Abstract
Background
During infectious outbreaks like COVID-19, it is essential that every healthcare personnel (HCP) strictly adheres to infection prevention and control (IPC) policies. To boost IPC measures, training to reinforce preventive practices, which are pertinent to needs and encompass the expectations of the HCP, is indispensable. Thus, these expectations of the HCP should be explored.
Methods
In this cross-sectional descriptive survey, we used convenience sampling technique to ask the participants to list their expectations on of covid-19 IPC training paper based forms. Using the category construction approach, we organised the expectations and grouped the participants on the basis of their work and place of work to analyse the association using the chi-square test.
Results
Many participants expected to learn about the use of PPE and masks, hand hygiene, physical distancing, cleaning and disinfection, basic precautions for personal protection during the training. Expectations also included various administrative queries, sample collection and clinical skills for diagnosis and management. There was significant association of many categories of expectations with the nature and place of work in the hospital.
Conclusion
When planning IPC training, these expectations of the HCP may be carefully addressed. Information about causative agent, transmission and clinical aspects may will give a contextual meaning to IPC training. Some important preventive measures, which few participants expected to learn must be analysed in detail to understand the attitude of the HCP towards them. Efforts to appraise the HCP for the importance of these measures and promoting its practice may play a vital role to curb the spread of infectious diseases.
Keywords: Infection prevention and control, Training, Expectations, COVID-19
Introduction
Infection prevention and control (IPC) in a healthcare organisation (HCO) is an important aspect of healthcare delivery, especially when facing a pandemic. As the world is facing a crisis due to the rampant spread of COVID-19, with no definitive treatment or vaccine available, prevention remains the mainstay for mitigating the crisis. During the early stages of the pandemic, when many aspects of viral transmission were still under research and best practices to prevent transmission are still being updated, the healthcare personnel (HCP) could be in a state of dilemma about finding the right balance between saving lives and preventing themselves from getting infected. At such times, the IPC team at HCO must play many vital functions, from updating the policies to preventing panic among the professionals in providing the optimum care.
HCOs are at the frontline of handling the pandemic crisis involved in the treatment of diseased patients and prevention of the spread of infection. During such times, prevention within the premises of HCO by following strict IPC is important for a safe work environment. Moreover, a HCP who efficiently adheres to prescribed precaution act as a role model and inspiration for the rest of the community.
For the maintenance of strict IPC practices and ensuring adherence to norms, adequate training is essential. In a systematic review of literature for attitude, knowledge and practice of infection control among nurses by Nasiri et al.,1 it was revealed that most studies reported adequate knowledge and positive attitude but, average and poor practices regarding adherence to infection control standards. Thus, a periodic re-enforcement of practices, exploring the hurdles and solving the doubts with the help of planned training sessions focussing on the needs and filling the lacunae may be the key to ensure effective preventive practices. Such enhanced and upgraded training should be considered as an integral part of preparedness for infectious outbreak prevention and mitigation by an HCO.
There are many factors that potentially dictate the expectations of HCP, like the nature of the appointment, their expertise, experience level, previous training, the experience of working in similar situations and personal background, including high-risk dependents whom they take care of at home. Thus, designing relevant training sessions, encompassing these expectations and making hospital policies keeping them in mind could improve the adherence to the norms.
Stone et al.2 performed an in-depth interview-based qualitative study of infection control practices at geriatric nursing homes in the United States. They explored the legal requirement of infection control practices, the training, the practices and various hurdles to implementing effective infection control at nursing homes. Infection control should be considered as a part of continued education, and mandating a periodic update could help the HCP to be more involved and polish their skills periodically.
In this study, we have explored the expectations of HCP from IPC training for prevention of the spread of COVID-19 and have further tried to find out how the nature of their services or the healthcare settings where they were employed, dictated these expectations.
Material and methods
Study design
It was a descriptive cross-sectional survey to investigate the expectations and training needs of HCPs from the hospital infection control team (HICT) in the wake of the current pandemic. Approval from Institutional Ethical Committee (IEC) was obtained through the HICT prior to the study (IEC approval number: IEC/20/160).
Setting and participants
As part of COVID-19 pandemic preparedness of HCO, training of all the employees for IPC was undertaken by HICT. The training included classroom, video-based training sessions conducted by trained tutors and moderated by HICT. 1672 HCPs attended these mandated training and were the sampling population for our study.
The sessions were designed for small groups, according to the perceived need based on the work capacity of the employees. The HCP trained included – doctors, nursing officers (NO), hospital attendants, supervisors of housekeeping staff, security personals, administrative staff, lab operators and technicians, hospital support staff (repair and maintenance), kitchen and laundry staff. Participants were included by consecutive sampling technique and their written informed consent was obtained. Efforts were made to include most of the HCPs of the HCO who attended the IPC training between 30th March to 29th April 2020.
The video modules used for training differed according to the work expertise. All were trained regarding Do’s and Don’ts, Hand hygiene, and Environmental cleaning and disinfection. Those expected to work in COVID areas, impertinent to their work expertise, were also trained regarding Donning and Doffing of Personal protective equipment. Two training modules were especially targeted for doctors, NO and laboratory technicians viz sample collection and transport and Cardiopulmonary resuscitation (CPR).
We asked one open-ended question to all who attended the training: ‘What are your expectations from training to prevent the spread of “COVID-19” in this situation of the pandemic?’. Before the start of their training session, the participants were asked to answer the question on an individual paper-based form (Fig. 1), which was available in English and Hindi. The question was self-validated. We received consent and responses from 836 (50% of attendees), which were further analysed. We also periodically upgraded our training sessions based on the responses we received.
Fig. 1.
Specimen of form for data collection in English (Left) and Hindi (Right).
Data collection, analysis and reporting
Using a category construction approach, we began our inductive analysis with a detailed review of all the transcripts to identify various expectations and enquiries of the participants. We used open coding and memoing for our initial evaluation of the transcripts, in which interview data were repeatedly reviewed line by line to identify various categories of expectations. We assigned labels to each category and identified illustrative quotes from the responses.
These responses were collected, and the expectations were categorised into: standard precautions (hand hygiene; PPE – donning doffing and discarding; cleaning and disinfection and masks), general enquiries (physical distancing; Do’s and Don’ts; basic precautions in hospital; prevent transmission for personal safety), administrative enquiries (policies/protocols/guidelines; knowledge about the virus; managing exposure; COVID-19 isolation area; inspiring and train others), clinical skills (symptoms of COVID 19, CPR and airway management; management and care of suspected/infected COVID-19 patient; emergency and resuscitation). The accuracy of categorising process was ensured by way of cross checking by another author.
For observing how the nature of appointments affected their expectations, the participants were categorised, according to their employment, into doctors (faculties, residents, medical officers, interns, MBBS students), nursing officers (nursing tutors and nursing officers), cleaning staff (field helpers, hospital attendants, trolley man, staff supervisors, ward boys), nonmedical supportive staff (security personnel, kitchen staff and cooks, computer operator, office assistants, accountants and cashiers, ambulance drivers, arogya mitras, storekeepers, clerks) and medical support staff (lab technicians, field in charge, multipurpose social workers, radiology technicians, technical advisors, technical assistants).
HCP were further categorised based on healthcare setting in the HCO i.e. medical, surgical, critical care, diagnostics and others (administrative and academic).
Data were collected and entered in a Microsoft Excel® spreadsheet and further coded and analysed using SPSS (IBM SPSS statistics for windows version 21.0; IBM Corp., Armonk, NY, USA). To ensure that the coding scheme was well grounded in the data, supportable and consistent in meaning, codes were systematically developed and documented.
We have described the data as the frequency of expectations and compared the differences in expectations between groups using the Chi-square test. All statistical analysis is carried out at a 5% level of significance, and p-value <0.05 is considered as significant.
Results
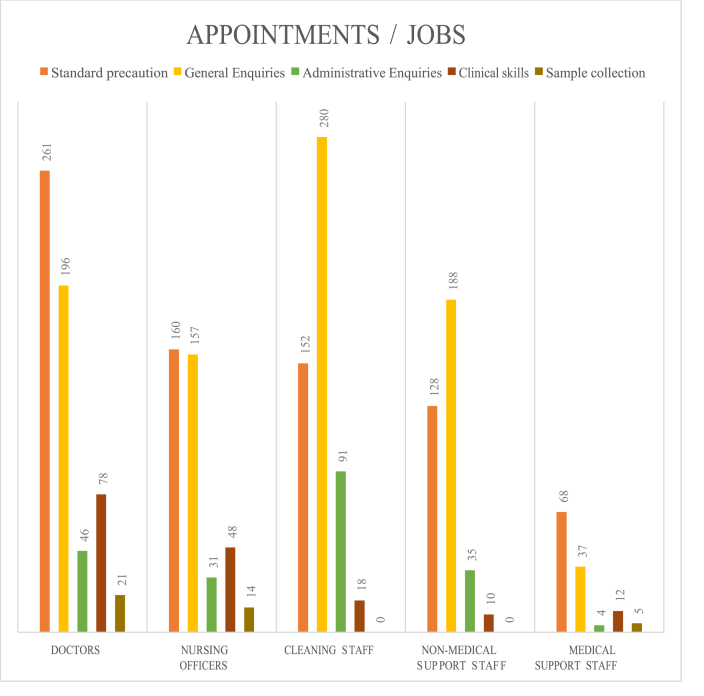
During a 2-month period, 836 HCPs participated in the study. Their expectations according to their appointments are shown in Fig. 2. The detailed expectations as frequency and percentage of participants having those expectations is given in Table 1.
Fig. 2.
Expectations of healthcare personnel distributed based on their appointments.
Table 1.
Expectations of healthcare personnel distributed according to their appointments and work.
| Doctors N = 255 |
Nursing officers N = 164 |
Cleaning staff N = 226 |
Nonmedical support staff N = 141 |
Medical support staff N = 50 |
p-value | ||
|---|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Gender | Male | 156 (61.2%) | 98 (59.8%) | 143 (63.3%) | 118 (83.7%) | 35 (70%) | <0.01 |
| Female | 99 (38.8%) | 66 (40.2%) | 83 (36.7%) | 23 (16.3%) | 15 (30%) | <0.01 | |
| Standard precautions | Hand Hygiene | 68 (26.7%) | 42 (25.6%) | 50 (22.1%) | 58 (41.1%) | 27 (54%) | <0.01 |
| PPE – Donning doffing and discarding | 153 (60%) | 94 (57.3%) | 45 (19.9%) | 14 (9.9%) | 24 (48%) | <0.01 | |
| Cleaning and disinfection | 33 (12.9%) | 17 (10.4%) | 26 (11.5%) | 14 (9.9%) | 4 (8%) | 0.80 | |
| Masks | 7 (2.7%) | 7 (4.3%) | 31 (13.7%) | 42 (29.8%) | 13 (26%) | <0.01 | |
| General enquiries | Physical Distancing | 18 (7.1%) | 36 (22%) | 35 (15.5%) | 42 (29.8%) | 18 (36%) | <0.01 |
| Do’s and Don’ts | 20 (7.8%) | 6 (3.7%) | 35 (15.5%) | 29 (20.6%) | 4 (8%) | <0.01 | |
| Basic Precautions in hospital | 61 (23.9%) | 34 (20.7%) | 115 (50.9%) | 59 (41.8%) | 4 (8%) | <0.01 | |
| Prevent transmission for Personal safety | 97 (38%) | 81 (49.4%) | 95 (42%) | 58 (41.1%) | 11 (22%) | 0.10 | |
| Administrative enquiries | Policies/protocols/guidelines | 17 (6.7%) | 8 (4.9%) | 3 (1.3%) | 0 (0%) | 0 (0%) | <0.01 |
| Knowledge about virus | 8 (3.1%) | 8 (4.9%) | 50 (22.1%) | 20 (14.2%) | 2 (4%) | <0.01 | |
| Managing exposure | 7 (2.7%) | 4 (2.4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.02 | |
| COVID-19 isolation area | 3 (1.2%) | 7 (4.3%) | 29 (12.8%) | 10 (7.1%) | 0 (0%) | <0.01 | |
| Inspire and train others | 11 (4.3%) | 4 (2.4%) | 9 (4%) | 5 (3.5%) | 2 (4%) | 0.89 | |
| Clinical skills | Symptoms of COVID-19 | 5 (2%) | 5 (3%) | 12 (5.3%) | 9 (6.4%) | 5 (10%) | 0.04 |
| CPR and Airway management | 24 (9.4%) | 13 (7.9%) | 1 (0.4%) | 0 (0%) | 2 (4%) | <0.01 | |
| Management and care of suspected/Infected COVID-19 patient | 35 (13.7%) | 25 (15.2%) | 5 (2.2%) | 1 (0.7%) | 5 (10%) | <0.01 | |
| Emergency and resuscitation | 14 (5.5%) | 5 (%) | 0 (0%) | 0 (0%) | 0 (0%) | <0.01 | |
| Sample collection | Collection, handling and transport of samples | 21 (8.2%) | 14 (8.5%) | 0 (0%) | 0 (0%) | 5 (10%) | 0.04 |
∗: Analysis was performed using Chi-square test, p-values <0.05 was considered significant.
PPE: Personal Protective Equipment; CPR: Cardiopulmonary resuscitation.
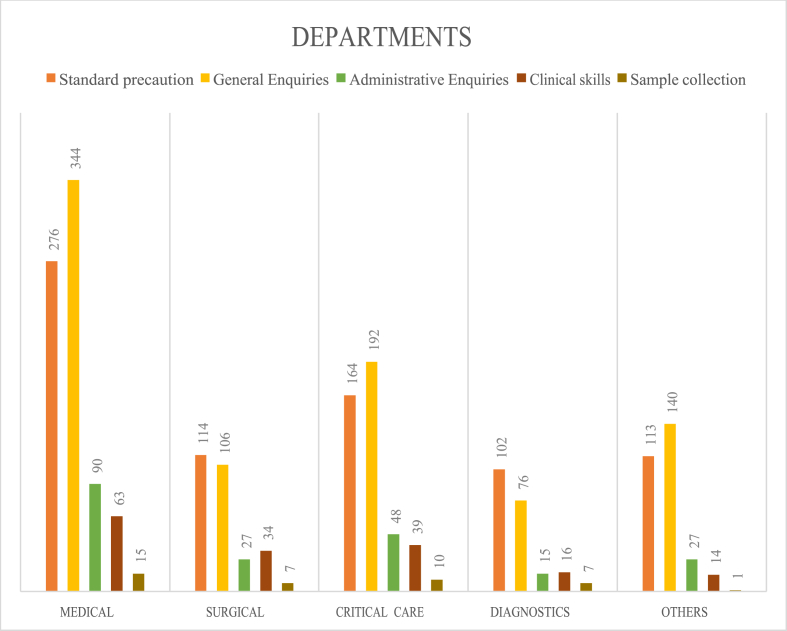
The expectations of study participants in relation to healthcare settings is shown in Fig. 3 and Table 2.
Fig. 3.
Expectations of healthcare personnel distributed based on healthcare settings in a healthcare organisation.
Table 2.
Expectations of healthcare personnel distributed according to the healthcare settings in a healthcare organisation.
| Medical (N = 325) |
Surgical (N = 126) |
Critical care (N = 178) |
Diagnostic branches (N = 86) |
Others department t (N = 121) |
p-value | ||
|---|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Gender | Male | 214 (65.8%) | 74 (58.7%) | 113 (63.5%) | 58 (67.4%) | 91 (75.2%) | 0.89 |
| Female | 111 (34.2%) | 52 (41.3%) | 65 (36.5%) | 28 (32.6%) | 30 (24.8%) | 0.82 | |
| Standard precaution | Hand Hygiene | 86 (26.5%) | 37 (29.4%) | 45 (25.3%) | 34 (39.5%) | 43 (35.5%) | 0.06 |
| PPE - Donning doffing and discarding | 131 (40.3) | 57 (45.2%) | 84 (47.2%) | 33 (38.4%) | 25 (20.7%) | <0.01 | |
| Cleaning and disinfection | 27 (8.3%) | 12 (9.5%) | 21 (11.8%) | 15 (17.4%) | 19 (15.7%) | 0.05 | |
| Masks | 32 (9.8%) | 8 (6.3%) | 14 (7.9%) | 20 (23.3%) | 26 (21.5%) | <0.01 | |
| General Enquiries | Physical Distancing | 65 (20%) | 14 (11.1%) | 27 (15.2%) | 19 (22.1%) | 24 (19.8%) | 0.13 |
| Do’s and Don’ts | 36 (11.1%) | 8 (6.3%) | 20 (11.2%) | 10 (11.6%) | 20 (16.5%) | 0.16 | |
| Basic Precautions in hospital | 110 (33.8%) | 34 (27%) | 57 (32%) | 24 (27.9%) | 48 (39.7%) | 0.23 | |
| Prevent transmission for Personal safety | 133 (40.9%) | 50 (39.7%) | 88 (49.4%) | 23 (26.7%) | 48 (39.7%) | 0.13 | |
| Administrative Enquiries | Policies/protocols/guidelines | 6 (1.8%) | 4 (3.2%) | 12 (6.7%) | 4 (4.7%) | 2 (1.7%) | 0.03 |
| Knowledge about virus | 41 (12.6%) | 11 (18.7%) | 20 (11.2%) | 6 (7%) | 10 (8.3%) | 0.43 | |
| Managing exposure | 2 (0.6%) | 4 (3.2%) | 3 (1.7%) | 0 (0%) | 2 (1.7%) | 0.20 | |
| COVID-19 isolation area | 25 (7.7%) | 3 (2.4%) | 9 (5.1%) | 3 (3.5%) | 9 (7.4%) | 0.17 | |
| Inspire and train others | 16 (4.9%) | 5 (4%) | 4 (2.2%) | 2 (2.3%) | 4 (3.3%) | 0.57 | |
| Clinical skills | Symptoms of COVID-19 | 13 (4%) | 3 (2.4%) | 11 (6.2%) | 8 (9.3%) | 1 (0.8%) | 0.02 |
| CPR and Airway management | 17 (5.2%) | 8 (6.3%) | 9 (5.1%) | 2 (2.3%) | 4 (3.3%) | 0.63 | |
| Management and care of suspected/Infected COVID-19 patient | 27 (8.3%) | 19 (15.1%) | 15 (8.4%) | 5 (5.8%) | 5 (4.1%) | 0.02 | |
| Emergency and resuscitation | 6 (1.8%) | 4 (3.2%) | 4 (2.2%) | 1 (1.2%) | 4 (3.3%) | 0.77 | |
| Sample collection | Collection, handling and transport of samples | 15 (4.6%) | 7 (5.6%) | 10 (5.6%) | 7 (8.1%) | 1 (0.8%) | 0.31 |
∗: Analysis was performed using Chi-square test, p-values <0.05 was considered significant.
PPE: Personal Protective Equipment; CPR: Cardiopulmonary resuscitation.
Other expectations included, ‘how to take care of babies at home?’ (n = 4), ‘How to cope up with anxiety, stress and depression?’ (n = 2), ‘How to ensure proper nutrition?’ (n = 10) and ‘Various prophylactic drugs and other strategies, which can be used as preventive measure’ (n = 2).
Discussion
As correctly stated by an editorial in The Lancet, ‘Presently, health-care workers are every country’s most valuable resource’.3 Worldwide, people are directed to stay indoors to prevent transmission of COVID-19, while HCPs are called upfront. During this outbreak, HCPs from various specialities were called upfront to supplement the preventive, diagnostics or management of patients. These professionals were asked to deal the emergencies that were different from their expertise, and thus, unexpected and unforeseen by many. Thus, panic, depression, anxiety and confusion were to be expected, along with a lack of experience in many practices related to infection control.
Infection control should not be considered as a job of few assigned individuals; rather, it is an output of collective effort by every HCP. In an interview-based study by Ward et al,4 one can see how practices of nursing mentors mould the attitude of nursing students towards infection control, which might alter their knowledge and skills. Here in our study, we can see that HCPs from various backgrounds are having varied expectations from infection control training for the prevention of the spread of COVID-19.
Cleaning staff (n = 280) and nonmedical support staff (n = 188) had expectations of learning general enquiries, especially the basic precautions in healthcare setup and the precautions to prevent transmission of COVID-19 and personal safety (Table 1 and Fig. 2). On the other hand, fewer of them expected to learn about standard safety precautions (Cleaning support staff (n = 152) and nonmedical support staff (n = 128)). In standard precautionary measures, their concern was to learn hand hygiene. The doctors had more expectations to learn about standard precautions (n = 261) than general enquiries (n = 196). These expectations were similar among NO. Medical support staff had a greater number of expectations regarding standard precautions.
There is a risk for HCP to get infected by COVID-19 at HCO as shown by many reports.3,5, 6, 7, 8 A Chinese study also reports higher infection among HCPs working in low contagious healthcare settings.7 However, on the positive side, the infection control practices may prevent the transmission of COVID-19, as was seen in a case report, wherein HCP was exposed to an infected patient with severe pneumonia.9
Physical distancing, use of face mask and eye protection are some of the major preventive measures as explored by a systematic review.10 These act along with important standard precautions at HCO like hand hygiene, appropriate use of PPE, cleaning and disinfection and behavioural modifications to protect one from infection.11
In our study, medical (54%) and nonmedical (41.1%) support staffs were expecting to learn mainly about hand hygiene. This expectation was lower in doctors (26.7%), NO (25.6%) and cleaning staff (22.1%). The need to follow strict hand hygiene is essential in all areas of HCO, and it is good to see no significant difference in expectations to learn about hand hygiene from HCPs of different departments (Table 2). Hand hygiene is an integral aspect of patient care and it not only just protects HCP but also prevents the transmission of infection among patients. All the healthcare workers, thus, should be inspired to learn and practice hand hygiene, not just in the context of COVID-19 but as a part of good patient care practices.
Few participants expected to learn about the use of masks – Doctors (N = 7), NO (N = 7) and medical support staff (N = 13) (Table 1). More number of cleaning staff (N = 31) and nonmedical support staff (N = 42) showed interest in learning about masks (Table 1). There was a significant difference in expectations to learn about masks across various departments, with more interest among diagnostic and other academic departments, while medical, surgical and critical care areas showed lesser interest (Table 2). However, with the mask being one of the important aspects of protection from COVID-19 infection, with added confusion about which mask to use when and where, there needs to be more awareness and change in attitude towards the use of masks to protect oneself. It is essential that HCPs do not take the mask as just an accessory or a mandate but as a shield, and remember, it could be infected too, thus needing proper and timely disposal.10, 11, 12
Like masks, eye protection is equally important; although no HCP expected to learn about it, protecting the eye and face by using a face shield should be considered as a part of personal protection and needs urgent attention.
Physical distancing is another measure, which many participants expected to learn from the training. However, only 18 (7.1%) doctors expected to learn it. In some healthcare settings, it might not always be possible to maintain the suggested distance with patients; this is where the proper use of PPE may come in to play. One must remember, at time of outbreak, along with physical distancing from patients, it must also be observed among colleagues and co-workers. It is a simple measure that does not require any material means and thus, followed to the maximum possible extent.
PPE are important for protection in high-risk areas and procedures where there is aerosolisation of an infectious agent. There is a significant difference in expectation to learn the proper use of PPE across various departments and between participants of various designations. It was expected to be learned by participants working in critical care (47.2%) followed by surgical (45.2%), Medical (40.3%), diagnostic branches (38.4%) and other departments (20.7%). From this distribution, it appears that this expectation is majorly influenced by perceived use of PPE at their workstation, which is least expected in academic areas and maximum in critical care areas. However, few participants from these academic areas expected to be appointed in COVID19 isolation areas where they may need to use PPE, and thus, expected to learn its use. Fewer nonmedical support staff (9.9%) and cleaning staff (19.9%) expected to learn about PPE, irrespective of their workstation. These groups of HCPs need to be inspired about the importance and necessity of the proper use of PPE to prevent infection transmission.
Cleaning and disinfection are another major IPC measure, which takes special importance in an HCO. It should not be considered as a responsibility on one group of individual, rather a collaborative effort. Participants of various designations and department expected to learn about these, which shows their favourable interest and involvement in these practices.
There were many general enquiries pertaining do’s and don’ts, basic precautions, prevention of transmission and personal safety among all cadres of participants. Similarly, many also enquired about various administrative policies, protocols and work timing. The general nature of these expectations as compared to concern about learning specific infection control practices may highlight the participants’ interest but lack of awareness and knowledge.
It is interesting to see participants eager to know about the causative organism, modes of transmissions, clinical symptoms and management. These aspects may be considered in further training to inspire HCPs to follow better infection control practises and make them more vigilant for possible infection, to burst circulating myths about infection and treatments.
CPR is an aerosolising procedure and although lifesaving, its training puts HCP at increased risk of infection. Thus, American Heart Association updated its CPR guidelines based on the requirements raised by the COVID-19 outbreak.13 The definite need for CPR and resuscitation in the management of COVID-19 patients may have raised these expectations among the involved HCP i.e. doctors and NO.
Along with patient management, the other procedure that may be highly infectious is the collection and processing of samples for diagnostics. Few participants expected to learn about the procedure for sample collection and transport of COVID-19 samples, while only four participants expected to learn about other samples (i.e. blood) from an infected/suspected patient. The HCPs needs to be appraised that various samples from an infected/suspected patient may harbour the virus and thus, spread it to unaware individuals.
There was a significant difference in expectations from an infection control training of HCP, working at different levels of jobs (Table 1). However, this difference was minimal among HCPs working in different areas. While conducting infection control training, one must fulfil these expectations, and if not included in the training, the information may be made available on various platforms later. However, the training should also appraise and inculcate the important practices that might not be expected, and thus, bring about change in attitude, awareness, knowledge and practices of HCP.
Future perspectives
Training is an integral part of ICP. Targeted training addressing needs and expectations of HCP may improve the safety culture at HCO and result in quality improvements. However, these improvements must be assessed based on before and after training tests, as well as IPC quality assessment at various healthcare settings.
Limitation
In this study, we asked an open-ended question, which could be influenced by multiple factors. For getting an in-depth picture of these expectations, a structured interview should be conducted to explore what and why an HCP is expecting to learn from infection control training.
Disclosure of competing interest
The authors have none to declare.
Acknowledgements
We would like to be thankful to hospital infection control team for their invaluable support for conduct of this study.
References
- 1.Nasiri A., Balouchi A., Rezaie-Keikhaie K., Bouya S., Sheyback Mahmood, Rawajfah O.A. Knowledge, attitude, practice, and clinical recommendation toward infection control and prevention standards among nurses: a systematic review. Am J Infect Contr. 2019;47:827–833. doi: 10.1016/j.ajic.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 2.Stone P.W., Herzig C.T.A., Pogorzelska-Maziarz M. Understanding infection prevention and control in nursing homes: a qualitative study. Geriatr Nurs N Y N. 2015;36:267–272. doi: 10.1016/j.gerinurse.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Lancet COVID-19: protecting health-care workers. Lancet Lond Engl. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ward D.J. Attitudes towards infection prevention and control: an interview study with nursing students and nurse mentors. BMJ Qual Saf. 2012;21:301–306. doi: 10.1136/bmjqs-2011-000360. [DOI] [PubMed] [Google Scholar]
- 5.548 Doctors, Nurses, Paramedics Infected with Covid-19 across India: Report [Internet] Hindustan Times; 2020. https://www.hindustantimes.com/india-news/548-docs-nurses-paramedics-infected-with-covid-19-across-india-report/story-o2pM3w2adM4g3PXI6TBlkN.html [cited 2020 Jun 28]. Available from: [Google Scholar]
- 6.Barranco R., Ventura F. Covid-19 and infection in health-care workers: an emerging problem. Med Leg J. 2020 doi: 10.1177/0025817220923694. [DOI] [PubMed] [Google Scholar]
- 7.Lai X., Wang M., Qin C. Coronavirus disease 2019 (COVID-2019) infection among health care workers and implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.9666. e209666–e209666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wee L.E., Sim X.Y.J., Conceicao E.P. Containment of COVID-19 cases among healthcare workers: the role of surveillance, early detection, and outbreak management. Infect Control Hosp Epidemiol. 2020:1–7. doi: 10.1017/ice.2020.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ng K., Poon B.H., Kiat Puar T.H. COVID-19 and the risk to health care workers: a case report. Ann Intern Med. 2020;172:766–767. doi: 10.7326/L20-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet Lond Engl. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacIntyre C.R., Wang Q. Physical distancing, face masks, and eye protection for prevention of COVID-19. Lancet Lond Engl. 2020;395:1950–1951. doi: 10.1016/S0140-6736(20)31183-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Supehia S., Singh V., Sharma T., Khapre M., Gupta P.K. Rational use of face mask in a tertiary care hospital setting during COVID-19 pandemic: an observational study. Indian J Publ Health. 2020;64:S225–S227. doi: 10.4103/ijph.IJPH_493_20. [DOI] [PubMed] [Google Scholar]
- 13.Edelson Dana P., Comilla Sasson, Chan Paul S. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]