Abstract
Objective
This study aimed to compare the percutaneous oblique osteotomy (POO) and the open chevron osteotomy technique for correction of hallux valgus deformity at a 2‐year follow‐up.
Methods
This is a retrospective study of consecutive patients undergoing operative correction of hallux valgus using one of two techniques (POO vs open chevron osteotomy) from 2014 to 2018. Forty eight feet (41 patients) that underwent the POO was compared with 64 feet (58 patients) that underwent open chevron osteotomy. The hallux valgus angle (HVA), intermetatarsal angle (IMA) and American Orthopedic Foot & Ankle Society Hallux Metatarsophalangeal‐Interphalangeal scores (AOFAS‐HMI) were assessed preoperatively and postoperatively at the 1, 2‐year follow‐up. The Manchester–Oxford Foot Questionnaire (MOXFQ) were assessed preoperatively and postoperatively at the 2‐year follow‐up. The VAS score was collected preoperatively and on 2 weeks,1 year and 2‐year follow‐up.
Results
Both groups achieved significant correction of the hallux deformity. The HVA in the POO group during the follow‐up period were 12.5 ± 2.22 and 17.9 ± 9.31, respectively, and in the open chevron group were 14.1 ± 6.78 and 14.8 ± 7.83, respectively. The IMA in the POO group during the follow‐up period were 7.61 ± 1.63 and 6.94 ± 1.53, respectively, and in the open chevron group were 6.89 ± 3.06 and 6.97 ± 2.95, respectively. Postoperative MOXFQ scores in all domains were significantly improved in both groups, however there was no significant difference in the improvement of any domain between POO and open groups at a 2‐year follow‐up. The AOFAS HMI scores in the POO group during the follow‐up period were 86.5 ± 10.7 and 85.2 ± 13.8, respectively, and in the open chevron group were 88.2 ± 10.8 and 79.5 ± 23.7, respectively. The VAS scores in the POO group during the follow‐up period were 2.00 ± 0.98, 2.00 ± 0.99 and 1.55 ± 1.11, respectively, and in the open chevron group were 5.51 ± 1.45, 2.56 ± 2.88 and 2.56 ± 2.88 respectively. The 1‐year and 2‐year follow‐up outcomes between POO and open groups showed no significant difference regarding AOFAS HMI scores and VAS scores, however the POO group showed statistically significant improvement of VAS scores in the postoperative 2 weeks (P < 0.001). There was no statistical significance between the POO and open group in terms of complications rates (8.3% vs 12.5%, P = 0.480).
Conclusion
The POO technique is reliable and shows a comparable outcome to the open chevron osteotomy. However, the POO technique shows significantly less pain in the first 2 weeks after surgery.
Keywords: Akin, AOFAS scores, Chevron, Hallux valgus, MOXFQ scores, Percutaneous oblique osteotomy
We compare a percutaneous oblique osteotomy (POO) technique and the open chevron technique for correction of hallux valgus deformity at a 2‐year follow‐up. This POO technique is reliable and shows a comparable outcome to the open chevron technique. However, the POO technique had significantly less pain in the first 2 weeks following surgery.
Introduction
Percutaneous and minimally invasive surgery (MIS) for hallux valgus is increasingly common in orthopedics by reason of the inherent for smaller scars, lesser postoperative pain, rapid recovery, reduced rehabilitation times, and decreased risk of infection 1 , 2 . Initially, percutaneous hallux valgus technique was accomplished applying Isham, Bosch or Reverdin‐Isham procedures and modifications of these, which consist of arthroscopic assistant technique, the Endolog technique, extra‐articular reverse‐L Chevron (PERC) and percutaneous Chevron/Akin osteotomies 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 . The method of fixation is a critical aspect for the surgical correction of hallux valgus. First‐generation percutaneous technique was reported by Isham and no internal fixation after the osteotomy 3 . Later, the second generation of axial K‐wire fixation was carried out after the distal transverse osteotomy of the first metatarsal 10 , 11 . At present, screw fixation was carried out in order to enhance the stability 12 .
To date, many studies have evaluated the results of MIS techniques and open therapeutic surgeries for hallux valgus 9 , 13 , 14 , 15 . Meanwhile, systematic reviews have been reported to estimate the results of MIS techniques for treating the hallux valgus 1 , 16 . The excessive shortening of the first metatarsal and absence of intrinsic stability were complications in the percutaneous chevron osteotomy 12 . We use a percutaneous oblique osteotomy (POO) to avoiding excessive shortening of the first metatarsal and providing the intrinsic stability of the osteotomy as much as possible.
We have implemented the POO and adopted the screw fixation method. To accept a different operative technique, it is essential to see clinical outcomes and compare these with traditional techniques. The purpose of this study was to compare the radiographic correction, complication, postoperative pain levels and clinical outcomes between two groups of patients who accepted a POO technique and open distal chevron osteotomy at a 2‐year follow‐up. The hypothesis was that the POO technique shows significantly less pain, however, there would be no significant difference in both radiologic and clinical outcomes at follow‐up postoperatively.
Methods and Materials
Inclusion and Exclusion Criteria
Inclusion criteria for this study were: (i) older than 18 years with painful hallux valgus and failed conservative treatment; and (ii) hallux valgus correction underwent operative treatment via POO or open chevron osteotomy technique. The exclusion criteria for all these patients in our study were as follows: (i) patients had peripheral vascular disease, neuromuscular disease, rheumatoid arthritis; (ii) recurrent hallux valgus; and (iii) less than 2‐year follow‐up.
Patients
This retrospective cohort study was approved by institutional review board and consecutive patients from 2014 to 2018 were enrolled. We chose the POO as the study group and chevron open osteotomy as the control group and assessed 2‐year clinical and radiological results of both two groups.
We first enrolled 70 cases underwent open surgery and 60 cases for the MIS technique of hallux valgus. Patients with recurrent hallux valgus (three cases) and less than 2‐year follow‐up (15 cases) were excluded. Finally, 48 feet (41 patients) that underwent a percutaneous oblique osteotomy of hallux valgus and 64 feet (58 patients) that underwent open surgery were followed‐up for a 2‐year. There was no significant difference between the two groups in terms of sex, age, and BMI preoperatively (Table 1).
TABLE 1.
Patient demographics
| Demographics | MIS Group (n = 48) | Open Group (n = 64) | P |
|---|---|---|---|
| Sex, male/female | 3/45 | 3/61 | 0.72 |
| Age, mean ± SD, years | 60.9 ± 12.2 | 60.6 ± 9.69 | 0.87 |
| Body mass index, mean ± SD, kg/m2 | 22.5 ± 2.96 | 22.5 ± 2.32 | 0.99 |
Operative Technique
Percutaneous Oblique Osteotomy (POO)
The patient was operated on using regional anesthesia or general anesthesia without a tourniquet in a supine position.
A medial 5mm incision was used just proximal to the first metatarsal head, and the medial eminence was excised with a 1.5 × 20 mm burr and the bone debris was discharged (Fig. 1A). We always rinsed the incision and burr with ice sterile saline to prevent the burn complication during the osteotomy. The speed of the burr was not exceeding 3000 rpm to avoid thermal necrosis of the skin and bone.
Fig. 1.
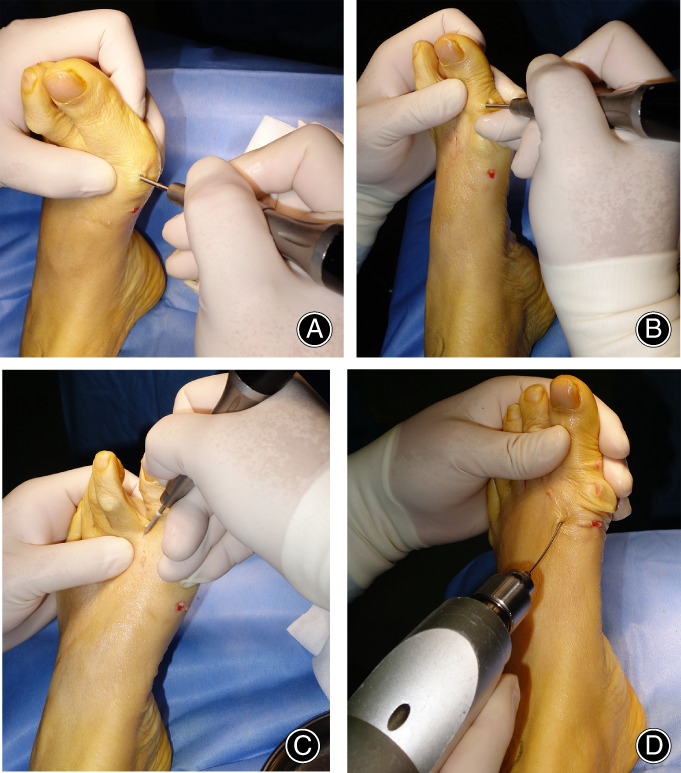
(A): The starting point of osteotomy and the direction of osteotomy was from the distal to the proximal; (B): An Akin osteotomy was undertaken through a dorsomedial approach using a 1.5 × 20 mm burr; (C): The distal second metatarsal osteotomy was performed with a 1.5 × 20 mm burr without screw fixation; (D): One or two the hollow nail guidewires were inserted through separate incisions to fix the osteotomy.
The starting point of osteotomy was at about 5 mm proximal to the first metatarsal head, an oblique osteotomy using a 2 × 20 mm burr was carried out, and the direction of osteotomy was from the distal to the proximal at about plantarization 45 degrees from the lateral view. The length of the osteotomy was longer than traditional percutaneous chevron osteotomy.
When the distal osteotomy was completely loosened, an assistant surgeon kept the first toe longitudinal traction to control the first metatarsal shortening as soon as possible. Meanwhile, the surgeon could manually control the rotation of the head of the metatarsal. One or two the hollow nail guidewires were inserted through separate incisions to fix the osteotomy (Fig. 1D), and the position was verified fluoroscopically and adjusted accordingly (Fig. 2A,B). After the position was satisfactory, one or two 2.5 mm‐diameter hollow headless nails (Wright, TN, USA) were selected for fixation (Fig. 2C,D).
Fig. 3.
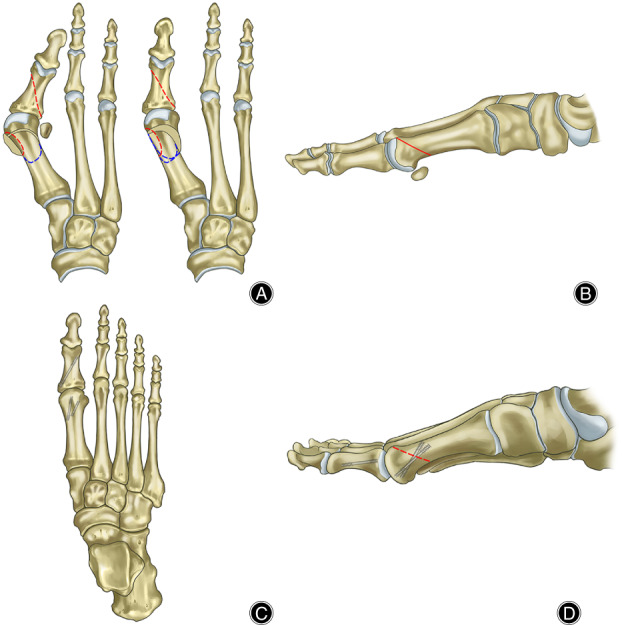
Schematic drawings of the POO osteotomy. (A) A‐P view: red line: the 1.5 × 20 mm burr; blue line: the 2 × 20 mm burr. When the distal osteotomy was completely and reduced the osteotomy manually. (B): From the lateral view, the direction of the osteotomy was about plantarization 45 degrees; (C) and (D): Two screws were used to fix the first metatarsal osteotomy and one screw for Akin osteotomy.
An Akin osteotomy was performed if there was residual hallux valgus after the first metatarsal osteotomy. This was undertaken through a dorsomedial approach, using a 1.5 × 20 mm burr (Fig. 1B), and one screw fixation after the akin osteotomy (Fig. 2C,D).
The osteotomy of the 2–5 metatarsals depends on the preoperative symptoms and the length of the 2–5 metatarsals after the first metatarsal osteotomy and fixation. The burr of these osteotomies is 1.5 × 20 mm, without screw fixation (Fig. 1C). The schematic procedures are shown in Fig. 3.
Fig. 2.
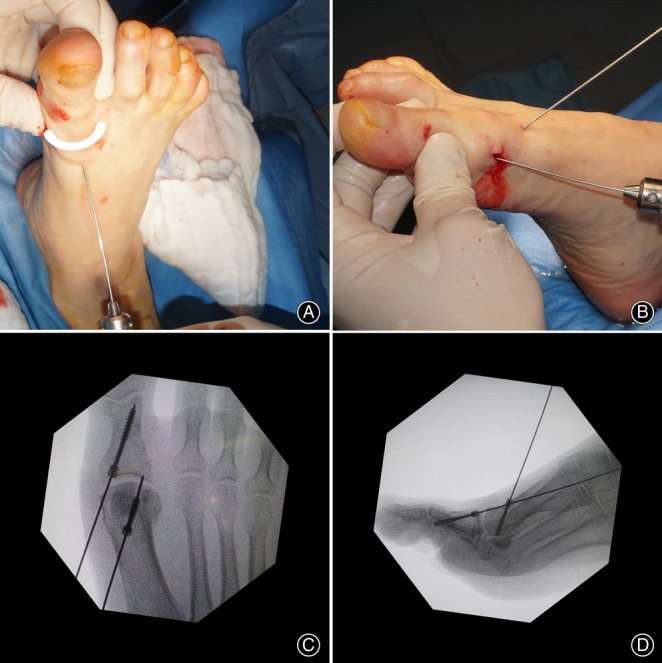
(A): Clinical photo showing the correction maneuver of the deformity (force applied as demonstrated with arrow). (B): Applying hollow nail guidewires for fixation of the fragment. Radiography showing placement of the screw percutaneously after osteotomy. (C): A‐P view; (D): lateral view.
Postoperatively, the hallux was mobilized in 8‐shaped bandage and the patients were allowed fully weightbearing immediately in a hard‐bottom shoe (Darco, TN, USA) without the aid of crutches. Patients were encouraged to elevate the foot in the first 2 weeks after surgery to reduce the swelling. The shoe was removed after 6 weeks and patients were encouraged to wear a pair of sneakers.
Open Chevron Osteotomy
The patient was performed using general anesthesia using a tourniquet in a supine position. The distal Chevron osteotomy was performed through the 4‐cm dorsomedial incision. When the medial eminence was resected, a V‐shaped osteotomy was performed. The apex of the chevron was positioned at the center of the first metatarsal head, and the angle of the chevron was 60 degrees. The distal osteotomy fragment was shifted laterally at a maximal half of the diameter of the first metatarsal due to the angle of the hallux valgus. Fixation was achieved with one or two cannulated screws (3.2 mm, Wright, USA). An Akin osteotomy was performed if there was residual hallux valgus after the first metatarsal osteotomy. The osteotomy of the 2–3 metatarsals depends on the preoperative symptoms and Weil osteotomy was performed using the breaking screws (Wright, USA). The hallux was mobilized immediately in 8‐shaped bandage immediately and the patients were mobilized in a forefoot decompression shoe (Darco, USA). The shoe was removed after 6 weeks and patients were encouraged to full weightbearing.
Evaluation Methods
Radiographic Measurements
Weightbearing anteroposterior (AP) and lateral radiographs of the foot were collected for all patients to evaluate the severity of the deformity. The hallux valgus angle (HVA) and intermetatarsal angle (IMA) were assessed as the radiological parameters preoperatively and postoperatively at the 1‐, 2‐year follow‐up. The HVA was measured through the anteroposterior view as the angle between the long axis of the first metatarsal and the long axis of the proximal phalanx. The IMA was measured between the long axis of the first metatarsal and long axis of the second metatarsal. The relationship among the IMA and HVA values was classified into three groups according to the presence of Mann and Coughlin parameters: (i) mild HV was defined as an IMA ≤11° and HVA <20°; (ii) moderate HV was an IMA >11 but <16° and HVA of 20° to 40°; and (iii) severe HV was an IMA ≥16° and HVA of >40°.
MOXFQ Scores
Clinical outcomes were measured by Manchester–Oxford Foot Questionnaire (MOXFQ) preoperatively and postoperatively at the 1, 2‐year follow‐up 17 . The MOXFQ included three domains: walking/standing score, pain score, and a social interaction score. Response options consist of a 5‐point scale ranging from no limitation to maximal limitation. An individual score was used for each domain and converted into a metric score 0 to 100, where 100 is the most severe.
AOFAS HMI Scores
Clinical outcomes were measured by American Orthopedic Foot & Ankle Society Hallux Metatarsophalangeal‐Interphalangeal (AOFAS HMI) score preoperatively and postoperatively at the 1, 2‐year follow‐up. The AOFAS HMI score consists of subjective and objective variables classified into three major categories: pain, function, and alignment. The scores were divided into categories as follows: a score of 90 to 100 was graded as excellent; 75 to 89, as good; 50 to 74, as fair; and less than 50 points, as poor.
VAS Scores
The VAS scores were collected preoperatively and on 2 weeks,1 year and 2‐year follow‐up postoperatively. The visual analogue scale (VAS) is an instrument used to quantify the intensity of pain. A commonly used VAS is a 10cm line labeled with “worst pain imaginable” on the right border and “no pain” on the left border. The patient is instructed to make a mark along the line to represent the intensity of pain currently being experienced. The clinician records the distance of the mark in centimeters from the left end of the scale. The range of the VAS score was from 0 to 10.
Complications
All the clinical complications including wound problem, numbness, nonunion, stiffness of the first MTPJ and revision were collected at the 2‐year follow‐up.
Statistical Analysis
Power analysis was carried out to guarantee that the study sample size was adequate. The sample size was based on acquiring a 90% power with an alpha level risk of 5%. All the continuous variables are described as means ± standard deviations. Mann–Whitney U test or Student t test was used for continuous variables, depending on the data distribution. The Matched‐pairs t test was used to analyze any significant difference between the preoperative and postoperative clinical outcomes. Fisher exact test was performed for the categorical variables. For angular values not normally distributed, we used the Wilcoxon test of signed ranks. The alpha level was set at less than 0.05. Statistical analyses were using Stata statistical software (version 15, StataCorp, College Station, TX).
Results
Surgical Outcomes
Fifty required Akin osteotomy (35 in open group and 15 in POO group) and 39 required a Weil osteotomy (23 in open group and 16 in POO group). POO group achieved significant correction of the hallux deformity (Figs 4 and 5).
Fig. 4.
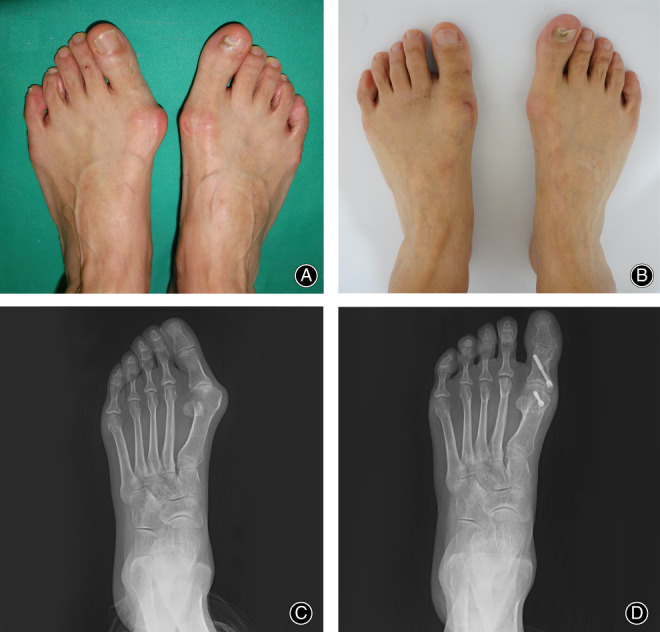
Clinical and radiographic view of a 60‐year‐old female with a left hallux valgus. Preoperative clinical photo: preoperative (A) and postoperative 24 months follow‐up (B); radiographic X‐ray: preoperative (C) and postoperative 24 months follow‐up (D).
Fig. 5.

Clinical and radiographic view of a 44‐year‐old female with a right hallux valgus. Preoperative clinical photo (A) and radiographic X‐ray (B). (C): The fluoroscopy shows that two screws are used to fix the first metatarsal osteotomy and the second metatarsal osteotomy has no fixation. (D): The photo of the clinical incision during the operation. Postoperative clinical photo (E) and radiographic X‐ray (F) at 24 months follow‐up.
Radiographic Outcomes
According to the Mann and Coughlin grading system, 26 patients (21 in open group and 15 in POO group) were classified in mild HV, 73 patients (44 in open group and 29 in POO group) in moderate HV and 13 patients (9 in open group and 4 in POO group) in severe HV.
Compared with preoperative radiographic outcomes, both groups demonstrated significant differences in the HVA and IMA at the final follow‐up (P < 0.05). When comparing groups, both HVA and IMA demonstrated similar results at a 1‐year and 2‐year follow‐up respectively (Fig. 6). Table 2 summarizes the radiographic outcomes.
Fig. 6.
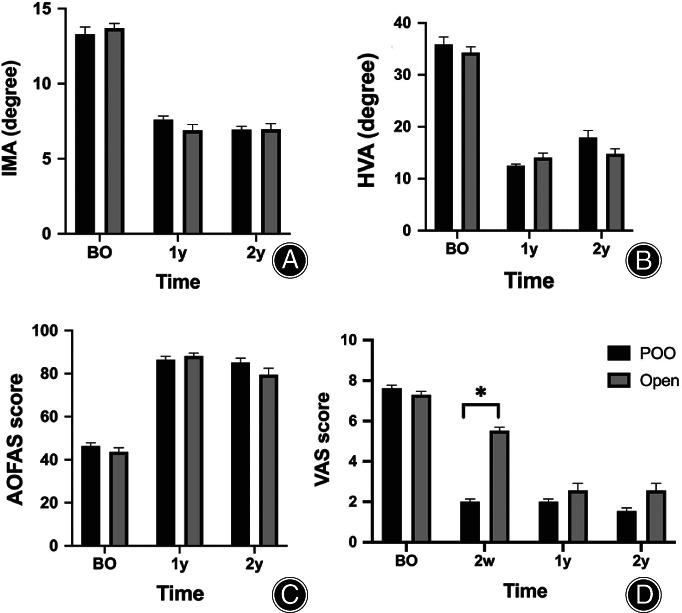
(A) Comparison of IMA between the two groups preoperatively (P = 0.46) and at 1 (P = 0.14), 2 (P = 0.95) years of follow‐up. (B) Comparison of HVA between the two groups preoperatively (P = 0.38) and at 1 (P = 0.12), 2 (P = 0.06) years of follow‐up. (C) Comparison of AOFAS between the two groups preoperatively (P = 0.64) and at 1 (P = 0.40), 2 (P = 0.66) years of follow‐up. (D) Comparison of VAS between the two groups preoperatively (P = 0.07) and at 2 weeks (P = 0.00), 1 (P = 0.53), 2 (P = 0.37) years of follow‐up. AOFAS, American Orthopedic Foot & Ankle Society Hallux Metatarsophalangeal‐Interphalangeal score; BO, before operation; VA, hallux valgus angle; IMA, intermetatarsal angle.
TABLE 2.
Summary of clinical outcome and radiological outcome
| POO group (n = 48) | Open group (n = 64) | P | |
|---|---|---|---|
| Clinical outcomes | |||
| MOXFQ scores | |||
| Walking | |||
| Preoperative | 50.3 ± 8.59 | 49.8 ± 10.4 | 0.24 |
| Postoperative 2 years | 13.5 ± 7.83 | 15.2 ± 8.08 | 0.23 |
| Pain | |||
| Preoperative | 51.6 ± 9.87 | 49.8 ± 10.4 | 0.16 |
| Postoperative 2 years | 15.8 ± 13.3 | 22.7 ± 17.3 | 0.06 |
| Social interaction | |||
| Preoperative | 56.9 ± 10.7 | 58.6 ± 9.22 | 0.41 |
| Postoperative 2 years | 13.3 ± 10.9 | 17.6 ± 16.8 | 0.40 |
| AOFAS score | |||
| Preoperative | 46.4 ± 10.1 | 43.7 ± 15.1 | 0.64 |
| Postoperative 1 year | 86.5 ± 10.7 | 88.2 ± 10.8 | 0.40 |
| Postoperative 2 years | 85.2 ± 13.8 | 79.5 ± 23.7 | 0.66 |
| VAS | |||
| Preoperative | 7.63 ± 1.06 | 7.29 ± 1.42 | 0.07 |
| Postoperative 2 weeks | 2.00 ± 0.98 | 5.51 ± 1.45 | 0.00 |
| Postoperative 1 year | 2.00 ± 0.99 | 2.56 ± 2.88 | 0.53 |
| Postoperative 2 years | 1.55 ± 1.11 | 2.56 ± 2.88 | 0.37 |
| Radiologic outcomes | |||
| HVA | |||
| Preoperative | 35.9 ± 10.0 | 34.3 ± 8.85 | 0.38 |
| Postoperative 1 year | 12.5 ± 2.22 | 14.1 ± 6.78 | 0.12 |
| Postoperative 2 years | 17.9 ± 9.31 | 14.8 ± 7.83 | 0.06 |
| IMA | |||
| Preoperative | 13.2 ± 3.31 | 13.7 ± 2.53 | 0.46 |
| Postoperative 1 year | 7.61 ± 1.63 | 6.89 ± 3.06 | 0.14 |
| Postoperative 2 years | 6.94 ± 1.53 | 6.97 ± 2.95 | 0.95 |
MOXFQ scores
The MOXFQ scores are summarized in Table 2. Preoperative scores showed similarly in all the domains. Postoperative scores in all domains were significantly improved in both groups, however there was no significant difference in the improvement of any domain between POO and open groups (Fig. 6). In the POO group, the walking score improved from 50.3 to 13.5 (P < 0.001), the pain score from 51.6 to 15.8 (P < 0.001), and the social interaction score from 56.9 to 13.3 (P < 0.001) at the 2‐year follow‐up. In the open group, the walking score improved from 49.8 to 15.2 (P < 0.001), the pain score from 49.8 to 22.7 (P < 0.001), and the social interaction score from 58.6 to 17.6 (P < 0.001) at the 2‐year follow‐up.
AOFAS HMI and VAS scores
The AOFAS HMI and VAS scores improved significantly in both groups postoperatively (P < 0.001). The 1‐year and 2‐year follow‐up outcomes between POO and open groups were no significant difference regarding AOFAS HMI scores and VAS scores, however the POO group showed statistically significant improvement of VAS scores in the postoperative 2 weeks (Fig. 6).
Clinical outcomes of different classifications of the deformity
The 2‐year follow‐up of clinical outcomes of different classifications of the deformity were showed in Table 3. The 2‐year follow‐up clinical outcomes between POO and open groups with different classifications of the deformity showed no significant difference regarding MOXFQ scores, AOFAS HMI scores and VAS scores.
TABLE 3.
2‐year follow‐up of clinical outcomes of different classifications of the deformity
| POO group | Open group | P | |
|---|---|---|---|
| Mild HV | |||
| MOXFQ scores | |||
| Walking | 14.1 ± 10.3 | 13.9 ± 11.1 | 0.61 |
| Pain | 13.3 ± 10.8 | 24.1 ± 21.3 | 0.23 |
| Social interaction | 12.9 ± 6.5 | 20.5 ± 22.4 | 0.74 |
| AOFAS score | 86.8 ± 9.2 | 85.1 ± 19.8 | 0.59 |
| VAS | 1.9 ± 1.1 | 2.5 ± 2.9 | 0.97 |
| Moderate HV | |||
| MOXFQ scores | |||
| Walking | 13.7 ± 6.8 | 16.1 ± 7.1 | 0.57 |
| Pain | 18.3 ± 14.8 | 24.2 ± 16.6 | 0.51 |
| Social interaction | 14.4 ± 12.9 | 18.9 ± 16.2 | 0.21 |
| AOFAS score | 83.5 ± 16.0 | 77.7 ± 24.7 | 0.64 |
| VAS | 1.4 ± 1.1 | 2.9 ± 3.0 | 0.15 |
| Sever HV | |||
| MOXFQ scores | |||
| Walking | 10.7 ± 2.9 | 12.7 ± 8.6 | 0.10 |
| Pain | 7.5 ± 2.9 | 13.9 ± 13.9 | 0.52 |
| Social interaction | 6.3 ± 5.1 | 7.6 ± 7.5 | 0.57 |
| AOFAS score | 91.3 ± 10.3 | 81.7 ± 24.7 | 0.18 |
| VAS | 1 ± 1.2 | 1.1 ± 1.3 | 0.97 |
Complications
In the POO group, there was one screw irritation, one revision, one patient with paresthesia of the medial of first metatarsal and one stiffness of the first MTPJ. The patient had the screw irritation after the surgery and the screws were removed 3 months later. The patient underwent a revision surgery at the postoperative sixth day due to screws displacement after the initial weight‐bearing postoperative first day. In the open group, there was one wound problem, two screw irritations, two cases of second metatarsalgia, one paresthesia of the medial of first metatarsal, and two stiffness of the first MTPJ. There was no avascular necrosis, nonunion, hallux varus or recurrence. There was no statistical significance between the POO and open group in terms of complication rates (8.3% vs 12.5%, P = 0.48).
Discussion
This study retrospectively compared the outcomes between the open chevron osteotomy and the POO technique at a 2‐year follow‐up. The POO technique is a percutaneous oblique osteotomy of hallux valgus correction in which it uses the stable screws internal fixation. This study showed comparable radiological results, clinical results, and the rates of complications between the two groups at a 2‐year follow‐up. However, during the early postoperative 2 weeks stage, the POO group showed a statistically significant improvement of pain level.
Previous Studies Involving Percutaneous Hallux Valgus Surgery
Traditional open hallux valgus surgery needs broad operation, which may bring joint stiffness, would pain, swelling and even the wound complications. Surgeons carrying out a minimally invasive surgery approach. The first‐generation percutaneous technique was reported by Stephen Isham, and the second generation was the Bosch osteotomy 3 , 18 . First and second generation of MIS techniques have comprised first metatarsal osteotomies with either no fixation or K‐wire fixation. Both the average of HVA and IMA correction for mild, moderate, and severe hallux valgus have been shown improved from preoperatively to postoperatively 1 . The main drawback of the first and second generation of MIS techniques is the deficiency of stable fixation. Third generation of MIS techniques used the headless compression screws to achieve more stable internal fixation 15 .
Third generation of MIS techniques were reported in some literatures. Jowett et al. 13 reported a prospective study of 78 patients with a mean follow‐up of 25 months. The AOFAS score and the radiographic parameters (HVA and IMA) had improved significantly. Lee et al. 19 reported a prospective randomized study of 25 percutaneous Chevron/akin (PECA) vs 25 open technique cases with 6 months follow‐up. They reported that both groups demonstrated comparable good to excellent clinical and radiologic results at 6 months follow‐up. However, the PECA technique showed less pain in the first 6 weeks after surgery. Brogan et al. 10 reported a retrospective cohort study of 81 cases (49 MIS and 32 open distal chevron osteotomies) with a minimum 24 months follow‐up and reported that both groups showed comparable clinical and radiological results of hallux valgus. Lucas y Hernandez et al. 9 reported that 53 cases of hallux valgus correction using the percutaneous extra‐articular reverse‐L Chevron (PERC) technique with a mean follow‐up of 60 months showed a main improvement of good first MTPJ range of motion underwent this technique. Vernois and Redfern et al. 15 reported a case series of 341 patients with a minimum 12 months follow‐up and reported HVA and IMA had improved significantly, and the excellent or good satisfaction rates were 95%.
Technical Points
Our technique has some differences from previously reported literature. First, the main problem associated with chevron osteotomy is excessive shortening of the first metatarsal, owing to the thickness of the burr. In addition, if the cuts are short, the intrinsic stability of the osteotomy is absent 12 . We use an oblique metatarsal osteotomy, which is different from transverse metatarsal osteotomy and chevron osteotomy. An oblique metatarsal osteotomy could avoid the excessive shortening of the first metatarsal and provide the intrinsic stability of the osteotomy as much as possible. We can both rotate the distal osteotomy block and correct distal metatarsal articular angle (DMAA) simultaneously after osteotomy. DMAA has not been measured in our cases, because there is poor interobserver reliability and is not frequently used in research due to this reason 1 , 20 . Second, we use one or two 2.5 mm‐diameter headless hollow screws to fix the osteotomy to provide the stability and allow fully weight‐bearing immediately after surgery in a hard bottom shoe without the aid of crutches. The first MTPJ can be exercised to avoid joint stiffness due to the immediate weight‐bearing after operation. Third, we perform the osteotomy of the 2–5 metatarsals depending on the preoperative symptoms and the length of the 2–5 metatarsals after the first metatarsal osteotomy. Our theory is that the position of 2–5 metatarsals after the osteotomy using 1.5 mm‐diameter burr without fixation can be adjusted automatically after the weight‐bearing.
Complications
Because of high rate of major complications, a previous prospective study evaluating percutaneous hallux valgus surgery was abandoned after 3 months during early follow‐up 21 . The burn wound complications varied from 0% to 13% in beginners during the learning curve of the MIS technique. In our cases, we rinsed the incision and burr with ice sterile saline and low‐speed burr to reduce the risk of thermal damage. Consequently, no burn complication was recorded. The rates of the complications were diverse widely even within the same technique. During the third‐generation techniques, the rate of complication also varied from 24% or 15.5% or 14% or 10% or 2% 9 , 13 , 14 , 15 , 19 . There was no statistical significance of complication rates between the two groups in our study.
Limitations
There are several limitations to this study. First, a relatively small number of participants in a limited period are enrolled. It is important to recognize the long‐term clinical outcomes of a new technique, and it is apparently true that the absolute benefits of MIS are in the early postoperative period and long‐term data collection, including recurrence and patient satisfaction, will be evaluated in the future studies. Second, this is a retrospective study and not a prospective randomized study. Lastly, the open chevron technique as the control group was only one of the traditional techniques among many techniques.
Conclusion
The present study objectively describes comparable clinical outcomes and radiographic outcomes of the POO technique by a known traditional open chevron technique. However, the POO technique had significantly less pain in the first postoperative 2 weeks.
Authorship Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and that all authors agree with the manuscript.
Acknowledgments
This study was supported in part by a research grants from National Natural Science Foundation of China grants (No. 81772372).
Disclosure: The authors have no conflict of interest.
References
- 1. Bia A, Guerra‐Pinto F, Pereira BS, Corte‐Real N, Oliva XM. Percutaneous osteotomies in hallux valgus: a systematic review. J Foot Ankle Surg, 2018, 57: 123–130. [DOI] [PubMed] [Google Scholar]
- 2. Kaufmann G, Dammerer D, Heyenbrock F, Braito M, Moertlbauer L, Liebensteiner M. Minimally invasive versus open chevron osteotomy for hallux valgus correction: a randomized controlled trial. Int Orthop, 2019, 43: 343–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Isham SA. The Reverdin‐Isham procedure for the correction of hallux abducto valgus. A distal metatarsal osteotomy procedure. Clin Podiatr Med Surg, 1991, 8: 81–94. [PubMed] [Google Scholar]
- 4. Bosch P, Wanke S, Legenstein R. Hallux valgus correction by the method of Bosch: a new technique with a seven‐to‐ten‐year follow‐up. Foot Ankle Clin, 2000, 5: 485–498. [PubMed] [Google Scholar]
- 5. Maffulli N, Longo UG, Oliva F, Denaro V, Coppola C. Bosch osteotomy and scarf osteotomy for hallux valgus correction. Orthop Clin North Am, 2009, 40: 515–524. [DOI] [PubMed] [Google Scholar]
- 6. Bauer T, Biau D, Lortat‐Jacob A, Hardy P. Percutaneous hallux valgus correction using the Reverdin‐Isham osteotomy. Orthop Traumatol Surg Res, 2010, 96: 407–416. [DOI] [PubMed] [Google Scholar]
- 7. Lui TH, Chan KB, Chow HT, Ma CM, Chan PK, Ngai WK. Arthroscopy‐assisted correction of hallux valgus deformity. Arthroscopy, 2008, 24: 875–880. [DOI] [PubMed] [Google Scholar]
- 8. Di Giorgio L, Touloupakis G, Simone S, Imparato L, Sodano L, Villani C. The Endolog system for moderate‐to‐severe hallux valgus. J Orthop Surg (Hong Kong), 2013, 21: 47–50. [DOI] [PubMed] [Google Scholar]
- 9. Lucas y Hernandez J, Golano P, Roshan‐Zamir S, Darcel V, Chauveaux D, Laffenetre O. Treatment of moderate hallux valgus by percutaneous, extra‐articular reverse‐L Chevron (PERC) osteotomy. Bone Joint J, 2016, 98: 365–373. [DOI] [PubMed] [Google Scholar]
- 10. Brogan K, Lindisfarne E, Akehurst H, Farook U, Shrier W, Palmer S. Minimally invasive and open distal chevron osteotomy for mild to moderate hallux valgus. Foot Ankle Int, 2016, 37: 1197–1204. [DOI] [PubMed] [Google Scholar]
- 11. Magnan B, Pezze L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. J Bone Joint Surg Am, 2005, 87: 1191–1199. [DOI] [PubMed] [Google Scholar]
- 12. Brogan K, Voller T, Gee C, Borbely T, Palmer S. Third‐generation minimally invasive correction of hallux valgus: technique and early outcomes. Int Orthop, 2014, 38: 2115–2121. [DOI] [PubMed] [Google Scholar]
- 13. Jowett CRJ, Bedi HS. Preliminary results and learning curve of the minimally invasive chevron akin operation for hallux valgus. J Foot Ankle Surg, 2017, 56: 445–452. [DOI] [PubMed] [Google Scholar]
- 14. Holme TJ, Sivaloganathan SS, Patel B, Kunasingam K. Third‐generation minimally invasive chevron akin osteotomy for hallux valgus. Foot Ankle Int, 2020, 41: 50–56. [DOI] [PubMed] [Google Scholar]
- 15. Vernois J, Redfern D. Percutaneous Chevron; the union of classic stable fixed approach and percutaneous technique. Fuß Sprunggelenk, 2013, 11: 70–75. [Google Scholar]
- 16. Malagelada F, Sahirad C, Dalmau‐Pastor M, et al. Minimally invasive surgery for hallux valgus: a systematic review of current surgical techniques. Int Orthop, 2019, 43: 625–637. [DOI] [PubMed] [Google Scholar]
- 17. Dawson J, Boller I, Doll H, et al. Responsiveness of the Manchester‐Oxford Foot Questionnaire (MOXFQ) compared with AOFAS, SF‐36 and EQ‐5D assessments following foot or ankle surgery. J Bone Joint Surg Br, 2012, 94: 215–221. [DOI] [PubMed] [Google Scholar]
- 18. Portaluri M. Hallux valgus correction by the method of Bosch: a clinical evaluation. Foot Ankle Clin, 2000, 5: 499–511. [PubMed] [Google Scholar]
- 19. Lee M, Walsh J, Smith MM, Ling J, Wines A, Lam P. Hallux valgus correction comparing percutaneous chevron/akin (PECA) and open scarf/akin osteotomies. Foot Ankle Int, 2017, 38: 838–846. [DOI] [PubMed] [Google Scholar]
- 20. Chi TD, Davitt J, Younger A, Holt S, Sangeorzan BJ. Intra‐ and inter‐observer reliability of the distal metatarsal articular angle in adult hallux valgus. Foot Ankle Int, 2002, 23: 722–726. [DOI] [PubMed] [Google Scholar]
- 21. Kadakia AR, Smerek JP, Myerson MS. Radiographic results after percutaneous distal metatarsal osteotomy for correction of hallux valgus deformity. Foot Ankle Int, 2007, 28: 355–360. [DOI] [PubMed] [Google Scholar]


