Human activity existentially threatens the earth’s ecosystems, on which economic prosperity and human health depend. The most severe consequences of jeopardizing these ecosystems are the multifactorial loss of biodiversity and the climate crisis, the latter being an effect of anthropogenic greenhouse gas emissions [1]. The health sector plays two pivotal roles in dealing with these fundamental challenges: first, it must become resilient against the effects of climate change (extreme weather events, heat waves, pandemics or spread of various infectious (zoonotic) diseases) [2]. Secondly, as the health care sector is responsible for almost 5% of global greenhouse gas emissions and due to the high social standing and credibility of health care professionals, the sector has a key role in the mitigation of climate change—by getting our own house in order (Maria Neira, Director, Department of Public Health and Environment, World Health Organization [3]). This accounts for hospitals and is especially true for critical resources such as intensive care units.
The contribution of critical care to the carbon footprint
The precise contribution of critical care medicine products, processes, and systems to carbon dioxide emissions (CO2e) and other aspects of environmental harm (energy and water consumption, single-use devices and waste production, global warming potential of drugs or medical items) have not been analyzed in detail so far, but a few studies provide valuable insights into them.
A study from England calculated an average daily consumption of 15 kWh of electric energy per intensive care unit (ICU) patient, mostly for delivering care to patients and monitoring their condition, which is similar to that of an average 4-person household [4]. Several studies have conducted bottom-up ‘life cycle assessments’ (LCAs) for an analysis of the carbon footprint of natural resource extraction, manufacturing, packaging, transport, use/reuse, and recycling/waste disposal of certain products or processes [5], but such analyses are always influenced by regional factors (e.g. local costs of energy or transportation, level of wages and salaries, etc.). The administration of drugs is a core element in intensive care; and LCA’s of drugs begin with the extraction of raw material over the manufacturing and packaging up to the transport to the ICU. MacAlister et al. [6] performed an LCA-study of morphine ‘from opium poppy to the packaged drug’, and they assessed a carbon footprint for a standard infusion bag (100 mg morphine) of 204 g CO2e, corresponding to driving a car 1 km. In an audit of recyclable waste in a 10-bed Australian ICU [7], the total waste for the week was 540 kg, of which 60% could be recycled with appropriate processes (safeguard, education, or training). Based on a prospective observational LCA analysis in the United States, the carbon footprint related to the treatment of ten septic shock patients [8] (energy for heating, ventilation, air conditioning, lighting, machines, all consumables and waste) revealed an average one-patient energy consumption of 272 kWh/day and consumption of 3.4 kg/day of single-use material. All this sums up to an average CO2e footprint of 178 kg per day (equivalent to the total daily carbon footprint for 3.5 Americans).
ICU sustainability: how can we get our own house in order?
Intensive care medicine is—evidently—one of the highest carbon footprint relevant sectors in health care. Given the urgency to reduce carbon footprint and based on LCAs, it is imperative to start with a shift to practical measures (conversion to renewable energies, reduction of energy consumption, avoiding direct greenhouse gas emissions whenever equivalent alternatives are available). Several publications have analysed specific measures to consistently reduce CO2-emissions in critical care [4, 8–10]. These recommendations refer mainly to carefully performed LCAs of frequently used medical items (and in consequence possible changes to daily routine), the management of consumables and waste, and a vigilant check of possible reductions in energy use. They also refer to the avoidance of futile treatment in critical care (a treatment that never reaches patient’s goals, or where death is imminent, or where the patient would never be able to survive outside an ICU [11]) which implies not only ethical but also environmental aspects. The general prevention of overtreatment is possibly the best current contribution to environmental sustainability (Fig. 1).
Fig. 1.
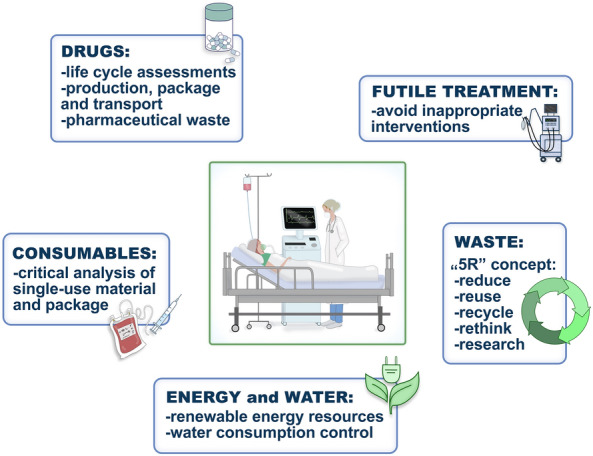
Components of a concept of environmental sustainability in intensive care medicine
However, for many procedures or items, LCA-results are missing or contradictory, especially for the comparison between single-use and re- or multi-use items. For example, McGain et al. [12] found out in Australia that the environmental costs for reusable central venous catheter insertion kits were considerably greater than those for single-use kits, even under the condition of careful waste management. For the multifaceted sector of high-level intensive care, more LCAs like McGain’s are needed (e.g. for face masks, breathing circuits, linens, sterile cover, plastic or glas bags, blood pressure cuffs), or for many other drugs used frequently in the ICU (antibiotics, analgesics, sedation). For sustainable management of consumables, a critical analysis of the frequent usage of single-use material should be given a push in a dialogue with manufacturers, medical industry, and ‘consumers’.
While currently waste generation is inevitable in critical care, adopting waste programmes for the rational use of resources and participation of intensivists in-hospital product evaluation comitees are important ways to reduce carbon footprint [6]. For the “5R-concept” (reduce, reuse, recycle, rethink, and research) several aspects, from plastic packaging to handling of dangerous wastes, are currently under critical discussion or constitute research projects [10]. Additionally, the use of telemedicine [13], the promotion of online meetings, and the streaming of regional or global conferences may prove to be efficient alternatives to reducing carbon footprint-associated flight, car or railway travels.
The Hippocratic Oath “First do not harm” refers not only to the interaction with individual patients, but also to the responsibility of maintaining a healthy ecosystem as a prerequisite for human health. Thus, health care professionals are required to adapt their daily routine and supporting efforts to reducing global warming. Furthermore, in global critical care supply, there is a marked variation representing disparities between developed countries with a (too) large chunk of intensive care spending (and consequently high carbon footprint) and developing countries with a greater burden of critical illness, but little infrastructure to provide care [14]. The dissolution of such inequality may be another precondition to aiming long-term sustainability. Such engagement requires new models of collective leadership [15], critical reflections, inclusivity and motivated action on all levels of healthcare stakeholders, policy, professional societies, hospital administration and ICU staff. Financial and social incentives may enhance the efforts to stop the deleterious effects of deteriorating ecosystems on public health [16]. Time is pressing and critical care medicine must participate in the race to zero-emission health care systems.
Funding
Open Access funding enabled and organized by Projekt DEAL. SK: Inventor of two patents (PCT/EP2019/060788/PCT/EP2019/065832), sold to Medtronic/Covidien. Received speaker’s honoraria from Medtronic. Received personal fees from Georg Thieme Verlag. Reports grants during the conduct of a study from the German Research Society.
Declarations
Conflict of interests
TB and CS declare no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, Ezeh A, Frumkin H, Gong P, Head P, Horton R, Mace GM, Marten R, Myers SS, Nishtar S, Osofsky SA, Pattanayak SK, Pongsiri MJ, Romanelli C, Soucat A, Vega J, Yach D. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet. 2015;386:1973–2028. doi: 10.1016/S0140-6736(15)60901-1. [DOI] [PubMed] [Google Scholar]
- 2.Bein T, Karagiannidis C, Quintel M. Climate change, global warming, and intensive care. Intensive Care Med. 2020;46:485–487. doi: 10.1007/s00134-019-05888-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation: Healthy Hospitals—Healthy Planet—Healthy People (2021) Addressing climate change in health care settings. https://www.who.int/globalchange/publications/healthcare_settings/en/. Accessed 22 May 2021
- 4.Pollard AS, Paddle JJ, Taylor TJ, Tillyard A. The carbon footprint of acute care: how energy intensive is critical care? Public Health. 2014;128:771–776. doi: 10.1016/j.puhe.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 5.McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth. 2020;125:680–692. doi: 10.1016/j.bja.2020.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McAlister S, Ou Y, Neff E, Hapgood K, Story D, Mealey P, McGain F. The Environmental footprint of morphine: a life cycle assessment from opium poppy farming to the packaged drug. BMJ Open. 2016;6(10):e013302. doi: 10.1136/bmjopen-2016-013302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGain E, Hendel SA, Story DA. An audit of potentially recyclable waste from anaesthetic practice. Anaesth Intensive Care. 2009;37:820–823. doi: 10.1177/0310057X0903700521. [DOI] [PubMed] [Google Scholar]
- 8.McGain F, Burnham JP, Lau R, Aye L, Kollef MH, McAlister S. The carbon footprint of treating patients with septic shock in the intensive care unit. Crit Care Resuse. 2018;20:304–312. [PMC free article] [PubMed] [Google Scholar]
- 9.Baid H, Richardson J, Scholes J, Hebron C. Sustainability in critical care practice: a grounded theory study. Nurs Crit Care. 2021;26:20–27. doi: 10.1111/nicc.12493. [DOI] [PubMed] [Google Scholar]
- 10.Schuster M, Richter H, Pecher S, Koch S, Coburn M. Ecological sustainability in Anesthesiology and Intensive Care Medicine. A DGAI and BDA position paper with specific recommendations. Anaesth Intensivmed. 2020;61:329–338. [Google Scholar]
- 11.Huynh TN, Kleerup EC, Wiley JF, Savitsky TD, Guse D, Garber BJ, Wenger NS. The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med. 2013;173:1887–1894. doi: 10.1001/jamainternmed.2013.10261. [DOI] [PubMed] [Google Scholar]
- 12.McGain F, McAlister S, McGavin A, Story D. A life cycle assessment of reusable and single-use central venous catheter insertion kits. Anesth Analg. 2012;114:1073–1080. doi: 10.1213/ANE.0b013e31824e9b69. [DOI] [PubMed] [Google Scholar]
- 13.Holmner A, Ebi KL, Lazuardi L, Nilsson M. Carbon footprint of telemedicine solutions—unexplored opportunity for reducing carbon emissions in the health sector. PLoS ONE. 2014;9:e105040. doi: 10.1371/journal.pone.0105040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fowler RA, Adhikari NK, Bhagwanjee S. Clinical review: critical care in the global context–disparities in burden of illness, access, and economics. Crit Care. 2008;12:5. doi: 10.1186/cc6984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacNeill A, Forbes McGain F, Sherman J. Planetary health care: a framework for sustainable health systems. Lancet Planet Health. 2021;5:e66–e68. doi: 10.1016/S2542-5196(21)00005-X. [DOI] [PubMed] [Google Scholar]
- 16.Baid H, Damm E. Reducing critical care’s carbon footprint with financial and social co-benefit. Intensive Crit Care Nurs. 2021 doi: 10.1016/j.iccn.2021.103030. [DOI] [PMC free article] [PubMed] [Google Scholar]


