Abstract
Currently, we have different technologies and techniques that improve the results in orbital trauma. However, there are few studies that study the technological integration in orbital trauma and the synergism of all the techniques. For this reason, the objective of this case is to illustrate the management of orbital trauma by integrating endoscopic support, virtual surgical navigation, patient-specific implant, virtual surgical planning in the management of a sequel due to insufficient reconstruction of orbital volume.
Keywords: Endoscopic support, Virtual surgical navigation, Patient-specific implant, Virtual surgical planning, Orbital trauma
Introduction
Orbital fractures can be isolated or combined with other facial fractures. Although its management is usually routine, the best surgical approach, or the adequate time, and the best reconstruction material have become a topic of discussion. Furthermore, today, the increasing use of technology can increase this confusion [1]. Endoscopic support, in orbital trauma, has been used since 1972 when Walter used a transantral approach for the early repair of these types of fractures, providing a direct view of the defect and the most relevant anatomical structures [2]. Virtual intraoperative navigation in the reconstruction of the zygomatic complex began in the 1990s with high costs for the health system and additional training that limited its use [3]. However, detailed images of the defect caused by the fracture can be obtained and allow the application of volumetric tools of great importance in orbital trauma [4]; this provides better intraoperative orientation concerning adjacent critical structures and facilitates proper positioning of the reconstruction implants [5].
Although the use of technology in medicine has increased, the scientific literature studying the combination of these techniques is still scarce. Therefore, this case presentation aims to illustrate the applicability and synergy of technology in orbital trauma reconstruction.
Case Presentation
A 35-year-old female attends the otolaryngology and oral and maxillofacial surgery services at the Hospital Universitario de la Samaritana, Bogotá, Colombia, with sequelae of orbital trauma. The patient underwent an operation with conventional techniques 8 months before the time of her consultation. The diplopia and an enophthalmos of 2.8 mm quantified with a Hertel or Naugle exophthalmometer were not resolved.
To manage the sequelae, a CT scan was requested from the patient, and the DICOM files were imported into the software (iPlan CMF 3.0 BrainLab, Brainlab Inc., Westchester, IL). Next, images were obtained in STL format, and virtual surgical planning was performed using the mirror image technique as shown in Fig. 1. Then, the volumetric assessment was taken into account, observing a preoperative volume on the affected side of 28.91 cm3 (Fig. 1a). The virtual surgical plan was uploaded to the Kick navigation station (Munich, Brainlab AG) (version 3.5.0.213, Munich, Brainlab AG) for intraoperative use. It is detected by impedance and additional spheres on the pointer (Soft touch Pointer VV Cranial/ENT 7.9.1 Brainlab Inc Munich), which is correlated with presurgical images (Fig. 2). The planning includes the design and fabrication of a custom-made, patient-specific prosthesis (PEKK OPTIMAR LT1PL40) (Fig. 2a). The endoscope is integrated into the navigation flow using an instrument adapter according to the size of the instrument, and the adapter has a clamp and a reference star that has spheres on it that act as reference points. The reference star is responsible for establishing the instruments’ location during the navigation (Instrument Adapter Array, Brainlab AG Munich). The integration then continues with the calibration matrix, setting the length, the diameter (Calibration of the Matrix instrument: VectorVision Cranial/ENT 6.01 Brainlab AG Munich) and the vector of the instrument that is being integrated, in this case the endoscope, to be able to accurately represent it in navigation (Hopkins RII Wide Angle Oblique Forward 30° diameter 4 mm Length 18 cm Storz Tuttlingen, Germany) as shown in Fig. 3. The procedure then is carried out using a transconjunctival approach; the titanium mesh from the left orbital floor is removed. Nevertheless, the osteosynthesis material from the frontonasal region used in the first surgical period is left in position because it did not interfere with the new procedure or affect orbital volume. Transmaxillary endoscopic examination is performed to identify anatomical landmarks and borders, reposition orbital content including the fat tissue, adequately relocate the orbital globe and position the patient-specific implant making sure it is passively seated, and then fixating the implant with titanium screws. The entire procedure was performed with endoscopically assisted intraoperative navigation in real time (Figs. 4, 5). In the end, extraocular movements are assessed with a forced duction test.
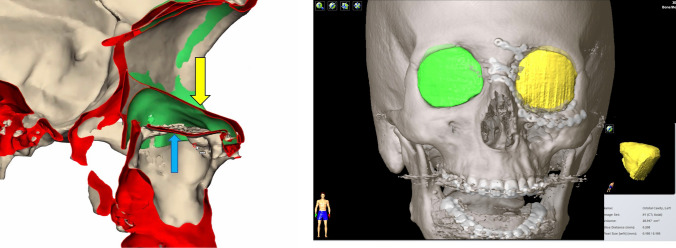
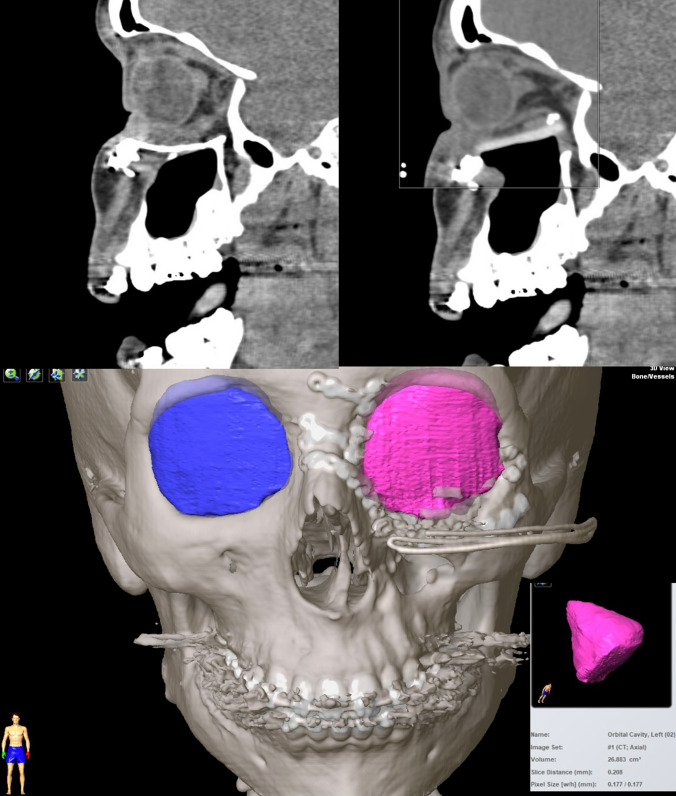
Fig. 1.
Mirror image, sagittal section. Yellow arrow shows the orbital floor of the unaffected side, overlapping on the affected left orbit; blue arrow shows titanium mesh used on the fractured side from initial surgical procedure (position difference). A. Volumetric reconstruction of the orbit (yellow areas and cone)
Fig. 2.
Virtual planning allows us to design and fabricate an implant with the correct position of the orbital floor. a PEEK Orbital Floor Implant. 3D printed model with implant guide
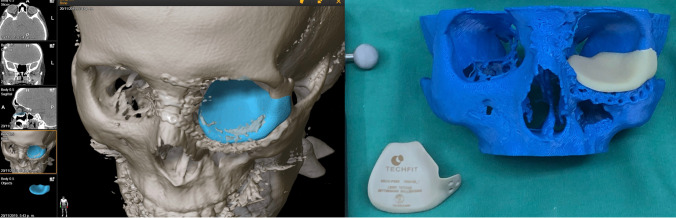
Fig. 3.
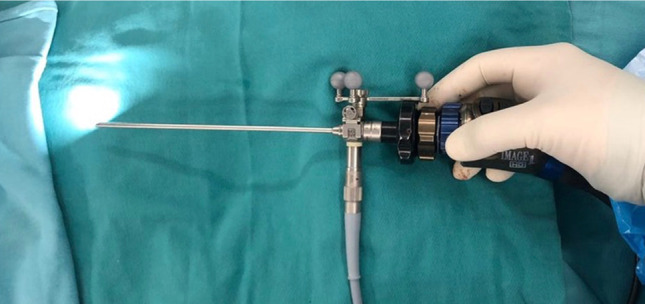
Integration of the endoscope in the navigation flow Arrow: Instrument adapter with clamp and reference star with the three spheres
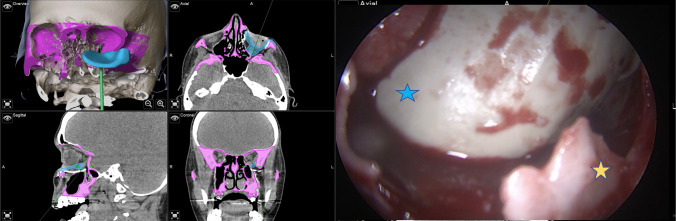
Fig. 4.
The real-time navigation module allows to improve the location of the implant of the floor of the left orbit, interacting with the virtual planning. Blue star: The lower posterior portion of the PEEK implant. Yellow arrow: posterior portions of the floor of the left orbit. Evaluating the anatomical posterior boundaries
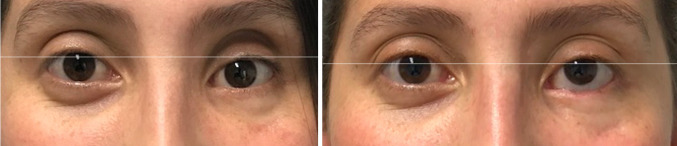
Fig. 5.
Presurgical enophthalmos with 2.8 mm. Correction of the enophthalmos now resulting in 0.3 mm
The procedure was completed without complications, and at 2-week follow up, there was a slight restriction of extraocular movements, likely due to edema. At six months, a photograph was obtained, and there was an improvement in the enophthalmos, going from 2.8 to 0.3 mm (Fig. 6). A postoperative computed tomography (CT) scan was performed to verify orbital volume, and it had decreased to 26.8 cm3
Fig. 6.
Slices of the CT scan with the correction of the orbital floor. 3D image with 26.8 cm3 postoperative orbital volume
Discussion
Complications associated with the position of the orbital balloon vary between 20 and 80%, possibly due to failure to restore the patient’s innate previous anatomy before the trauma. However, through the mirror technique, different software programs were reestablishes as close as possible to the patient’s initial anatomy [7]. Consequently, enophthalmos is related to the insufficient reconstruction of orbital volume or persistence of muscle entrapment and necrosis of adipose tissue. On the other hand, stereolithographic models allow the design and manufacture of patient-specific implants, which improves the risks of a severely bent plate and reduces the time of conformation during surgery. Persistent diplopia has been reported between 10% and 37%, affecting the postoperative quality of life [8]. This is generally related to the loss of anatomical landmarks and limited space, without a proper reconstruction [9].
Copelli et al. [10] published a study that included 53 subjects with different orbital fractures. Only eight cases used endoscopic support, seven additionally used virtual planning and 38 received conventional treatment. According to their results, they suggest that endoscopic support provides a noninvasive surgical approach with adequate visualization. Nonetheless, they add that intraoperative navigation improves anatomical understanding to reduce risks and obtain better reconstruction. Chen et al. [6] studied 24 patients with postoperative diplopia or enophthalmos with early management (first 30 days) and late management (after 30 days); 87.5% had better results with early treatment when they were managed using intraoperative navigation and endoscopic support. When fractures are managed 6 months after injury, 72% of enophthalmos can persist. In contrast, if management is performed in the first 2 weeks, the enophthalmos persists only in 20%, with time being an important variable to take into account.
The use of custom-made PEEK implants facilitates orbital reconstructions due to the complex anatomy that would increase intra-surgical modeling times with conventional techniques. The costs are high and the planning time must be taken into account. However, the physical and mechanical properties are similar to bone, and excellent biocompatibility generates interest [11]. 3D printing in medicine continues to gain importance; however, like new technologies, it has the drawbacks of high costs, planning time, printing time and additional training. In orbital reconstruction, whether oncological or trauma, it has excellent versatility due to the adequate adaptation to the orbit’s complex anatomical structures [12].
Conclusion
This case illustrates a secondary orbital reconstruction. This supports that virtual surgical planning, intraoperative navigation, preparation of patient-specific implants and the integration of endoscopic techniques are useful to avoid complications and/or sequelae in primary treatment, avoiding complex procedures. In our extensive literature search, a small number of studies observed the synergism of the different techniques in orbital trauma, which should be taken into account in the subsequent studies.
Acknowledgements
We want to thank Dr. Andres Gomez for all his teachings and recommendations to continue in this process.
Funding
Not applicable.
Compliance with Ethical Standards
Conflict of interest
The authors have expressed no conflict of interest.
Availability of Data and Material
Data available.
Consent to Participate
Consent to participate was approved by the patient.
Consent for Publication
It was obtained.
Ethics Approval
The ethics approval was obtained.
Informed Consent
The consent for publication was obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liss J, Stefko ST, Chung WL. Orbital surgery: state of the art. Oral Maxillofac Surg Clin North Am. 2010;22:59–71. doi: 10.1016/j.coms.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Walter WL. Early surgical repair of blowout fracture of the orbital floor by using the transantral approach. South Med J. 1972;65:1229–1243. doi: 10.1097/00007611-197210000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Ikeda K, Suzuki H, Oshima T, Takasaka T. Endoscopic endonasal repair of orbital floor fracture. Arch Otolaryngol Head Neck Surg. 1999;125:59–63. doi: 10.1001/archotol.125.1.59. [DOI] [PubMed] [Google Scholar]
- 4.Jansen J, Schreurs R, Dubois L, Maal TJJ, Gooris PJJ, Becking AG. The advantages of advanced computer-assisted diagnostics and three-dimensional preoperative planning on implant position in orbital reconstruction. J Craniomaxillofac Surg. 2018;46:715–721. doi: 10.1016/j.jcms.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Watzinger F, Wanschitz F, Wagner A, Enislidis G, Millesi W, Baumann A, Ewers R. Computer-aided navigation in secondary reconstruction of post-traumatic deformities of the zygoma. J Craniomaxillofac Surg. 1997;25:198–202. doi: 10.1016/S1010-5182(97)80076-5. [DOI] [PubMed] [Google Scholar]
- 6.Chen CT, Pan CH, Chen CH, Shyu VB, Wu JC, Kang GC. Clinical outcomes for minimally invasive primary and secondary orbital reconstruction using an advanced synergistic combination of navigation and endoscopy. J Plast Reconstr Aesthet Surg. 2017;71:90–100. doi: 10.1016/j.bjps.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 7.Bly RA, Chang SH, Cudejkova M, Liu JJ, Moe KS. Computer-guided orbital reconstruction to improve outcomes. JAMA Facial Plast Surg. 2013;15:113–120. doi: 10.1001/jamafacial.2013.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu CK, Hsieh MW, Chang HC, Tai MC, Chien KH. Anatomic factors predicting postoperative strabismus in orbital wall fracture repair. Sci Rep. 2019;9:14785. doi: 10.1038/s41598-019-51127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bell RB, Markiewicz MR. Computer-assisted planning, stereolithographic modeling, and intraoperative navigation for complex orbital reconstruction: a descriptive study in a preliminary cohort. J Oral Maxillofac Surg. 2009;67:2559–2570. doi: 10.1016/j.joms.2009.07.098. [DOI] [PubMed] [Google Scholar]
- 10.Copelli C, Manfuso A, d’Ecclesia A, Catanzaro S, Cassano L, Pederneschi N, Tewfik Hanna K, Cocchi R. Endoscopic transnasal approach and intraoperative navigation for the treatment of isolated blowout fractures of the medial orbital wall. J Craniomaxillofac Surg. 2015;43:1974–1978. doi: 10.1016/j.jcms.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Tian W, Chen J, Yu J, Zhang J, Chen J. The application of polyetheretherketone (PEEK) implants in cranioplasty. Brain Res Bull. 2019;153:143–149. doi: 10.1016/j.brainresbull.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Ruiters S, Mombaerts I. Applications of three-dimensional printing in orbital diseases and disorders. Curr Opin Ophthalmol. 2019;30:372–379. doi: 10.1097/ICU.0000000000000586. [DOI] [PubMed] [Google Scholar]