Abstract
Introduction
Condylar displacement after bilateral sagittal-split osteotomy (BSSO) occur in the sagittal plane as clockwise/counter-clockwise rotation of the ramus, in the coronal plane as medial/lateral inclination, or in the axial plane as medial/lateral condylar torquing. The purpose of this prospective CT study was to evaluate the role of plate fixation in minimizing condylar torquing or rotational changes in the axial plane.
Materials and Methods
This prospective study was carried out on 26 patients, 13 of whom underwent advancement BSSO and 13 setback BSSO, without maxillary LeFort I osteotomies. All mandibular movements were symmetrical. Fixation of the osteotomized segments was achieved with a single 4-hole plate and monocortical screws. In case of mandibular setbacks, a straight plate was used, whereas an inset-bent plate was used for advancements. Computed tomography scans were obtained preoperatively and postoperatively to measure condylar rotation or torqueing in the axial plane. An increase in condylar angle on axial slices was considered as lateral condylar torquing, whereas a decrease was considered as medial condylar torquing
Results
A mean medial condylar torquing of 0.2° was noted postoperatively in case of setbacks (p > 0.05 not significant). This suggested minimal condylar torquing, indicating that the proximal and distal segments maintained contact at the anterior vertical osteotomy fixed with a straight plate. In case of advancements, a mean lateral condylar torquing of 2.2° was noted postoperatively (p < 0.005, highly significant). This suggested that the proximal segment flare at the anterior vertical osteotomy site was maintained by inset-bent plate fixation.
Conclusion
The gaps between the proximal and distal segments created by mandibular advancement and setback should be maintained. An attempt to close these gaps, especially in mandibular advancement, will result in an unfavourable axial condylar torque. Consequently, the areas of bony contact between the proximal and distal osteotomy sites created by mandibular advancement and setback should be maintained as well.
Keywords: Condylar torque, Condylar rotation, Mandibular sagittal-split osteotomy, BSSO fixation
Introduction
The postoperative position of the condyle-bearing ramus or proximal segment after bilateral sagittal-split osteotomy (BSSO) is influenced by various factors. It involves condylar positioning methods, the interference between the proximal and distal segments, type of fixation, operator experience, and influence of the masticatory muscles. The main reasons to justify precise repositioning of the condylar segment after sagittal-split osteotomies of the mandible is to ensure long-term stability of the surgical result, to reduce adverse and/or potentially adverse effects on the temporomandibular joint (TMJ) and improve postoperative masticatory efficiency [1].
Appropriate seating of the condyle in the glenoid fossa during fixation of the osteotomized segments in BSSO is paramount in preventing postoperative sequelae like TMD/internal derangement, condylar resorption, condylar sag (peripheral and central), malocclusion, and relapse secondary to condylar displacement. Condylar displacement can occur in the sagittal plane as clockwise/counter-clockwise rotation of the ramus, in the coronal plane as medial/lateral inclination, or in the axial plane as medial /lateral condylar torquing.
Simple sagittal displacement of the condyle can usually be corrected by postoperative adjustment of the occlusion. However, condylar displacement with axial rotation does not respond to occlusal adjustment and has an increased risk of temporomandibular disorders [2, 3]. Such axial rotational changes also play an important part in condylar resorption after BSSO [4, 5].
The purpose of this prospective CT study was to evaluate the role of plate fixation in minimizing condylar rotational changes or torquing or in the axial plane.
Methodology
This prospective study was carried out at the Department of Oral and Maxillofacial Surgery on 26 patients, 13 of whom underwent advancement BSSO and 13 setback BSSO. No simultaneous maxillary LeFort I procedures were carried out. There were a total of 17 males and 9 females. The ages of the patients ranged from 17 to 29 years, with an average age of 21 years. The amount of setback ranged from 4 to 12 mm (mean 6.6 mm). The amount of mandibular advancement ranged from 4 to 13 mm (mean 6.0 mm). All mandibular movements were symmetrical. The study was approved by the Ethics Review Board of the Institution. All patients received presurgical orthodontics. All cases were performed by the two senior authors of this study employing a standard osteotomy technique, the same condylar positioning method, and a standard fixation technique. All patients underwent a modified bilateral sagittal-split osteotomy technique as described by Wolford et al. [6]. Any bony interferences between the contacting cortical surfaces of the proximal and distal segments were eliminated in order to ensure a uniform contact area before fixation. Fixation of the osteotomized segments was achieved with a single 4-hole plate and monocortical screws along the external oblique ridge. In case of mandibular setbacks, a straight plate was used (Fig. 1), whereas an inset-bent plate (Fig. 2) was used for advancements. The gap or flare between the proximal and distal segments on mandibular advancements was maintained during fixation. No condylar positioning devices were used. During fixation, the anteroinferior border of the proximal segment was pushed posteriorly and slightly inferiorly with a straight Cottle osteotome, while applying light extraoral digital pressure to the angle of the mandible pushing superiorly and slightly anteriorly. The resultant vector to the proximal segment was anterosuperior.
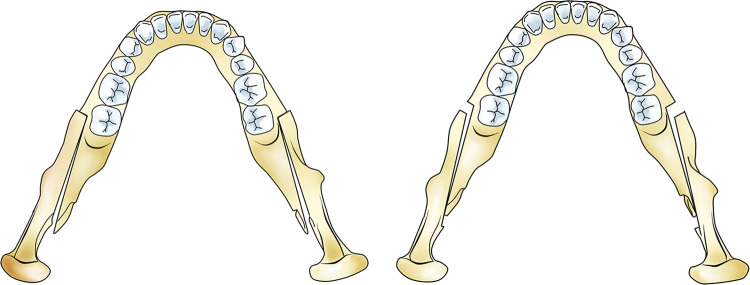
Fig. 1.

Straight plate fixation for mandibular setback
Fig. 2.

Inset-bent plate fixation for mandibular advancement
Measurement of Condylar Angle on Axial CT
Preoperative (1 week prior to surgery) and postoperative (3 months post-surgery) computed tomography (CT) scans were obtained. All preoperative and postoperative CTs were taken with the patient biting in centric occlusion or maximum intercuspation. In axial scan images, the slice with the greatest mediolateral dimension of the condylar head was obtained for each side. A midsagittal line was drawn from the base of vomer to the midpoint of clivus of the sphenoid (line A). Line B was drawn along the axis of the condyle from the lateral pole to the medial pole. Axial rotation of the condyle was measured as a change in the angulation between lines A and B, indicating the medial or lateral rotation of the condyles (Fig. 3).
Fig. 3.
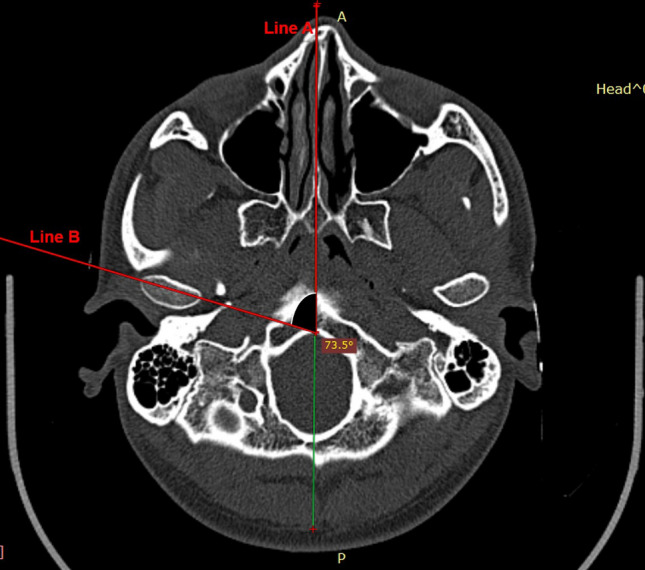
Condylar angle measurement on axial CT scan images
Interpretation of Condylar Axial Angle Changes with Proximal Segment Movement
An increase (positive change) in condylar angle in the axial slices was considered as lateral condylar torqueing/rotation with lateral ramal movement at the anterior osteotomy site. A decrease (negative change) in condylar angle in the axial slices was considered as medial condylar torqueing/rotation with medial ramal movement at the anterior osteotomy site.
Clinical Assessment of Temporomandibular Joint
Pain/tenderness, joint sounds like clicks, pops and crepitation, mouth opening, episodes of intermittent locking/dislocation, and deviation of TMJ were assessed preoperatively and postoperatively at intervals of 1, 3, 6, and 9 months, respectively.
Statistical Analysis
A paired sample t-test set at a significance level of 95% was carried out using SPSS statistics software version 25 which was performed for the postoperative condylar angle changes for each of the condyles in the 13 cases in the setback and advancement groups. Hence 26 condylar angle changes were measured in each group (setback and advancement), considering that two condylar angle changes (left and right) were possible, independently in each case.
Results
Mandibular Setback
The amount of setback ranged from 4 to 12 mm (mean 6.6 mm, SD 2.7 mm).
The preoperative condylar axial angle ranged from 53.8° to 86.4° (mean 74.9°, SD 7.5°). The postoperative condylar axial angle ranged from 54.8° to 86.1° (mean 74.6°, SD 7.3°). The condylar torquing ranged from 1.7° (medial) to 1.0° (lateral) for mandibular setback. The mean value was 0.2° (medial) (Table 1).
Table 1.
Mandibular setback (straight plate group)—condylar axial angles
| Condylar axial angle | N | Mean | SD | SE mean |
|---|---|---|---|---|
|
Preoperative Postoperative Amount of torquing |
26 26 26 |
74.8538 74.6577 0.1962 |
7.46535 7.25629 0.71804 |
1.46407 1.42308 0.14082 |
A mean medial condylar torquing of 0.2° was noted postoperatively. Using a paired sample t-Test, this change was not significant (p > 0.05) (Table 2).
Table 2.
Paired sample t-test: condylar axial angle changes (mandibular setback—straight plate group)
| 95% CI of the difference | ||||||||
|---|---|---|---|---|---|---|---|---|
| Pre-op vs Post-op |
Mean 0.19615 |
SD 0.71804 |
SE mean 0.14082 |
Lower -0.09387 |
Upper 0.48618 |
t 1.393 |
df 25 |
Significance (2-tailed) .176 |
Mandibular Advancement
The amount of mandibular advancement ranged from 4 to 13 mm (mean 6.0 mm, standard deviation 3.3 mm).
The preoperative condylar axial angle ranged from 61° to 90.7° (mean 70.5°, standard deviation 6.3°). The postoperative condylar axial angle ranged from 63.2 ° to 93.4° (mean 72.6°, standard deviation 6.4°). The condylar torquing ranged from 1.3° (lateral) to 2.9° (lateral). The mean value was 2.2° (lateral) (Table 3).
Table 3.
Mandibular advancement (Inset-bent plate group)—condylar axial angles
| Condylar axial angle | N | Mean | SD | SE mean |
|---|---|---|---|---|
|
Preoperative Postoperative Amount of torquing |
26 26 26 |
70.4692 72.6269 2.1577 |
6.28972 6.35613 0.47089 |
1.23352 1.24654 0.09235 |
A mean lateral condylar torquing of 2.2° was noted postoperatively. Using a paired sample t-Test, this change was highly significant (p < 0.001) (Table 4).
Table 4.
Paired sample t-test: condylar axial angle changes (mandibular advancement: inset-bent plate group)
| 95% CI of the difference | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Pre-op Vs Post-op |
Mean 2.15769 |
SD 0.47089 |
SE mean 0.09235 |
Lower − 2.34789 |
Upper − 1.96750 |
t − 23.364 |
df 25 |
Significance (2-tailed) .000 |
Temporomandibular Joint Symptoms
No TMJ clinical signs or symptoms were noted postoperatively during follow-up reviews at 1, 3, 6, and 9 months, respectively.
Discussion
The purpose of this prospective study was to evaluate the role and technique of plate fixation to minimize condylar torquing after BSSO setback and advancement using computed tomography.
The postoperative stability following BSSO depends on the osteotomy technique, amount and direction of surgical movement, type of fixation, soft tissue tension caused by surgical changes, occlusal stability, condylar displacement, amount of bone contact between the proximal and distal segments, and surgeon’s experience [7].
Good occlusal interdigitation and normal condylar position after orthognathic surgery are regarded as important factors in the prevention of postoperative relapse. These two factors are interdependent; abnormal interdigitation with normal condylar position can be controlled postoperatively by orthodontic treatment, but malpositioned condyles cannot be corrected postoperatively and eventually disrupt postoperative occlusal stability [8].
Influence of Mandibular Anatomy on Proximal and Distal Segment Contact/Gap
The mandible when viewed axially is convergent to the anterior. The sagittal cuts for the BSSO placed in the convergent body and ramus of the mandible are also convergent. As the distal segment is moved anteriorly, the contact between the distal and proximal segments flares the proximal segment. The most common point of contact is not posterosuperior but posteroinferior with symmetric advancements [9]. In the present paper, every effort was undertaken to eliminate any bony inferences or ‘high points’ along the contacting cortical surfaces of the proximal and distal segments to ensure a uniform contact area and prevent any excessive flare of the proximal segment on mandibular advancement.
In a submentovertex radiographic study of BSSO advancement, Hackney et al. [10] did not find any evidence that V-shaped mandibles with more divergent rami would produce larger increases in intercondylar width (ICW) when compared to U-shaped mandibles, when advanced. They concluded that fixation probably had more of an influence on condylar displacement than the direction, amount of surgical movement, or the shape of the mandible. Bony interferences or gaps between the proximal and distal segments can result in lateral displacement of the proximal segment, leading not only to relapse but also temporomandibular joint pain, clicks, disc displacement, and condylar resorption [10, 11].
This gap would be apparent at the posterior osteotomy site in case of mandibular setbacks and at the anterior osteotomy site in case of advancements. The maintenance of these gaps is the key to ensuring the preoperative condylar position. The greater the mandibular movement on setback or advancement, the larger the gaps. An attempt to close this gap, especially on mandibular advancement where the gap is present at the anterior vertical osteotomy, would result in lateral displacement of the ramus with medial rotation or torquing of the condyle within the glenoid fossa (Fig. 4).
Fig. 4.
The bony contacts and gaps between the segments after BSSO. The gap would be apparent in the posterior osteotomy site in case of mandibular setbacks and in the anterior osteotomy site in case of advancements
Role of Fixation
According to Ellis [12], displacement of the condyles medially or laterally within the mandibular fossa can occur when the proximal and distal segments are not passively positioned to one another during the application of internal fixation devices. If the surgeon forcefully closes a gap between the segments, the condyle will be displaced medially or laterally, depending on the location of the gap. Forcefully closing this gap is most often caused by surgical manipulation, the use of a bone clamp between the segments, or the use of lag screws.
Rigid internal fixation can induce condylar displacement more frequently than semi-rigid fixation during BSSO, especially inward condylar torque with lateral shifting, which can be clearly observed on axial plane images on immediate postoperative CT [13]. Mandibular advancement usually produces greater condylar displacement than mandibular setback if the anterior osteotomy gap is forcefully closed with rigid fixation [14]. Rigid fixation can cause a positional change of the condyle because fixation with screws tends to eliminate the gaps between the proximal and the distal segment, which are normally generated with mandibular movement in any direction [8]. If a condyle is rigidly held in a displaced postoperative position and that position places a load on the condyle or meniscal tissues or both, irreversible TMJ changes may occur [9].
To offset the effects of this anterior osteotomy closure, a bent titanium plate or bone graft at the anterior gap can be used to maintain the gap between the proximal and distal segments [14–17]. Periera et al. [18] described a ‘hybrid’ fixation technique using an inset-bent 4-hole miniplate with monocortical screws along with 2 bicortical positional screws posterior to the miniplate. In the present study, the lateral flare at the anterior osteotomy site was maintained using an inset-bent plate for fixation (Fig. 1). A mean lateral condylar torquing of 2.2 ° was noted postoperatively. This change was highly significant (p < 0.001).
In a study assessing the stability of the intersegmental space maintained with bone grafts after BSSO, Bettega et al. [19] reported that the patient group with bone graft showed more stable results 1 year after surgery compared to the non-grafted group. According to them, it was important to maintain a gap in the osteotomy site when placing the screw so as not to impose a torque constraint on the proximal osseous fragment. In a study by Kang et al. [20], bone fragments from the proximal segment were used in the intersegmental gap to reduce postoperative condylar displacement, facilitating the maintenance of the intersegmental space, stable segmental management, and easier fixation.
Lag screws in combination with position screws may also be used for fixation. When advancing the mandible, a lag screw can be used to stabilize the posterior natural contact area and a position screw fixed anteriorly through a bone graft maintaining the gap. In mandibular setbacks, the natural contact area is situated in the front; hence a lag screw can be fixed at that point. Fixing lag screws to the passive gaps between the proximal and distal segments may cause the proximal segment to torque medially in the case of advancements and laterally in case of setbacks [21].
Condylar Torquing with Plate and Monocortical Screw Fixation
Choi et al. [13], Roh et al. [22], Ueki et al. [23], and Yeo et al. [24] all found statistically significant medial torquing of the condylar angles of 1.3° (p < 0.05), 2.7° (p < 0.05), 5.2° (p < 0.05), and 1.7 ° (p < 0.001), respectively, after BSSO setback on axial images.
However, Katsumata et al. [25] found that rotation of the condylar long axes after BSSO setback was minimal (average 0) on axial CT. In the present study as well, a mean medial condylar torquing of 0.2° was noted postoperatively, which was not significant (p > 0.05). Xi et al. [26] found that the condyle torqued medially by 1° on axial images after BSSO advancement and LeFort I osteotomy, which was significant (p < 0.05).
None of these studies with monocortical screw fixation reported any postoperative TMJ symptoms in their study populations, who were assessed at periodic intervals from 3 months till 2 years. In the study by Ueki et al. [23], the authors also reported that preoperative TMJ symptoms of clicking, crepitus, and pain on mouth opening improved in 76.5% of 19 patients who underwent isolated BSSO setback procedures. Similarly, no temporomandibular clinical signs or symptoms were noted postoperatively (assessed at intervals of 1, 3, 6, and 9 months, respectively) in the present study as well.
Han et al. [27] found medial condylar torquing of 0.95 ° on axial images, after mandibular setback and LeFort I osteotomy with monocortical plate fixation, which was not significant (p > 0.05). In two other groups of patients in the same study, they used a ‘hybrid technique’ of monocortical plate fixation along with bicortical positional screws. The site and number of bicortical screws were determined intraoperatively to increase intersegmental stability in cases of small bone contact surface between the proximal and distal segments. In comparing the three different fixation techniques used in this study, the authors found that semi-rigid fixation using a miniplate allowed the recovery of condylar displacement better than the hybrid technique. However, with the hybrid technique, the condyle moved to its original position better with one bicortical positional screw than with two or three bicortical screws. They concluded that stronger rigid internal fixation in orthognathic surgery using BSSO was associated with reduced flexibility of postoperative functional adjustment of the displaced condyle to the preoperative condylar position. In their study, when the condyles were divided into symptomatic and non-symptomatic groups depending on the presence of postoperative TMJ symptoms, there was no significant difference between the two groups in the amount of condylar displacement and rotational movement 3–6 months after surgery. According to the authors, slight to mild postoperative intersegmental movement in terms of slippage between the proximal and distal segments as a result of the loosening of rigid fixation from muscle activity might be helpful for postoperative functional adjustment of the displaced condyle into the glenoid fossa, while maintaining the occlusion in a stable position without severe disturbance. They postulated that stronger rigid internal fixation was associated with reduced flexibility of the postoperative functional adjustment of displaced condyle to the preoperative condylar position or maintenance of stable occlusion.
Regarding stability of BSSO with the type of fixation used, a recent systemic review and meta-analysis study found that there was no statistically significant difference in skeletal stability between bicortical screw versus monocortical plate and screw fixation following mandibular setback or advancement [28, 29].
In the present study, a mean medial condylar/ramal torquing of 0.2° was noted postoperatively in case of mandibular setbacks. This change was not significant (p > 0.05) suggesting minimal condylar rotation. This indicated that the proximal and distal segments maintained their contact at the anterior vertical osteotomy which was fixed with a straight plate. However, in case of mandibular advancements, a mean lateral condylar/ramal torquing of 2.2° was noted postoperatively. This change was highly significant (p < 0.001). This suggested that the proximal segment ‘kicked out’ at the anterior vertical osteotomy site in mandibular advancement, and this gap was maintained by the inset-bent plate fixation technique.
Conclusion
The gaps between the proximal and distal segments created by mandibular advancement and setback should be maintained. This is especially imperative in case of mandibular advancements. An attempt to close this gap at the anterior vertical osteotomy in mandibular advancement by attempting to align the segments with a straight plate would result in lateral displacement of the ramus with medial rotation or torquing of the condyle within the glenoid fossa.
Consequently, the areas of bony contact between the proximal and distal osteotomy sites created by mandibular advancement and setback should be maintained as well.
Temporomandibular joint function as well as occlusal adjustment is better suited to adapt with semi-rigid fixation of the BSSO segments postoperatively.
Acknowledgment
Line diagram courtesy of Dr Vidya Devi, MDS (OMFS). E- mail: vidya.devi.vuyyuru@gmail.com
Author contributions
All authors contributed to the study conception and design. TZ performed material preparation, analysis and interpretation of data; RBK helped in the acquisition of data; MR and AP revised it critically for important intellectual content and made substantial contributions to the conception and design of the work. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
Funding
No funding was received for this study.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.”
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Epker BN, Wylie GA. Control of the condylar-proximal mandibular segments after sagittal split osteotomies to advance the mandible. Oral Surg Oral Med Oral Pathol. 1986;62(6):613–617. doi: 10.1016/0030-4220(86)90251-3. [DOI] [PubMed] [Google Scholar]
- 2.Rotskoff KS, Herbosa EG, Nickels B. Correction of condylar displacement following intraoral vertical ramus osteotomy. J Oral Maxillofac Surg. 1991;49(4):366–374. doi: 10.1016/0278-2391(91)90372-S. [DOI] [PubMed] [Google Scholar]
- 3.Tornes K, Gilhuus-Moe O, McCallum CA, Jr, Wisth PJ. Positioning and mobility of the mandibular condyle after surgical correction of the asymmetric, prognathic mandible. Int J Adult Orthodon Orthognath Surg. 1990;5(1):29–34. [PubMed] [Google Scholar]
- 4.Hwang SJ, Haers PE, Sailer HF. The role of a posteriorly inclined condylar neck in condylar resorption after orthognathic surgery. J Craniomaxillofac Surg. 2000;28(2):85–90. doi: 10.1054/jcms.2000.0129. [DOI] [PubMed] [Google Scholar]
- 5.Hoppenreijs TJ, Stoelinga PJ, Grace KL, Robben CM. Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery. Int J Oral Maxillofac Surg. 1999;28(6):411–418. doi: 10.1016/S0901-5027(99)80052-6. [DOI] [PubMed] [Google Scholar]
- 6.Wolford LM, Bennett MA, Rafferty CG. Modification of the mandibular ramus sagittal split osteotomy. Oral Surg Oral Med Oral Pathol. 1987;64(2):146–155. doi: 10.1016/0030-4220(87)90080-6. [DOI] [PubMed] [Google Scholar]
- 7.Yang HJ, Hwang SJ. Evaluation of postoperative stability after BSSRO to correct facial asymmetry depending on the amount of bone contact between the proximal and distal segment. J Craniomaxillofac Surg. 2014;42(5):e165–e170. doi: 10.1016/j.jcms.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Lee W, Park JU. Three-dimensional evaluation of positional change of the condyle after mandibular setback by means of bilateral sagittal split ramus osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(3):305–309. doi: 10.1067/moe.2002.126452. [DOI] [PubMed] [Google Scholar]
- 9.Arnett GW. Temporomandibular joint ramifications of orthognathic surgery. Modern Pract Orthognath Reconstr Surg. 1992;1:522–593. [Google Scholar]
- 10.Hackney FL, Van Sickels JE, Nummikoski PV. Condylar displacement and temporomandibular joint dysfunction following bilateral sagittal split osteotomy and rigid fixation. J Oral Maxillofac Surg. 1989;47(3):223–227. doi: 10.1016/0278-2391(89)90221-8. [DOI] [PubMed] [Google Scholar]
- 11.Harris MD, Van Sickels JE, Alder M. Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. J Oral Maxillofac Surg. 1999;57(6):650–655. doi: 10.1016/S0278-2391(99)90422-6. [DOI] [PubMed] [Google Scholar]
- 12.Ellis E., 3rd A method to passively align the sagittal ramus osteotomy segments. J Oral Maxillofac Surg. 2007;65(10):2125–2130. doi: 10.1016/j.joms.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 13.Choi BJ, Choi YH, Lee BS, Kwon YD, Choo YJ, Ohe JY. A CBCT study on positional change in mandibular condyle according to metallic anchorage methods in skeletal class III patients after orthognatic surgery. J Craniomaxillofac Surg. 2014;42(8):1617–1622. doi: 10.1016/j.jcms.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Ueki K, Nakagawa K, Takatsuka S, Yamamoto E. Plate fixation after mandibular osteotomy. Int J Oral Maxillofac Surg. 2001;30(6):490–496. doi: 10.1054/ijom.2001.0171. [DOI] [PubMed] [Google Scholar]
- 15.Ueki K, Degerliyurt K, Hashiba Y, Marukawa K, Nakagawa K, Yamamoto E. Horizontal changes in the condylar head after sagittal split ramus osteotomy with bent plate fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(5):656–661. doi: 10.1016/j.tripleo.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Ueki K, Hashiba Y, Marukawa K, et al. Evaluation of bone formation after sagittal split ramus osteotomy with bent plate fixation using computed tomography. J Oral Maxillofac Surg. 2009;67(5):1062–1068. doi: 10.1016/j.joms.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Ueki K, Moroi A, Sotobori M, et al. Changes in temporomandibular joint and ramus after sagittal split ramus osteotomy in mandibular prognathism patients with and without asymmetry. J Craniomaxillofac Surg. 2012;40(8):821–827. doi: 10.1016/j.jcms.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Pereira FL, Janson M, Sant'Ana E. Hybrid fixation in the bilateral sagittal split osteotomy for lower jaw advancement. J Appl Oral Sci. 2010;18(1):92–99. doi: 10.1590/S1678-77572010000100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bettega G, Cinquin P, Lebeau J, Raphaël B. Computer-assisted orthognathic surgery: clinical evaluation of a mandibular condyle repositioning system. J Oral Maxillofac Surg. 2002;60(1):27–35. doi: 10.1053/joms.2002.29069. [DOI] [PubMed] [Google Scholar]
- 20.Kang MG, Yun KI, Kim CH, Park JU. Postoperative condylar position by sagittal split ramus osteotomy with and without bone graft. J Oral Maxillofac Surg. 2010;68(9):2058–2064. doi: 10.1016/j.joms.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Ehrenfeld M, Manson PN, Prein J. 7.2 Standard osteotomies in the mandible. In: Ehrenfeld M, Manson PN, Prein J, editors. Principles of internal fixation of the craniomaxillofacial skeleton trauma and orthognathic surgery. New York: Thieme; 2012. p. 342. [Google Scholar]
- 22.Roh YC, Shin SH, Kim SS, Sandor GK, Kim YD. Skeletal stability and condylar position related to fixation method following mandibular setback with bilateral sagittal split ramus osteotomy. J Craniomaxillofac Surg. 2014;42(8):1958–1963. doi: 10.1016/j.jcms.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 23.Ueki K, Marukawa K, Nakagawa K, Yamamoto E. Condylar and temporomandibular joint disc positions after mandibular osteotomy for prognathism. J Oral Maxillofac Surg. 2002;60(12):1424–1434. doi: 10.1053/joms.2002.36098. [DOI] [PubMed] [Google Scholar]
- 24.Yeo BR, Han JJ, Jung S, Park HJ, Oh HK, Kook MS. Horizontal changes of the proximal mandibular segment after mandibular setback surgery using 3-dimensional computed tomography data. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(1):14–19. doi: 10.1016/j.oooo.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Katsumata A, Nojiri M, Fujishita M, Ariji Y, Ariji E, Langlais RP. Condylar head remodeling following mandibular setback osteotomy for prognathism: a comparativestudy of different imaging modalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(4):505–514. doi: 10.1016/j.tripleo.2005.07.028. [DOI] [PubMed] [Google Scholar]
- 26.Xi T, van Luijn R, Baan F, et al. Three-dimensional analysis of condylar remodeling and skeletal relapse following bimaxillary surgery: a 2-year follow-up study. J Craniomaxillofac Surg. 2017;45(8):1311–1318. doi: 10.1016/j.jcms.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Han JJ, Hwang SJ. Three-dimensional analysis of postoperative returning movement of perioperative condylar displacement after bilateral sagittal split ramus osteotomy for mandibular setback with different fixation methods. J Craniomaxillofac Surg. 2015;43(9):1918–1925. doi: 10.1016/j.jcms.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 28.Al-Moraissi EA, Ellis E. Stability of bicortical screw versus plate fixation after mandibular setback with the bilateral sagittal split osteotomy: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016;45(1):1–7. doi: 10.1016/j.ijom.2015.09.017. [DOI] [PubMed] [Google Scholar]
- 29.Al-Moraissi EA, Al-Hendi EA. Are bicortical screw and plate osteosynthesis techniques equal in providing skeletal stability with the bilateral sagittal split osteotomy when used for mandibular advancement surgery? A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2016;45(10):1195–1200. doi: 10.1016/j.ijom.2016.04.021. [DOI] [PubMed] [Google Scholar]