1097/ACM.0000000000001138. [DOI] [PubMed] [Google Scholar]
- 16.Erevik EK, Torsheim T, Ø V, Andreassen CS, Pallesen S. Alcohol use among business students: demographic, personality, and social correlates of increased consumption. Scand J Educ Res. 2017;62(6):900–910. doi: 10.1080/00313831.2017.1307277. [DOI] [Google Scholar]
- 17.Myers SB, Sweeney AC, Popick V, Wesley K, Bordfeld A, Fingerhut R. Self-care practices and perceived stress levels among psychology graduate students. Train Educ Prof Psych. 2012;6:55–66. [Google Scholar]
- 18.Silverstein ST, Kritz-Silverstein D. A longitudinal study of stress in first-year dental students. J Dental Educ. 2010;74(8):836–848. doi: 10.1002/j.0022-0337.2010.74.8.tb04940.x. [DOI] [PubMed] [Google Scholar]
- 19.Wyatt T, Oswalt SB. Comparing mental health issues among undergraduate and graduate students. Am J Health Educ. 2013;44(2):96–107. doi: 10.1080/19325037.2013.764248. [DOI] [Google Scholar]
- 20.Dl Wn V, Haake S. Measuring the self-stigma associated with seeking psychological help. J Counsel Psych. 2006;53 (3):325–337. doi: 10.1037/0022-0167.53.3.325. [DOI] [Google Scholar]
- 21.White MA, Mayer M, Vanderlind WM, Allswede D. Evaluation of a behavioral self-care intervention for public health students. Am J Health Educ. 2018;49 (1):40–47. doi: 10.1080/19325037.2017.1369199. [DOI] [Google Scholar]
- 22.White MA, Whittaker SD, Gores AM, Allswede D. Evaluation of a self-care intervention to improve student mental health administered through a distance-learning course. Am J Health Educ. 2019;50(4):213–224. doi: 10.1080/19325037.2019.1616012. [DOI] [Google Scholar]
- 23.Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium. Hlth Psych. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Measuring Healthy Days. Atlanta, GA: CDC; 2000. [Google Scholar]
- 25.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 26.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey Questionnaire. In: National Center for Health Statistics (NCHS). Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 27.Amireault S, Godin G. The Godin-Shephard leisure-time physical activity questionnaire: validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept Motor Skill. 2015;120(2):604–622. doi: 10.2466/03.27.PMS.120v19x7. [DOI] [PubMed] [Google Scholar]
- 28.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–146. [PubMed] [Google Scholar]
- 29.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety & Stress Scales. 2nd ed. Sydney, AU: Psychology Foundation; 1995. [Google Scholar]
- 30.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- 31.Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan SaO S, ed. The Social Psychology of Health. Newbury Park, CA: Sage; 1988:31–67. [Google Scholar]
- 32.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 33.Lee E-H. Review of the psychometric evidence of the perceived stress scale. Asian Nursing Res. 2012;6(4):121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Roberti JW, Harrington LN, Storch EA. Further psychometric support for the 10-item version of the perceived stress scale. J College Couns. 2006;9(2):135–147. doi: 10.1002/j.2161-1882.2006.tb00100.x. [DOI] [Google Scholar]
- 35.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eriksson I, Unden AL, Elofsson S. Self-rated health. Comparisons between three different measures. Results from a population study. Int J Epidemiol. 2001;30(2):326–333. doi: 10.1093/ije/30.2.326. [DOI] [PubMed] [Google Scholar]
- 37.Schwarzer R, Jerusalem M. The general self-efficacy scale (GSE). Anxiety Stress Coping. 2010;12:329–345. [Google Scholar]
- 38.Scholz U, Doña BG, Sud S, Schwarzer R. Is general self-efficacy a universal construct? Psychometric findings from 25 countries. Euro J Psych Assmt. 2002;18 (3):242–251. doi: 10.1027//1015-5759.18.3.242. [DOI] [Google Scholar]
- 39.Vogel DL, Armstrong PI, Tsai PC, et al. Cross-cultural validity of the Self-Stigma of Seeking Help (SSOSH) scale: examination across six nations. J Couns Psychol. 2013;60(2):303–310. doi: 10.1037/a0032055. [DOI] [PubMed] [Google Scholar]
- 40.Sweet JA, Bumpass LL. The national survey of families and households-waves 1 and 2: data description and documentation. Center for Demography and Ecology, University of Wisconsin-Madison. http://www.ssc.wisc.edu/nsfh/home.htm. Published 1996. Accessed January 2020 [Google Scholar]
- 41.Harris AD, McGregor JC, Perencevich EN, et al. The use and interpretation of quasi-experimental studies in medical informatics. J Amer Med Informatics Ass. 2006;13(1):16–23. doi: 10.1197/jamia.M1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


