Abstract
The purpose of this study was to examine the effectiveness and feasibility of translating a 4-week “Stand Up and Move More” (SUMM) intervention by State Aging Units to older adults (N=56, mean age=74yrs). A randomized controlled trial assessed sedentary behavior, physical function, and health-related quality of life (HRQoL) before and after the intervention. Participants included healthy community-dwelling, sedentary (sit > 6 hrs/day) and aged ≥ 55yrs adults. For the primary outcome, the SUMM group (n=31) significantly (p < .05) reduced total sedentary time post-intervention by 68 minutes/day on average (Cohen’s d=−0.56) compared to no change in the wait-list control group (n=25; Cohen’s d=0.12). HRQoL and function also improved (p < .05) in the SUMM group post-intervention. Workshop facilitators indicated the intervention was easy to implement, and participants expressed high satisfaction. The SUMM intervention reduced sedentary time, improved physical function and HRQoL, and was feasible to implement in community settings.
INTRODUCTION
Adults over the age of 65 years represent the fastest growing segment of our global population. In fact, the older adult population is expected to more than double by 2050 and more than triple by 2100 (Manini, 2011). Given that aging is associated with complex health issues that often lead to functional decline, it is crucial to preserve functional performance in later life in order to maintain independence, enhance quality of life, and reduce health care costs (Semanik et al., 2015). Unfortunately, older adults spend approximately 60% - 70% of their waking hours engaging in sedentary activities (i.e., prolonged sitting), which significantly increases their risk of functional decline and other negative health outcomes (e.g., chronic disease development, premature mortality, obesity; Matthews et al., 2008; Copeland et al., 2017; Keadle et al., 2015; de Rezende et al., 2014).
Exercise has been shown to be effective for preventing functional decline, but older adults tend to report low levels of exercise, i.e., less than 7% meet current World Health Organization (WHO) recommendations of at least 150 minutes per week of moderate-intensity aerobic exercise (Matthews et al., 2008). Emerging research with older adults suggests that more frequent breaks in sedentary time are associated with better overall health and physical function (Copeland et al., 2017; Sardinha et al., 2015; Yasunga et al., 2017; Gennuso et al., 2016). Therefore, interventions aimed at breaking up sedentary time by standing up and moving more throughout the day may be an effective and feasible approach to improve health, particularly for older adults with existing limitations who may not be exercising to the extent recommended by WHO. However, little research has been conducted with older adults examining interventions designed to reduce sedentary behavior compared to the more traditional intervention of increasing exercise (Gardiner et al., 2013; Fitzsimmons et al., 2013; Rosenberg et al., 2015; Lewis et al., 2016; Kerr et al., 2016; Maher et al., 2017). Thus, there is a need for additional research, especially research examining interventions that can be successfully disseminated into community settings to benefit sedentary older adults.
Implementation of evidence-based programs in real-world community settings has the potential to improve the health and functioning of a wide range of older adults. Through collaboration between researchers from the University of Wisconsin-Madison and the Community-Academic Aging Research Network (CAARN), a behavior change intervention was designed to help older adults reduce sedentary behavior through breaking up prolonged sitting by standing up and moving multiple times throughout the day. The intervention was developed to target the benefits of small increases in standing up and moving throughout the day and was based on research indicating benefits of increasing activity in the low-moderate end of the physical activity spectrum. The intervention, offered as a once per week, 4-week small group workshop (with a refresher session four weeks after the last session), was designed to be administered by trained facilitators to older adults in their communities. A curriculum manual was developed and, with funding from the Greater Wisconsin Agency on Aging Resources, the intervention was then pilot-tested in collaboration with our community partner, the director of the Rock County Council on Aging, in two small urban and rural communities. Results indicated that sedentary behavior was significantly reduced by 60 minutes/day, and there were moderately large effect size improvements in physical function and vitality in older adults after participating in the workshop (Koltyn et al., 2019). These results provided preliminary evidence that the behavior change intervention was effective in reducing sedentary behavior in a small sample of community-dwelling older adults. Therefore, to expand upon these promising results, the next step was to examine the effectiveness and feasibility of implementation of the “Stand Up and Move More” intervention by State Aging Units for sedentary older adults in multiple small urban and rural communities.
METHODS
The study was approved by the UW-Madison Social and Behavioral IRB Committee. The work described in this manuscript was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans, and all participants completed written informed consent. See Crombie et al. for a complete description of the methods and study protocol (Crombie et al., 2019).
Participants and Intervention to Reduce Sedentary Behavior
Participants were recruited by health promotion coordinators from State Aging Units in various communities within three counties in Wisconsin. Recruitment strategies included announcements in senior newsletters, and flyers posted at congregate dining sites, churches, libraries, and grocery stores. In addition, announcements were posted on State Aging Unit websites, and flyers were sent to mailing lists of older adults in various communities (see supplementary material for additional information regarding participant recruitment and power analysis calculation indicating a targeted sample size of 34 participants per group).
In order to participate in this study, participants had to be healthy community-dwelling (i.e., residing in a home or apartment), sedentary (i.e., sit more than 6 hrs per day), and aged 55 years and older. Interested and eligible participants were randomly assigned to either the “Stand Up and Move More” intervention group or a wait-list control group (See supplementary material and study protocol manuscript for additional information on participant randomization (Crombie et al., 2019). The intervention consisted of 4 weekly small-group workshop sessions (1 to 1 ½ hours) with a refresher session four weeks after the last workshop session. The sessions were facilitated by community partners in each county who regularly offer health promotion programs to older adults. Prior to the start of the workshops, the facilitators attended a 6-hour training session in which they learned about and practiced delivering the “Stand Up and Move More” curriculum. The intervention was based on self-regulation and social cognitive theories with sessions designed to provide information on sedentary behavior, elicit ideas from older adults regarding how they could reduce their sitting time, help them set practical and individualized goals, develop action plans to reach their goals, and refine their plans across sessions to promote behavior change. The facilitators were provided with a curriculum binder providing scripts, hand-outs, key points to emphasize, and questions for discussion for each session (see supplementary material for overview of the weekly sessions). Between workshop sessions, participants were asked to break up bouts of prolonged sitting (> 1 hour) with short breaks; specifically, they were asked to break up sitting time an extra 3 to 5 times/day during the first week of the intervention progressing to 10 to 12 times/day by the end of the four-week intervention. Participants self-monitored their activity by using a small click counter every time they stood up and completed a daily log at the end of each day throughout the study.
Participants randomly assigned to the waitlist control condition were asked to go about their daily routines during the first 12 weeks of the study. They completed assessments in the same manner as the intervention group (see below) and received the “Stand Up and Move More” intervention shortly after completing their last assessment visit (Crombie et al., 2019).
Assessments
Assessments were conducted one week prior to the first workshop session (at an introductory meeting), post-intervention (i.e., at 4 weeks after start of intervention), and at follow-up (i.e., at 8 weeks following completion of intervention). The primary outcome of interest was activity-monitor derived sedentary behavior (total minutes/day) obtained from accelerometers (ActiGraph; WGT3X-BT; ActiGraph LLC, Fort Walton Beach, FL, USA) and inclinometers (activPAL; PAL Technologies LTD, Glascow, UK). Secondary outcomes of interest included additional sedentary behavior and physical activity outcomes (e.g., self-reported sedentary time, average sedentary bout duration, number of sit-to-stand transitions, time spent engaging in light- and moderate-intensity physical activity), physical function, health-related quality of life, and pain intensity and interference.
Participants wore the monitors during waking hours for a one-week period during all data collection time points. The activPAL is a small (matchbook sized) inclinometer used to measure horizontal/vertical position of the device, and thus posture. The device was affixed directly to the midline of the thigh of the participant with a temporary hypoallergenic adhesive. This device measured time spent in sedentary behavior and the number of times sedentary behavior was disrupted by standing up. The ActiGraph monitor recorded the frequency of accelerations during ambulatory activities and thus quantified physical activity across the entire spectrum (light intensity, moderate intensity, and vigorous intensity physical activity; Note: vigorous-intensity physical activity was not included in analyses due to low baseline levels). Data were first downloaded by ActiLife (ActiGraph, LLC, Pensacola, FL) and activPAL (PAL Technologies LTD, Glascow, UK) software and then processed via the Sojourns Including Posture method (Ellingson et al., 2016). Additionally, participants were interviewed by research staff about their time spent engaging in different sedentary activities over the past week using a previously validated questionnaire for older adults (Gardiner et al., 2011). Physical function was assessed with the Short Physical Performance Battery (SPPB; Guralnik et al., 1994) consisting of a balance test, a 4-meter walk for usual gait speed, and a timed five-repetition sit-to-stand chair test. Additionally, at the introductory session (i.e., pre-intervention), participants completed a questionnaire assessing health status and demographic information (i.e., age, sex, race, ethnicity, education, income, occupational status, and marital status), current physical activity behaviors, smoking status, current alcohol intake, and present or past history of various health conditions (e.g., cancer, diabetes, arthritis, stroke). At all assessment time points (pre- and post-intervention and follow-up), participants completed a packet of questionnaires assessing health-related quality of life (SF-36; Ware & Sherbourne, 1992; subscales include: general health, vitality, social functioning, mental health, physical functioning, bodily pain, and role limitations due to physical and emotional health), the presence or absence of sarcopenia (SARC-F; Malmstrom et al., 2016), pain intensity and interference (PROMIS-pain; Deyo et al., 2016), and mediators of behavior change, including: self-regulation strategies (Umstattd et al., 2009), self-efficacy (Marcus et al., 1992), outcome expectancies (Resnick et al., 2000), and habit strength (Verplanken & Orbell, 2003) (Note: the SARC-F and mediators of behavior change outcomes are the focus of a subsequent manuscript).
Feasibility of older adults completing the “Stand Up and Move More” workshop was assessed by adherence to the program and a facilitator-led group satisfaction discussion immediately post-intervention in which they were asked if they found the workshop to be beneficial and what they liked and disliked about the workshop. To assess the feasibility of delivering the intervention in a community setting, the workshop facilitators completed a feedback survey developed for this project. Facilitators were asked to rate four items (i.e., clarity of content in the leader manual; ease of implementation of the workshop; attendance rates; and access to resources) on 1–5 Likert scale with 1=needs improvement, 2=fair, 3=good, 4=very good, and 5=excellent. A fifth item asked about overall satisfaction with the workshop and was rated on the following scale: 1=very dissatisfied, 2=somewhat dissatisfied, 3=neutral, 4=satisfied, 5=very satisfied. Also, the survey provided space for the facilitators to write additional comments. Further, feasibility of implementing the workshop was discussed at a wrap-up meeting for the facilitators and researchers after the workshop ended. Fidelity of delivery of the curriculum was assessed by a Community Research Associate with CAARN who traveled to each site and observed a workshop session, documented fidelity, and provided feedback to each of the health promotion coordinators leading the workshops. Adverse events were monitored at the beginning of each workshop session through a safety questionnaire. Workshop facilitators discussed any safety concerns with the participants and reported them to the research team.
Statistical Analyses
A series of one-way ANOVAs (for parametric data) and Pearson’s chi-squared tests (for categorical data) were conducted in order to detect the presence of group differences in baseline variables (see Table 1 for means, standard deviations, frequencies, and percentages). Changes in sedentary behaviors, physical activity levels, physical function, health-related quality of life, and pain intensity and interference between and within groups were analyzed using a series of 2 (group) x 3 (time) mixed-design repeated measures ANOVAs (see Tables 2 and 3 for means, standard deviations, and effect sizes). The overall alpha familywise was set at α=0.05. Following Fisher’s LSD procedures, if the initial ANOVA yielded a significant interaction, simple effects were calculated for all pairwise comparisons. Effect sizes (Cohen’s d) were calculated to examine the magnitude of differences between groups as well as the magnitude (small [d=0.20 to 0.49; moderate [d=0.50 to 0.79]; large [d ≥ 0.80]) of change throughout the intervention (Cohen, 1988). All analyses were by intention-to-treat. All analyses were conducted with SPSS Version 25.0 for Windows.
Table 1.
Participant Characteristics
| Control (n=25) | Intervention (n=31) | |
|---|---|---|
|
| ||
| Age (years; M ± SD) | 72.8 ± 6.5 | 75.0 ± 7.7 |
| Sex (# of women, % of sample) | 23 (92) | 26 (84) |
| Height (cm; M ± SD) | 165.0 ± 6.3 | 163.1 ± 9.2 |
| Weight (kg; M ± SD) | 94.0 ± 20.2 | 83.3 ± 20.1 |
| Body mass index (BMI; kg/m2; M ± SD) | 34.6 ± 7.6 | 31.7 ± 7.7 |
| Race (#, % Caucasian) | 25 (100) | 31 (100) |
| Ethnicity (#, % non-Hispanic or Latino) | 25 (100) | 31 (100) |
| Marital status | ||
| Single (#, %) | 1 (4) | 2 (6.5) |
| Married (#, %) | 3 (12) | 15 (48) |
| Divorced (#, %) | 12 (48) | 2 (6.5) |
| Widowed (#, %) | 9 (36) | 12 (39) |
| Educational Attainment (% with college degree) | 12 (48) | 19 (61) |
| Overall Health (self-reported) | ||
| Excellent (#, %) | 1 (4) | 0 (0) |
| Very good (#, %) | 6 (24) | 15 (48) |
| Good (#, %) | 12 (48) | 12 (39) |
| Fair (#, %) | 6 (24) | 4 (13) |
| Poor (#, %) | 0 (0) | 0 (0) |
| Health History (#, % reporting yes) | ||
| High blood pressure | 17 (68) | 17 (55) |
| Cardiovascular disease | 2 (8) | 4 (13) |
| Diabetes | 11 (44) | 7 (23) |
| Stroke | 0 (0) | 0 (0) |
| Past heart problems | 4 (16) | 6 (19) |
| Cancer | 4 (16) | 10 (32) |
| Arthritis | 15 (60) | 20 (65) |
| Hip/knee replacement | 4 (16) | 7 (23) |
Note. M = mean; SD = standard deviation; kg/m2 = kilograms per square meter
Table 2.
Means, standard deviations, and effect sizes for sedentary behavior and physical activity outcomes at pre- and post-intervention and follow-up
| Means and Standard Deviations | Effect Sizes | ||||
|---|---|---|---|---|---|
|
|
|||||
| Pre-Intervention | Post-Intervention | Follow-Up | Pre to Post | Pre to Follow-up | |
|
|
|||||
| Outcomes | M ± SD | M ± SD | M ± SD | Cohen’s d | Cohen’s d |
|
| |||||
| Sedentary mins/day (monitor derived) | |||||
| Control | 627.16 ± 139.11 | 643.66 ± 133.12 | 616.99 ± 119.72 | 0.12 | −0.08 |
| Intervention | 619.75 ± 125.65 | 551.39 ± 120.51* | 602.12 ± 116.16 | −0.56 | −0.15 |
| Sedentary mins/day (self-reported) | |||||
| Control | 606.07 ± 124.34 | 536.97 ± 134.27# | 520.09 ± 143.62 | −0.53 | −0.64 |
| Intervention | 582.66 ± 144.81 | 441.26 ± 138.84# | 391.55 ± 142.98# | −1.00 | −1.33 |
| Average sedentary bout duration | |||||
| Control | 64.11 ± 43.40 | 65.09 ± 41.89 | 59.12 ± 33.45 | 0.02 | −0.13 |
| Intervention | 63.58 ± 27.54 | 55.08 ± 35.48 | 52.59 ± 21.48 | −0.27 | −0.49 |
| Sit-to-stand transitions | |||||
| Control | 38.08 ± 9.70 | 39.81 ± 12.70 | 39.00 ± 12.76 | 0.15 | 0.08 |
| Intervention | 37.96 ± 9.57 | 39.71 ± 16.19 | 46.40 ± 20.16 | 0.14 | 0.57 |
| Sedentary bouts of ≥ 60 min | |||||
| Control | 240.18 ± 136.61 | 246.86 ± 123.32 | 226.12 ± 147.83 | 0.05 | −0.09 |
| Intervention | 255.54 ± 133.04 | 191.77 ± 104.30 | 211.33 ± 119.31 | −0.54 | −0.35 |
| Light-intensity PA mins/day | |||||
| Control | 199.32 ± 116.25 | 191.41 ± 95.91 | 107.76 ± 172.95 | −0.07 | −0.63 |
| Intervention | 198.57 ± 119.10 | 222.96 ± 116.03 | 165.64 ± 101.20 | 0.21 | −0.30 |
| Moderate-intensity PA mins/day | |||||
| Control | 33.49 ± 13.90 | 35.68 ± 16.32 | 34.57 ± 17.52 | 0.14 | 0.07 |
| Intervention | 37.61 ± 24.07 | 43.20 ± 29.22 | 47.79 ± 46.16 | 0.21 | 0.29 |
Note. Effect sizes are derived from within-group calculations. PA = physical activity. Sedentary behavior and physical activity data listed above was derived from activity monitors (i.e., accelerometers/inclinometers) with the exception of self-reported sedentary mins/day obtained via an interview (Gardiner et al., 2011).
indicates significant (p < .05) group x time interaction. The intervention group significantly decreased their total sedentary minutes per day (monitor-derived) from pre- to post-intervention in comparison to the control group.
indicates significant (p < .05) group x time interaction. The intervention and control group reported significant reductions in self-reported sedentary minutes per day from pre- to post-intervention, with an additional significant decrease from post-intervention to follow-up for the intervention group.
Table 3.
Means, standard deviations, and effect sizes for SF-36 (health-related quality of life), pain intensity, and pain interference outcomes
| Means and Standard Deviations | Effect Sizes | ||||
|---|---|---|---|---|---|
|
|
|||||
| Pre-Intervention | Post-Intervention | Follow-Up | Pre to Post | Pre to Follow-up | |
|
|
|||||
| Outcomes | M ± SD | M ± SD | M ± SD | Cohen’s d | Cohen’s d |
|
| |||||
| General Health | |||||
| Control | 64.73 ± 17.64 | 61.91 ± 18.14 | 61.00 ± 19.43 | −0.15 | −0.20 |
| Intervention | 71.10 ± 11.57 | 76.97 ± 11.71* | 74.45 ± 14.15* | 0.50 | 0.26 |
| Vitality | |||||
| Control | 53.00 ± 18.76 | 52.00 ± 17.47 | 52.75 ± 20.74 | −0.05 | −0.01 |
| Intervention | 54.96 ± 21.02 | 64.44 ± 16.71* | 65.95 ± 17.96* | 0.50 | 0.56 |
| Social Functioning | |||||
| Control | 80.00 ± 21.04 | 78.50 ± 22.10 | 77.00 ± 24.39 | −0.07 | −0.13 |
| Intervention | 81.90 ± 26.43 | 82.33 ± 26.63 | 83.62 ± 26.75 | 0.02 | 0.06 |
| Mental Health | |||||
| Control | 71.80 ± 18.42 | 74.20 ± 16.69 | 75.60 ± 17.64 | 0.14 | 0.21 |
| Intervention | 77.83 ± 16.38 | 83.00 ± 11.64 | 81.83 ± 13.03 | 0.37 | 0.27 |
| Physical Functioning | |||||
| Control | 52.89 ± 22.75 | 58.16 ± 23.82 | 57.63 ± 23.06 | 0.23 | 0.21 |
| Intervention | 64.79 ± 14.56 | 68.13 ± 18.81 | 67.08 ± 20.95 | 0.20 | 0.13 |
| Bodily Pain | |||||
| Control | 61.38 ± 21.21 | 58.38 ± 26.56 | 60.04 ± 28.08 | −0.13 | −0.05 |
| Intervention | 62.86 ± 23.70 | 67.60 ± 23.38 | 63.10 ± 26.06 | 0.20 | 0.00 |
| Role Limitations - Physical | |||||
| Control | 59.09 ± 25.50 | 53.69 ± 23.52 | 59.94 ± 26.84 | −0.23 | 0.03 |
| Intervention | 62.50 ± 23.33 | 75.22 ± 22.99* | 73.49 ± 26.86* | 0.55 | 0.44 |
| Role Limitations - Emotional | |||||
| Control | 75.69 ± 26.78 | 68.75 ± 28.58 | 71.53 ± 26.57 | −0.25 | −0.16 |
| Intervention | 76.11 ± 26.78 | 84.72 ± 20.07* | 83.89 ± 23.46* | 0.37 | 0.29 |
| Pain Intensity | |||||
| Control | 2.46 ± 0.52 | 2.62 ± 0.77 | 2.08 ± 0.86 | 0.24 | 0.53 |
| Intervention | 2.31 ± 0.12 | 1.75 ± 0.68* | 2.25 ± 0.58 | −1.15 | 0.14 |
| Pain Interference | |||||
| Control | 9.23 ± 3.85 | 11.77 ± 4.02 | 8.85 ± 3.85 | 0.65 | −0.10 |
| Intervention | 9.63 ± 4.27 | 8.06 ± 2.86* | 9.63 ± 1.18 | −0.43 | 0.00 |
Note. Higher health-related quality of life (SF-36) scores indicate better health outcomes. Lower pain intensity and pain interference scores indicate less pain. Effect sizes are derived from within-group calculations.
indicates significant (p < .05) group x time interaction. The intervention group reported significant improvements in vitality and general health and fewer role limitations due to physical or emotional health from pre- to post-intervention compared to no significant change in the control group. Significant improvements in the intervention group were still present at follow-up. Additionally, the intervention group reported significant reductions in pain intensity and pain interference from pre- to post-intervention compared to a significant increase in pain interference and no change in pain intensity from pre- to post-intervention for the control group.
RESULTS
Participant Characteristics
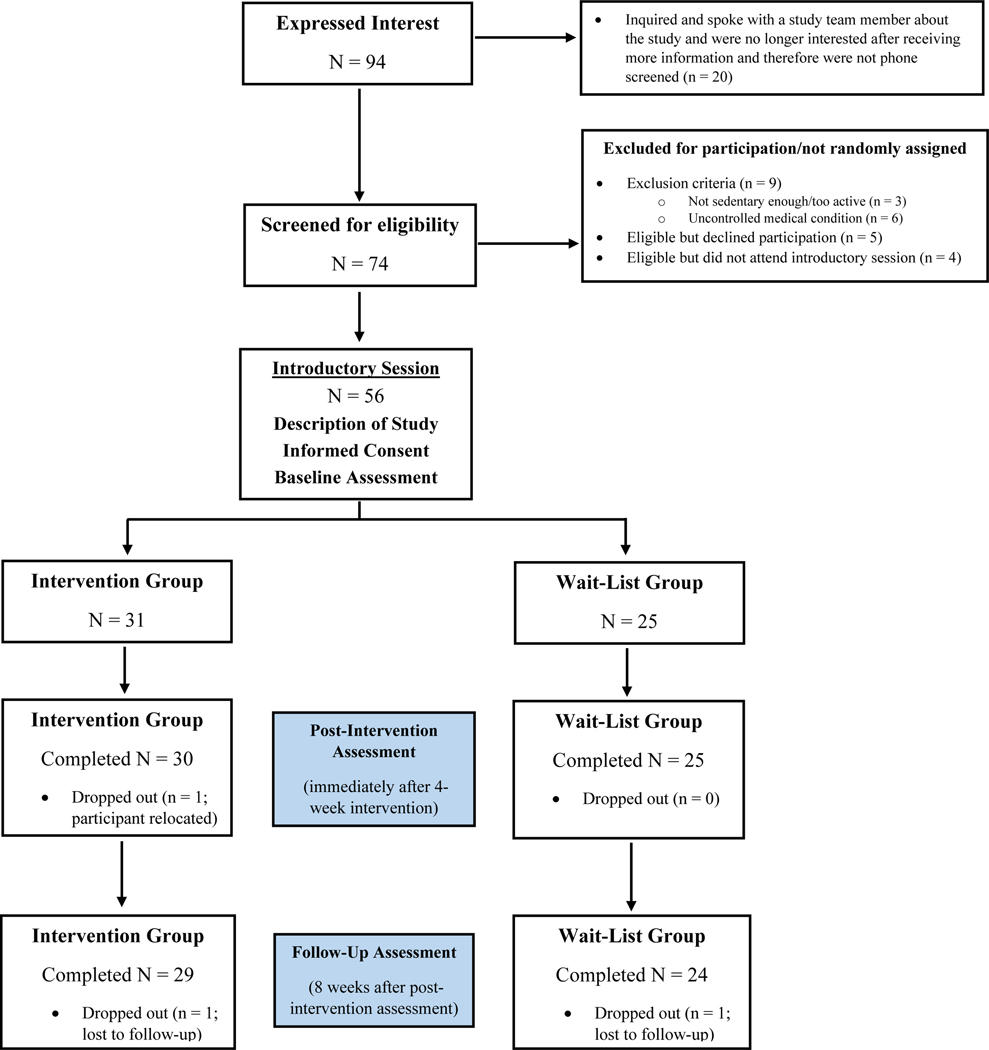
Seventy-four adults from three counties were screened for eligibility. Fifty-six adults meeting inclusion criteria were randomly assigned to the intervention (n = 31) or wait-list control (n = 25) groups, with 53 participants (mean age = 74 years) completing the study (intervention group n = 29, wait-list control n = 24; participant relocation n = 1, participants lost to follow-up n = 2; see Figure 1). At baseline, participants spent on average more than 10 hours/day in sedentary behavior (as assessed via activity monitors). The average duration of sitting bouts was 64 minutes. Based on sedentary behavior interviews, both groups spent the majority of their time watching TV, followed by using the computer/internet, and reading (see Supplementary Table 1). There were no significant (p > .05) group differences in baseline characteristics of interest (i.e., age, sex, or body mass index; see Table 1 for complete summary of participant characteristics).
Figure 1.
Consort diagram depicting enrollment of subjects, allocation to treatment, and participant completion at post-intervention and follow-up.
Sedentary Behavior
Descriptive data for sedentary behavior and physical activity are summarized in Table 2. There were no significant (p > .05) group differences for average monitor wear time (minutes/day) throughout the intervention (intervention mean = 841.73, sd = 76.94; control mean = 855.45, sd = 85.09), indicating that both groups wore the monitors for the same amount of time during the assessments. For the primary outcome of monitor-derived total sedentary minutes/day, there was a significant group x time interaction (F2,92 = 3.97, p = .022). Analysis of simple effects indicated that in comparison to the control group, the intervention group significantly decreased their total sedentary minutes per day from pre- to immediately post-intervention. The decrease in total sedentary time for the intervention group averaged 68 minutes/day (d=−0.56, moderate effect size decrease), in contrast to the control group which increased their sedentary time by 16 minutes/day (d=0.12, very small effect size increase; see Table 2). There were no significant group differences in total sedentary minutes per day at follow-up. Regarding self-reported sedentary behavior (minutes/day), there was also a significant group x time interaction (F2,104 = 5.55, p = .005), as both groups reported significant decreases from pre- to post-intervention with the intervention group reporting an additional reduction in sedentary behavior at follow-up compared to the control group. Summary data pertaining to secondary sedentary behavior and physical activity outcomes (e.g., self-reported sedentary time, average sedentary bout duration, number of sit-to-stand transitions, time spent engaging in light- and moderate-intensity physical activity) is shown in Table 2. Participants reported using a variety of strategies to reduce sedentary behavior. The strategies used most often included standing up during TV commercials, spreading household chores out across the day, placing reminders around the house, and standing up while quilting, sewing, reading, working on puzzles, talking on the phone, and paying bills.
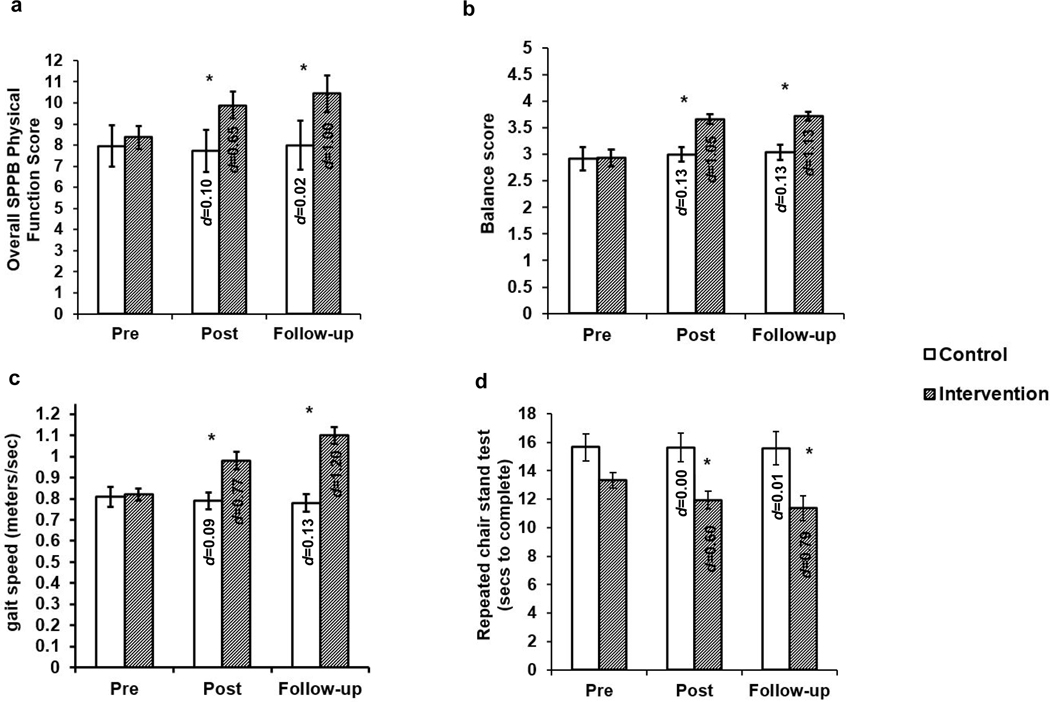
Physical Function
There were significant group x time interactions for balance (F2,102 = 4.95, p = .009), gait speed (meters per second; F2,102 = 18.47, p < 0.001), chair stands (time to complete five chair stands; F2,90 = 4.15, p = .019), and overall physical function (total SPPB score; F2,104 = 10.61, p < 0.001; see Figure 2). Specifically, the intervention group significantly (all ps < .001) improved their balance (d=1.05, large effect size improvement), gait speed (d=0.77, moderate effect size improvement), chair stands (d=0.60, moderate effect size improvement), and overall physical function score (d=0.65, moderate effect size improvement) from pre- to immediately post-intervention compared to no significant (ps = .432 to .977) change in the control group (see Figure 2). These functional improvements in the intervention group were maintained over time as significant (all ps < .001) improvements in balance (d=1.13, large effect size improvement), gait speed (d=1.20, large effect size improvement), chair stands (d=0.79, moderate effect size improvement), and overall physical function score (d=1.00, large effect size improvement) were still present at follow-up.
Figure 2.
Physical function outcomes prior to and following the sedentary behavior intervention for wait-list control and intervention groups. a) = overall physical function score; b) = balance score; c) = gait speed in meters per second; d) = repeated chair stand test (i.e., seconds to complete). *= significant group x time interaction. Physical function data was obtained from administration of the Short Physical Performance Battery (SPPB). Cohen’s d effect sizes (within-group) from pre- to post-intervention and pre-intervention to follow-up are included in the bar graphs (i.e., value listed in post bar graph is the within group effect size from pre- to post-intervention, and value listed in the follow-up bar graph is the within-group effect size from pre-intervention to follow-up).
Health-related Quality of Life
There were significant group x time interactions for vitality (F2,104 = 5.34, p = .006), general health (F2,98 = 3.80, p = .026), and role limitations due to physical (F2,98 = 5.46, p = .006) and emotional health (F2,104 = 3.39, p = .037). Specifically, the intervention group reported significant improvements in vitality (p < .001) and general health (p = .003) and fewer role limitations due to physical (p < .001) or emotional health (p = .044) (ds=0.37 to 0.55, small to moderate effect size improvements) from pre- to immediately post-intervention compared to no significant (ps = .186 to .737) change in the control group. These improvements were maintained over time, as significant (ps < .05) improvements (ds=0.29 to 0.56, small to moderate effect size improvements) in the intervention group were still present at follow-up. Table 3 shows means, standard deviations, and effect sizes for all of the subscales.
Pain Intensity and Interference
At baseline, 29 older adults (52% of sample) reported pain (i.e., mild to moderate pain). Among the 29 adults (control n = 13; intervention n = 16) that reported pain, results indicated there were significant group x time interactions for pain intensity (F2,104 = 9.41, p < .001) and pain interference (F2,104 = 9.01, p < .001). Specifically, the intervention group reported a significant (p < .05) reduction in pain intensity from pre- to post-intervention (d=−1.15, large effect size reduction), which is in contrast to the control group which reported no significant change in pain intensity (d=0.24, small effect size increase) from pre- to post intervention. There were no significant (p = .524) group differences in pain intensity at follow-up. Additionally, there were significant (p < .05) reductions in pain interference (d=−0.43, small effect size reduction) from pre- to post-intervention in the intervention group with scores returning to baseline at follow-up. In contrast, the control group reported a significant (p < .05) increase in pain interference (d=0.65, moderate effect size increase) from pre- to post-intervention, with a return to baseline at follow-up. Table 3 shows means, standard deviations, and effect sizes for pain intensity and interference outcomes.
Feasibility
Older adults who participated in the “Stand Up and Move More” intervention indicated high satisfaction with the workshop. All participants reported that they thought the workshop was beneficial. When asked what they liked about the workshop, participants indicated it made them aware of the importance of standing up and moving more throughout the day, the workshop sessions were interactive providing good conversation and sharing of ideas, the action plans created structure for establishing goals, and the workshop improved their thoughts, attitudes, and confidence levels. As for what participants disliked about the workshop, a couple of participants indicated there was too much paperwork (completing logs at the end of the day). Also, several individuals did not like the click counters at first, but most participants thought the click counters provided a good way to monitor their progress. Attendance at the workshop sessions was very good (89% attended all sessions), and the overall adherence rate (95%; i.e., percent of participants that completed assessments at all three time-points) was excellent (only two participants dropped out of the intervention group with one participant dropping out of the wait-list control group). In addition, there were no adverse events. Therefore, feasibility of older adults completing the workshop was high.
The workshop facilitators indicated the feasibility of delivering the “Stand Up and Move More” workshop in a community setting was high. There was unanimous agreement on ratings for: clarity of content in the leader manual = 4 (very good); ease of implementing = 4 (very good); attendance = 5 (excellent); resources provided = 5 (excellent); and overall satisfaction with the workshop = 5 (very satisfied). Also, during the wrap-up meeting, the facilitators indicated the curriculum was practical, easy to deliver, and was a good fit for health promotion programming for older adults in their communities. Further, fidelity checks indicated the facilitators delivered the curriculum as intended.
DISCUSSION
This study offers experimental evidence to support the role of a behavior change workshop as an effective and feasible intervention to reduce sedentary behavior in community-dwelling older adults. The main finding from this study was that older adults who participated in the “Stand Up and Move More” workshop had significant reductions in sedentary behavior and improvements in physical function and health-related quality of life. Pain intensity and pain interference decreased, and there were no adverse events from participating in the workshop. Therefore, the “Stand Up and Move More” intervention was found to be safe and effective for older adults. Participants reported frequent use of easy-to-implement strategies to reduce sedentary behavior including, for example: standing up during TV commercials, spreading household chores out across the day, and standing up while doing daily activities which they previously did while sitting down (e.g., reading, quilting, etc.). These strategies resulted in an average reduction in total sitting time of 68 minutes/day.
The reported reduction in sedentary time following our sedentary behavior intervention is consistent with previous investigations involving older adults that reported sedentary behavior reductions ranging from 9 to 132 minutes following intervention, with larger reductions for self-reported sedentary behavior (Gardiner et al., 2011; Fitzsimmons et al., 2013; Rosenberg et al., 2015; Lewis et al., 2015; Kerr et al., 2016; Maher et al., 2017). However, as a recent review highlighted, many of the prior investigations have been limited due to small samples, a lack of randomized control groups and a tendency to rely on self-report for assessing sedentary time at a single time point immediately following the intervention (Aunger et al., 2018). The results from the current study adds to the literature by addressing these limitations in addition to assessing physical function and health-related quality of life in conjunction with sedentary behavior.
In addition to reducing sedentary behavior, the current study also revealed improvements in physical function (i.e., balance, mobility, and getting up from a chair) for sedentary, older, community dwelling adults who engaged in the workshop. This is important as physical function has been shown to play a vital role in maintaining independence (Semanik et al., 2015). Loss of independence in older adults can place considerable financial burden on them, their families, and the healthcare system (Guralnik et al., 2002), thus, interventions like the “Stand Up and Move More” intervention, which improved physical function, could be important in helping older adults maintain their independence. Finally, older adults who participated in the “Stand Up and Move More” workshop reported significant improvements in vitality and general health and indicated fewer role limitations due to physical and emotional health.
It is interesting to note that although there was close agreement between self-reported and monitor-derived sedentary time prior to the start of the intervention, there were rather large discrepancies between self-reported and monitor-derived sedentary behavior when assessed immediately following the intervention and at follow-up. This finding suggests a behavioral artifact of potentially self-reporting less sedentary behavior after receiving an intervention, and thus highlights the importance of not solely relying on self-report when conducting intervention studies (Copeland et al., 2017). Assessing self-reported sedentary behavior with an interview still yields valuable information as it allows researchers to understand the type of specific activities (e.g., watching TV, reading, socializing) that result in the accumulation of total sedentary time, which is data that are not attainable from activity monitors. Furthermore, information obtained from self-report may shed light on the context in which one engages in sedentary behaviors (e.g., sitting alone in the dark versus sitting with others in a social setting; or sitting while reading versus sitting watching TV), which is a relatively unexplored area that may have important implications for and differentially influence various physical and mental health outcomes (e.g., cognition, depression).
Participants reported being highly satisfied with the “Stand Up and Move More” workshop, attendance rates were excellent, and all participants found participation in the workshop to be beneficial. In addition, participants reported that breaking up sitting time was more appealing to them than increasing exercise. The workshop facilitators were also highly satisfied with the workshop, and reported the curriculum was easy to understand and provided excellent interaction with participants. The workshop was characterized as practical, easy to implement, and a good fit for the community. Thus, the “Stand Up and Move More” intervention was found to be feasible to implement (i.e., acceptable, easy to deliver, and could be integrated into community health programming) by workshop facilitators in small urban and rural communities.
Most of the participants in this study were women (88%) which is a potential limitation because it is not clear whether the results from this study generalize to men. In addition, all of the participants were Caucasian so results cannot be generalized to other ethnic/racial older adults (Note: we recently conducted a study examining the effectiveness and feasibility of the “Stand Up and Move More” intervention for African American elders and a paper summarizing the results is currently in preparation). Among its strengths, this study utilized a randomized controlled trial design, and was a collaborative effort between university researchers and county health promotion coordinators in small urban and rural communities. Also, inclusion of a follow-up assessment (i.e., 8 weeks post-intervention) was a strength because it provided information regarding whether improvements in sedentary behavior, physical function, and HRQoL were maintained after the intervention ended. Findings from the present study indicated that sedentary time began to increase again in the weeks following the intervention but, importantly, improvements in physical function and HRQoL were maintained in the intervention group 8 weeks following participation in the workshop. Currently, it is unclear how much of a reduction in sedentary time is needed to maintain improvements in physical function and HRQoL after an intervention ends. In the present study, participants at follow-up were on average, sitting 18 minutes/day less than baseline. They had increased the number of times they stood up each day by 9 stands/day. In addition, participants at follow-up had decreased the duration of their sitting bouts by 9 minutes/bout and had increased their moderate-intensity physical activity by 10 minutes/day. It is unclear whether these small changes across the day were responsible for maintaining improvements in physical function and HRQoL after the workshop ended. Further research is needed to determine the “dose” of a reduction in sedentary behavior or the combination of breaks in sedentary behavior along with small increases in physical activity that are effective in improving health and function, as well as in maintaining improvements over time in older adults.
In sum, translating effective interventions into community practice is essential for improving the health and function of older adults. Partnering with community aging organizations is advantageous because it capitalizes on social networks in the community as well as on existing resources that provide an opportunity to offer the intervention on a continuing basis. The “Stand Up and Move More” workshop was developed with community collaborators to be implemented in community settings. The health promotion coordinators saw it as a viable intervention for older adults in their communities, particularly older adults with compromised health and functional limitations who are currently inactive. The “Stand Up and Move More” intervention was designed to help older adults make small incremental changes to their daily routines resulting in improved physical function and health-related quality of life. Interventions that remediate functional decline are of high priority (McAuley et al., 2011). Thus, findings from this study could have important public health implications as the intervention provides a practical, easy to implement strategy to improve functional performance in older adults. As the population of older adults continues to increase, the dissemination of effective strategies to help older adults maintain their independence is essential for containing costs in this growing population. Sitting less seems simple but intervention is necessary to get older adults to do it. Breaking up sitting time is a practical, low-cost intervention with the potential to improve the health and function of older adults that could be translated to communities across the country.
Supplementary Material
Acknowledgements:
We would like to thank our health promotion coordinators (Joyce Lubben, Brittany Mainwaring, Amie Rein) for delivering the workshops, Jill Renken for leading the training session on delivering the “Stand Up and Move More” curriculum, Samantha Dawes for assisting with data entry, and all of the participants.
Funding: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under award AG054916 awarded to Kelli F. Koltyn. The project was facilitated by the University of Wisconsin Community-Academic Aging Research Network (CAARN), through funding from the UW School of Medicine & Public Health, and from the Clinical & Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR002373. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institutes of Health. The funding source had no role in the collection, analysis, and interpretation of data; in writing the report; or in the decision to submit the article for publication.
IRB protocol/human subjects approval numbers: This study was approved by the University of Wisconsin – Madison Social and Behavioral Sciences IRB (2013-1155-CR004).
Footnotes
Conflict of interest statement: The authors declare that there is no conflict of interest.
Clinical trial registration: ClinicalTrials.gov Identifier: NCT03412084
References
- Aunger JA, Doody P, & Greig CA (2018). Interventions targeting sedentary behavior in nonworking older adults: A systematic review. Maturitas, 116, 89–99. 10.1016/j.maturitas.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Cohen J Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Erlbaum Associates; 1988. [Google Scholar]
- Copeland JL, Ashe MC, Biddle SJ, Brown WJ, Buman MP, Chastin S, Gardiner PA, Inoue S, Jefferis BJ, Oka K, Owen N, Sardinha LB, Skelton DA, Sugiyama T, & Dogra S. (2017). Sedentary time in older adults: A critical review of measurement, associations with health, and interventions. British Journal of Sports Medicine, 51(21), 1539. 10.1136/bjsports-2016-097210 [DOI] [PubMed] [Google Scholar]
- Crombie KM, Leitzelar BN, Almassi NE, Mahoney JE, & Koltyn KF (2019). Translating a “Stand Up and Move More” intervention by state aging units to older adults in underserved communities: Protocol for a randomized controlled trial. Medicine, 98(27), e16272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Rezende LFM, Rey-López JP, Matsudo VKR, & do Carmo Luiz O. (2014). Sedentary behavior and health outcomes among older adults: A systematic review. BMC Public Health, 14, 333. 10.1186/1471-2458-14-333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyo RA, Katrina Ramsey, null, Buckley DI, Michaels L, Kobus A, Eckstrom E, Forro V, & Morris C. (2016). Performance of a Patient Reported Outcomes Measurement Information System (PROMIS) Short Form in Older Adults with Chronic Musculoskeletal Pain. Pain Medicine (Malden, Mass.), 17(2), 314–324. 10.1093/pm/pnv046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellingson LD, Schwabacher IJ, Kim Y, Welk GJ, & Cook DB (2016). Validity of an Integrative Method for Processing Physical Activity Data. Medicine and Science in Sports and Exercise, 48(8), 1629–1638. 10.1249/MSS.0000000000000915 [DOI] [PubMed] [Google Scholar]
- Fitzsimons CF, Kirk A, Baker G, Michie F, Kane C, & Mutrie N. (2013). Using an individualised consultation and activPALTM feedback to reduce sedentary time in older Scottish adults: Results of a feasibility and pilot study. Preventive Medicine, 57(5), 718–720. 10.1016/j.ypmed.2013.07.017 [DOI] [PubMed] [Google Scholar]
- Gardiner PA, Clark BK, Healy GN, Eakin EG, Winkler EAH, & Owen N. (2011). Measuring older adults’ sedentary time: Reliability, validity, and responsiveness. Medicine and Science in Sports and Exercise, 43(11), 2127–2133. 10.1249/MSS.0b013e31821b94f7 [DOI] [PubMed] [Google Scholar]
- Gennuso KP, Thraen-Borowski KM, Gangnon RE, & Colbert LH (2016). Patterns of sedentary behavior and physical function in older adults. Aging Clinical and Experimental Research, 28(5), 943–950. 10.1007/s40520-015-0386-4 [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, & Wallace RB (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49(2), M85–94. 10.1093/geronj/49.2.m85 [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Alecxih L, Branch LG, & Wiener JM (2002). Medical and long-term care costs when older persons become more dependent. American Journal of Public Health, 92(8), 1244–1245. 10.2105/ajph.92.8.1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keadle SK, Arem H, Moore SC, Sampson JN, & Matthews CE (2015). Impact of changes in television viewing time and physical activity on longevity: A prospective cohort study. The International Journal of Behavioral Nutrition and Physical Activity, 12, 156. 10.1186/s12966-015-0315-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr J, Takemoto M, Bolling K, Atkin A, Carlson J, Rosenberg D, Crist K, Godbole S, Lewars B, Pena C, & Merchant G. (2016). Two-Arm Randomized Pilot Intervention Trial to Decrease Sitting Time and Increase Sit-To-Stand Transitions in Working and Non-Working Older Adults. PloS One, 11(1), e0145427. 10.1371/journal.pone.0145427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koltyn KF, Crombie KM, Brellenthin AG, Leitzelar B, Ellingson LD, Renken J, & Mahoney JE (2019). Intervening to reduce sedentary behavior in older adults—Pilot results. Health Promotion Perspectives, 9(1), 71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis LK, Rowlands AV, Gardiner PA, Standage M, English C, & Olds T. (2016). Small Steps: Preliminary effectiveness and feasibility of an incremental goal-setting intervention to reduce sitting time in older adults. Maturitas, 85, 64–70. 10.1016/j.maturitas.2015.12.014 [DOI] [PubMed] [Google Scholar]
- Maher JP, Sliwinski MJ, & Conroy DE (2017). Feasibility and preliminary efficacy of an intervention to reduce older adults’ sedentary behavior. Translational Behavioral Medicine, 7(1), 52–61. 10.1007/s13142-016-0394-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, & Morley JE (2016). SARC-F: A symptom score to predict persons with sarcopenia at risk for poor functional outcomes. Journal of Cachexia, Sarcopenia and Muscle, 7(1), 28–36. 10.1002/jcsm.12048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manini T. (2011). Development of physical disability in older adults. Current Aging Science, 4(3), 184–191. 10.2174/1874609811104030184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Selby VC, Niaura RS, & Rossi JS (1992). Self-efficacy and the stages of exercise behavior change. Research Quarterly for Exercise and Sport, 63(1), 60–66. 10.1080/02701367.1992.10607557 [DOI] [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, & Troiano RP (2008). Amount of time spent in sedentary behaviors in the United States, 2003–2004. American Journal of Epidemiology, 167(7), 875–881. 10.1093/aje/kwm390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E, Szabo A, Gothe N, & Olson EA (2011). Self-efficacy: Implications for physical activity, function, and functional limitations in older adults. American Journal of Lifestyle Medicine, 5(4), 361–369. 10.1177/1559827610392704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick B, Zimmerman SI, Orwig D, Furstenberg AL, & Magaziner J. (2000). Outcome expectations for exercise scale: Utility and psychometrics. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 55(6), S352–356. 10.1093/geronb/55.6.s352 [DOI] [PubMed] [Google Scholar]
- Rosenberg DE, Gell NM, Jones SMW, Renz A, Kerr J, Gardiner PA, & Arterburn D. (2015). The Feasibility of Reducing Sitting Time in Overweight and Obese Older Adults. Health Education & Behavior: The Official Publication of the Society for Public Health Education, 42(5), 669–676. 10.1177/1090198115577378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardinha LB, Santos DA, Silva AM, Baptista F, & Owen N. (2015). Breaking-up sedentary time is associated with physical function in older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 70(1), 119–124. 10.1093/gerona/glu193 [DOI] [PubMed] [Google Scholar]
- Semanik PA, Lee J, Song J, Chang RW, Sohn M-W, Ehrlich-Jones LS, Ainsworth BE, Nevitt MM, Kwoh CK, & Dunlop DD (2015). Accelerometer-monitored sedentary behavior and observed physical function loss. American Journal of Public Health, 105(3), 560–566. 10.2105/AJPH.2014.302270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umstattd Michelle Renee, Motl R, Wilcox S, Saunders R, & Watford M. (2009). Measuring physical activity self-regulation strategies in older adults. Journal of Physical Activity & Health, 6 Suppl 1, S105–112. 10.1123/jpah.6.s1.s105 [DOI] [PubMed] [Google Scholar]
- Verplanken B, & Orbell S. (2003). Reflections on past behavior: A self-report index of habit strength. Journal of Applied Social Psychology, 33, 1313–1330. [Google Scholar]
- Ware JE, & Sherbourne CD (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483. [PubMed] [Google Scholar]
- Yasunaga A, Shibata A, Ishii K, Koohsari MJ, Inoue S, Sugiyama T, Owen N, & Oka K. (2017). Associations of sedentary behavior and physical activity with older adults’ physical function: An isotemporal substitution approach. BMC Geriatrics, 17(1), 280. 10.1186/s12877-017-0675-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.