Abstract
An 80-year-old man was transferred to our institution with lower limb edema and worsening dyspnea following the administration of diuretic medication. Transthoracic echocardiography and computed tomography revealed a giant hepatic cyst (176×190 mm) compressing his right atrium and inferior vena cava (IVC). Laparoscopic cyst deroofing combined with omental packing and subsequent tube drainage immediately alleviated all his symptoms. The procedure was uneventful, and he was discharged without any complications on postoperative day 9; he had no recurrent symptoms or hepatic cysts at the postoperative 2-month follow-up. Therefore, a giant hepatic cyst can cause IVC syndrome, and laparoscopic deroofing is a beneficial approach for the treatment of accessible cysts.
Keywords: hepatic cyst, inferior vena cava syndrome, surgical intervention, laparoscopic deroofing
Introduction
Accurately diagnosing the etiology of clinical symptoms is important; as such, physicians should include every possible etiology as part of a thorough differential diagnosis. Hepatic cyst is a benign disease found in approximately 1-5% of the general population (1). Patients with hepatic cysts infrequently experience complications such as a spontaneous rupture, hemorrhaging, bacterial infection, torsion of a pedunculated cyst, or biliary obstruction (2). We herein describe a rare case of a giant hepatic cyst that compressed the patient's right atrium and inferior vena cava (IVC) thus leading to IVC syndrome. Laparoscopic deroofing was considered as the first-line therapy, which immediately resolved the symptoms.
Case Report
An 80-year-old man presented with lower limb edema, worsening dyspnea, and faintness. His medical history included hypertension and paroxysmal atrial fibrillation. Lower limb edema developed gradually over 4 months. His family doctor diagnosed him with simple idiopathic edema and prescribed 20 mg of furosemide, which induced severe fainting, dyspnea, and feebleness. Thereafter, the patient was transferred to our institution. He was alert with a blood pressure of 131/86 mmHg, a heart rate of 91 bpm, a respiratory rate of 20 bpm, and an oxygen saturation of 98% in room air. His jugular vein and cardiac sounds were normal; however, no respiratory sounds could be auscultated in the right lower lung field, and moderate bilateral pretibial edema was detected (Fig. 1). An electrocardiogram revealed a sinus rhythm with left axis deviation and no significant ST-T change (Fig. 2, left panel). A chest radiograph indicated eventration of the right diaphragm and left deviation of the cardiac silhouette (Fig. 2, right panel). Transthoracic echocardiography revealed that his right atrium and IVC were compressed by an extra-cardiac mass (176×190 mm), while also observing a preserved ejection fraction, an enlarged left atrium, and mild tricuspid regurgitation (Fig. 3). Laboratory evaluations revealed the following values: 1.0 mg/dL of total bilirubin, 48 U/L of aspartate aminotransferase, 50 U/L of alanine aminotransferase, 3.8 g/dL of albumin, 1.11 mg/dL of creatinine, <10 pg/mL of high-sense cardiac troponin I, 39.0 pg/mL of brain natriuretic peptide in the plasma, 1.40 μIU/mL of thyroid stimulating hormone, 2.89 pg/mL of free T3, 1.06 ng/dL of free T4, and no significant albuminuria. Subsequent contrast computed tomography demonstrated a giant hepatic cyst compressing the right atrium and IVC (Fig. 4).
Figure 1.

Bilateral pretibial edema at the first visit.
Figure 2.
Left panel: an electrocardiogram showing a sinus rhythm with left axis deviation and no significant ST-T change. Right panel: a chest radiograph indicating great eventration of the right diaphragm and left deviation of a cardiac silhouette.
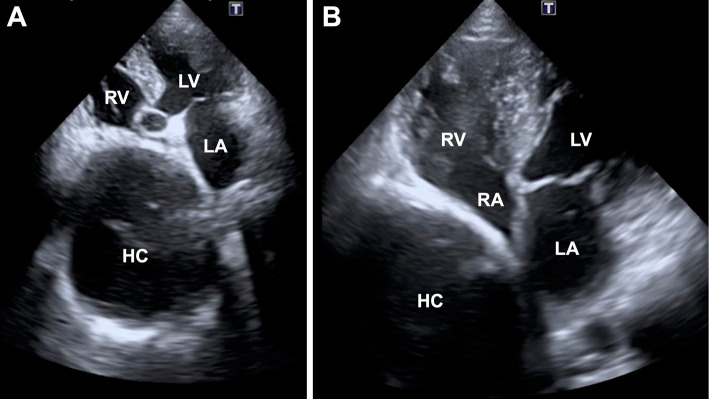
Figure 3.
Transthoracic echocardiography (A: 4-chamber view in high-depth. B: 4-chamber view in low-depth) shows the right atrium excluded by the extra-cardiac mass (176×190 mm) with a preserved ejection fraction. The compressed inferior vena cava cannot be detected. HC: hepatic cyst, LA: left atrium, LV: left ventricle, RA: right atrium, RV: right ventricle
Figure 4.
Computed tomography shows a giant hepatic cyst compressing the right atrium and IVC. Left panel: plane imaging. Middle panel: arterial phase. Right panel: venous phase. AO: aorta, HC: hepatic cyst, IVC: inferior vena cava, LA: left atrium, LV: left ventricle, PV: pulmonary vein, RA: right atrium, RV: right ventricle, SVC: superior vena cava
Based on these physical and objective findings, we diagnosed the patient with IVC syndrome or secondary Budd-Chiari syndrome along with a congestive liver. The suspected etiology was mechanical compression of the IVC, presenting as lower limb edema and a low pre-load of the left heart due to decreased venous return leading to dyspnea and faintness. As a result, the previously prescribed diuretics were deemed to have exacerbated the patient's dyspnea and fainting spells.
First, the diuretics were discontinued and the surgical team was consulted to plan the removal of the cyst causing mechanical compression. As percutaneous transhepatic cholangio drainage and subsequent minocycline-infusion have some risk of recurrence, laparoscopic deroofing of the giant hepatic cyst was chosen in combination with omental packing and subsequent tube drainage. His congestive liver dysfunction immediately resolved, and the lower limb edema disappeared. The drain tube was removed on postoperative day 7, confirming that the drainage had no bile. The patient was discharged without any complications on postoperative day 9 and he did not experience a recurrence of either any symptoms or hepatic cysts based on computed tomography performed 2 months after his surgery (Fig. 5). We obtained the patient's informed consent to publish this case report.
Figure 5.
Computed tomography 2 months after the operation indicates no recurrence of the giant hepatic cyst, thus maintaining the structural integrity and adequate functioning of the right atrium (RA) and inferior vena cava (IVC).
Discussion
This case is instructive and educational, describing an unusual etiology of the IVC syndrome, namely, a giant hepatic cyst compressing the right atrium and IVC. Few reports have been published in this regard (3,4). Our case illustrates two important findings. First, the differential diagnosis of the etiology of patients' clinical symptoms is important for selecting the appropriate treatment. Second, benign hepatic cysts can cause extra-hepatic morbidity.
The symptom of lower limb edema in this case has various etiologies. The relatively most common etiologies are heart failure including right-sided heart failure, hypoalbuminemia, nephrotic syndrome, renal failure, liver cirrhosis, deep venous thrombosis, or lymphedema. As the treatment should be based on its etiology, identifying the specific etiology is key. Right-sided heart failure is actually a representative etiology of lower limb edema, most of which results from left-sided heart failure. In other words, most right-sided heart failure can be treated with medication for left-sided heart failure such as by administering diuretics or vasodilators. However, diuretics without identification of the specific etiologies can also further reduce the systemic venous return and left ventricular pre-load leading to significant symptoms as was seen in our case. This illustrates that the proper identification of the underlying etiology can prevent inappropriate and harmful medications. IVC syndrome causes right-sided heart-failure “like” hemodynamics and mimics right-sided heart failure. Hence, we discontinued diuretics and enforced an appropriate fluid intake, tolerating some lower limb edema. In addition, surgical intervention was the sole intervention required for this patient. After releasing the mechanical compression, he was free from clinical symptoms without any medication.
Though hepatic cysts are benign, our case illustrates they can cause extra-hepatic morbidity. Hepatic cysts are found in approximately 1-5% of the general population (1). Although most hepatic cysts are asymptomatic, a few cases involve complications such as spontaneous rupture, hemorrhaging, bacterial infection, torsion of a pedunculated cyst, or biliary obstruction (2). Compression of the right heart system leading to symptoms such as right-sided heart failure is very rare, but has been reported (3,4). All these morbidities require surgical intervention; this is the sole etiology-orientated treatment in these cases. Several surgical approaches have been suggested for giant hepatic cysts. Simple aspiration could be a symptomatic therapy, but it does not provide any permanent therapeutic benefit in most cases (5). The injection of sclerosants such as minomycin has a low incidence of cyst recurrence or complications (6). Laparoscopic surgery is a less invasive strategy compared to conventional open procedures, and recurrence rates ranging from 0-14.3% and morbidity rates of 0-15% have been reported after laparoscopic deroofing of simple hepatic cysts (7). Laparoscopic deroofing should therefore be considered as a first-line therapy for accessible cysts.
In conclusion, a giant hepatic cyst can cause IVC syndrome. Laparoscopic deroofing is a beneficial choice in cases with accessible cysts.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Regev A, Reddy KR, Berho M, et al. Large cystic lesions of the liver in adults: a 15-year experience in a tertiary center. J Am Coll Surg 193: 36-45, 2001. [DOI] [PubMed] [Google Scholar]
- 2.Gadzijev E, Dragan S, Verica FM, Jana G. Hepatobiliary cystadenoma protruding into the common bile duct, mimicking complicated hydatid cyst of the liver. Report of a case. Hepatogastroenterology 42: 1008-1010, 1995. [PubMed] [Google Scholar]
- 3.Kashiwagi H, Kumagai K, Nozue M. Single incision laparoscopic surgery for a life-threatening, cyst of liver. Tokai J Exp Clin Med 36: 13-16, 2011. [PubMed] [Google Scholar]
- 4.O'Connor A, Lee M, McEntee G, McNamara DA. Massive hepatic cyst presenting as right-sided heart failure. Ir J Med Sci 181: 365-367, 2012. [DOI] [PubMed] [Google Scholar]
- 5.Saini S, Mueller PR, Ferrucci Jr JT, Simeone JF, Wittenberg J, Butch RJ. Percutaneous aspiration of hepatic cysts does not provide definitive therapy. AJR Am J Roentgenol 141: 559-560, 1983. [DOI] [PubMed] [Google Scholar]
- 6.Danza FM, Falcione M, Bordonaro V, Infante A, Paladini A, Bonomo L. Minocycline hydrochloride as a soft sclerotizing agent for symptomatic simple renal and hepatic cysts. Eur Rev Med Pharmacol Sci 21: 408-415, 2017. [PubMed] [Google Scholar]
- 7.Zacherl J, Scheuba C, Imhof M, Jakesz R, Fugger R. Long-term results after laparoscopic unroofing of solitary symptomatic congenital liver cysts. Surg Endosc 14: 59-62, 2000. [DOI] [PubMed] [Google Scholar]