Abstract
Objective
Excess administrative costs in the US health care system are routinely referenced as a justification for comprehensive reform. While there is agreement that these costs are too high, there is little understanding of what generates administrative costs and what policy options might mitigate them.
Data Sources
Literature review and national utilization and expenditure data.
Study Design
We developed a simulation model of physician billing and insurance‐related (BIR) costs to estimate how certain policy reforms would generate savings. Our model is based on structural elements of the payment process in the United States and considers each provider's number of health plan contracts, the number of features in each health plan, the clinical and nonclinical processes required to submit a bill for payment, and the compliance costs associated with medical billing.
Data Extraction
For several types of visits, we estimated fixed and variable costs of the billing process. We used the model to estimate the BIR costs at a national level under a variety of policy scenarios, including variations of a single payer “Medicare‐for‐All” model that extends fee‐for‐service Medicare to the entire population and policy efforts to reduce administrative costs in a multi‐payer model. We conducted sensitivity analyses of a wide variety of model parameters.
Principal Findings
Our model estimates that national BIR costs are reduced between 33% and 53% in Medicare‐for‐All style single‐payer models and between 27% and 63% in various multi‐payer models. Under a wide range of assumptions and sensitivity analyses, standardizing contracts generates larger savings with less variance than savings from single‐payer strategies.
Conclusion
Although moving toward a single‐payer system will reduce BIR costs, certain reforms to payer‐provider contracts could generate at least as many administrative cost savings without radically reforming the entire health system. BIR costs can be meaningfully reduced without abandoning a multi‐payer system.
Keywords: administrative costs, health care reform, health insurance, single‐payer systems
What is Known
Billing and insurance‐related administrative costs are higher in the United States than in nearly every other OECD country
Advocates for single‐payer models in the United States cite reducing administrative costs as a benefit of their proposals
It is not known how other market reform models could impact billing and insurance‐related administrative costs in the United States
What This Study Adds
We developed a model that can be used to understand national billing and insurance‐related costs at an activity‐based level
We estimate the effects of assorted reforms on billing and insurance‐related administrative costs, and we compare reductions from instituting a single‐payer system with reforms of the current private, multi‐payer system.
Reforms to our current multi‐payer system can reduce administrative costs comparbly to a single‐payer system. It therefore is possible to reduce billing and insurance‐related administrative costs without requiring disruption of the entire health insurance model in the United States.
1. INTRODUCTION
The transaction cost of paying for services with a commercial credit card is approximately 2% of the total cost, whereas Tseng (2018) 1 calculated that it is 14.5% when providers bill insurance companies for physician services. A similar percentage is consumed for hospital billing, and approximately an additional 15% is retained by commercial insurers for claims processing and other costs under the Affordable Care Act.
Health care administrative costs in the United States are higher than in other rich nations. Estimates suggest over $265 billion of annual spending is wasted due to administrative complexity, 2 yet the substantial literature on wasted health care spending offers little discussion of what drives these costs or how to reduce them. 3 , 4 When administrative costs are discussed in policy circles, it is usually to contrast the American system to single‐payer systems in countries like Canada. 5 , 6 One notable exception is David Cutler's recent proposal for a national clearinghouse, 7 though Cutler's innovative idea is the exception that proves the rule. The most common proposal to reduce the transaction costs of paying for health care has been to advocate for a single‐payer “Medicare‐for‐All” model that nationalizes Medicare fee‐for‐service coverage, with all of that program's complexity.
Studies measuring BIR costs in the United States assemble costs based either on the costs of departments 8 or the costs of time spent on billing by individual personnel. 9 , 10 , 11 We construct a model relying on data from Tseng (2018) 1 to generalize the drivers of BIR costs nationwide. Tseng (2018) 1 employs activity‐based costing to measure the costs of specific steps of the billing process, thus measuring administrative costs at the level of individual bills. Using Tseng (2018) 1 data thereby allows estimates of cost savings if certain billing procedures were simplified. We categorize the service‐specific and activity‐specific BIR cost data provided in Tseng (2018) 1 to identify three components of BIR costs (fixed costs, per‐visit clinical documentation variable costs, and per‐visit nonclinical documentation variable costs) associated with five types of visits (primary care, emergency department visits, inpatient stays, ambulatory surgery, and inpatient surgery). This level of granularity allows us calculate the ratios of fixed to variable costs and of clinical documentation costs to nonclinical documentation costs (Table S1).
Using these building blocks, we use national volume data from the CDC to estimate the relative magnitude of national BIR costs for each of the five types of visits described (Table S2). This reduction allows us, via the mathematical model used, to avoid measuring the cost ratios for every provider and visit type or assuming that providers and visit types have BIR cost structures identical to those studied in Tseng (2018) 1 . Instead, we categorize national costs in terms of the fraction of costs associated with each visit type and each provider based only on assumptions about the provider's ratio of fixed to variable costs, ratio of clinical to nonclinical documentation costs, and the number of contracts they currently administer. We use these parameters to study how the impact of reform differs across providers and to account for the uncertainty in the parameter estimates with extensive sensitivity analyses (Tables S3‐S5). We are thus able to simulate savings from reforms to the American multi‐payer health insurance market and to compare those savings to estimated savings from a single‐payer system.
Our simulation is an effort to measure national BIR costs from the bottom‐up—that is, from a derivation of specific, transaction‐level administrative costs—instead of relying on aggregate numbers. 3 , 5 , 6 , 9 It is structured not to produce specific estimates but instead to uncover the potential of reducing BIR costs at their source. Although our approach has the shortcoming of resting on measurements from a single representative site and then extrapolating nationwide, it offers more specificity than prior approaches since it identifies specific sources of BIR costs. This allows for a direct determination of the impact of specific reforms and estimating their nationwide effect.
Our results indicate that standardizing and simplifying US billing procedures can produce BIR savings that are comparable—and in some cases superior—to savings produced by a single‐payer system. 8 , 10 There have been considerable studies documenting that single‐payer systems generate fewer BIR costs than the current US system, so our results should be read as a cautionary tale. It suggests that incremental changes to BIR processes could generate savings of a similar magnitude as a wholesale revamping of our health financing system. To the degree that our findings indicate that there are less disruptive but similarly fruitful paths ahead, these administrative reforms deserve greater consideration.
2. DATA AND METHODS
2.1. Categorizing BIR costs
Tseng (2018) 1 documented that American providers expend significant resources to file a bill and receive payment from US commercial insurers. The study revealed three categories of the underlying drivers of costs across five types of patient visits. The visit types and categories of costs are detailed in Table S1.
The first category of costs arise from simultaneously administering multiple, dissimilar contracts. One of the defining characteristics of the US health care market is the presence of multiple and (compared to other nations) loosely constrained payers. This variety and flexibility is expressed in the individualized contracts that each payer executes with participating providers. Each provider has contracts with multiple payers. For example, providers caring for patients from zip code 33 497 in Florida will have to administer up to all 47 concurrent Medicare Advantage plans in the area. Because each contract imposes a unique payment model onto an already complex delivery system, providers are caught in a crossfire of complexity. Providers develop separate collection strategies to obtain payment from separate payers, accommodate to multiple documentation requirements, and even manage multiple payment models, especially as payers pursue bundling or other payment reforms. Tseng (2018) 1 revealed that providers expend resources administering multiple payment systems and that those costs increase with each additional plan offered in the market. We call these architectural complexity (AC) costs and assume that they scale linearly with the number of contracts a provider administers. A single‐payer model or a reduction in the number of different payer contracts would reduce architectural complexity costs.
The second category of costs arise from the complexity of the individual contracts that providers consummate with insurers. These contracts require providers to register patients, fully document the services provided, and detail plan‐specific justifications for providing those services. Typically, these contracts impose substantial administrative burdens. For example, the updates to Medicare's 2019 payment rules are over 1,000 pages long. Moreover, these already‐complex contracts incorporate other documents, such as online coverage manuals with detailed billing instructions, and these provisions often change at the unilateral discretion of the payers. For example, Blue Shield of California maintains four different provider manuals for physicians: the HMO IPA/Medical Group Procedure Manual, the Independent Physician and Provider Manual, the Blue Shield Promise Cal MediConnect and Medi‐Cal Provider Mauals, and the Medical Interface Manual (for behavioral health). The HMO/IPA Medical Group Procedure Manual is a 428 page document issued January 1, 2021, that had a 20 page update issued the same day. 12 Even though many patient‐provider interactions are governed by a common contract, administering that contract for each interaction requires costly attention by billing personnel. We call these contractual complexity (CC) costs. A single‐payer model or a change in the structure of multi‐payer contracts could either reduce or increase contractual complexity costs.
The third category of costs arise from the legal, regulatory, or negotiated requirements of billing, which we call compliance (C) costs. Compliance costs associated with billing the government are reflected in the dangers of committing Medicare fraud, violating Stark or Antikickback laws, or otherwise failing to conform to federal reimbursement rules. Medicare's rigid administrative payment rules introduce costs of their own that can be avoided in private settings. 13 Complying with federal government regulations is widely considered to be more costly than complying with obligations to private payers, in large part because disputes with private payers can be navigated without the rigidity of public procedures or the threat of criminal sanctions. These two features—the potential for criminal sanctions and the burdens of federal bureaucratic inflexibility—motivate our assertion that compliance costs are higher for Medicare. Although Medicare might more readily issue payments, and issue fewer rejections, to providers, Medicare also retroactively prosecutes violations of their payment rules, and health care systems have developed large compliance programs to preclude such violations. We introduce compliance costs into our estimations when making comparisons between multi‐payer and public payment systems.
2.2. Modeling BIR costs
We construct a model of provider BIR costs that is built upon the three costs (AC, CC, C) listed above. We begin with the observation that total BIR costs are a sum of variable costs, which increase with patient volume, and fixed costs. We further model variable costs to include clinical documentation costs and nonclinical documentation costs. We used detailed observation data from Tseng (2018) 1 on fixed and variable costs associated with provider billing—including clinical and nonclinical documentation costs—to decompose BIR costs into more detailed this model estimates as AC, CC, and C costs. In this analysis, we are limited to billing costs considered in Tseng (BIR costs are a subset of all provider administrative costs). Our model's constituent parts are as follows:
2.2.1. Per‐visit nonclinical documentation (ND) costs
Before the clinical documentation of a patient's visit is complete, the appropriate set of documentation and legal requirements must be identified. The costs of identifying these contractual and legal requirements increase with the number and complexity of contracts as well as with legal compliance costs. We model ND costs as being associated with the product of AC, CC, and C costs.
2.2.2. Per‐visit clinical documentation (CD) costs
Clinical documentation includes administrative efforts to translate patient care services into payments. Clinical documentation costs increase with compliance costs and the complexity of the relevant contract. We model CD costs as being associated with the product of CC and C costs.
2.2.3. Annual provider fixed costs (FC)
These cost represent the costs associated with establishing and maintaining contracting and billing operations (eg, physical plant and software,). These are independent of patient volume. We model FC costs as being associated with the product of ND, CC, and C costs as well as the fraction (F) of contracts that are negotiated or renegotiated each year. In the single‐payer model, there are no negotiations with the government. Instead, as government rules are updated annually, providers bear costs associated with interpreting and adhering to the updates applicable to the institution.
These variables and their mathematical relationships to each other and to BIR costs are summarized in Table 1
TABLE 1.
Variables defining provider‐specific billing and insurance‐related (BIR) costs
| Category | Parameter | Symbol | Mathematical formulation | Assumptions b |
|---|---|---|---|---|
| Provider‐specific parameters dependent on policy reform a | For each provider, the number of features per contract as a fraction of baseline depends on reforms to contractual complexity | X | Baseline value 1 | Varies between 0.5 and 1.2 across scenarios |
| For each provider, the legal burden of administering contracts as a fraction of baseline depends on reforms to legal compliance | L | Baseline value 1 | Varies between 0.5 and 1.2 across scenarios | |
| For each provider, the number of contracts depends on reforms to architectural complexity | N | Whole number, assumed to vary across providers and scenarios. | Median 1000 and interquartile range [100,10000] at baseline | |
| Provider‐specific a | Clinical documentation cost per visit | CD | Provider‐specific per‐visit cost of clinician time spent on documenting exclusively for the purpose of billing and administration. | Table S1 |
| Nonclinical documentation cost per visit | ND | Provider‐specific per‐visit cost of nonclinician time spent on documenting exclusively for the purpose of billing and administration. | Table S1 | |
| Fraction of contracts that are negotiated or renegotiated each year | F | Default value 0.25, set to either 0.25 or 1 across scenarios | Set to either 0.25 or 1 across scenarios | |
| Marginal cost of per‐visit clinical documentation as a linear multiple of the complexity and legal burden of the provider's contracts | aCD | CD = aCD*X*L | May vary arbitrarily across providers | |
| Marginal cost of nonclinical documentation as a linear multiple of the complexity, legal burden, and number of the provider's contracts | aNC | NC = aND*X*L*N | May vary arbitrarily across providers | |
| Fixed annual contracting costs as a linear multiple of the complexity, legal burden, number, and fraction re‐negotiated annually of the provider's contracts | aFC | FC = aFC*X*L*N*F | May vary arbitrarily across providers | |
| Number of visits | V | Assumed fixed for each provider across scenarios | May vary arbitrarily across providers | |
| Ratio of per‐visit clinical to nonclinical documentation costs | r | CD/ND = a1/(a2N) | Table S1 | |
| Ratio of fixed to variable costs | s | FC/(v*VC) = a3NF/(v(a1 + a2NF)) | Table S1 |
Each of the provider‐specific variables differs for each provider and should technically be denoted with a subscript i to correspond to providers of type i, for example, ai,CD. We omit these subscripts since the relationships between the variables are identical across providers.
2.3. Overview of mathematical model
We model the costs associated with the legal, architectural, and compliance complexity as unknown and potentially different for each provider. To avoid calculating costs at baseline for each intervention for thousands of providers, each with particularized BIR values, we instead calculate for each provider the ratio of BIR costs at baseline to BIR costs under each of the proposed policies. Calculating these ratios allows for an algebraic simplification that cancels provider‐specific constants and depicts the change in BIR costs in terms of each provider's ratio s, of fixed costs to variable costs; ratio r, of nonclinical documentation costs to clinical documentation costs; and N, the number of contracts the provider administers. To estimate the relative contribution to national expenditures, we use the estimates for the values r and s for each type of visit (Table S1) the relative contribution of each type of visit to total national spending, and the fraction of national providers with 10, 100, 1000, and 10,000 contracts (Table S2). We perform extensive analyses of the sensitivity of the results to variations in the value of the variables r,s, and N (Tables S3‐S5).
We model the impact of each policy on national administrative costs as the average of the provider‐ and visit‐specific percent cost reductions weighted by the fraction of the total expenditure associated with each type of provider and visit. We assume provider BIR costs were 14.5% of physician revenue and then allocated billing costs at a national level across visit types.
2.4. Detailed example illustrating the mathematical model
We consider two hypothetical primary care providers to illustrate the mathematical model of how provider‐specific variables change with national policy reform (Table 1). Provider A operates a single physician practice in a region dominated by a single insurer (such as Alabama, where 99% of the commercially insured population is covered by Blue Cross Blue Shield). This provider cares only for local patients, and her patients collectively are insured under only ten insurance contracts (N = 10). Her small practice has relatively low overhead costs as a fraction of total costs (s = 1/4), and the majority of her documentation costs are clinical (clinical visit notes) rather than nonclinical (documentation tasks related to billing requirements), leading to a 3:1 ratio of clinical to nonclinical documentation costs (r = 3). Provider B is employed by a large academic medical center with the custom deployment of a large commercial EHR. Her patients come from across the state and thus are collectively covered by two thousand separate insurance contracts (N = 2000). Due to the complexity of her practice, she has relatively high overhead costs as a fraction of total costs (s = 1/2) and her nonclinical documentation costs are two‐thirds of her clinical documentation (r = 1.5). Both providers re‐negotiate each contract once every 4 years, that is, re‐negotiate one fourth of their contracts each year (F = 0.25).
Companies in industries such as finance and consumer credit use a combination of technical and regulatory reforms to simplify the contracts they commonly use. As a proxy for similar reform in health care, we let X and L denote, respectively, the average number of features per contract and the legal burden of maintaining each contract, as a fraction of the current baseline.
The clinical documentation for each patient's care is governed by a single contract. The provider's per‐visit clinical documentation (CD) costs are assumed to be some provider‐specific multiple of the product of contractual complexity (aCD,XX) and a provider‐specific multiple of legal burden (aCD,LL). Note that these costs are independent of the provider's total number of contracts. These costs are denoted CD = aCDXL where aCD = aCD,X*aCD,L indicating that, for example, if contractual complexity doubled than so would the provider's clinical documentation costs. Since the variables aCD,X and aCD,L may differ between providers, this does not require any assumptions about similarities between providers beyond that costs change linearly with changes to complexity and legal burden. Under the baseline assumptions (X = 1, L = 1), suppose that Provider A and Provider B have, respectively, contractual complexity multipliers of 4.5 (aCD,X = 4.5) and 3 (aCD,X = 3) and legal burden multipliers of 2 (aCD,L = 2) and 2.5 (aCD,L = 2.5). This corresponds to their, respective, costs being CD = 4.5X2L = 9 and CD = 3X2.5L = 7.5 that decline by 50% if contractual complexity is cut in half.
The nonclinical documentation costs for each patient's care include the “search costs” of identifying the appropriate contract and corresponding rules, a cost that scales with the number of contracts. Similarly to CD, each provider's per‐visit nonclinical documentation (ND) are assumed to be a product of the provider‐specific multiples of contractual complexity (aND,X X), legal burden (aND,LL), and the number of contracts they administer (aND,NN) denoted ND = aNDXLN where aND = aND,X* aND,L* aND,N. Note that ND do not depend on the frequency with which contracts are renegotiated. Finally, the annual fixed costs of maintaining a claim system depend on the complexity of the contracts, the associated legal burden, the number of contracts, and the fraction of contracts re‐negotiated annually necessitating system updates. This is defined as above as a product of provider‐specific multiples of each of X, L, N, and F denoted FC = aFXLNF where aFC = aFC,X* aFC,L* aFC,N* aFC,F.
The myriad multiplicative constants introduced above allow each provider to have its own cost structure and allow each factor to contribute differently to each component of that cost structure. The first key modeling decision is to calculate the ratio, rather than the difference, of each provider's costs under each reform to their costs at baseline. For example, the ratio of each provider's variable costs under optimistic single payer (XSP = 1, LSP = 1, NSP = 1) to costs at baseline (X = 1, L = 1, N = 10 or 2,000) is:
Supplement B works through the algebra of such simplifications to calculate the change in each provider's costs under each of the scenarios considered.
The second key modeling decision is to cancel out the constants aCD, aND, and aFC in a way that allows us to categorize national costs based only on assumptions about the provider's ratio of fixed to variable costs, ratio of clinical to nonclinical documentation costs, and the number of contracts they currently administer. For example, we can write each provider's ratio of per‐visit clinical to nonclinical documentation costs as r = CD/ND = aCDXL/aNDXLN = aCD/aNDN. Thus, in any subsequent calculation, we may solve the above to produce rN = aCD/aF and replace the ratio of the unknown provider‐specific ratio aCD/aF with rN. Returning to the example introduced at the begging of this section, providers 1 and 2 were assumed, respectively, to be characterized by values r = 3 and N = 10 corresponding to aCD/aF = rN =3*10 = 30 and r = 1.5 and N = 2000 corresponding to aCD/aF = r*N = 1.5*2000 = 3000. This translates into:
These results match the intuition that the provider with more contracts sees greater savings under single payer.
Through these two modeling assumptions, the results of the model depend only on the assumption that the value of r, s, and N for providers across the nation lie in a range of values close to those identified in Tseng 2018. The thorough analysis of the sensitivity of the model to changes in these values bolsters the generality of the model.
2.5. Estimating policy impacts
We explored different variants of policy approaches to reducing administrative costs, including a single‐payer model and reforms to the current multi‐payer health insurance market.
In the single payer “Medicare‐for‐All” fee‐for‐service model, we set to 1 the number of contracts for each provider. We modeled an “optimistic” variant of a single‐payer policy, in which neither contract complexity costs nor compliance costs increase from current levels. Since a single‐payer contract would have to be more comprehensive than the typical commercial contract and would be subject to federal payment rules, we also modeled alternatives that allowed for increases in contractual complexity and compliance costs: a “pessimistic” variant of a single‐payer policy with a 20% increase each type of cost and an “intermediate” variant with a 10% increase in each.
We modeled three types of administrative simplification reforms based on the current market: one that simplifies individual contracts (ie, reduces the number of features), thereby reducing contractual complexity; one that standardizes contracts across the market and thus limiting the number of kinds of contracts to 1, thereby reducing architectural complexity; and one that both simplifies and standardizes contracts, thereby reducing both contractual and architectural complexity.
3. RESULTS
Baseline estimation of the fixed and variable BIR costs per provider organization for each type of patient is shown in Table 2.
TABLE 2.
Starting values for the BIR model
| Visit type | Physician office visit | ED | Inp | Amb Sur | Inp Sur | Total |
|---|---|---|---|---|---|---|
| Per‐visit BIR cost | $20.49 | $61.54 | $124.26 | $170.4 | $215.1 | ‐ |
| Percent of total BIR costs | 55.33% | 17.89% | 9.56% | 13.04% | 4.17% | 100% |
| Total BIR cost, (100 thousands) | $61 615 | $19 922 | $10 646 | $14 521 | $4644 | $111 360 |
Estimation of the fixed and variable BIR costs per patient encounters in the United States. Physician payments in 2019 were $768 billion, 22 14.5% of which were estimated to represent BIR costs, 2 or a total of $111.36 billion. We further allocate these costs across different patient encounters, based on the number of patient visits nationally and the reported BIR cost per visit. 2 , 23 , 24 , 25 , 26
Single‐payer systems and reformed multi‐payer systems generate significant savings in BIR costs. National BIR costs are reduced between 33%, 43%, and 53% in the single‐payer models and between 27%, 50%, and 63% in the multi‐payer models (Table 3). BIR costs under intermediate single payer are 1.58 higher than costs under multi‐payer contractual and architectural simplification.
TABLE 3.
Estimated policy impact on total BIR costs
| Policy scenario | Contractual complexity as a fraction of baseline, ratio | Compliance costs as a fraction of baseline, ratio | Number of contracts per provider, mean [interquartile range] | Fraction of contracts negotiated annually, mean [interquartile range] | National BIR Costs, billion (change, %) |
|---|---|---|---|---|---|
| Current state | 1 | 1 |
1000 [100, 10 000] |
0.25 | $111.4 (0) |
| Single payer (optimistic) | 1 | 1 | 1, [1,1] | 1 | $52.5 (–53) |
|
Single payer (intermediate) |
1.1 | 1.1 | 1, [1,1] | 1 | $63.5 (–43) |
| Single payer (pessimistic) | 1.2 | 1.2 | 1, [1,1] | 1 | $75.6 (–33) |
|
Multi‐payer Contract complexity |
0.5 | 1 |
1000 [100, 10 000] |
0.25 | $55.7 (−50) |
|
Multi‐payer Architectural complexity |
1.0 | 1 | 500 [50, 5000] | 0.25 | $81.7 (–27) |
| Multi‐payer contract complexity and architectural complexity | 0.5 | 1 | 500 [50, 5000] | 0.25 | $40.9 (–63) |
Since we allow for heterogeneity across providers in the number and complexity of contracts to which they agree, changes in BIR costs for different providers vary across the different reform proposals. These differences depend on the number of contracts into which they enter and each providers’ ratio of variable costs to fixed costs. For all scenarios and across all sensitivity analyses, savings were highest when the ratio of fixed to variable costs, s, was increased and the ratio of clinical to nonclinical documentation costs, r, was decreased; similarly, savings were lowest when s was decreased and r was increased (Figure 1). This is because the reforms are positively correlated with fixed costs and nonclinical documentation costs. Across sensitivity analyses, single payer saw a larger range of savings (31.4%‐55.0% for intermediate scenario) than multi‐payer reform (60.9%‐65.8% for both contractual and architectural simplification) (Tables S5).
FIGURE 1.
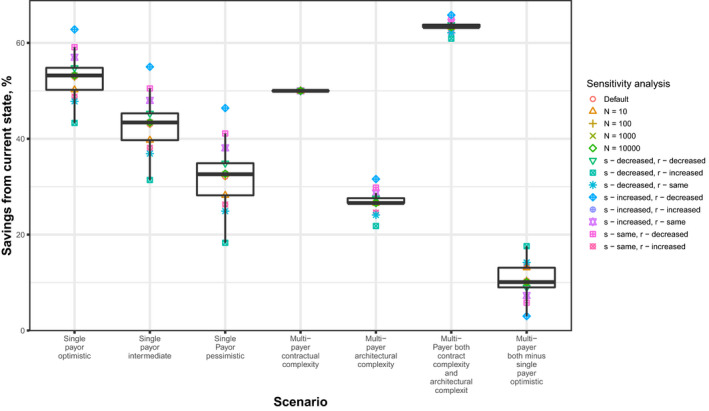
BIR Costs Under Alternative Policy Proposals and Sensitivity Analyses. Reduction in BIR costs under alternative policy proposals and sensitivity analyses (detailed in Appendix S2). In the single‐payer model, compliance costs were assumed to increase 10% in the intermediate model from the current state, 0% in the optimistic model, and 20% in the pessimistic model. In the contract complexity model, contract complexity was reduced by 50% from the current state, in the architectural complexity model the number of plans were reduced by 50%, and in the contract complexity and architectural complexity model both elements were reduced by 50%. The last column shows the difference in savings between the contract complexity and architectural complexity and the single‐payer optimistic models
In the multi‐payer model, reductions in contractual complexity and in architectural complexity lead to national savings that scale with the magnitudes of the reductions. The savings may be smaller, equal to, or larger than savings achieved by variants of single payer depending on the variants of the specific policy (Figure 2A). Reductions of 50% in architectural complexity and in contractual complexity correspond to 27% and 50%, reductions in national BIR costs, respectively. This is because reductions in contractual complexity lower the cost of billing for every patient visit, while reductions in architectural complexity have a smaller impact on providers with fewer contracts and higher clinical documentation costs. National savings from single‐payer models depend on curbing the growth in compliance costs and contractual complexity. If these costs increase significantly, then the savings associated with the single‐payer model are significantly lower than savings under multi‐payer reform (Figure 2B). The ratio of provider‐specific BIR costs under intermediate single payer to BIR costs under multi‐payer reform depend on provider characteristics. This ratio is lower for providers with more contracts and higher for providers with a higher ratio of clinical to nonclinical documentation costs (Figure 2C).
FIGURE 2.
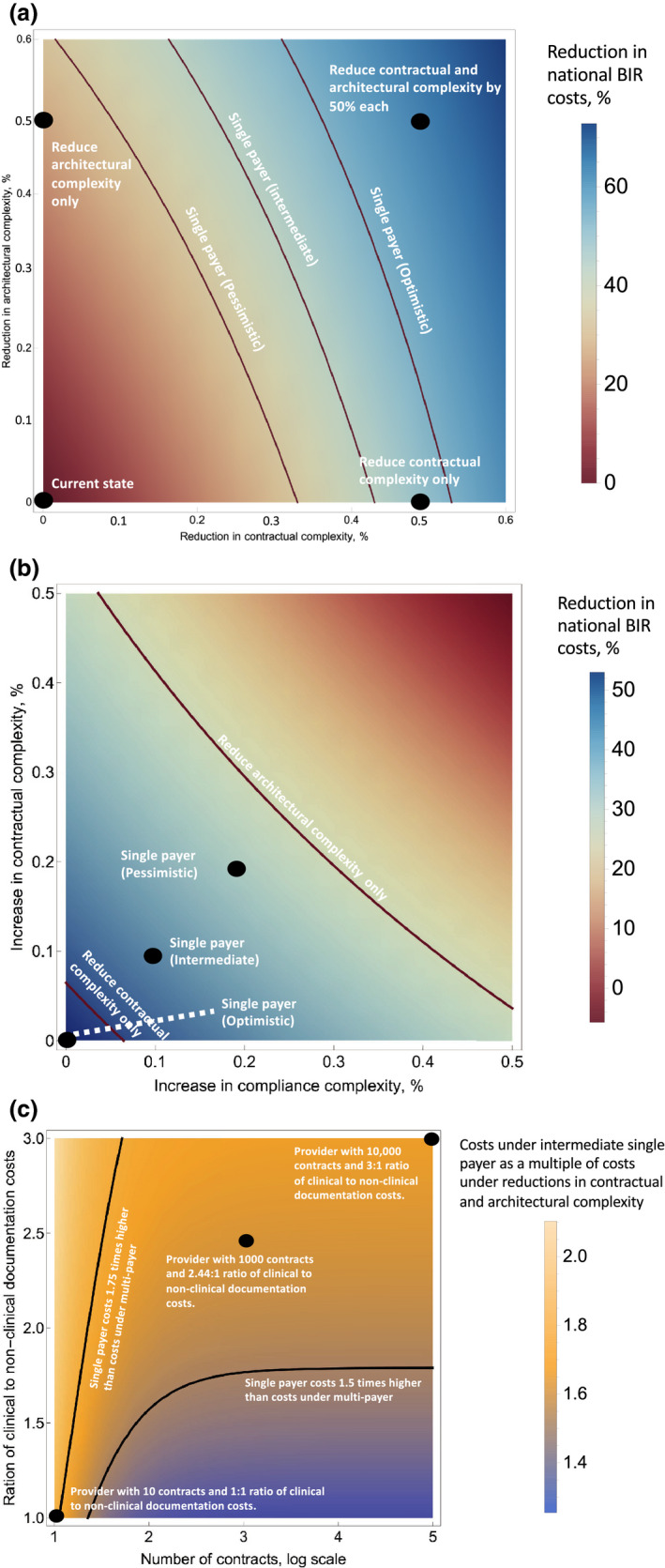
A, Reduction in national BIR costs under variants of multi‐payer reform. The colors correspond to the percent reduction in national BIR costs associated with multi‐payer reform in which the architectural complexity and contractual complexity are reduced by the percents on the x and y axes. The black dots correspond to current state and the variants of multi‐payer reform listed in Table 2. The lines correspond to the variants of single payer listed in Table 2. Each line is composed of the points for which the savings from that variant of single payer equal the savings from the corresponding multi‐payer reform. For example, the middle “Intermediate” Single Payer is composed of the points corresponding to the variants of multi‐payer reform that result in 43% savings in national BIR costs. B, Reduction in national BIR costs under variants of single‐payer reform. The colors correspond to the percent reduction in national BIR costs associated with single‐payer reform in which contractual complexity and compliance costs increase by the percents on the x‐ and y‐axes, respectively. The black dots correspond to the variants of single‐payer reform listed in Table 2. The lines correspond to the variants of multi‐payer listed in Table 2. Each line is composed of the points for which the savings from that variant of multi‐payer reform equal the savings from the corresponding single‐payer reform. For example, the top multi‐payer architectural complexity reduction only line is composed of the points corresponding to the variants of single reform that result in 27% savings in national BIR costs. C, Ratio of national BIR costs under intermediate single payer to BIR costs under variants of multi‐payer reform. The contours represent providers for whom BIR costs under intermediate single payer are a constant multiple of BIR costs under multi‐payer reductions to contractual and architectural complexity. The black dots correspond to the providers whose number of contracts and ratio of clinical to nonclinical documentation costs correspond to values used in the sensitivity analyses
3.1. Policy implications
Non‐value‐added transaction costs impose a heavy financial burden on the US health sector. Moreover, complexity feeds upon itself, as our system's burdensome thicket of contractual complexity offers perverse profit opportunities to both payers and providers. Providers often purchase software that combs through the interstices of complex payment arrangements to maximize revenue. Similarly, payers purchase their software to minimize payments. Some software vendors service both sides. And each side's search for marginal savings makes wholesale and mutually beneficial simplification more elusive.
Nonetheless, creative reforms to reduce administrative burdens—and careful assessments of those reforms—have been lacking because policy makers, industry leaders, and the health service research community have not precisely identified the specific causes of those costs. Our model provides one approach to understanding how BIR costs arise and thereby allows an assessment of alternative policy approaches for reducing them. In our analysis, both single‐payer models and reforms of the current multi‐payer health insurance model can achieve significant reductions in BIR costs. Under a broad range set of modeling assumptions, reforms to the current multi‐payer market achieve greater savings than transforming the sector to a single‐payer system, especially variants of single payer that significantly increase contractual complexity or the burden of legal compliance.
Policy experts ought not accept high transaction costs as an inevitable consequence of financing health care with third‐party private insurance. Other sectors—ranging from real estate to financial derivatives trading—have successfully reduced industry‐wide transaction costs. Our simulation suggests that the US health sector can meaningfully reduce BIR costs by mimicking the strategies pursued by other industries.
3.2. Contract complexity
Assorted payment models can bring greater simplicity to payer‐provider contracts. Global budgets or capitated payment models, for example, would avoid expensive coding and the time‐consuming categorization of services. Eliminating preauthorizations, which have come under persistent criticism, would reduce the time clinicians spend in documenting conditions and treatments. 14 More simply, making payments insensitive to comorbidities—and eliminating the temptation to upcode—might also reduce contract‐related BIR costs. These are reforms that individual payers and providers could pursue, particularly as narrow networks or integrated systems are formed.
3.3. Architectural complexity
The group health insurance model in the United States seems to be unique to the degree that health insurance is “customized” for individual employer clients. The health insurance sales model drives this approach to differentiation of health plan sponsors while externalizing the costs of the resulting architectural complexity to providers. An alternative approach, one pursued by many other industries, would be to standardize health plans that can be offered in the market. This strategy reduces the costs of negotiation and drafting contracts, routinizes ongoing multi‐party relations, and mitigates switching costs thereby lowering barriers to competition. The health sector fruitfully experimented with standardized contracts with Medicare Supplemental plans under OBRA 1990 15 and the individual insurance market under the ACA. 16
Industry leaders could take the initiative by agreeing to standardized payer‐provider contracts. The industry‐led model has been successfully implemented in similar markets. Alternatively, state‐based nonprofit entities or collaboratives could provide a common framework for creating and administering payment contracts. California's Integrated Healthcare Association, for example, manages and updates provider networks for each of the state's insurance products. 17 It has done so cost‐effectively by standardizing the templates for updating networks and centralizing administrative procedures. A third path could be led by state insurance commissioners, who have the authority and responsibility to approve payer‐provider contracts. Although the authority enjoyed by insurance commissioners varies by state, most would have the knowledge and skill to facilitate a state‐wide convergence to standardized contracts.
One lingering question about a single‐payer model is whether such a plan would allow for the continuation of private health plans serving the public payers, (34% of Medicare beneficiaries 17 and 71% of Medicaid beneficiaries are in private health plans 18 ). If these plans are not required to pursue a standardized contract strategy, then a single‐payer model could fail to achieve its anticipated savings.
3.4. Compliance
Hospitals spend $39 billion annually, or $1200 per admitted patient, on regulatory compliance, two‐thirds of which is related to participation adherence and BIR costs. 19 Standardized contracts would increase the effectiveness of automated fraud detection and could reduce compliance costs by limiting the number of providers subject to the highest level of scrutiny (one study with a simple algorithm detected only 3% of providers that were of potential concern over billing activities 20 ).
All of the multi‐payer models assume the equal participation of the public programs in the market reform effort. Further, since plans offered by self‐insured employers are exempt from state regulation under ERISA, federal regulation may be required to achieve the savings we estimate.
3.5. Differential impact based on provider size
Providers that have fewer contracts and relatively high clinical documentation costs, and thus relatively low overhead costs, see significantly smaller benefits under single payer, especially in simulations in which contractual complexity and the legal burden increase. In contrast, since contract simplification reduces the cost of clinical‐documentation for all visits, the benefits accrue to all providers independently of size.
We recognize the limitations of our approach. Our model was developed based on extrapolations from BIR activities at a single clinical site. The visit types were based on the data reported by Tseng. Absent significant structural differences in the billing processes for other types of visits, for example, specialty office visits, these modeled results should apply. While the model was robust to our sensitivity analysis, there may be other unmeasured factors which have an influence on these costs. While a single‐payer system with simpler contracts and lower burdens of legal compliance would provide far greater savings in BIR costs than any of the models presently considered, the present work considers only one type of single‐payer model, Medicare‐for‐All that expands access to fee‐for‐service Medicare and inherits the contractual complexity of traditional Medicare (this final assumption appears reasonable even to advocates of a single‐payer model, who concede that “poorly designed (single payer) legislation might perpetuate Medicare's burdensome payment and monitoring strategies.” 21 ). This contrasts with single‐payer systems such as those in Canada that exhibit simpler billing procedures but subject new technologies to heavier regulated oversight and feature longer wait times than in the United States for certain procedures. Further work is necessary to expand the model presented to study single‐payer scenarios based on other nations. This work considers only costs paid by providers. Subsequent work is necessary to expand this model to consider the significant administrative costs placed on the insurer and the patients/enrollees. In other respects, our model also overlooks certain differences between single‐payer and private systems. For example, some states manage their Medicaid bills by delaying payment to providers. Such measures, which reduce public administrative costs at the expense of the providers, are unaccounted for here and should be examined in future studies. Finally, though we recognize that providers currently enter into different numbers and kinds of contracts, we do not allow providers to adjust to the listed reforms differently. Our simulation builds off what little data are available and aims to encourage serious investigation into alleviating the BIR costs that heavily burden our current system. We do not represent our simulations as a comprehensive evaluation of single‐payer reform.
4. CONCLUSION
The costs of administering the current health insurance system have attracted long‐overdue attention in policy debates. We highlight the origins of these costs and consider specific mechanisms in which they can be reduced. We confirm the suggestion of many that a single‐payer scheme exhibits lower administrative costs than our current system, but we also explore how administrative reforms to our multi‐payer system could achieve similarly beneficial results. Since reforming the structure of the multi‐payer health insurance market would be less disruptive to patients than a single‐payer model, reforms that reduce BIR costs while keeping intact multi‐payer health insurance could be especially attractive.
Simplifying and standardizing payer‐provider contracts are no panacea for our health system. Moreover, it will impose costs on some: it would lead to fewer hours for lawyers, less authority for bill collectors, and smaller managerial kingdoms for hospital revenue departments. But reducing administrative costs, which translate into savings for patients and fiscally strapped governments without affecting the quality or quantity of care, is as close to a win‐win reform as there is in a health policy world comprised mostly of tradeoffs. We encourage future work in this area, both because potential savings are substantial and because they such savings are virtually unassailable.
Supporting information
Supplementary Material
Appendix S1
Appendix S2
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: Arnold Milstein serves as the unpaid Medical Director of the Pacific Business Group on Health, a coalition of self‐insured employers. The coalition within the last 5 years has made charitable contributions to Stanford University for the benefit of a Stanford research center led by Professor Milstein. Dr Schulman, Professor Scheinker and Professor Richman have all been affiliated with the center. These gifts are not allocated to support the compensation of Professor Milstein.
Scheinker D, Richman BD, Milstein A, Schulman KA. Reducing administrative costs in US health care: Assessing single payer and its alternatives. Health Serv Res. 2021;56:615–625. 10.1111/1475-6773.13649
REFERENCES
- 1. Tseng P, Kaplan RS, Richman BD, Shah MA, Schulman KA. Administrative costs associated with physician billing and insurance-related activities at an academic health care system. Jama. 2018;319(7):691‐697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Himmelstein DU, Jun M, Busse R, et al. A comparison of hospital administrative costs in eight nations: U.S. costs exceed all others by far. Health Aff. 2014;33(9):1586‐1594. [DOI] [PubMed] [Google Scholar]
- 3. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA. 2019;322(15):1501‐1509. 10.1001/jama.2019.13978 [DOI] [PubMed] [Google Scholar]
- 4. Himmelstein DU, Jun M, Busse R, et al. A comparison of hospital administrative costs in eight nations: US costs exceed all others by far. [DOI] [PubMed] [Google Scholar]
- 5. Woolhandler S, Campbell T, Himmelstein DU. Costs of health care administration in the United States and Canada. N Engl J Med. 2003;349(8):768‐775.PubMed PMID: 12930930 [DOI] [PubMed] [Google Scholar]
- 6. Morra D, Nicholson S, Levinson W, Gans DN, Hammons T, Casalino LP. US physician practices versus Canadians: spending nearly four times as much money interacting with payers. Health Aff (Millwood). 2011;30(8):1443‐1450. 10.1377/hlthaff.2010.0893 [DOI] [PubMed] [Google Scholar]
- 7. Cutler DM. Reducing Administrative Costs in Healthcare. The Hamilton Project. https://www.blueshieldca.com/bsca/bsc/wcm/connect/provider/provider_content_en/guidelines_resources/overview. Accessed February 6, 2021. [Google Scholar]
- 8. Kahn JG, Kronick R, Kreger M, Gans DN. The cost of health insurance administration in california: estimates for insurers. Phys Hosp Health Affairs. 2005;24(6):1629‐1639. [DOI] [PubMed] [Google Scholar]
- 9. Sakowski JA, Kahn JG, Kronick RG, Newman JM, Luft HS. Peering into the black box: billing and insurance activities in a medical group. Health Aff. 2009;28(Suppl. 1):w544‐w554. [DOI] [PubMed] [Google Scholar]
- 10. Casalino LP, Nicholson S, Gans DN, et al. What does it cost physician practices to interact with health insurance plans? Health Aff. 2009;28(Suppl. 1):w533‐w543. [DOI] [PubMed] [Google Scholar]
- 11. Kahn JG, Kronick R, Kreger M, Gans DN. The cost of health insurance administration in California: estimates for insurers. Phys Hosp Health Affairs. 2005;24(6):1629‐1639. [DOI] [PubMed] [Google Scholar]
- 12. https://www.blueshieldca.com/bsca/bsc/wcm/connect/provider/provider_contenten/guidelines_resources/overview. Accessed February 6, 2021.
- 13. Woolhandler S, Himmelstein DU. Single‐payer reform—“medicare for all”. JAMA. 2019;321(24):2399‐2400. 10.1001/jama.2019.7031 [DOI] [PubMed] [Google Scholar]
- 14.“Concensus Statement on Improving the Prior Authorization Process, https://www.ama‐assn.org/sites/default/files/media‐browser/public/arc‐public/prior‐authorization‐consensus‐statement.pdf; plus 2 articles against prior auth in JAMA; Resneck JS. Refocusing Medication Prior Authorization on Its Intended Purpose. JAMA. Published online February 03, 2020. doi:10.1001/jama.2019.21428. Accessed February 6, 2021. [DOI] [PubMed] [Google Scholar]
- 15. https://oig.hhs.gov/oei/reports/oei‐09‐93‐00230.pdf. Accessed February 6, 2021.
- 16. https://www.healthcare.gov/choose‐a‐plan/plans‐categories/. Accessed February 6, 2021.
- 17. https://www.iha.org/. Accessed February 6, 2021.
- 18. https://www.kff.org/medicare/issue‐brief/a‐dozen‐facts‐about‐medicare‐advantage‐in‐2019/. Accessed February 6, 2021.
- 19. https://www.healthaffairs.org/do/10.1377/hblog20180430.387981/full/. Accessed February 6, 2021.
- 20. https://www.aha.org/guidesreports/2017‐11‐03‐regulatory‐overload‐report
- 21. Fang H, Gong Q. Detecting potential overbilling in medicare reimbursement via hours worked. Am Econ Rev. 2017;107(2):562‐591. [DOI] [PubMed] [Google Scholar]
- 22. https://www.cms.gov/Research‐Statistics‐Data‐and‐Systems/Statistics‐Trends‐and‐Reports/NationalHealthExpendData/NationalHealthAccountsProjected. Accessed February 6, 2021.
- 23. Centers for Disease Control . https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed February 6, 2021.
- 24. Centers for Disease Control . https://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2010_ed_web_tables.pdf. Accessed February 6, 2021.
- 25. Centers for Disease Control . https://www.hcup‐us.ahrq.gov/reports/statbriefs/sb223‐Ambulatory‐Inpatient‐Surgeries‐2014.pdf. Accessed February 6, 2021.
- 26. Centers for Disease Control . https://www.cdc.gov/nchs/data/nhsr/nhsr102.pdf: https://www.cdc.gov/nchs/data/hus/2017/082.pdf. Accessed February 6, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Appendix S1
Appendix S2


