Abstract
Background
Post-arthroscopic shoulder surgery pain is severe enough to interfere with initial recovery and rehabilitation.
Objectives
We aimed to evaluate the analgesic effects of postoperative ultrasound-guided suprascapular plus axillary nerve blocks superficial subepidermal axon bundles (SSAB) with interscalene block (ISB) in arthroscopic shoulder surgery.
Methods
In this single-blind randomized, open-label clinical trial, 80 candidates of elective arthroscopic shoulder surgery were randomly allocated to receive either SSAB or ISB at a postoperative care unit. The severity of resting and changing position pain was measured using visual analogue scale (VAS) score at 4h, 8h, 12h, 16h, and 24h, postoperatively. Timing of first opioid request, 24h dose requirement, patients' satisfaction rate, and side effects were also recorded. All registered data were analyzed using SPSS software version 23 for Windows (SPSS, Chicago, IL).
Results
Resting and changing position pain scores were comparable between SSAB and ISB groups in the most time intervals. At 12h, moving and resting pain was significantly lower in ISB than SSAB group, while moving pain was more severe in ISB group at 24h assessment. Patient satisfaction scores were comparable between the two groups except for 12h assessment. Time to first analgesic requirement and total dose of 24h opioid requirement were not significantly different between the two groups.
Conclusions
Suprascapular plus axillary nerve block could be an effective and safe alternative for interscalene block for pain management after arthroscopic shoulder surgery.
Keywords: Interscalene Block, Suprascapular Nerve Block, Axillary Nerve Block, Ultrasound-Guided, Arthroscopic Shoulder Surgery
1. Background
Post-arthroscopic shoulder surgery pain can be very severe (up to 45%), which interferes with initial recovery. This pain can be controlled using a high dosage of opioids. However, opioids have various side effects such as nausea, vomiting, sedation, or inadequate pain relief (1). Interscalene block (ISB), which covers both shoulder and upper limb, has been recommended for postoperative pain management. However, it has side effects such as unintentional local anesthetic injections in the epidural, intrathecal, or vertebral arteries spaces, unpredictable expansion of anesthetics to structures such as the phrenic, vagus, and laryngeal recurrent nerve, and satellite ganglion. Its potentially dangerous side effect was the reason for finding an effective nerve block with fewer side effects (2). Suprascapular nerve block (SSNB) is considered an effective method compared to ISB in postoperative anesthesia, showing fewer side effects (1%). However, since SSNB is not the only nerve responsible for sensory and motor innervation of the shoulder joint, it cannot be used alone as an anesthesia technique for shoulder surgery. The axillary nerve completes the innervation of the shoulder joint (3-6). Blocking this nerve alongside SSNB, identified as shoulder block, can be effective in postoperative pain management. By reducing pain, the length of postoperative hospitalization can be reduced as well (4-9). An ultrasound machine is used to avoid unintentional anesthetic spread and damage to important adjacent structures. Some studies have shown that targeted blocking of shoulder nerves has lower side effects with a shoulder limited block area compared to ISB.
2. Objectives
This study aimed to compare the effects of SSAB with ISB on postoperative pain score and analgesic demands.
3. Methods
This single-blind randomized, open-label clinical trial was conducted on 80 patients who underwent elective arthroscopic shoulder surgery admitted to Rasool Akram Medical Complex, Tehran, Iran. This study was approved by the research deputy and ethics committee of Iran University of Medical Sciences, Tehran, Iran (code: IR.IUMS.FMD.REC1396.9511174016). The present study was also registered and approved by Iran Randomized Clinical Trial Center under the registration number: IRCT20120814010599N23. Informed consent was obtained from all individual participants included in the study. This study adhered to the consolidated standards of reporting trials (CONSORT) guideline and was carried out in accordance with the declaration of Helsinki (1964). Inclusion criteria were as follows: (1) patients aged between 20 to 60 years old; (2) American Society of Anesthesiology (ASA) score of 1 – 2; (3) scheduled for elective surgery; and (4) body mass index (BMI) < 35 kg/m2. Exclusion criteria were also as follows: (1) patients with allergy to local anesthetics or any drugs included in the study; (2) patients who had a history of kidney or liver disease; (3) patients who had a history of drug and alcohol misuse; (4) patients who had BMI more than 35 kg/m2; (5) patients with a history of diabetic neuropathy; (6) patients with a history of lung disorders; (7) patients with a history of neurologic disorders; (8) patients with coagulation problems; (9) patients with mental issues; and (10) patients who had no ability to answer the questions properly. After the patients provided consent to participate in this trial, they were randomly allocated (allocation ratio: 1: 1) to ISB and SSAB groups using block randomization method with the block size of four.
3.1. Preoperative Pain Assessment
An anesthetist visited the patients the day before surgery, described the visual analogue scale (VAS) for them, and described for them about analgesic pump infusion. VAS is a 10-cm measuring tool where 0 points to no pain, whereas 10 represents the most severe imaginable pain (5). Patients were given the standard monitoring of non-invasive blood pressure (NIBP), electrocardiography (EKG), capnography, pulse oximetry (POM), and bispectral index (BIS) at the time of entrance to the operation room.
3.2. Anesthesia
All of the patients initially received an infusion of 5 cc/kg Ringer’s lactate. Preoperatively, fentanyl and midazolam, and for anesthesia induction, propofol and cisatracurium were injected and then intubated. To maintain anesthesia, propofol plus remifentanil was used. During surgery, BIS was maintained between 40 to 60, and end-tidal CO2 (ETCO2) was between 30 to 35 mmHg. At the end of the surgery, patients were extubated.
3.3. Postoperative Analgesia Regimen
In post-anesthesia care unit (PACU), randomization was done using a randomized computer-generated sequence: (1) ISB, and (2) SSAB. An anesthesia resident enrolled the patients in the study and assigned the patients randomly to the interventions under the supervision of the attending anesthetist in charge of the patients. He was not blinded to the assignments. The blockade was performed under ultrasound guidance (sonosite, EdgeII, WA, USA) and with a linear probe and 50 mm needle (Sonoblock, Pajung, Germany). Patients were kept in a supine position for ISB. The anterior and middle scalene muscles were scanned, and 15 cc of 0.2% ropivacaine (Molteni, Italy) was injected into the Scalene groove after finding stoplight sign as peri-truncal manner. For suprascapular block, patients were kept in a supine position. A linear probe was located on supraclavicular fossa beside the bandaged area. The omohyoid muscle was found, the nerve is visible under this muscle in posterior cervical triangle as a hypoechoic circle, and then via in-plane technique, 10 cc of 0.2% ropivacaine was injected. For the axillary nerve block, patients were kept in lateral position. The linear probe was kept on the long axis until the Deltoid and teres minor muscles were seen. Then, 10 cc of 0.2% ropivacaine was injected in the interfacial plane between the deltoid and teres minor muscles, next to the circumflex artery. For the two groups, pain pump was used, containing 2 g of paracetamol and 60 mg of ketorolac in 100 mL normal saline with a constant flow of 4 cc/h. In the case of VAS > 4, Pethidine 15 mg was injected and recorded.
3.4. Outcome Variables Measures and Data Collection
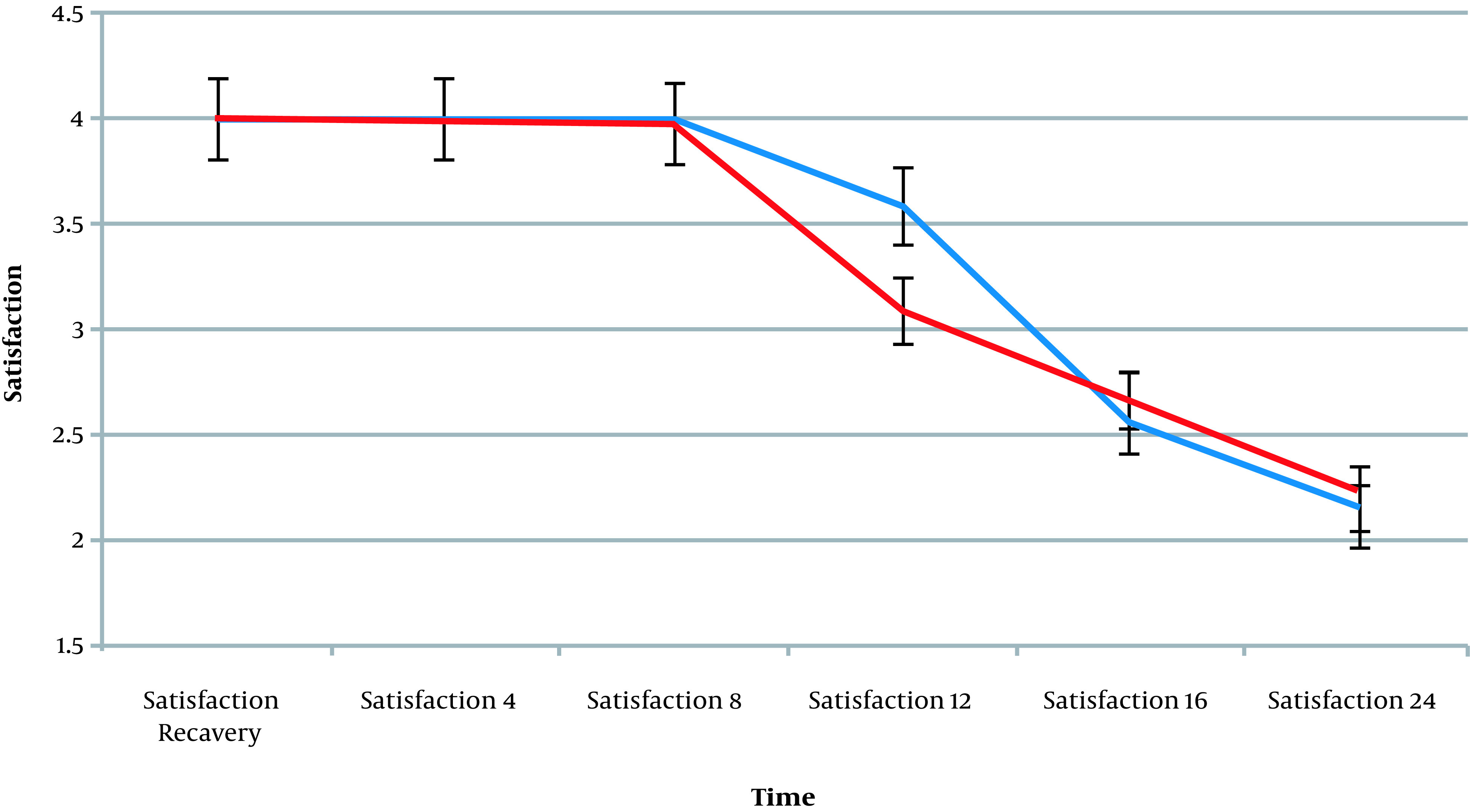
The outcome assessor was blinded to the assignments. Patient’s VAS score was recorded at recovery and 4- 8- 12- 16- 24-hours after surgery in both resting and changing positions as the primary outcomes of the study. Changing position pain means pain while moving side to side or any positional changes. As the secondary outcomes, the first analgesic request time, the total amount of rescue analgesic in 24 h post-operation, and patient satisfaction rate was also recorded. If the VAS score exceeded 3, 20 mg of Pethidine was injected as rescue analgesic. The patient satisfaction rate during recovery was also recorded at 4- 8- 12- 16- 24-h. post-operation, using the following scale: 0 = poor, 1 = moderate, 2 = good, 3 = very good, 4 = excellent. Possible side effects, such as shortness of breath, pneumothorax, epidural or subarachnoid injection, diaphragmatic paralysis, damage of the supra laryngeal nerve, nausea, and vomiting were monitored.
3.5. Sample Size Calculation and Statistical Analysis
The sample size was calculated based on a study done by Lee et al. (6) using the following formula with alpha error of 0.05 and power of 80% (40 patients in each group):
After collecting all information, data were entered into SPSS (version 23) for statistical analysis. Quantitative descriptive data was reported as averages, with 95% confidence intervals (CI), and qualitative data as frequency and frequency percentage. To study the trends, the repeated measure tests were taken, and the significance level was considered P < 0.05. Also, t-independent t-test and chi-square test were used.
4. Results
The current study was conducted on 80 arthroscopic shoulder surgery candidate patients in a university hospital. According to the patients’ data in Table 1, there was no significant difference in the demographic distribution of data between the two groups. The flowchart shows the study participants (Figure 1). Patient postoperative pain was recorded at recovery and 4- 8- 12- 16- 24-h after, using VAS score. The result showed that resting pain had no significant difference at all timings (P > 0.05). Only the VAS mean at 12th hours post-operation was significantly higher in the SSAB than the ISB group (P > 0.001) (Table 2). Patients’ pain while changing position was evaluated using VAS score at recovery and 4- 8- 12- 16- 24-h post-operation. The result shows that moving pain at 12 h postoperative was significantly higher in the SSAB group (P > 0.001). At 24 h post-operation, the VAS score average was significantly higher in the ISB group (P = 0.016). During the other times recorded, no significant differences were found (P > 0.05) (Table 2). Patient satisfaction score was evaluated at recovery and 4- 8- 12- 16- 24-h post-operation. The result shows that, at 12th hour, this score was significantly higher in the ISB group (P < 0.001). During the other recorded times, no significant differences were found (P > 0.05) (Figure 2). The average time of the first analgesic request in the ISB and SSAB groups was comparable (10.5 ± 5.5 vs. 9.0 ± 3.6 h, P = 0.15). Also, the 24 h-required dose of pethidine in ISB (16.0 ± 8.1 mg) and SSAB (17.0 ± 7.2 mg) groups was not statistically different (P = 0.56). Side effects were not reported in either of the groups. The reported incidence rate of nausea/vomiting in the ISB (12.5%) and SSAB (17.5%) groups was comparable (P = 0.378).
Table 1. Demographic Variables and Baseline Characteristics of Patients in Two Groups a.
| Variables | ISB (n = 40) | SSAB (n = 40) | P-Value |
|---|---|---|---|
| Male Sex | 28 (70) | 30 (75) | 0.41 |
| Age (y) | 48.80 ± 7.48 | 49.70 ± 7.05 | 0.599 |
| BMI | 23.26 ± 1.77 | 23.47 ± 1.67 | 0.967 |
| Duration of surgery | 2.53 ± 0.34 | 2.41 ± 0.31 | 0.887 |
a Values are presented as No. (%) or mean ± SD.
Figure 1. The consort diagram.
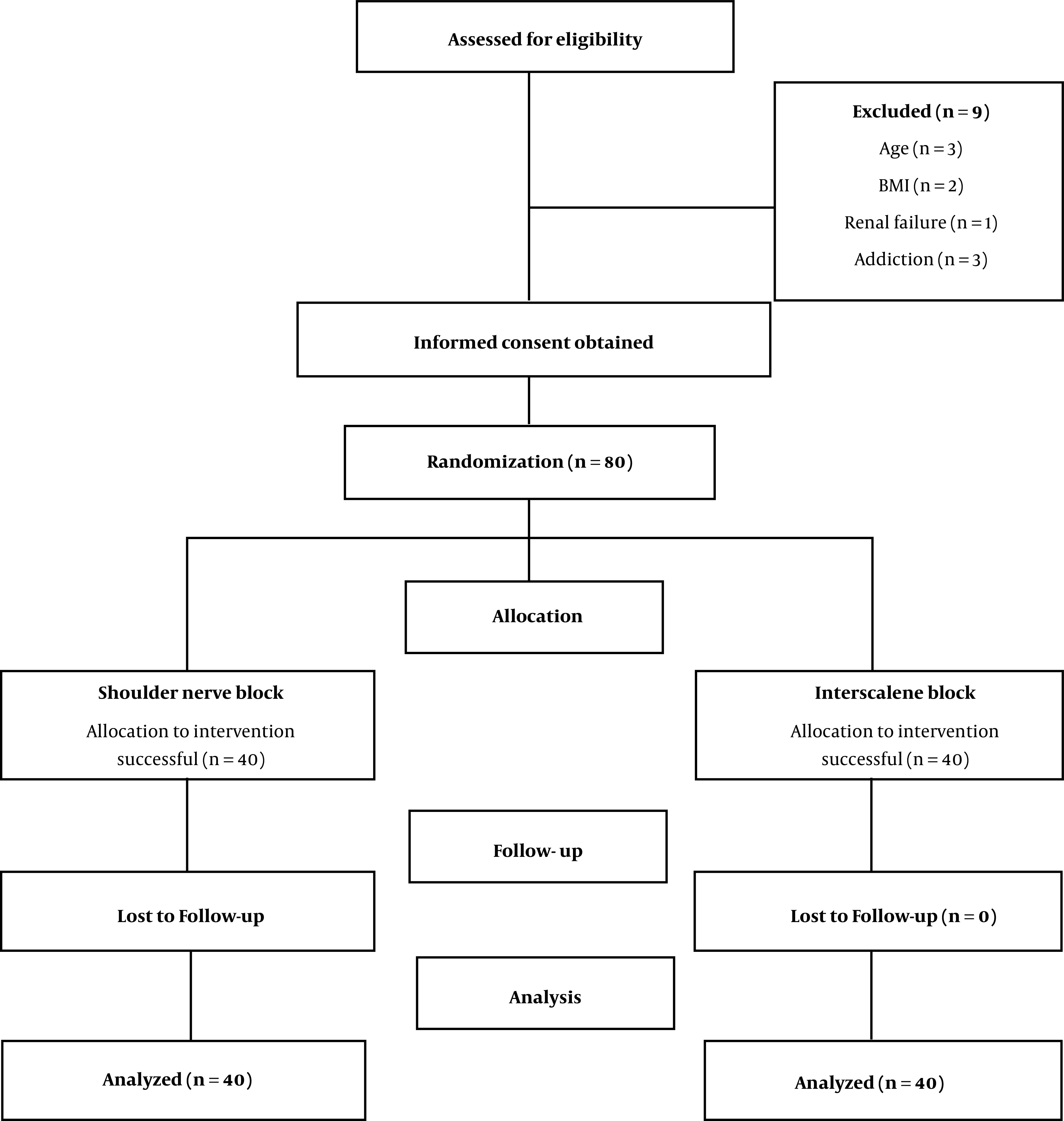
Table 2. The Mean Resting and Movement Pain Scores at the Measured Time Intervals a.
| Time of Measurement | Resting Pain | Movement Pain | ||||
|---|---|---|---|---|---|---|
| ISB (n = 40) | SSAB (n = 40) | P-Value | ISB (n = 40) | SSAB (n = 40) | P-Value | |
| At recovery | 0 ± 0 | 0 ± 0 | NS | 0 ± 0 | 0 ± 0 | NS |
| 4th h | 0 ± 0 | 0 ± 0 | NS | 0 ± 0 | 0 ± 0 | NS |
| 8th h | 0.015 ± 0.66 | 0.38 ± 0.92 | 0.21 | 0.35 ± 0.86 | 0.63 ± 1.19 | 0.24 |
| 12th h | 1.05 ± 1.41 | 3.05 ± 0.55 | 0.001 | 1.98 ± 1.70 | 3.58 ± 0.78 | 0.001 |
| 16th h | 3.38 ± 0.49 | 3.33 ± 0.52 | 0.001 | 4.38 ± 0.58 | 4.36 ± 0.52 | 1.00 |
| 24th h | 4.20 ± 0.60 | 3.98 ± 0.73 | 0.13 | 5.18 ± 0.50 | 4.83 ± 0.74 | 0.01 |
Abbreviation: NS, non-significant.
a Data are presented as mean ± SD.
Figure 2. The trend of patients’ satisfaction at the measured time intervals [mean, standard error of mean (SEM)].
5. Discussion
In the present study, there were no significant differences between the two patient groups in terms of age, gender, BMI, and operation time. The results show that there was no significant difference in terms of resting pain at different times between the groups. Only at the 12th hour, the VAS rate was significantly higher in the SSAB than in the ISB group, which might be due to the longer duration of anesthesia of the ISB. In a study carried out by Dhir, the ISB group showed better pain scores at 6 h post-operation, while at the 24th hour, the shoulder block demonstrated better pain control compared to the ISB group. This result differs from the result of the current study (10).
At 12th hour, movement pain was significantly higher in the SSAB than in the ISB group. This might be related to the longer anesthesia induced by ISB. A review of the literature regarding the quality of postoperative pain control while changing position did not show enough specific data. According to Waleed study in 2016 (5), SSAB can be used as a very safe alternative for ISB in shoulder surgery. Based on the VAS score, there was no significant difference in terms of pain intensity between the two groups in the current study.
Lee et al. (6) in 2017 evaluated the differences in pain relief between ISB + SSNB with ISB, finding showed that SSNB + ISB patients had better pain control in the recorded hours. In the current study, patients with shoulder nerve block showed similar effects to those with ISB. Only at 12th hour, the ISB group reported less pain, which might due to longer analgesic action.
During arthroscopic shoulder surgery, a considerable amount of fluid enters the shoulder joint and its surrounding structures. This situation can cause Compartment Syndrome, which is one of the main reasons for intense pain in the surgical area. It was observed that, although the analgesic effects of blocks at 12th hour decreased since the liquid volume was absorbed and edema decreased, the pain score decreased. It means that after 24h, one of the major pain generators, which is tissue edema, is weakened.
The patient satisfaction rate was significantly higher among the ISB group at 12th hour. Otherwise, there was no significant difference between the two groups at the other measured times. In a study done by Pitombo et al. (10) no significant difference was observed between the two groups. However, in the SSAB group, immobility was limited to the shoulder area, which was more preferable for the patient due to the non-paralysis of the upper limbs. In Dhir’s study (11), the patient satisfaction rate was higher in the ISB group at 6th hour. However, the rate of motor block in the ISB group was up to 61%, which might be due to the usage of 0.5% Bupivacaine. In the present study, no motor blockade was observed in either of the groups, which may be due to the lower concentrations of ropivacaine. The average time of the first analgesic request and its prescribed dosage on the first post-operation day showed no significant difference between the two groups. These findings are comparable with most earlier studies (12-16).
In terms of the appearance of side effects, there were not any significant differences between them. These results correspond with the earlier results suggesting that these methods are low risk with few side effects (10, 11, 17, 18). One factor to be considered is that, in the current study, 0.2% ropivacaine was used, with a total volume limited to 15cc, to reduce the possible side effects. One of the limitations of this study is the use of subjective criteria for rating pain intensity, which may affect the meaningfulness of the results. Another limitation is using the same anesthesiologist for all blocking and the same shoulder surgeon. This may decrease the generalizability of the results. However, this method also decreases the potential bias level.
5.1. Conclusions
The present study shows that concurrent SSAB has no significant differences in comparison to the ISB in terms of pain control and patient satisfaction rates. Therefore, considering the lower side effects of this method, it can be a beneficial alternative for ISB; however, further studies with larger sample size are needed.
Acknowledgments
The study was approved by the Ethics Committee of Iran University of Medical Sciences. The authors thank the Rasool Akram Medical Complex Clinical Research Development Center (RCRDC) for its technical and editorial assists.
Footnotes
Authors' Contribution: Study concept and design, SHRF, PR, FI; Analysis and interpretation of data, PR, MM; Drafting of the manuscript, FI, SHRF, MKA, PR; Critical revision of the manuscript for important intellectual content, SHRF, PR, FI, MM; Statistical analysis, SHRF, PR, SM.
Clinical Trial Registration Code: The study was registered with Iran Randomized Clinical Trial Center under the registration number: IRCT 20120814010599N23, approval date: 2018-03-16.
Conflict of Interests: The authors declare that they have no conflict of interests.
Ethical Approval: Written permission was obtained from the authorities of the Rasool Akram Medical Complex in Tehran, the researcher explained the research and education for patients emphasizing their information would remain confidential and that the results of the research would be published anonymously, and they could leave the study at any time. The procedures of this study were approved by the Ethics Committee of Iran Registry of University of Medical Science (IR.IUMS.FMD.REC1396.9511174016).
Funding/Support: There was no funding support for this research.
Informed Consent: Informed consent was obtained from all individuals.
Contributor Information
Seyed Hamid Reza Faiz, Email: hrfaiz@hotmail.com.
Masood Mohseni, Email: masood.mohseni@gmail.com.
Farnad Imani, Email: farnadimani@yahoo.com.
Mohamad Kazem Attaee, Email: mohamadkazemattaee.rcrdc@gmail.com.
Shima Movassaghi, Email: shmovassaghis2020@gmail.com.
Poupak Rahimzadeh, Email: p.rahimzadeh.anesthesiology@gmail.com.
References
- 1.Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: An evaluation of the first results. Arthroscopy. 2008;24(6):689–96. doi: 10.1016/j.arthro.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 2.Singelyn FJ, Lhotel L, Fabre B. Pain relief after arthroscopic shoulder surgery: A comparison of intraarticular analgesia, suprascapular nerve block, and interscalene brachial plexus block. Anesth Analg. 2004;99(2):589–92. doi: 10.1213/01.ANE.0000125112.83117.49. [DOI] [PubMed] [Google Scholar]
- 3.Conn RA, Cofield RH, Byer DE, Linstromberg JW. Interscalene block anesthesia for shoulder surgery. Clin Orthop Relat Res. 1987;216:94–8. doi: 10.1097/00003086-198703000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: A prospective study. Anesthesiology. 2001;95(4):875–80. doi: 10.1097/00000542-200110000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Waleed A. Postoperative analgesia for arthroscopic shoulder surgery: comparison between ultrasound-guided interscalene block and combined suprascapular and axillary nerve blocks. Ain-Shams Journal of Anaesthesiology. 2016;9(4):536. doi: 10.4103/1687-7934.198260. [DOI] [Google Scholar]
- 6.Lee JJ, Hwang JT, Kim DY, Lee SS, Hwang SM, Lee NR, et al. Effects of arthroscopy-guided suprascapular nerve block combined with ultrasound-guided interscalene brachial plexus block for arthroscopic rotator cuff repair: A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2121–8. doi: 10.1007/s00167-016-4198-7. [DOI] [PubMed] [Google Scholar]
- 7.Divizia M, Germani G, Urti I, Imani F, Varrassi G, Meloncelli S. Endoscopic neuromodulation of suprascapular nerve in chronic shoulder pain: A case report. Anesth Pain Med. 2020;10(2):e103624. doi: 10.5812/aapm.103624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blaivas M, Lyon M. Ultrasound-guided interscalene block for shoulder dislocation reduction in the ED. Am J Emerg Med. 2006;24(3):293–6. doi: 10.1016/j.ajem.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Rahimzadeh P, Imani F, Faiz SHR, Boroujeni BV. Impact of the ultrasound-guided serratus anterior plane block on post-mastectomy pain: A randomised clinical study. Turk J Anaesthesiol Reanim. 2018;46(5):388–92. doi: 10.5152/TJAR.2018.86719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pitombo PF, Meira Barros R, Matos MA, Pinheiro Modolo NS. Selective suprascapular and axillary nerve block provides adequate analgesia and minimal motor block. Comparison with interscalene block. Braz J Anesthesiol. 2013;63(1):45–51. doi: 10.1016/S0034-7094(13)70197-1. [DOI] [PubMed] [Google Scholar]
- 11.Dhir S, Sondekoppam RV, Sharma R, Ganapathy S, Athwal GS. A comparison of combined suprascapular and axillary nerve blocks to interscalene nerve block for analgesia in arthroscopic shoulder surgery: An equivalence study. Reg Anesth Pain Med. 2016;41(5):564–71. doi: 10.1097/AAP.0000000000000436. [DOI] [PubMed] [Google Scholar]
- 12.Price D. How I do it: Ultrasound-guided combined suprascapular and axillary nerve block. Am Soc Reg Anesth Pain Med News. 2013;13:22–5. [Google Scholar]
- 13.Pani N, Routray SS, Pani S, Mallik S, Pattnaik S, Pradhan A. Post-operative analgesia for shoulder arthroscopic surgeries: A comparison between inter-scalene block and shoulder block. Indian J Anaesth. 2019;63(5):382–7. doi: 10.4103/ija.IJA_65_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim JY, Kang MW, Lee HW, Noh KC. Suprascapular nerve block is an effective pain control method in patients undergoing arthroscopic rotator cuff repair: A randomized controlled trial. Orthop J Sports Med. 2021;9(1):2325967120970906. doi: 10.1177/2325967120970906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lim YC, Koo ZK, Ho VW, Chang SS, Manohara S, Tong QJ. Randomized, controlled trial comparing respiratory and analgesic effects of interscalene, anterior suprascapular, and posterior suprascapular nerve blocks for arthroscopic shoulder surgery. Korean J Anesthesiol. 2020;73(5):408–16. doi: 10.4097/kja.20141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ozkan D, Cemaloglu S, Catma FM, Akkaya T. Effects of suprascapular and axillary nerve block on postoperative pain relief sevoflurane consumption and visual clarity in arthroscopic shoulder surgery. Agri. 2020;32(1):1–7. doi: 10.14744/agri.2019.04875. [DOI] [PubMed] [Google Scholar]
- 17.Kay J, Memon M, Hu T, Simunovic N, Duong A, Paul J, et al. Suprascapular nerve blockade for postoperative pain control after arthroscopic shoulder surgery: A systematic review and meta-analysis. Orthop J Sports Med. 2018;6(12):2325967118815859. doi: 10.1177/2325967118815859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Divella M, Vetrugno L, Orso D, Langiano N, Bignami E, Bove T, et al. Interscalenic versus suprascapular nerve block: Can the type of block influence short- and long-term outcomes? An observational study. Minerva Anestesiol. 2019;85(4):344–50. doi: 10.23736/S0375-9393.18.12791-X. [DOI] [PubMed] [Google Scholar]


