Abstract
Background:
Brief contact interventions such as telephone-based contacts appear to be useful in individuals who attempted suicide. Most studies of telephone-based contacts in such individuals typically consisted of frequent phone reminders for adherence to treatment and seeking help for mental health issues. Telephone-based psychosocial interventions that incorporate elements of supportive and problem-solving strategies are of interest in Indian settings due to their potential application in mitigating the wide mental health gap. Feasibility studies of telephone-based psychosocial interventions could help ascertain the difficulties that arise in the implementation of such treatments.
Methods:
A multicentric randomized controlled trial (RCT) is currently underway in general hospital settings in two Indian cities to study the efficacy of telephone-based psychosocial interventions in individuals with a recent suicide attempt, with routine telephone contacts (TCs) serving as the comparator. Prior to that RCT, this feasibility study was conducted to assess the acceptability of the telephone-based intervention and telephone contacts. Feasibility was assessed using dropout rates. Acceptability was assessed using participant-rated Likert-based visual analog scores from 0 to 10, with higher scores indicating greater acceptability.
Results:
Dropout rates and mean acceptability scores for telephone-based psychosocial interventions were 38.5% and 8.63, while those for TCs were 41.7% and 7.57, respectively.
Conclusions:
Telephone-based psychosocial interventions are feasible and acceptable in individuals with a recent suicide attempt.
Keywords: Suicide attempt, telephone interventions, brief contact, psychosocial, suicide
Key Messages:
Telephone-based psychosocial interventions are feasible and acceptable to implement in general hospital settings in individuals with a recent suicide attempt. Telephone-based psychosocial interventions can be evaluated for their role as additional interventions, along with treatment as usual, in individuals at risk of suicide.
Individuals who attempt suicide do not always seek help from mental health services.1 Their reasons include a perceived lack of need for mental health care, fear of hospitalization, financial difficulties, and stigma.1,2 These low rates of utilization of mental health service raise concerns due to increased future risk of repeat attempts and death due to suicide.3
Depression and anxiety are the leading causes of suicide-related burden worldwide.4 In India, mental illnesses and psychosocial stressors have been associated with suicide attempts.5 Reviews of studies on suicide prevention and treatment have emphasized the need for biopsychosocial interventions.6 Individuals with suicidal behaviors are, however, often difficult to engage in treatment.7 Psychological interventions that emphasize early and sustained engagement could reduce rates of suicidal behavior.8
Brief contact interventions that involve regular, short duration, structured contact through telephone calls, short message services, or postcards have shown promise in reducing suicide attempts.9 Telephone contacts (TCs) have functioned as reminders to seek help for mental health issues and have not explicitly delivered psychosocial interventions.10 Individuals with recent self-harm attempts have found contact interventions like telephone calls to be “gestures of caring,” indicating the usefulness of such strategies.11 Telephone-based counseling has also shown utility in conditions like alcohol use disorders that increase the risk of suicide attempts.12
Although the research from India strongly supports the role of brief telephone contact reminders in preventing suicides, there is inadequate evidence on the role of longer, telephone-based psychosocial interventions.10 Feasibility trials—by serving as preliminary evaluations of such telephone interventions—could provide the necessary corroboration. Feasibility trials are conducted prior to main studies and help shed light on the difficulties that could occur during the conduct of those studies and the consequent implementation issues in real-world settings.13 Most feasibility interventional trials achieve this by using outcome measures like participant reported acceptability and dropout rates.13
In this background, we report findings from a randomized controlled trial (RCT) that evaluated the feasibility and acceptability of telephone-based psychosocial interventions, along with short-duration TCs as the comparator, in individuals with recent suicide attempts. This feasibility trial was performed prior to the conduct of an ongoing RCT that compares the efficacy of telephone-based psychosocial interventions with routine telephone reminders in individuals with a recent suicide attempt. For the purpose of this study, telephone interventions and comparator were not the primary interventions and only supplemented treatment-as-usual.
Material and Methods
Objective: To assess the feasibility and acceptability of telephone-based psychosocial intervention (TBPI) in comparison with routine TCs in individuals with a recent suicide attempt, prior to the conduct of an ongoing RCT that is studying the efficacy of these on suicidal behaviors. We used a randomized controlled design for feasibility trials, according to CONSORT guidelines extension to pilot and feasibility trials.14 TBPI and TC were intended to be additional interventions and did not substitute the prescribed mental health treatments (pharmacotherapy and/or psychotherapy) as usual for the participants.
Rationale for this feasibility study: There is a paucity of evidence on the efficacy of telephone and other mobile-based counseling and psychosocial interventions in mental health and suicide prevention in India.15 Hence, this study was designed as part of a capacity-building exercise in implementation research under the National Mental Health Program.16
We deliberately avoided using treatment as usual as a comparator group in view of already existing evidence supporting TC and the associated ethical issues in denying any form of telephone communications to study participants.10 The comparison would also provide information about the nature of telephone communication that would be acceptable.
In this context, this feasibility trial was conducted prior to and independently as part of the preparation for a larger RCT that aimed to compare the efficacy of telephone-based psychosocial interventions with TCs on suicidal ideation in individuals with a history of a suicide attempt. That RCT is expected to be completed by September 2021. We received approval from ethics review boards of St John’s Medical college hospital, Bengaluru, and Atal Bihari Vajpayee Institute of Medical Science & Dr R M L Hospital, New Delhi. We conducted the study in accordance with the declaration of Helsinki. The study is being funded by the Indian Council of Medical Research (ICMR) as part of Capacity Building Projects for Implementation Research under NMHP.
At least 12 participants were aimed to be recruited per arm at the initial stage, in line with the existing recommendations for feasibility studies.17 This feasibility study was conducted over a period of 3–5 months from November 2018 till March 2019.
Participants’ Eligibility Criteria
Participants were individuals with a recent suicide attempt in the last one month at the time of screening. Participants speaking Hindi or English were included in New Delhi, while participants speaking Kannada, Hindi, Telugu, Tamil, or English were included in Bangalore. We included those between the ages of 18–55 years and of both genders. We deliberately aimed to include most individuals with recent suicide attempt as this would render greater applicability of the intervention. We excluded those with active psychotic illness, as these individuals may not be appropriate for our interventions and would also require specific pharmacological interventions along with intensive psychoeducation. Persons with a history of substance abuse as per Mini International Neuropsychiatric Interview (M.I.N.I) version 6.0 were excluded, as these individuals would require specific psychological interventions targeting motivation enhancement and relapse prevention. Persons with unstable medical illnesses were also excluded as they would require more intensive individualized medical and mental health treatments, preventing baseline assessment. Persons with cognitive impairment, either pre-existing or after the suicide attempt, were also excluded as they would require specialized and individualized interventions.
Study Settings
This study was conducted in two general hospitals in the metropolises of Bangalore and New Delhi in India. Research fellows identified and recruited participants using hospital registers in outpatient and inpatient psychiatry departments and internal medicine specialty settings. We also recruited from emergency referrals. Participants were recruited from all settings in order to increase the application potential of the intervention. At both sites, research fellows consulted treating medical and mental health teams about participants’ medical condition and psychiatric disorders. Research fellows obtained written informed consent from all participants who met inclusion criteria.
Training of Study Personnel
STS, VSSV, VG, and NK with a postgraduate degree in psychology were trained to assess participants and deliver TBPI and TC at each site. As part of their training, the research fellows first observed mental health specialists assessing and treating individuals with suicide attempts. RPB and PS who are experienced specialist mental health professionals then trained the research fellows in using recreations of clinical scenarios. The research fellows eventually evaluated participants and delivered TBPI and TC under constant supervision during the course of this feasibility study. Their phone communications were audio-recorded in those instances where the participants provided consent for the recording and were assessed for the fidelity of TBPI and TC using a structured checklist.
Overview of TBPI and TC
We intended to deliver a total of three sessions of TBPI and TC, one session each at weekly intervals, over a month. After written informed consent, a research fellow would obtain a participant’s sociodemographic details and events leading to a suicide attempt, including associated psychosocial stressors. The participant’s psychiatric diagnosis was recorded on the basis of the clinical impression of the treating mental health team, according to ICD-10 diagnostic criteria.
After this evaluation, a different research fellow would deliver a standard baseline psychological intervention to all participants. This intervention consisted of information on the risk of repeat suicide attempts, the need for treatment adherence, and help-seeking avenues, similar to the large WHO multicenter trial.10 This intervention would also contain suggestions and discussion of specific types of individualized problem solving strategies derived from dialectical behavior therapy worksheets.18 We developed a menu of such strategies from which participants would be provided appropriate strategies in accordance with their socioeconomic status and cultural belief systems.
The strategies were developed after an extensive literature review and expert discussions. A literature review showed that in India, a significant proportion of individuals who attempted suicide had prominent psychosocial stressors.19 Gender-related personality variables have been suggested as mediating factors in suicide attempts.20 In a record review of individuals with suicide attempt treated in an Indian general hospital setting, impulsive suicide attempts were associated with a greater degree of hopelessness and stressors.21 Following this literature review, three experts from the field of psychiatry and clinical psychology (the first three authors) designed the problem solving strategies, which were further reviewed by other experts and eventually refined.
Telephone-Based Psychosocial Intervention (TBPI)
TBPI is a manualized intervention that aimed to provide counseling by building upon the strategies suggested as part of baseline intervention. The literature review showed that telephone interventions with motivational support increased follow-up with mental health services in individuals presenting with suicide attempts.22 Another study compared telephone interventions that used principles of empathy and reassurance to treatment-as-usual in individuals with a suicide attempt not later than one month.23 From this literature review, TBPI was conceptualized as a manualized psychosocial intervention that used strategies derived from supportive, cognitive behavior, as well as dialectical behavior schools of therapy.24
The first session of TBPI was to be delivered around 7–10 days after the baseline intervention. This would consist of an initial inquiry into the mental status, followed by encouraging the participant to ventilate using reflective listening. This would be followed by a discussion on whether the participant was able to implement the problem-solving strategies that were suggested as part of baseline interventions, along with counseling about other possible strategies. TBPI would conclude with gentle reminders for treatment adherence, avoidance of substance use, and follow-up with mental health services as indicated. Two other similar sessions would be delivered around 14–17 days and 21–24 days after the baseline intervention. All TBPI sessions were intended to be of at least 12–15 minutes duration.
Telephone Contacts (TC)
TC consisted only of inquiry into mental status along with gentle reminders for treatment adherence, avoidance of substance use, and follow-up with mental health services as indicated. All sessions of TC were intended to be of 2–5 minutes duration. No problem solving or any other strategy was mentioned. TC was intended as a shorter duration, manualized comparator for TBPI. TC was similarly delivered around 7–10 days, 14–17 days, and 21–24 days after the baseline interventions.
Study Design
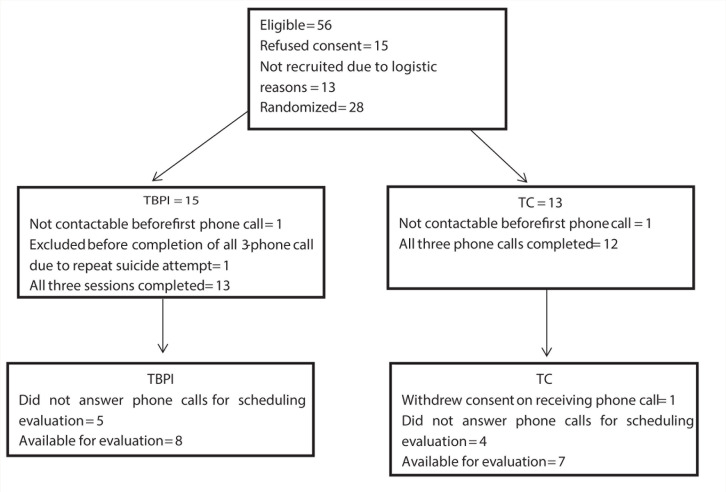
We used a randomized controlled parallel-group study design to evaluate the feasibility and acceptability of TBPI and TC. Participants were randomly allocated in a 1:1 ratio to either TBPI or TC, using a simple, computerized randomization performed separately at each site in blocks of ten. The randomization sequence was derived by other study personnel who were not involved in the delivery or feasibility evaluation of TBPI and TC (see Figure 1 for flow diagram).
Figure 1. Flow Diagram of Trial.
Research fellows reminded all the participants not to reveal the nature of their telephone conversations during the evaluation process. TBPI and TC sessions were delivered by the VSSV, and VG, who delivered the baseline intervention. TBPI and TC were evaluated for acceptability by STS, and NK, who had performed initial participant evaluation and was blind to whether participants had received TBPI or TC. With respect to those participants who did not have their own telephone and were keen on being part of this trial, we aimed to contact them to deliver the intervention on the telephone number of a caregiver identified by the participant.
Assessment of Feasibility and Acceptability of TBPI
Research fellows assessed outcomes face to face one month after the baseline interventions. Published recommendations state that feasibility trials should evaluate parameters that could impact the successful conduct of the main trial and should not evaluate the outcome of interest of the main study.25 In line with this, we did not use suicidal ideation, which is the primary outcome measure of the ongoing RCT, for this feasibility trial. We used dropout rates and acceptability scores as parameters of assessment. We deemed any participant who refused evaluation for acceptability scores after completing all the three sessions as a dropout. We considered dropout rates of <50% as adequate, in concordance with published research.26 We assessed acceptability using participant rated scores on a Likert visual analog scale with scores ranging from 0 to 10, similar to other studies.27 We considered scores >5 to represent greater acceptability.
We excluded participants who had a repeat suicide attempt prior to completion of all sessions of TBPI and TC as they needed more intensive psychiatric care. We assessed the feasibility and acceptability of TBPI in comparison to TC using SPSS version 16 with Mann–Whitney U test and chi-square tests, wherever appropriate, at 95% confidence intervals.
Safety Considerations
Both TBPI and TC were additional treatments that supplemented standard treatments as usual and encouraged adherence to prescribed pharmacological and psychological interventions. Research fellows took the utmost precautions to maintain confidentiality during recruitment, assessments, and delivery of interventions. Research fellows also noted down the phone number of at least one designated caregiver of the participant. Although it was aimed to maintain confidentiality at all times, in the event of the participant expressing prominent suicidal ideas or behaviors, the caregiver would be informed to ensure that the participant receives urgent mental health care in keeping with accepted clinical practice guidelines. (This was mentioned in the consent form also.) The participants continued to receive their existing mental health treatments as indicated.
Results
A total of 28 participants were recruited between January 2019 and April 2019 at the two sites. Table 1 shows participant details of age, gender, marital status, and type of psychiatric diagnosis. There were no significant differences between the TBPI and TC groups with respect to age, number of years of education, or gender, indicating that both groups were comparable.
Table 1.
Profile of Participants Receiving TBPI and TC
| Variable | TBPI (n = 15) | TC (n = 13) | Significance |
| Age in years | Median = 37 | Median = 30 | P = 0.28, Mann–Whitney U = 74.5 |
| Number of years of education | Median = 15 | Median = 15 | P = 0.54, Mann–Whitney U = 23 |
| Gender Male/female | 5/10 | 2/11 | P = 0.39, χ = 1.1197 |
| Relationship status Married/single | 8/7 | 9/4 | P = 0.46, χ = 0.738 |
| Type of psychiatric diagnosis | Common mental disorders (depression, anxiety, adjustment
disorders, dissociation) = 11 Nil psychiatric diagnosis = 4 Personality = 0 Others = 0 |
Common mental disorders (depression, anxiety, adjustment
disorders, dissociation) = 5 Nil psychiatric diagnosis = 5 Personality = 1 Others = 2 |
In view of small numbers, no tests of significance were performed |
TBPI: telephone-based psychosocial intervention, TC: telephone contact.
There were no significant differences in dropout rates (TBPI = 38.5% for 5 dropouts out of 13 participants, TC = 41.7% for 5 dropouts of 12 participants, χ = 0.027, P = 0.87) or acceptability scores (mean TBPI score = 8.63, SD = 2.326, range: 4–10, mean TC score = 7.57, SD = 2.149, range: 5–10; P = 0.29, Mann–Whitney U: 19.5). There were no significant differences between participants who did not drop out and those who dropped out with respect to age or number of years of education (age: Mann–Whitney U = 58.5, P = 0.07; the number of years of education: Mann–Whitney U = 12.0, P = 0.05) or sex (χ = 0.449, P = 0.50). There were no suicide attempts recorded in the participants who did not drop out in both TBPI and TC groups at one month after the baseline intervention.
Discussion
The immediate period after an attempted suicide is a critical phase for mental health interventions, due to an increased risk of recurrence and reattempt.28 This feasibility study demonstrated that telephone-based interventions are feasible and acceptable as a part of a mental health aftercare treatment package in individuals with a recent suicide attempt, in Indian general hospital settings. This study has also included a broad range of individuals with respect to age, gender, and psychiatric diagnoses and thus has generalizable findings. However, while dropout rates were within the expected range, these high dropout rates do indicate the difficulties in working with this vulnerable population that characteristically has low rates of engagement with mental health services.1
Periodic TCs in vulnerable individuals have been associated with better outcomes in comparison with routine referrals to specialist mental health services.29 However, there, TCs primarily comprised inquiry into the mental status of participants and reminders for treatment adherence.30 TBPI conceptualized in this study includes additional components of supportive therapy and problem solving techniques. This is relevant in view of Indian research demonstrating high rates of psychosocial stressors in suicide and the consequent need for appropriate psychosocial interventions.31
The National Mental Health Survey showed that the one-month prevalence of high suicidal risk was 0.9%, and the treatment gap for mental illnesses was 70%–86%.32 In this current scenario of COVID 19 pandemic, where telemedicine is important in ensuring the continued provision of mental health care in the absence of real-life access to psychiatric services, interventions like TBPI could provide additional help to those at high risk of suicide.33
A large multisite study showed that a combination of brief interventions, including phone calls, significantly reduced suicide behaviors in individuals at risk.34 Our findings demonstrate that TBPI could be an option to explore in individuals with suicide attempt, as part of a follow-up mental health care package in addition to standard treatments.
It is to be noted that our findings are from general hospitals in metropolitan cities. As this was a study of feasibility and acceptability, the sample size—although small—was according to accepted recommendations, and the study duration was relatively short.26 Feasibility studies help prospective researchers in assessing the potential implementation difficulties of the intervention under evaluation and the factors that can affect the validity of the main study findings.14 Feasibility studies are recommended to have objectives different from those of the main studies and usually assess issues of uncertainty around the main study.35 The outcome measures used in this study were acceptability and dropout rates of interventions, which are in line with recommendations of experts.27
In a RCT that compared immediate and delayed mobile-phone-based psychotherapy, immediate psychotherapy showed a reduction in suicidal ideation at six months.36 TBPI uses elements of problem solving similar to therapies in the aforementioned study.36 A systematic review showed that it was possible to engage vulnerable populations from all settings using phone and web-based interventions.15 Although evidence favors frequent contacts with high-risk individuals and the use of problem solving strategies in them, there is a need for more rigorous studies to provide confirmation.37 Studies from India have reported upon the utility of crisis helplines in community-based clinics in suicide prevention.38 Telepsychiatry models of mental health care appear to have an economic edge over traditional models in India.39 In this background, we infer that it is essential to go beyond feasibility studies and evaluate the efficacy of telephone-based psychosocial interventions in larger sample on outcomes like persistent suicidal ideation and behaviors that are associated with increased future suicide risk.
Conclusion
It is feasible to conduct studies on telephone-based psychosocial interventions and consider their use in individuals with recent suicide attempts in Indian settings. Telephone-based psychosocial interventions and contacts in the immediate aftermath of a suicide attempt are acceptable to vulnerable individuals. We are now continuing with the main RCT to evaluate the efficacy of such interventions on suicide behaviors.
Acknowledgments
We thank Dr Soumya Swaminathan (then Secretary, Dept. of Health Research, DHR), Dr Balram Bhargav, current Secretary DHR, Prof. VL Nimgaonkar, Dr Ravinder Singh, and Dr Harpreet Singh. We thank the faculty of “Cross-Fertilized Research Training for New Investigators in India and Egypt” (D43 TW009114, HMSC File No. Indo-Foreign/35/M/2012-NCD-1, funded by Fogarty International Centre, NIH). We are also thankful to National Coordinating Unit of ICMR for NMHP Projects for their constant support and guidance. We thank Data Management Unit of ICMR for designing the database.
We also thanks to Dr (Prof.) MV Ashok for his wholehearted support in conducting this study, Mrs Navneet Kaur for her brief stint as JRF, Mrs Vinnarasi, Mr Vikas for data entry, Mrs Jayasudha N, service manager (Assertive Management of Attempted Suicide) in Bengaluru, for participant recruitment and guidance.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The work was supported by the Indian Council Medical Research (ICMR) under Capacity Building Projects for National Mental Health Programme, ICMR-NMHP.
Data Sharing
This study was funded by the Indian Council of Medical Research (ICMR), with research oversight by a National Coordination Unit, under Capacity Building Projects of National Mental Health Program, ICMR-NMHP.
ICMR-NMHP has also set up a Data Managing Unit (DMU) with a data repository and server into which anonymized data from this study and other similar projects are deposited.
Any data sharing will be considered after the funded study is complete and due permission from ICMR is obtained.
References
- 1.Hom MA, Stanley IH, and Joiner TE. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: a review of the literature. Clin Psychol Rev, 2015; 40 28–39. [DOI] [PubMed] [Google Scholar]
- 2.Lester D and Walker RL. The stigma for attempting suicide and the loss to suicide prevention efforts. Crisis, 2006; 27 147–148. [DOI] [PubMed] [Google Scholar]
- 3.Ribeiro JD, Franklin JC, Fox KR, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med, 2016; 46 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferrari AJ, Norman RE, Freedman G, et al. The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study, 2010. PLoS One 2014; 9: e91936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vijayakumar L. Indian research on suicide. Indian J Psychiatry, 2010; 52: 291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zalsman G, Hawton K, Wasserman D, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry, 2016; 3 646–659. [DOI] [PubMed] [Google Scholar]
- 7.Lizardi D and Stanley B. Treatment engagement: a neglected aspect in the psychiatric care of suicidal patients. Psychiatr Serv, 2010; 61 1183–1191. [DOI] [PubMed] [Google Scholar]
- 8.McCabe R, Garside R, Backhouse A, et al. Effectiveness of brief psychological interventions for suicidal presentations: a systematic review. BMC Psychiatry, 2018; 18 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Milner A, Spittal MJ, Kapur N, et al. Mechanisms of brief contact interventions in clinical populations: a systematic review. BMC Psychiatry, 2016; 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fleischmann A, Bertolote JM, Wasserman D, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull World Health Organ, 2008; 86 703–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper J, Hunter C, Owen-Smith A, et al. “Well it’s like someone at the other end cares about you.” A qualitative study exploring the views of users and providers of care of contact-based interventions following self-harm. Gen Hosp Psychiatry, 2011; 33 166–176. [DOI] [PubMed] [Google Scholar]
- 12.Gates P and Albertella L. The effectiveness of telephone counselling in the treatment of illicit drug and alcohol use concerns. J Telemed Telecare, 2016; 22 67–85. [DOI] [PubMed] [Google Scholar]
- 13.Tickle-Degnen L. Nuts and bolts of conducting feasibility studies. Am J Occup Ther, 2013; 67 171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud, 2016; 2 1–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menon V, Rajan TM, and Sarkar S. Psychotherapeutic applications of mobile phone-based technologies: a systematic review of current research and trends. Indian J Psychol Med, 2017; 39: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hawk M, Nimgaonkar V, Bhatia T, et al. A ‘Grantathon’ model to mentor new investigators in mental health research. Health Res Policy Syst, 2017; 15: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical Stat: J Appl Stat Pharmaceutical Ind, 2005; 4 287–291. [Google Scholar]
- 18.Pederson L and Pederson CS. The expanded dialectical behavior therapy skills training manual: practical DBT for self-help, and individual and group treatment settings. PESI Publishing & Media, 2012. [Google Scholar]
- 19.Radhakrishnan R and Andrade C. Suicide: an Indian perspective. Indian J Psychiatry, 2012; 54: 304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Menon V, Sarkar S, and Kattimani S. Association between personality factors and suicide intent in attempted suicide: gender as a possible mediator? Indian J Psychol Med, 2015; 226 220–226. [DOI] [PubMed] [Google Scholar]
- 21.Kattimani S, Sarkar S, Rajkumar RP, et al. Stressful life events, hopelessness, and coping strategies among impulsive suicide attempters. J Neurosci Rural Pract, 2015; 6: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cedereke M, Monti K, Öjehagen A. Telephone contact with patients in the year after a suicide attempt: does it affect treatment attendance and outcome? A randomised controlled study. Eur Psychiatry, 2002; 17 82–91. [DOI] [PubMed] [Google Scholar]
- 23.Vaiva G, Ducrocq F, Meyer P, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. Br Med J, 2006; 332 1241–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawton K, Witt KG, Salisbury TLT, et al. Psychosocial interventions following self-harm in adults: a systematic review and meta-analysis. Lancet Psychiatry, 2016; 3 740–750. [DOI] [PubMed] [Google Scholar]
- 25.Arain M, Campbell MJ, Cooper CL, et al. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol, 2010; 10: 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei S, Liu L, Bi B, Tan S, et al. An intervention and follow-up study following a suicide attempt in the emergency departments of four general hospitals in Shenyang, China. Crisis, 2013; 34 107–115. [DOI] [PubMed] [Google Scholar]
- 27.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med, 2009; 36 452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hunt IM, Kapur N, Webb R, et al. Suicide in recently discharged psychiatric patients: a case-control study. Psychol Med, 2009; 443–449. [DOI] [PubMed] [Google Scholar]
- 29.Vijayakumar L, Shujaath Ali Z, Kesavan K, et al. Intervention for suicide attempters: a randomized controlled study. Indian J Psychiatry, 2011; 53: 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cebrià AI, Parra I, Pàmias M, et al. Effectiveness of a telephone management programme for patients discharged from an emergency department after a suicide attempt: controlled study in a Spanish population. J Affect Disord, 2013; 147 269–276. [DOI] [PubMed] [Google Scholar]
- 31.Dandona R, Bertozzi-Villa A, Kumar GA, et al. Lessons from a decade of suicide surveillance in India: who, why and how? Int J Epidemiol, 2016; 2 983–993. [DOI] [PubMed] [Google Scholar]
- 32.Murthy Rs. National mental health survey of India, 2015–2016. Indian J Psychiatry 2017; 59: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou X, Snoswell CL, Harding LE, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed e-Health, 2020. March 23; 26(4). DOI: 10.1089/tmj.2020.0068 [DOI] [PubMed] [Google Scholar]
- 34.Miller IW, Camargo CA, Arias SA, et al. Suicide prevention in an emergency department population: the ED-safe study. JAMA Psychiatry, 2017; 74 563–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lancaster GA. Pilot and feasibility studies come of age! Pilot Feasiblity Stud, 2015; 1: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marasinghe RB, Edirippulige S, Kavanagh D, et al. Effect of mobile phone-based psychotherapy in suicide prevention: a randomized controlled trial in Sri Lanka. J Telemed Telecare, 2012; 18 151–155. [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization MhGAP Humanitarian Intervention Guide (mhGAP-HIG): clinical management of mental neurological and substance use conditions in humanitarian emergencies. Geneva: World Health Organization, 2015. [Google Scholar]
- 38.Shrivastava AK, Johnston ME, Stitt L, et al. Reducing treatment delay for early intervention: evaluation of a community based crisis helpline. Ann Gen Psychiatry, 2012; 11: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moirangthem S, Rao S, Kumar CN, et al. Telepsychiatry as an economically better model for reaching the unreached: a retrospective report from South India. Indian J Psychol Med, 2017. May; 39(3): 271. [DOI] [PMC free article] [PubMed] [Google Scholar]