Abstract
Objective
To estimate the impact of urgent care centers on emergency department (ED) use.
Data Sources
Secondary data from a novel urgent care center database, linked to the Healthcare Cost and Utilization Project State Emergency Department Databases (SEDD) from six states.
Study Design
We used a difference‐in‐differences design to examine ZIP code‐level changes in the acuity mix of emergency department visits when local urgent care centers were open versus closed. ZIP codes with no urgent care centers served as a control group. We tested for differential impacts of urgent care centers according to ED wait time and patient insurance status.
Data Collection/Extraction Methods
Urgent care center daily operating times were determined via the urgent care center database. Emergency department visit acuity was assessed by applying the NYU ED algorithm to the SEDD data. Urgent care locations and nearby emergency department encounters were linked via zip code.
Principal Findings
We found that having an open urgent care center in a ZIP code reduced the total number of ED visits by residents in that ZIP code by 17.2% (P < 0.05), due largely to decreases in visits for less emergent conditions. This effect was concentrated among visits to EDs with the longest wait times. We found that urgent care centers reduced the total number of uninsured and Medicaid visits to the ED by 21% (P < 0.05) and 29.1% (P < 0.05), respectively.
Conclusions
During the hours they are open, urgent care centers appear to be treating patients who otherwise would have visited the ED. This suggests that urgent care centers have the potential to reduce health care expenditures, though questions remain about their net cost impact. Future work should assess whether urgent care centers can improve health care access among populations that often experience barriers to receiving timely care.
Keywords: emergency departments, health care access, health care costs, urgent care
What is Already Known on This Topic
Urgent care centers may offer a lower‐cost care setting for some conditions that might otherwise have been treated in an emergency department
Despite the impact the urgent care market could have on health care costs and access, few studies have estimated how it affects emergency department use
What This Study Adds
Urgent care centers reduce costly nonemergent ED visits during the hours they are open, especially among Medicaid enrollees and uninsured individuals, and in areas with long ED visit wait times.
Urgent care centers appear to improve care access for certain populations, but more work is needed to determine their impact care costs and outcomes
1. INTRODUCTION
Reducing nonurgent emergency department (ED) use is a well‐known—yet elusive—health policy goal. According to the most recent National Hospital Ambulatory Medical Survey, 28% of ED visits in 2017 were neither urgent nor emergent, though most prior studies suggest this number is upwards of 30%. 1 , 2 , 3 , 4 , 5 , 6 , 7 Given the high expense associated with ED care, substantial savings could be achieved if nonemergent patients were treated in less costly care settings. 8
Urgent care centers are a particularly suitable alternative to the ED for nonemergent visits. Comprising an $18 billion industry, urgent care centers are freestanding facilities that provide treatment for injuries or illnesses that are not life or limb threatening, but are beyond the scope or availability of primary care facilities. 9 , 10 Fifty‐seven percent of Americans report difficulty with same or next day access to health care appointments, and 63% of patients with primary care providers report difficulty with access on evenings, weekends, and holidays. 11 When primary care providers are unavailable during these times, patients often turn to the ED, which is always open. Individuals with greater difficulty in accessing primary care physicians after hours have more ED visits compared to those who have an easier time reaching their primary care provider. 12 By offering extended weeknight and weekend hours, as well as many services not available in PCP offices, urgent care centers might be treating patients who otherwise would have sought care in the ED. Annually, an estimated 36 million ED visits could be shifted to urgent care centers, where care is 10 times less expensive than that delivered in the ED. 8 , 13 , 14 , 15 , 16 , 17
Though urgent care centers could substantially improve healthcare access and reduce costs, studies on their effect on ED demand are conspicuously lacking. In part, this is because there are no reliable data sources that contain the years that urgent care centers opened or closed in a given area, which precludes the use of traditional panel‐data methods to determine their causal impact on health care use. We overcome this limitation by using daily operating times of urgent care centers to examine how ED demand changes in their presence (when they are open) or absence (when they are closed).
This paper contributes to the literature in several ways. First, we describe a novel dataset that contains detailed information on the locations and operating hours of US urgent care centers. Second, we conduct a difference‐in‐differences analysis that estimates how urgent care centers affect ED demand. If urgent care centers are effectively substituting for EDs, we would expect a decrease in nonemergent ED visits during the hours the clinics are open. Next, we assess whether the impact of urgent care centers varies according to local ED wait times, as nonurgent patients visiting more crowded EDs have a greater incentive to use urgent care centers to avoid long waits. Finally, we test whether the impact of urgent care centers is moderated by patient insurance status, which provides useful information for policy makers aiming to improve access and reduce costs among the most vulnerable populations.
1.1. The urgent care market
Research indicates that anywhere from 13% up to half of the 137 million annual US ED visits could be treated at a care site other than the ED. 4 , 8 , 18 , 19 A major barrier to treating these visits in more clinically appropriate settings is limited access to acute primary care in the community, due to physician shortages, long wait times for appointments, and/or a lack of after‐hours availability. 3 , 20 , 21 , 22 , 23 , 24
Urgent care centers provide a potential alternative care setting for many acute, nonemergent conditions. In addition to primary care services, practitioners at these facilities can provide immunizations, laboratory tests, X‐rays, fracture and laceration care, and intravenous fluids. 10 More than 9200 urgent care clinics are in operation, with about 122 million annual patient visits (an average of 44 patients a day per facility). 9 , 10 , 25 , 26 , 27 In comparison, the 4200 EDs in the US host 137 million visits per year (an average of 89 patients a day per facility), and 1,800 retail clinics see only 10.5 million annual visits (an average of 16 patients a day per facility). 28 , 29
The Urgent Care Association of America delineates urgent care centers from other delivery models based on whether a facility (a) is open on weekday evenings and on weekends, (b) does not require an appointment, (c) has onsite X‐ray, and (d) has the ability to perform suturing and casting procedures. 25 Beyond these attributes, services offered in an urgent care center can vary widely, from primary care to less common offerings, such as occupational medicine, weight loss, and physical therapy services. 25 , 30
Though data limitations have made it difficult to conduct research on urgent care centers, there is a slightly more established—albeit mixed—literature on retail clinics, for which data are more readily available. Retail clinics differ from urgent care centers in that they are located within a retail location (rather than operating as stand‐alone entities), are much more limited in number, are primarily staffed by nurse practitioners (rather than MDs), treat a smaller set of routine/minor conditions, have fewer clinical resources, and have lower out‐of‐pocket costs for patients. 31 , 32 , 33 , 34 However, they do share some similarities with urgent care centers, including walk‐in availability and later hours of operation.
Alexander, Currie, and Schnell found that individuals living near a retail clinic are between 4.7 and 11.4% less likely to go to the ED for minor illnesses. 35 Further, they estimated that expanding the retail clinic market across the state could save $70 million annually from reduced ED use. Hollingsworth found that retail clinics decreased the number of ED visits for bronchitis and upper respiratory infection. 36 In contrast, Martsolf et al found no impact of retail clinic penetration on low‐acuity ED visits. 37 Given their small market size and the limited scope of services and resources they offer, retail clinics are not as close a substitute for the ED as urgent care centers are. For example, urgent care centers offer diagnostic imaging and laceration repair, both of which are not provided in retail clinics. 9 This underscores the need for urgent care‐specific research.
2. METHODS
For this observational difference‐in‐differences study, we used a novel database that contains the names, addresses, and hours of operations for almost all the urgent care centers in the United States. The dataset came from an online searchable database (previously called urgentcarelocations.com, now called solvhealth.com) that allows patients to view urgent care centers within a certain distance of their ZIP code. It is the most comprehensive, independently verified directory of walk‐in clinics in the country, with over 90% of clinics indexed. 38 , 39 The 2012‐2013 edition of the database, which was provided for this study, contained 6655 urgent care centers, which was in line with numbers released from industry trade organization estimates at that time. 40
Our analytic approach leveraged the hours‐of‐operation data to assess how the acuity mix of ED visits changed when urgent care centers were open. An acuity mix can be thought of as the share of ED visits that are nonemergent versus those that are more emergent. When patients need nonemergent care and are unable to visit a PCP, they can choose to visit either the ED or—if available—an urgent care center. Urgent care center availability requires both geographic proximity to a patient, as well as being open at the time care is needed. The intuition behind our approach is that when urgent care centers are open, patients have an ED alternative available to them and thus would be less likely to visit the ED for nonemergent conditions. We therefore examined how the number of nonurgent versus emergent ED visits changed among people who live near (ie, in the same ZIP code as) urgent care centers when their local clinic is open versus closed. We used those who live in ZIP codes without any urgent care centers as a control group.
Our data on ED visits came from the 2012 Healthcare Cost and Utilization Project (HCUP) State Emergency Department Databases (SEDD), the largest collection of all‐payer, encounter‐level US ED visit data. 41 The data included patient and visit characteristics, such as patient ZIP code, insurance status, discharge code (ICD‐9), and hour of ED visit (arrival time, not admission time). Six states (AZ, FL, NE, NJ, NY, RI) included all the variables necessary to implement our analysis and comprised our study population. Our ED data did not provide the day of the week on which a visit occurred; it only provided whether the visit occurred on a weekday or weekend. Urgent care center hours tend to be very consistent from Monday through Friday, but change markedly from the work week to Saturday, and then again from Saturday to Sunday. For this reason, we excluded weekend visits from our analysis. Due to over‐coding of visits occurring in the midnight hour, we also excluded the 4.3% of visits that were listed as occurring between 12 and 1 am.
To determine the number of more or less emergent ED visits in each ZIP code, we used an updated version of the NYU ED visit algorithm, which classifies the urgency, preventability, and optimal care site of ED visits. 42 , 43 , 44 , 45 Using the primary diagnosis code for a given ED visit, the algorithm assigns the probability of the visit falling into each of four categories: (a) not urgent; (b) urgent, but primary care treatable; (c) emergent, ED care needed, but preventable/avoidable; (d) emergent, ED care needed, not preventable/avoidable. 43
The probability distribution across the four categories reflects the variability of possible urgency levels within any single code. For example, though strep throat is largely considered a nonurgent event, it can—in rare cases—require emergency care. In the NYU ED algorithm, a diagnosis of strep throat has the following probability distribution: nonurgent, 66%; urgent, primary care treatable, 28%; emergent, ED care needed, 6%; emergent, ED care needed, not preventable/avoidable, 0%. For the purpose of this study, these percentages can be thought of as fractions of visits (eg, a visit that has 66% chance of being nonurgent counts as 6.6/10 of a nonurgent visit).
We first applied the NYU ED algorithm to each visit's diagnosis code to get the acuity distribution for the visit. Next, we broke out all the ED visit records according to the patient's home ZIP code and the hour of their visit. We summed the fractions of ED visits for patients from each ZIP code‐hour combination to get the mean number of total visits across each algorithm category for each group. Then, we used the urgent care address data to determine whether a patient's ZIP code had an urgent care center or not. We used the urgent care center hours data to determine whether the clinic was open during the time the patient visited the ED. This procedure yielded three groups of ED patients for each hour of the day: those with no urgent care center in their home ZIP code, those with an urgent care center in their home ZIP code that was closed at the time of their visit, and those with an urgent care center in their home ZIP code that was open at the time of their visit.
We used a quasi‐experimental differences‐in‐differences design, with a two‐way fixed effects model:
| (1) |
where is the ZIP code aggregated outcome of interest among ED patients living in ZIP code at hour are ZIP code fixed effects; are hourly fixed effects; and represents a random error term. The key independent variable is an indicator equal to one if ZIP code had an urgent care center and the urgent care center was open at hour .
We ran the above model for each acuity category in the NYU ED algorithm, as well as the overall number of ED visits, analyzed at the ZIP‐hour level. For example, our first outcome was the mean number of nonurgent ED visits made by patients living in each ZIP code at a given hour. All analyses used an ordinary least squares model, weighted by the number of ED visits from each ZIP in each hour. Standard errors were clustered at the ZIP code level.
To trace out the time course of the changes in ED visits, we next conducted event study analyses, replacing the interaction term in Equation (1) with terms for having an urgent care center in ZIP code, interacted with the number of hours from urgent care closure that a given ED visit took place. We expected that urgent care center closure would increase the number of nonurgent visits to EDs, but that this effect would lessen over time.
Then, to assess whether urgent care centers play a larger role among patients who visit EDs with long wait times, we ran our original model (1) on the subset of patients who lived in ZIP codes that had an ED within the ZIP, stratified by quartiles of ED wait time. We hypothesized that patients living in ZIP codes with more crowded EDs (ie, longer wait times) might be more likely to substitute to an urgent care center, rather than waiting for a long time at the ED. The ED wait time data for this analysis came from the 2013 Hospital Compare database, made publicly available by the Centers for Medicare and Medicaid Services. 46
We finally tested for differential effects by stratifying our sample by payer type. We aggregated individual‐level ED visit data to the ZIP code‐hour‐insurance status level, then reran the model from (1). Unlike EDs, urgent care centers are not bound under the Emergency Medical Treatment and Labor Act (EMTALA) to treat all patients, regardless of their ability to pay. 47 As such, urgent care centers and EDs have different payer mixes. Uninsured patients comprise only a small fraction (7%) of UCC visits, but make up 1/5 of ED visits. 48 , 49 Given these numbers, we expected urgent care operating hours to have a larger effect for patients who are insured.
3. RESULTS
In Table 1, we present summary statistics for ZIP codes with and without urgent care centers. In our study states, 15.3% of ZIP codes had at least on least one urgent care center. These areas tended to be more populous, with younger and more racially diverse residents, and with higher median household incomes. Rates of insurance were also lower among these ZIP codes.
TABLE 1.
Summary statistics for ZIP codes with and without urgent care centers
| Without any urgent care center | With at least one urgent care center | |
|---|---|---|
| Total population (n) | 12 641 | 29 782*** |
| Age (median) | 42.1 | 40.7*** |
| Non‐Hispanic white (%) | 74.7 | 65.4*** |
| Household income (median) | $28 977 | $31 095*** |
| Did not earn high school degree (%) | 12.7 | 11.5*** |
| Uninsured (%) | 13.4 | 14.3** |
| Observations (5460) | 4625 (84.7%) | 835 (15.3%) |
Significance stars reflect results from means comparisons tests.
P < 0.05
P < 0.01
P < 0.001.
Source: Author analysis of American Community Survey Data.
Our final ED visit sample yielded 8.5 million visits made across the six states in our data year. The number of visits ranged widely across ZIP‐hours. For instance, residents from Jefferson County, NY (13601) visited an ED 5352 times between 7 and 8 AM over the year—about 12 visits during that hour on any given day. In contrast, residents from Albion, RI (02802) visited an ED only three times during that hour over the course of an entire year.
Table 2 presents results from our main difference‐in‐differences analysis. The coefficient in Equation (1) is presented for total ED visits, as well as each of the four acuity outcomes. On average, residents from each ZIP code visited the ED 161 times per hour over the course of the year. Having an urgent care center in a ZIP code reduced this number by 27.7 visits (P < 0.05), a relative decrease of 17.2%, during the hours the urgent care center was open.
TABLE 2.
Impact of urgent care center operating on number of emergency department visits, by acuity level
| n = 102 313 | Total visits | Nonurgent | Urgent, primary care treatable | Emergent, avoidable | Emergent, not avoidable |
|---|---|---|---|---|---|
| UCC in ZIP * UCC open | ‒27.68* | ‒14.27* | ‒8.555 | ‒3.552** | ‒1.301 |
| (SE) | (13.68) | (6.074) | (4.524) | (1.250) | (1.949) |
| Baseline | 160.9 | 52.80 | 58.29 | 17.30 | 32.51 |
| Relative change (%) | ‒17.2 | ‒27.03 | ‒14.68 | ‒20.53 | ‒4.00 |
Author analysis of State Emergency Department Databases for AZ, FL, NE, NJ, NY, and RI. Stars represent statistical significance.
P < 0.05
P < 0.01
P < 0.001.
Turning next to the different levels of acuity, we find the largest reduction in nonurgent visits, which decrease by 14.3 visits (P < 0.05), or 27%. This is in line with our hypothesis that when urgent care centers are open, nonurgent ED visits will decrease. We do not detect a statistically change in the number of urgent primary care treatable visits, nor in unavoidable emergency visits. We do find, however, a 3.6 visit (P < 0.01) reduction in the number of avoidable emergent cases.
Table 3 shows results by quartile of ED wait time. We found no effect of urgent care center operation on ED visits made to hospitals with wait times in the first through third quartiles. However, when we examined results from EDs with the longest wait times (mean 68 minutes), we found that urgent care centers reduced the total number of ED visits by 208.4 (P < 0.001), a relative decrease of 76.3%. Though this effect is most prominent among nonurgent visits (a reduction of 92.6 visits, P < 0.001), we also found large, statistically significant reductions across all visit acuity levels, including those that are considered most emergent.
TABLE 3.
Impact of urgent care center operating on number of emergency department visits, by acuity level and quartile of emergency department wait time
| Total visits | Nonurgent | Urgent, primary care treatable | Emergent, avoidable | Emergent, not avoidable | |
|---|---|---|---|---|---|
| 1st Quartile | |||||
| µ = 14.7 min | |||||
| n = 2330 | |||||
| UCC in ZIP * UCC open | ‒6.102 | ‒3.284 | ‒2.074 | ‒0.563 | ‒0.181 |
| (SE) | (22.02) | (8.555) | (8.115) | (2.095) | (3.702) |
| Baseline | 139.9 | 44.37 | 51.94 | 14.02 | 29.53 |
| Relative change (%) | ‒4.36 | ‒7.4 | ‒3.99 | ‒4.02 | ‒0.61 |
| 2nd Quartile | |||||
| µ = 24.9 min | |||||
| n = 1849 | |||||
| UCC in ZIP * UCC open | ‒8.964 | ‒6.461 | ‒1.237 | ‒0.203 | ‒1.063 |
| (SE) | (19.99) | (8.186) | (6.722) | (1.883) | (3.774) |
| Baseline | 155.6 | 49.92 | 56.48 | 15.76 | 33.42 |
| Relative change (%) | ‒5.76 | ‒12.94 | ‒2.19 | ‒1.29 | ‒3.18 |
| 3rd Quartile | |||||
| µ = 35.4 min | |||||
| n = 2451 | |||||
| UCC in ZIP * UCC open | ‒26.45 | ‒9.384 | ‒9.845 | ‒3.943 | ‒3.276 |
| (SE) | (38.07) | (17.20) | (13.03) | (3.186) | (5.832) |
| Baseline | 232.8 | 74.61 | 84.87 | 25.75 | 47.54 |
| Relative change (%) | ‒11.36 | ‒12.58 | ‒11.6 | ‒15.31 | ‒6.89 |
| 4th Quartile | |||||
| µ = 67.8 min | |||||
| n = 3178 | |||||
| UCC in ZIP * UCC open | ‒208.4*** | ‒92.61*** | ‒67.96*** | ‒22.04*** | ‒25.79** |
| (SE) | (60.57) | (26.94) | (19.74) | (6.002) | (8.312) |
| Baseline | 273.2 | 93.13 | 96.64 | 31.75 | 51.64 |
| Relative change (%) | ‒76.28 | ‒99.44 | ‒70.32 | ‒69.42 | ‒49.94 |
Author analysis of State Emergency Department Databases for AZ, FL, NE, NJ, NY, and RI. Stars represent statistical significance.
P < 0.05
P < 0.01
P < 0.001.
In Table 4, we stratified our analysis by payer type. Urgent care centers reduced the total number of uninsured visits to the ED by 7.3 [21% (P < 0.05)], a decrease driven primarily by reductions in nonurgent visits. This pattern is similar to that of Medicaid enrollees: having an open urgent care center in a ZIP code reduced overall Medicaid ED visits by 20.5 (29.1%, P < 0.05), with nonurgent visits dropping by almost 40% (P < 0.05). Across both of these groups, we also found statistically significant reductions in visits that were urgent and primary care treatable, as well as those that were emergent and avoidable. The reduction in total visits among privately insured individuals was smaller in magnitude (10.5%, P < 0.05), but also was driven largely by changes in nonurgent visits. Among the Medicare population, we found no effect of urgent care centers on total visits, nor any of the less emergent acuity levels. We do, however, detect a small change in the most emergent visits.
TABLE 4.
Impact of urgent care center operating on number of emergency department visits, by payer status and acuity level
| Total visits | Nonurgent | Urgent, primary care treatable | Emergent, avoidable | Emergent, not avoidable | |
|---|---|---|---|---|---|
| Uninsured | |||||
| UCC in ZIP * UCC open | ‒7.258* | ‒3.575* | ‒2.207* | ‒0.685** | ‒0.791 |
| (SE) | (3.351) | (1.536) | (1.104) | (0.232) | (0.522) |
| Baseline | 34.10 | 11.57 | 12.09 | 3.796 | 6.651 |
| Relative change (%) | ‒21.28 | ‒30.9 | ‒18.25 | ‒18.05 | ‒11.89 |
| Medicaid | |||||
| UCC in ZIP * UCC open | ‒20.50* | ‒9.396** | ‒6.536* | ‒2.451** | ‒2.116* |
| (SE) | (8.111) | (3.516) | (2.761) | (0.808) | (1.071) |
| Baseline | 70.44 | 23.88 | 26.27 | 7.871 | 12.42 |
| Relative change (%) | ‒29.1 | ‒39.35 | ‒24.88 | ‒31.14 | ‒17.04 |
| Private | |||||
| UCC in ZIP * UCC open | ‒3.917* | ‒2.270** | ‒1.282* | ‒0.584** | 0.220 |
| (SE) | (1.973) | (0.874) | (0.648) | (0.182) | (0.338) |
| Baseline | 37.50 | 11.77 | 13.52 | 3.733 | 8.471 |
| Relative change (%) | ‒10.45 | ‒19.29 | ‒9.48 | ‒15.64 | 2.6 |
| Medicare | |||||
| UCC in ZIP * UCC open | 0.321 | ‒0.518 | 0.196 | ‒0.170 | 0.813** |
| (SE) | (1.463) | (0.599) | (0.455) | (0.167) | (0.300) |
| Baseline | 17.97 | 5.097 | 6.124 | 1.844 | 4.903 |
| Relative change (%) | 1.79 | ‒10.16 | 3.2 | ‒9.22 | 16.58 |
Author analysis of State Emergency Department Databases for AZ, FL, NE, NJ, NY, and RI. Stars represent statistical significance.
P < 0.05
P < 0.01
P < 0.001.
Figure 1 traces out the time course of these effects, examining how the number of visits changed when urgent care centers closed for the day. Among all patients visiting EDs with long wait times, we confirmed that when urgent care centers were open, the number of nonurgent visits (Panel A) was lower, though this effect got smaller as closure time approaches. After the centers closed, the number of nonurgent visits increased compared with the hour immediately before closure. This effect remains until about four hours post closure. Panel B visually confirms that urgent care center closures do not significantly impact the rate of unavoidable emergency visits to EDs. The event studies for the other two categories can be found in Appendix S1.
FIGURE 1.
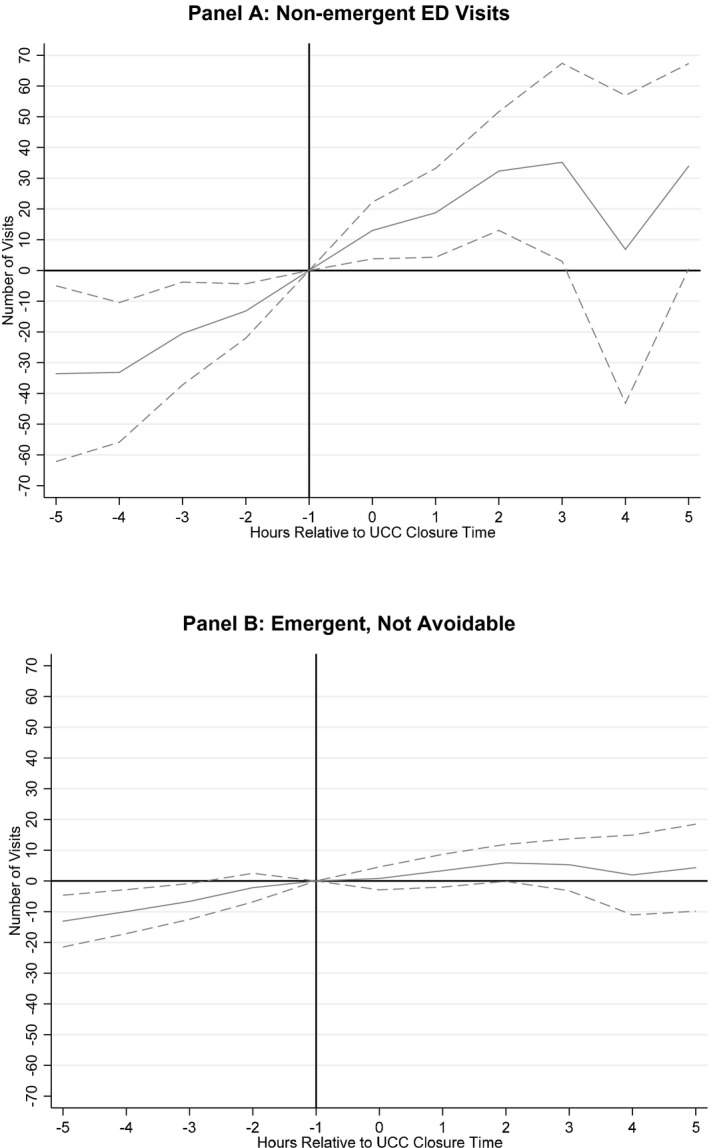
Event study analysis of emergency department visits, by hour relative to local urgent care center closure
4. DISCUSSION
Despite the magnitude and popularity of the urgent care industry, there is little information about its impact on ED demand, for which the clinics may act as a less costly substitute. We used a novel data set to leverage daily operating time of urgent care centers, which overcame previous data limitations. In a difference‐in‐differences framework, we tested whether the acuity mix of ED visits changes during the hours that urgent care centers were open in ZIP codes that had a center, comparing those changes to rates in the same ZIP codes while the centers were closed, as well as to rates in ZIP codes without any centers.
We found that the total number of ED visits fell about 17% among patients who live near urgent care centers, when those centers are open. Nonurgent visits, which decrease by 27%, were the major driver behind this decrease. We take this as evidence that urgent care centers are, to some degree, acting as an ED substitute during their hours of operation.
These impacts were concentrated among EDs with average wait times over an hour. This could be because patients are aware of long wait times in their local ED and choose to visit an urgent care center instead. Many EDs are now providing estimated wait times by text, smartphone apps, billboards and/or their websites, which may encourage patients to seek care elsewhere. In addition to reducing costs and improving access, shifting less emergent cases away from crowded EDs may have other benefits. Long wait times signal crowding and boarding in the ED, which have been associated with adverse outcomes such as increased mortality, hospital length of stay, and medication errors. 50 , 51 , 52 , 53 , 54 , 55 Fewer patients visiting the ED might mean reductions in these undesirable outcomes.
Though we expected our effects to be limited to nonurgent visits, or those that could be treated in a primary care office, we find evidence throughout our study that urgent care centers reduce ED visits across all four acuity levels. This is likely because the algorithm we used for determining acuity level was created during the 1990s when there were two main types of care available: primary or emergency. With the advent of the urgent care industry, which offers clinical resources beyond those of primary care, but not to the extent of the ED, more conditions can be treated outside these two venues. Some visits that would previously have been classified as requiring emergency care can be treated in urgent care centers.
One particularly policy‐relevant finding from our study is that the largest impacts of urgent care centers seem to occur among individuals who are uninsured, and among Medicaid enrollees. Because commercially insured individuals make up the majority (55% in 2018) of urgent care center visits, we hypothesized that this population would be the most affected by urgent care center operating times. 48 , 49 Though we do find effects among this group, visits by uninsured individuals and Medicaid enrollees showed larger relative and absolute declines in ED visits. This is of interest for several reasons. First, these two groups use the ED for nonurgent conditions at higher rates (30.1% for uninsured and 33% for Medicaid) than do other groups (26.6% of privately insured and 18.3% for nondual eligible Medicare). 56 Thus, urgent care centers may be an effective way to reduce ED use among these populations. Second, individuals who are uninsured or who have Medicaid are especially impacted by insufficient access to care. Research has found 42% of uninsured individuals, and 31% of Medicaid enrollees, are significantly more likely to report difficulty getting after‐hours care, compared to those with private insurance; in turn, they are more likely to seek care in the ED. 20 Because urgent care centers play a unique role in improving access during weeknights and weekends, they could be especially important for connecting these vulnerable groups to care. While prior work has shown urgent care centers locate preferentially in areas with higher rates of private insurance, 57 within our sample (Table 1), we find that ZIP codes with urgent care centers have higher percentages of uninsured residents (14.3%), compared to those without urgent care centers (13.4%, P < 0.01). Future research should further explore the predictors of urgent care locations to inform making affordable, after‐hours care available the uninsured and those with Medicaid.
We do not find an impact among Medicare enrolled individuals. There are two possible explanations for this. First, users of urgent care centers tend to be younger; patients age 60 or over comprise less than 10% of all urgent care center visits. 58 Second, adults age 65 and older are less likely than all other age groups to visit the ED for nonurgent care. 56 Nonetheless, around 16% of ED visits by older adults could potentially be shifted to urgent care centers 56 ; some have posited that urgent care centers might be safer for this medically fragile population, though this hypothesis needs to be empirically tested. 59
A key motivation for moving ED patients to other care settings is the potential for cost savings. In the context of the 137 million annual ED visits that take place in the United States, a decrease of 17.2% of total visits translates to about 8 million visits per year that might be treated in urgent care centers. Average costs of care for nonemergent episodes initiated at urgent care centers are substantially lower ($156) than matched episodes initiated at the ED ($570). 32 By multiplying the difference in costs between the two settings ($414) by 8 million fewer visits, we estimate that urgent care centers save about $3.3 billion annually—but this number does not consider the other ways in which urgent care centers might affect health care costs. While we are not aware of other studies that have estimated the impact of urgent care centers on ED use in a quasi‐experimental framework, we can place our findings in the context of the emerging literature on retail clinics, a much smaller market. These studies find that retail clinics have a small but statistically significant impact on reducing ED use and suggest that the walk‐in clinic industry (comprising both urgent care centers and retail clinics) may in turn reduce health care expenditures. 35 , 36 , 60
On the other hand, at least one study suggested that retail clinics may offset these health care savings by encouraging visits along the extensive margin (ie, those who would have forgone any care if a retail clinic were not open at the time of visit). 61 In this same vein, it is possible that urgent care centers encourage new health care use, potentially increasing costs. It is also possible that patients are visiting urgent care centers as a substitute for lower‐cost primary care clinics. Additional research is needed to identify the net effect of the walk‐in industry on health care costs.
One limitation of our study is its reliance on discharge codes in the ED record. These codes may not perfectly align with a patients' own perceptions of their condition's severity. A more valid measure for determining visit acuity might be the “reason for visit,” in which the patient tells the provider what symptoms prompted their visit, but this information was not available in our data.
A second limitation to our study is that due to our identification strategy, we were restricted to using data from six states (AZ, FL, NE, NJ, NY, RI), potentially limiting generalizability of our findings. The states we used, however, represent five different regions of the United States (Northeast, Mid‐Atlantic, Southeast, Mid‐west, and Southwest) and have populations that are diverse among a number of dimensions.
Notwithstanding these limitations, our study provides important foundational evidence that some patients are using urgent care centers as substitutes for the ED, a much costlier care setting. Notably, when patients substitute care urgent care centers for care in the ED, this is most likely to occur for less emergent visits; the number of visits for more emergent conditions, however, change only slightly when urgent care clinics are open or closed in a community. Greater investment in urgent care centers might be an effective policy lever for improving access to care and reducing health care costs, especially among patient populations that are more vulnerable to access barriers.
Supporting information
Author matrix
Supplementary Material
Acknowledgement
Joint Acknowledgement/Disclosure Statement: We thank Guy David, Ian McCarthy, participants at the Southeastern Study Group, and two anonymous reviewers for helpful feedback. Dr. Allen gratefully acknowledges funding (R36HS2484501) from the Agency of Healthcare Research and Quality. This study would not have been possible without data received from solvhealth. Disclosures: None.
Allen L, Cummings JR, Hockenberry JM. The impact of urgent care centers on nonemergent emergency department visits. Health Serv Res. 2021;56:721–730. 10.1111/1475-6773.13631
REFERENCES
- 1. Uscher‐Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Deciding to visit the emergency department for non‐urgent conditions: a systematic review of the literature. Am J Managed Care. 2013;19(1):47. [PMC free article] [PubMed] [Google Scholar]
- 2. Durand AC, Gentile S, Devictor B, et al. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med. 2011;29(3):333‐345. [DOI] [PubMed] [Google Scholar]
- 3. Kellermann AL. Nonurgent emergency department visits: meeting an unmet need. JAMA. 1994;271(24):1953‐1954. [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention . National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 5. Northington WE, Brice JH, Zou B. Use of an emergency department by nonurgent patients. Am J Emerg Med. 2005;23(2):131‐137. [DOI] [PubMed] [Google Scholar]
- 6. Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: a systematic review of prevalence and associated factors. Cadernos de saude publica. 2009;25(1):7‐28. [DOI] [PubMed] [Google Scholar]
- 7. Guttman N, Zimmerman DR, Nelson MSJJoHP. Policy, law. The many faces of access: reasons for medically nonurgent emergency department visits. J Health Polit Policy Law 2003;28(6):1089‐1120. [DOI] [PubMed] [Google Scholar]
- 8. Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Project Hope). 2010;29(9):1630‐1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stoimenoff L, Newman N. Urgent Care Industry White Paper 2018 (Unabridged): The Essential Role of the Urgent Care Center in Population Health. 2017. [Google Scholar]
- 10. Urgent Care Association of America . The Case for Urgent Care. 2011; https://ucaoa.site‐ym.com/resource/resmgr/Files/WhitePaperTheCaseforUrgentCa.pdf. Accessed July 14, 2015. [Google Scholar]
- 11. US Department of Health and Human Services . Projecting the Supply and Demand for Primary Care Practitioners Through 2020 . Rockville, MA: US Department of Health and Human Services; 2013. [Google Scholar]
- 12. O'Malley AS. After‐hours access to primary care practices linked with lower emergency department use and less unmet medical need. Health Aff. 2013;32(1):175‐183. [DOI] [PubMed] [Google Scholar]
- 13. Institute of Medicine . Hospital‐Based Emergency Care: At the Breaking Point. Washington, DC: The National Academies Press; 2007. [Google Scholar]
- 14. Uscher‐Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47‐59. [PMC free article] [PubMed] [Google Scholar]
- 15. Bohmer R. The rise of in‐store clinics — threat or opportunity? N Engl J Med. 2007;356(8):765‐768. [DOI] [PubMed] [Google Scholar]
- 16. Ho V, Metcalfe L, Dark C, et al. Comparing utilization and costs of care in freestanding emergency departments, hospital emergency departments, and urgent care centers. Ann Emerg Med. 2017;70(6):846‐857.e843. [DOI] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention . National Hospital Ambulatory Medical Care Survey: 2014‐2015 Emergency Department Summary Tables Centers for Disease Control and Prevention (CDC). Atlanta, GA: Centers for Disease Control and Prevention; 2019. [Google Scholar]
- 18. Niska RB, Farida X. Jianmin National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. National Health Statistics Reports. 2010;26. [PubMed] [Google Scholar]
- 19. Young GP, Wagner MB, Kellermann AL, Ellis J, Bouley D. Ambulatory visits to hospital emergency departments. Patterns and reasons for use. 24 Hours in the ED Study Group. JAMA. 1996;276(6):460‐465. [DOI] [PubMed] [Google Scholar]
- 20. O'Malley AS. After‐hours access to primary care practices linked with lower emergency department use and less unmet medical need. Health Aff (Project Hope). 2013;32(1):175‐183. [DOI] [PubMed] [Google Scholar]
- 21. Nadel V. Emergency departments: Unevenly affected by growth and change in patient use. US General Accounting Office: Report to the Chairman, Subcommittee on Health for Families and the Uninsured, Committee on Finance, US Senate. Washington, DC: US Government Printing Office; 1993. [Google Scholar]
- 22. Rask KJ, Williams MV, Parker RM, McNagny SE. Obstacles predicting lack of a regular provider and delays in seeking care for patients at an urban public hospital. JAMA. 1994;271(24):1931‐1933. [PubMed] [Google Scholar]
- 23. Gindi RM, Cohen RA, Kirzinger WK. Emergency Room Use Among Adults Aged 18–64: Early Release of Estimates from the National Health Interview Survey, January–June 2011. Hyattsville, MA: National Center for Health Statistics. 2012. [Google Scholar]
- 24. Cunningham PJ. What accounts for differences in the use of hospital emergency departments across U.S. communities? Health Aff (Project Hope). 2006;25(5):w324‐336. [DOI] [PubMed] [Google Scholar]
- 25. Urgent Care Association of America . Industry Frequently Asked Questions. 2015; http://www.ucaoa.org/general/custom.asp?page=IndustryFAQs. Accessed June 01, 2016. [Google Scholar]
- 26. Urgent Care Association of America . 2017 Benchmarking Report Summary: Headlines on Growth. Warrenville, IL: Urgent Care Association; 2017. [Google Scholar]
- 27. Stoimenoff L. The Essential Role of the Urgent Care Center in Population Health. 2019. [Google Scholar]
- 28. Camargo C, Sullivan A. National Emergency Department Inventory ‐ USA. 2018. [DOI] [PubMed] [Google Scholar]
- 29. Bachrach D, Frohlich J, Garcimonde A, Nevitt K. The Value Proposition of Retail Clinics. Princeton, NJ: Robert Wood Johnson Foundation. 2015;12. [Google Scholar]
- 30. Trueger NS, Chua K‐P, Hussain A, Liferidge AT, Pitts SR, Pines JM. Incorporating alternative care site characteristics into estimates of substitutable ED visits. Med Care. 2017;55(7):693‐697. [DOI] [PubMed] [Google Scholar]
- 31. Spetz J, Parente ST, Town RJ, Bazarko D. Scope‐of‐practice laws for nurse practitioners limit cost savings that can be achieved in retail clinics. Health Aff (Project Hope). 2013;32(11):1977‐1984. [DOI] [PubMed] [Google Scholar]
- 32. Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med. 2009;151(5):321‐328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rudavsky R, Mehrotra A. The sociodemographic characteristics of the communities served by retail clinics. JABFM. 2010;23(1):42‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kaissi A, Charland T. The evolution of retail clinics in the United States, 2006–2012. Health Care Manag (Frederick). 2013;32(4):336‐342. [DOI] [PubMed] [Google Scholar]
- 35. Alexander D, Currie J, Schnell M. Check Up Before You Check Out: Retail Clinics and Emergency Room Use. Cambridge, MA: National Bureau of Economic Research. 2017. [Google Scholar]
- 36. Hollingsworth A. Retail Health Clinics: Endogenous Location Choice and Emergency Department Diversion. 2014. [Google Scholar]
- 37. Martsolf G, Fingar KR, Coffey R, et al. Association between the opening of retail clinics and low‐acuity emergency department visits. Ann Emerg Med. 69(4):397–403.e395. [DOI] [PubMed] [Google Scholar]
- 38. Urgent Care Locations . Urgent Care Locations Provides Verified Urgent Care Directory. Chennai, India: Urgent Care Locations; 2013. [Google Scholar]
- 39. Barber M. Personal Communication with Michael Barber. 2015. [Google Scholar]
- 40. Urgent Care Association of America . Urgent Care Association of America Releases 2014 Urgent Care Survey, Shows Major Industry‐Wide Expansion. Urgent Care Association of America; 2014. [Google Scholar]
- 41. Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. ECP. 2001;5(3):143‐151. [PubMed] [Google Scholar]
- 42. Johnston KJ, Allen L, Melanson TA, Pitts SR. A “Patch” to the NYU emergency department visit algorithm. Health Serv Res. 2017;52(4):1264‐1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Billings J, Parikh N, Mijanovich T. Emergency department use in New York City: a survey of Bronx patients. Issue Brief (Commonw Fund). 2000;435:1‐5. [PubMed] [Google Scholar]
- 44. Feldman J, The NYU. Classification System for ED Visits: WSHA Technical Concerns. Washington State Hospital Association: Health Information Program; 2010. [Google Scholar]
- 45. Johnston Kenton J., Allen Lindsay, Melanson Taylor A., Pitts Stephen R. A “Patch” to the NYU Emergency Department Visit Algorithm. Health Services Res. 2017;52 (4):1264–1276. 10.1111/1475-6773.12638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Centers for Medicare and Medicaid Services . Hospital Compare Database ‐ Timely and Effective Care. 2013; https://data.medicare.gov/data/hospital‐compare. Accessed January, 2016. [Google Scholar]
- 47. American College of Emergency Physicians . EMTALA. 2018; https://www.acep.org/life‐as‐a‐physician/ethics‐‐legal/emtala/emtala‐fact‐sheet/. Accessed September 2020. [Google Scholar]
- 48. Ashman JJ, Rui P, Hing E. Expected Source of Payment at Emergency Department Visits for Adults Aged 18‐‐64 for the United States and in the Five Most Populous States, 2012. Hyattsville, MA: US Department of Health & Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2016. [Google Scholar]
- 49. Urgent Care Association . Urgent Care Association 2018 Benchmarking Survey; 2019. [Google Scholar]
- 50. Singer AJ, Thode HC Jr, Viccellio P, Pines JM. The association between length of emergency department boarding and mortality. Acad Emerg Med. 2011;18(12):1324‐1329. [DOI] [PubMed] [Google Scholar]
- 51. Carter EJ, Pouch SM, Larson EL. The relationship between emergency department crowding and patient outcomes: a systematic review. J Nurs Scholarsh. 2014;46(2):106‐115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Carr BG, Kaye AJ, Wiebe DJ, Gracias VH, Schwab CW, Reilly PM. Emergency department length of stay: a major risk factor for pneumonia in intubated blunt trauma patients. J Trauma Acute Care Surg. 2007;63(1):9‐12. [DOI] [PubMed] [Google Scholar]
- 53. Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35(6):1477‐1483. [DOI] [PubMed] [Google Scholar]
- 54. Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med. 2010;28(3):304‐309. [DOI] [PubMed] [Google Scholar]
- 55. Liu SW, Thomas SH, Gordon JA, Hamedani AG, Weissman JS. A pilot study examining undesirable events among emergency department–boarded patients awaiting inpatient beds. Ann Emerg Med. 2009;54(3):381‐385. [DOI] [PubMed] [Google Scholar]
- 56. Rui P, Kang K. National Hospital Ambulatory Medical Care Survey: 2017 Emergency Department Summary Tables. Hyattsville, MA: National Center for Health Statistics; 2018. [Google Scholar]
- 57. Le ST, Hsia RY. Community characteristics associated with where urgent care centers are located: a cross‐sectional analysis. BMJ Open. 2016;6(4):e010663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. FAIR Health . A New View of Place of Service Trends and Medical Pricing. 2018; https://s3.amazonaws.com/media2.fairhealth.org/whitepaper/asset/FH%20Medical%20Price%20Index%20and%20FH%20Healthcare%20Indicators‐‐whitepaper.pdf. Accessed November, 2020. [Google Scholar]
- 59. Cimons M. ERs can be loud, hectic and even dangerous for the elderly. Here's how hospitals are trying to fix that. Washington Post. December 8, 2018,2018; Accessed November 7. [Google Scholar]
- 60. Sussman A, Dunham L, Snower K, et al. Retail clinic utilization associated with lower total cost of care. Am J Manag Care. 2013;19(4):e148‐157. [PubMed] [Google Scholar]
- 61. Ashwood JS, Gaynor M, Setodji CM, Reid RO, Weber E, Mehrotra A. Retail clinic visits for low‐acuity conditions increase utilization and spending. Health Aff (Project Hope). 2016;35(3):449‐455. [DOI] [PubMed] [Google Scholar]
- 62. Billings J, Parikh N, Mijanovich T. Emergency Department Use: The New York Story. New York, NY: The Commonwealth Fund, November; 2000. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author matrix
Supplementary Material


