Abstract
Introduction:
In the early phase of the coronavirus disease 2019 (COVID-19) pandemic, United States Emergency Medical Services (EMS) experienced a decrease in calls, and at the same time, an increase in out-of-hospital deaths. This finding led to a concern for the implications of potential delays in care for the obstetric population.
Hypothesis/Problem:
This study examines the impact of the pandemic on prehospital care amongst pregnant women.
Methods:
A retrospective observational study was conducted comparing obstetric-related EMS activations in Maryland (USA) during the pandemic (March 10-July 20, 2020) to a pre-pandemic period (March 10-July 20, 2019). Comparative analysis was used to analyze the difference in frequency and acuity of calls between the two periods.
Results:
There were fewer obstetric-related EMS encounters during the pandemic compared to the year prior (daily average during the pandemic 12.5 [SD = 3.8] versus 14.6 [SD = 4.1] pre-pandemic; P <.001), although the percent of total female encounters remained unchanged (1.6% in 2020 versus 1.5% in 2019; P = .091). Key indicators of maternal status were not significantly different between the two periods. African-American women represented a disproportionately high percentage of obstetric-related activations (36.2% in 2019 and 34.8% in 2020).
Conclusions:
In this state-wide analysis of EMS calls in Maryland early in the pandemic, no significant differences existed in the utilization of EMS by pregnant women. Prehospital EMS activations amongst pregnant women in Maryland only decreased slightly without an increase in acuity. Of note, over-representation by African-American women compared to population statistics raises concern for broader systemic differences in access to obstetric care.
Keywords: Emergency Medical Services, maternal health, pandemics, pregnancy complications
Abbreviations: CDC, Centers for Disease Control and Prevention; COVID-19, coronavirus disease 2019; EMS, Emergency Medical Services; MIEMSS, Maryland Institute for Emergency Medical Services Systems; PUI, person under investigation (for COVID-19)
Background
The coronavirus disease 2019 (COVID-19) pandemic was declared a global emergency by the World Health Organization (WHO; Geneva, Switzerland) in January of 2020.1 Since its discovery in 2019, more than 88 million people have been infected resulting in over 1.9 million deaths (as of January 10, 2021).2 The body of evidence regarding the impact of COVID-19 on pregnancy and obstetric care continues to grow. Data from the Centers for Disease Control and Prevention (CDC; Atlanta, Georgia USA) from January 22-June 7, 2020 in the United States revealed that pregnant women with COVID-19 have a higher risk of hospital admission, intensive care unit admission, and mechanical ventilation than non-pregnant women with COVID-19.3 Higher rates of preterm birth and Cesarean delivery have also been reported.4,5 Although overall maternal mortality from COVID-19 infection has been reportedly low, the morbidity and mortality resulting from the pandemic is predicted to be far more significant.6–8
Emergency Medical Services (EMS; refers to a method of providing prehospital treatment, stabilization, and transport when indicated for urgent conditions, provided by emergency medical technicians and/or paramedics) in Maryland (USA) are coordinated at the state-wide level by the Maryland Institute for Emergency Medical Services Systems (MIEMSS; Baltimore, Maryland USA). Maryland’s state-wide approach to EMS care includes treatment protocols, a single electronic medical records system, a state-wide EMS radio communication network, as well as many other regulatory functions. Prehospital emergency medical care is delivered through 26 jurisdictional EMS agencies that are operated by county or local governments, who also operate communications centers responsible for receiving 911 calls and dispatching EMS units. In March 2020, MIEMSS implemented a standard state-wide EMS definition of a person under investigation (PUI) for COVID-19, based on recommendations from the CDC and the Maryland Department of Health (Baltimore, Maryland USA).9,10 These criteria include: shortness of breath, cough, sore throat, muscle aches, new loss of sense of smell or taste, or diarrhea.10
During the first several months of the COVID-19 pandemic, the EMS system experienced a significant decrease in calls for service, but an increase in out-of-hospital deaths, potentially indicating higher acuity of calls and/or people waiting too long to activate the EMS system.11 Although the impact of COVID-19 on maternal prehospital care is currently unknown, EMS systems may be experiencing a higher acuity in obstetric calls as people defer care until absolutely necessary. This study sought to examine the frequency and acuity of obstetric-related 911 calls for EMS in the state of Maryland during the first 103 days of the pandemic period, as compared to the same time period during the previous year, to assess for any changes to volume or acuity of obstetric-related 911 calls.
Methods
This was a retrospective observational study of obstetric-related 911 activations for EMS comparing the first 103 days of the pandemic period (March 10, 2020 through July 20, 2020) to the pre-pandemic period during the same time frame in the prior year (March 10, 2019 through July 20, 2019). All 911 calls for EMS that occurred in the state of Maryland between the two study periods were included in the study if they: (1) contained specific dispatch determinant codes related to pregnancy, or (2) contained non-obstetric specific dispatch determinant codes (eg, seizure, hemorrhage) and the EMS clinician’s documented primary or secondary impression indicated the patient was pregnant. All calls that were cancelled (prior to response or at the arrival on the scene) or calls in which no patient was found on the scene were excluded. Data were extracted via bulk query, de-identified, and provided to the research team by MIEMSS. Maryland EMS data contain state-wide prehospital care information collected from all 26 EMS jurisdictions and is centrally coordinated by MIEMSS. A descriptive analysis was then performed on all pre-defined categorical variables including dispatch date, dispatch determinant code, clinician primary and secondary impression, initial and final patient priority, patient vitals, and disposition. The initial designated priority of the call, determined by the dispatcher using standardized practices, and the final priority of the call, determined by the primary EMS clinician on scene with the patient, were used as indicators of call acuity. Priority 1 indicated critical illness, Priority 2 indicated less serious condition requiring emergency medical attention, Priority 3 indicated non-emergent condition, and Priority 4 indicated deceased or not requiring medical attention. Additionally, whether the patient met PUI criteria for COVID-19 was also reported.
All data were recorded in electronic format (Microsoft Excel; Microsoft Corp.; Redmond, Washington USA) and sent in aggregate to the research team for analysis. All analyses were conducted using IBM SPSS Statistics for Windows, version 25 (IBM Corp.; Armonk, New York USA). A comparative analysis was used to analyze the difference in frequency and acuity of calls between the two study periods. Independent samples were assessed using the Welch’s T-test given unequal variance in total EMS calls. The study was reviewed by the Johns Hopkins Medicine (JHM; Baltimore, Maryland USA) Institutional Review Board, protocol number IRB00258794.
Results
During the pre-pandemic period from March 10 through June 20, 2019, there were a total of 99,330 911 patient encounters for female patients by EMS in Maryland, of which 1,504 EMS activations were for obstetric-related concerns (1.5%). During the pandemic period from March 10 through June 20, 2020, there were a total of 79,398 EMS encounters for female patients with 1,286 activations for obstetric-related concerns (1.6%). There was an overall 20% decrease in EMS female patient encounters for any indication during the pandemic compared to the year prior, and a 14.5% decrease in obstetric-related calls. When assessing the average calls per day, there was also a lower average number of total EMS calls for female patients per day during the pandemic (2020) compared to the same time frame in 2019 (mean [SD] = 770.9 [SD = 70.1] versus 964.4 [SD = 50.4]; P <.001; Figure 1) and a lower daily average number of EMS calls for obstetric-related indications (12.5 [SD = 3.8] versus 14.6 [SD = 4.1]; P <.001; Figure 2) in 2020. However, there was no statistically significant difference between the two periods in the percentage of total calls that were for obstetric-related concerns (1.6% in 2020 versus 1.5% in 2019; P = .091).
Figure 1.
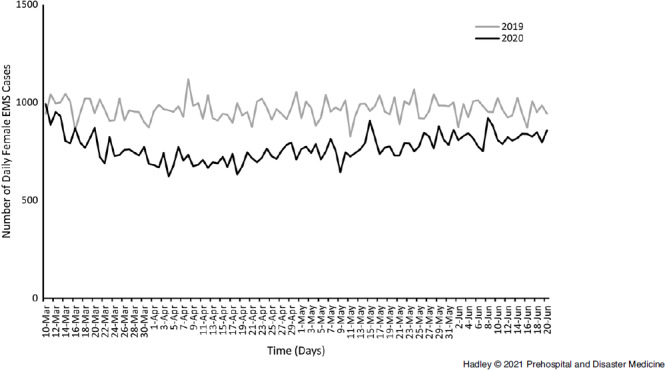
Daily EMS Encounters for All Female Patients from March 10-June 20, 2019 versus 2020.
Abbreviation: EMS, Emergency Medical Services.
Figure 2.
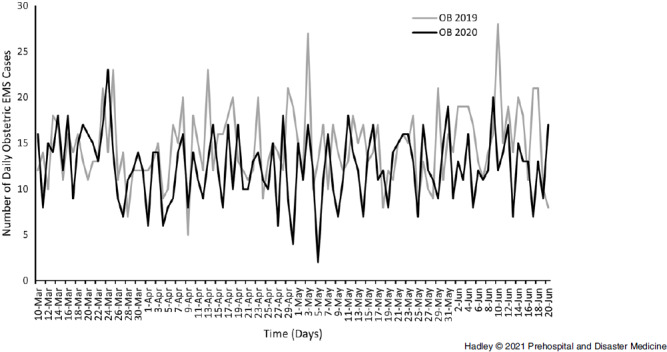
Daily EMS Encounters for Obstetric Indications from March 10-June 20, 2019 versus 2020.
Abbreviation: EMS, Emergency Medical Services.
Demographic data were collected on both age and race of patients treated by EMS clinicians. During the COVID-19 pandemic, most EMS activations were for pregnant women 20-29 years of age (570; 44.3%) followed by those 30-39 years of age (394; 30.6%). Race was often not specified (43.1%), but of those recorded, most women were Black or African American (448; 34.8%) followed by White (202; 15.7%). Locations where EMS calls occurred were also assessed, with most occurring from house/apartment/mobile homes (1,028; 79.9%). Data from 2019 revealed similar demographic trends with no statistically significant difference between pre-pandemic and pandemic time periods (Table 1). However, when compared to the proportion of Black or African American individuals residing in Maryland (29.5%), Black or African American comprised a greater proportion of 911 calls in both 2019, before the pandemic (36.2%; 95% CI, 33.8-38.6; P <.001), as well as during the pandemic in 2020 (34.8%; 95% CI, 32.2-37.4; P <.001).12
Table 1.
Characteristics of Obstetric-Related 911 Calls in Maryland from March 10-June 20, 2019 and 2020
| 2019 (N = 1,504) | 2020 (N = 1,286) | |
|---|---|---|
| Patient Age [mean (SD)] | 30.1 (SD = 14.0) | 30.5 (SD = 13.6) |
| Age Group | ||
| 0-9 | 36 (2.39%) | 24 (1.87%) |
| 10-19 | 152 (10.1%) | 120 (9.33%) |
| 20-29 | 695 (46.2%) | 570 (44.3%) |
| 30-39 | 430 (28.6%) | 394 (30.6%) |
| 40-49 | 79 (5.25%) | 74 (5.75%) |
| 50-59 | 33 (2.19%) | 23 (1.79%) |
| 60-69 | 9 (0.60%) | 22 (1.71%) |
| 70-79 | 25 (1.66%) | 24 (1.87%) |
| 80+ | 33 (2.19%) | 22 (1.71%) |
| Data Not Available | 12 (0.80%) | 13 (1.01%) |
| Race | ||
| Black or African American | 545 (36.2%) | 448 (34.8%) |
| Hispanic or Latino | 37 (2.46%) | 50 (3.89%) |
| Not Specified | 657 (43.7%) | 555 (43.2%) |
| Other Races | 39 (2.66%) | 31 (2.49%) |
| White | 226 (15.0%) | 202 (15.7%) |
| Incident Location | ||
| Assisted Living Facility - Home | 28 (1.86%) | 19 (1.48%) |
| Hotel/Motel - Building/Premises | 28 (1.86%) | 30 (2.33%) |
| House/Apartment/Mobile Home - Home | 1,067 (70.9%) | 1,028 (79.9%) |
| Transports and Roadway | 93 (6.18%) | 62 (4.82%) |
| Others | 288 (19.2%) | 147 (11.4%) |
Using priority status as indicators of call acuity, there was no statistical difference in the acuity of obstetric-related activations between the pre-pandemic and pandemic time periods, with most activations assigned Priority 3 on initial priority during both the pre-pandemic (923; 61.4%) and pandemic (771; 60.0%) time periods. Most activations were also assigned Priority 3 on final priority during the pre-pandemic (841; 55.9%) and pandemic (675; 52.5%) periods. Although the occurrence of Priority 4 calls was too infrequent to detect a significant difference, there were more Priority 4 calls during the COVID-19 pandemic (10; 0.8%) than prior to the pandemic (6; 0.4%). Whether or not the patient was transported to a higher level of care (final disposition) was also assessed. During the pandemic, 1,170 (91.0%) calls for obstetric concerns resulted in patient transport, while during the pre-pandemic time period, 1,423 (94.6%) calls resulted in transport (X2 (1, N = 2790) = 13.96; P <.001; Table 2).
Table 2.
Indicators of Acuity for Obstetric-Related 911 Calls in Maryland from March 10-June 20, 2019 and 2020
| 2019 (N = 1,504) | 2020 (N = 1,286) | |
|---|---|---|
| Initial Priority | ||
| Not Specified | 1 (0.07%) | 3 (0.23%) |
| Priority 1 | 39 (2.59%) | 45 (3.50%) |
| Priority 2 | 535 (35.6%) | 459 (35.7%) |
| Priority 3 | 923 (61.4%) | 771 (60.0%) |
| Priority 4 | 6 (0.40%) | 8 (0.62%) |
| Final Priority | ||
| Not Required/Not Specified | 122 (8.11%) | 145 (11.3%) |
| Priority 1 | 33 (2.19%) | 30 (2.33%) |
| Priority 2 | 508 (33.8%) | 434 (33.7%) |
| Priority 3 | 841 (55.9%) | 675 (52.5%) |
| Priority 4 | 0 (0.00%) | 2 (0.16%) |
| Initial Respiratory Rate | ||
| Abnormal | 161 (10.7%) | 136 (10.6%) |
| Normal | 1,193 (79.3%) | 977 (76.0%) |
| Not Documented | 150 (9.97%) | 173 (13.5%) |
| Initial Pulse Oximetry | ||
| ≤92 | 30 (1.99%) | 20 (1.56%) |
| Normal | 1,387 (92.2%) | 1,170 (91.0%) |
| Not Documented | 87 (5.78%) | 96 (7.47%) |
| Initial Temperature | ||
| <96° F | 3 (0.20%) | 5 (0.39%) |
| >100.4° F | 1 (0.07%) | 5 (0.39%) |
| 96°-100.4° F | 97 (6.45%) | 364 (28.3%) |
| Not Documented | 1,403 (93.3%) | 912 (70.9%) |
| Initial Heart Rate | ||
| <100 | 971 (64.6%) | 797 (62.0%) |
| ≥100 | 483 (32.1%) | 438 (34.1%) |
| Not Documented | 50 (3.32%) | 51 (3.97%) |
| Incident Patient Disposition | ||
| Non-Transports | 81 (5.39%) | 116 (9.02%) |
| Transports | 1,423 (94.6%) | 1,170 (91.0%) |
Vital signs were also assessed as a marker of maternal status at the time of the EMS arrival. There was no significant difference in initial respiratory rate, pulse oximetry, or heart rate between the two time periods assessed. During the pandemic, five women had a fever on arrival (0.39%) versus only one in the pre-pandemic period (0.07%). Most (98.1%) of the obstetric patients who utilized the EMS system during the pandemic met criteria for PUI for COVID-19.
Discussion
Much of the literature on maternal health during the pandemic has focused on hospital and out-patient settings. Early assessment of the EMS systems in the United States during the pandemic demonstrated that call volumes initially decreased, but the incidence of prehospital deaths increased, which could indicate higher acuity of EMS calls as people delay health care.11,13 For other urgent scenarios, such as myocardial infarctions, avoidance of the health system due to fear of COVID-19 and fear of burdening the health system led to delays in presentation to the emergency department and worsening of clinical presentations.14 A similar phenomenon, if seen among pregnant women, would have major implications for first responders. Delays in obstetric care can result in a multitude of critical presentations, including severe hypertension, eclampsia, placenta previa, placental abruption, preterm birth, ruptured ectopic pregnancy, pregnancy loss, maternal infections, unanticipated out-of-hospital birth, and hemorrhage. Some EMS systems, such as New York City (New York USA) have reported increases in out-of-hospital births.15 Several studies have reported increased maternal anxiety, especially regarding attendance of appointments in health care settings.16–18 Stress during pregnancy is associated with lower birthweight, maternal depression, and adverse neurodevelopment outcomes in children.19–21 In addition, maternal anxiety regarding the pandemic contributes to delays in care and can impact surveillance of severe maternal conditions such as hypertensive disorders.22
The findings from this analysis showed that the overall volume of obstetric-related EMS calls in Maryland decreased slightly during the pandemic, while the percentage of total calls did not change significantly. In addition, key indicators of maternal status at the time of the call, including initial and final patient clinical priority as well as maternal vital signs, were not significantly different between the two time periods. This indicates that pregnant women in Maryland were likely not experiencing significant disruptions in their access to urgent/emergent obstetric care, which may have prevented increased utilization of emergency services. It is worthy of note that since hospital data were not assessed in this study, women may have opted for self-transport to avoid multiple points of interaction with the health system. Future studies utilizing hospital admissions data could help clarify this outcome. The study showed a significant decrease in the number of obstetric-related calls that resulted in patient transport during the pandemic. This could reflect that patients were less frequently presenting with significant enough symptoms to warrant transportation by EMS.
In Maryland, Black or African American individuals (non-Hispanic) make up 29.5% of the population.12 However, in this series, an over-representation of obstetric-related EMS calls for Black or African American women was observed (36.2% in 2019 and 34.8% in 2020). This suggests that the EMS system responds disproportionately to this population and is likely reflective of the broader systemic differences in access to and quality of obstetric care that shape disparities in maternal morbidity and mortality. This is consistent with other reports of racial disparities in prehospital care in the United States, furthering the evidence that this setting demands attention in the national pursuit of health equity.23,24 These EMS data should be incorporated into health disparities research to further understand the structural causes and impacts of these differences on maternal health outcomes.
Emergency Medical Services plays a key role as the first members of the health care team to often contact patients experiencing obstetric emergencies. This study provides an opportunity to raise awareness, develop educational materials for EMS personnel, and inform public health issues surrounding obstetric care as the pandemic continues, in an effort to mitigate the pandemic’s impact on maternal morbidity.
Limitations
This study has several limitations. As a retrospective analysis, data quality associated with EMS documentation may exclude some pregnant patients if they were not documented as being pregnant. As such, it is possible they were inadvertently not included in the analysis. This analysis was limited to the information provided to the 911 call taker and to the EMS clinician’s documentation of pregnancy or obstetric-related concern and did not include a comprehensive review of each patient encounter. The methods attempted to account for this by broadening inclusion criteria to include calls in which the primary or secondary impressions were pregnancy-related, in addition to those with specific obstetric-related dispatch codes. The study was also limited to EMS in the state of Maryland. Although Maryland’s EMS system is state-wide, it is possible that other EMS jurisdictions are experiencing different trends in utilization by pregnant women during the COVID-19 pandemic. However, this state-wide analysis provides valuable insight into the broader context of health care and EMS utilization by pregnant patients during this unprecedented health care crisis. Finally, this study was retrospective, which limited the ability to draw conclusions about causation for the differences observed, as there may have been confounding variables which could not be accounted for in the analysis. As such, this study’s utility is primarily hypothesis generating, as opposed to hypothesis testing. Future studies could be designed to prospectively assess the utilization and acuity patterns and outcomes of the EMS system by pregnant patients during a pandemic.
Conclusion
During the COVID-19 pandemic in Maryland, there was no appreciable difference in the state-wide utilization of EMS by pregnant women. Although a slight decrease in call frequency was observed for obstetric concerns, this was in proportion to overall call volume, and there was no increase in call acuity. Therefore, despite concerns that pregnant women might delay health care out of fear and anxiety during the COVID-19 pandemic, this does not appear to have occurred. The additional finding of a higher proportional use of EMS services by minority ethnic groups is an important aspect of care that should be explored in health disparities research as well as resource allocation. This study highlights the potential importance of EMS data in both health disparities as well as emerging infectious disease research.
Acknowledgements
The authors would like to acknowledge Cyd Eaton, PhD and the Johns Hopkins Bead Core for biostatistical support in the analysis portion of this project.
Conflicts of interest/funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. No authors have any conflicts of interest to disclose.
Author Contributions
MEH and MJL conceived the project. MEH, MJL, and TPC conducted background research and drafted the initial manuscript. MEH, TA, MJL, TPC, and AJV conducted the analysis. All authors refined the manuscript, crafted the discussion, and contributed substantially to the manuscript’s revision. MJL takes responsibility for the paper as a whole.
References
- 1. World Health Organization. Rolling updates on coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed November 3, 2020.
- 2. World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/?gclid=Cj0KCQiA0fr_BRDaARIsAABw4Eu3F2X7gjRWFOiP8SqMhyLBUG1AF5Avpvr6IIUHKq06rtvAZ2qiSnwaAmbIEALw_wcB. Accessed January 10, 2021.
- 3. Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status – United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):769–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Matar R, Alrahmani L, Monzer N, et al. Clinical presentation and outcomes of pregnant women with COVID-19: a systematic review and meta-analysis. Clin Infect Dis. 2021;72(3):521–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sentilhes L, De Marcillac F, Jouffrieau C, et al. Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol. 2020;223(6):914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hessami K, Homayoon N, Hashemi A, Vafaei H, Kasraeian M, Asadi N. COVID-19 and maternal, fetal and neonatal mortality: a systematic review. J Matern Fetal Neonatal Med. 2020. Epub ahead of print. [DOI] [PubMed]
- 7. Takemoto ML, Menezes MO, Andreucci CB, et al. Maternal mortality and COVID-19. J Matern Fetal Neonatal Med. 2020. Epub ahead of print. [DOI] [PubMed]
- 8. Kc A, Gurung R, Kinney MV, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. 2020;8(10):e1273–e1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention. Clinical Care Guidance for Healthcare Professionals about Coronavirus (COVID-19). National Center for Immunization and Respiratory Disease. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care.html. Accessed November 25, 2020.
- 10. Maryland Institute for Emergency Medical Services. Maryland Institute for Emergency Medical Services Systems COVID-19 EMS Guidance. https://www.miemss.org/home/Portals/0/Docs/Infectious_Diseases/Guidance-COVID-19-EMS-Guidance-20201006.pdf?ver=2020-10-06-140048-197. Accessed November 25, 2020.
- 11. Lerner EB, Newgard CD, Mann NC. Effect of the coronavirus disease 2019 (COVID-19) pandemic on the US Emergency Medical Services system: a preliminary report. Acad Emerg Med. 2020;27(8):693–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Population Review. Maryland Population 2020. Maryland State Data Center. https://worldpopulationreview.com/states/maryland-population. Accessed January 19, 2021.
- 13. National EMS Information System. 2014 National Emergency Medical Services Information System. Salt Lake City, Utah USA: National EMS Information System; 2014. [Google Scholar]
- 14. Aldujeli A, Hamadeh A, Briedis K, et al. Delays in presentation in patients with acute myocardial infarction during the COVID-19 pandemic. Cardiol Res. 2020;11(6):386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. de Freytas-Tamura K. Pregnant and Scared of ‘Covid Hospitals,’ They’re Giving Birth at Home. New York Times. ~ʼʼ’https://www.nytimes.com/2020/04/21/nyregion/coronavirus-home-births.html#:~:text=home%2Dbirths.html-,Pregnant%20and%20Scared%20of%20ʼCovid%20Hospitals%2Cʼ%20They’re,home%20or%20in%20birthing%20centers. Accessed January 19, 2021.
- 16. Haruna M, Nishi D. Perinatal mental health and COVID-19 in Japan. Psychiatry Clin Neurosci. 2020;74(9):502–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Taubman-Ben-Ari O, Chasson M, Abu Sharkia S, Weiss E. Distress and anxiety associated with COVID-19 among Jewish and Arab pregnant women in Israel. J Reprod Infant Psychol. 2020;38(3):340–348. [DOI] [PubMed] [Google Scholar]
- 18. Kotabagi P, Fortune L, Essien S, Nauta M, Yoong W. Anxiety and depression levels among pregnant women with COVID-19. Acta Obstet Gynecol Scand. 2020;99(7):953–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Corbett GA, Milne SJ, Hehir MP, Lindow SW, O’Connell MP. Health anxiety and behavioral changes of pregnant women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol. 2020;249:96–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):25–35. [DOI] [PubMed] [Google Scholar]
- 21. Martini J, Knappe S, Beesdo-Baum K, Lieb R, Wittchen HU. Anxiety disorders before birth and self-perceived distress during pregnancy: associations with maternal depression and obstetric, neonatal and early childhood outcomes. Early Hum Dev. 2010;86(5):305–310. [DOI] [PubMed] [Google Scholar]
- 22. Takemoto MLS, Menezes MO, Andreucci CB, et al. Maternal mortality and COVID-19. J Matern Fetal Neonatal Med. 2020. Epub ahead of print. [DOI] [PubMed]
- 23. Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166(5):534–543. [DOI] [PubMed] [Google Scholar]
- 24. Hewes HA, Dai M, Mann NC, Baca T, Taillac P. Prehospital pain management: disparity by age and race. Prehosp Emerg Care. 2018;22(2):189–197. [DOI] [PubMed] [Google Scholar]


