Abstract
Background
Malaria continues to be a major disease of public health concern affecting several million people worldwide. The World Health Organization (WHO) started a pilot study on a malaria vaccine (RTS,S) in Ghana and two other countries in 2019. This study aimed at assessing the factors associated with uptake of the vaccine in the Sunyani Municipality of Ghana.
Methods
The study was a cross-sectional study employing a quantitative approach. Stratified sampling technique was used to select respondents. A structured questionnaire was administered to parents/caregivers with children eligible to have taken the first three doses of the malaria vaccine by December 2019. The Child Welfare Clinic (CWC) cards of the eligible children were also inspected. Ordinal logistic regression analysis was done to determine the association between the independent variables and full vaccine uptake.
Results
Uptake of RTS,S 1 was 94.1%. However, this figure reduced to 90.6% for RTS,S 2, and 78.1% for RTS,S 3. Children with a parent who had been educated up to the tertiary level had 4.72 (AOR: 4.72, 95% CI 1.27–17.55) increased odds of full uptake as compared to those who completed secondary education. Parents whose children had experienced fever as an adverse reaction were more likely to send their children for the malaria vaccine as compared to those whose children had ever suffered abscess as an adverse reaction (AOR: 2.27, 95% CI 1.13–5.10). Children with parents who thought vaccines were becoming too many for children had 71% (AOR: 0.29, 95% CI 0.14–0.61) reduced odds of full uptake as compared to those who thought otherwise.
Conclusion
Uptake of RTS,S 1 and RTS,S 2 in Sunyani Municipality meets the WHO’s target coverage for vaccines, however, RTS,S 3 uptake does not. Furthermore, there is a growing perception amongst parents/caregivers that vaccines are becoming too many for children which negatively affects uptake.
Keywords: Malaria, Vaccine, Uptake
Background
Malaria continues to be a major disease of public health concern affecting several million people worldwide. According to the 2018 world malaria report, about 219 million malaria cases occurred worldwide in 2017. The report further indicates that sub-Saharan Africa represents the region with the highest burden. Ghana, together with nine other African countries and India contributes about 70% of the world’s total malaria burden. Children under 5 years of age are the worst affected. In 2017, 49% and 61% of malaria cases and deaths respectively occurred in this age group according to the same report [1].
In Ghana, 11 million suspected cases of malaria and 5.5 million cases of confirmed malaria were estimated to have occurred in 2018. Approximately 30% of these cases occurred in children under 5 [2]. Malaria is an entirely preventable disease [3]. Several interventions have been introduced over the years in a bid to control malaria. Despite the proven effectiveness of these malaria control interventions, uptake remains low in some parts of the world [1]. The latest intervention to be introduced is the malaria vaccine.
The malaria vaccine known as Mosquirix, RTS,S/AS01, or simply RTS,S is the first vaccine proven to offer partial protection against malaria [3]. The World Health Organization (WHO), however, recommends the use of the vaccine on a pilot basis to inform its broader use. Subsequently, the world body approved a phased introduction of the malaria vaccine in 2019. Ghana, Kenya, and Malawi are the countries involved in this pilot study, in a program called Malaria Vaccine Implementation Programme (MVIP). Selected areas within these countries have been enrolled unto the programme [4].
In Ghana, between 120,000 and 150,000 children in 33 selected districts/Municipalities are targeted to receive the vaccine each year. The vaccine is to be given in four doses at 6, 7, 9 and 24 months of age through the routine Expanded Programme on Immunization (EPI) system [5].
Administration of the first doses of the malaria vaccine in Ghana begun in May 2019. However, news of the introduction of the vaccine was met with viral videos and messages on social media of some persons calling on the public to reject the vaccine. There were claims that the vaccine was unsafe and that Ghanaians were deceptively being used for vaccine trials [6].
The malaria vaccine is envisaged to prevent four out of ten malaria cases and three out of ten malaria deaths [3]. Nonetheless, globally, an estimated 1.5 million children die as a result of missing out on life-saving vaccines yearly [7]. In 2014, 31% out of the 216 districts in Ghana did not achieve the target coverage of 80% for the proxy vaccine (Penta 3), indicating that some children continue to miss out on life-saving vaccines in Ghana [8].
The expected impact of the malaria vaccine is not likely to be seen in Ghana if uptake of the vaccine is not optimum. This study, therefore, sought to assess the factors associated with malaria vaccine uptake in the Sunyani Municipality of Ghana so that uptake can be maximized.
Methods
Study area
Sunyani Municipality is one of the 27 administrative districts in the Bono region of Ghana. Its estimated population for 2019 was 151,378. Sunyani is the Municipality’s capital. It lies between Latitudes 70º20′N and 70º05′N, and Longitudes 20º30′W and 20º10′W. It shares boundaries with Sunyani West district to the north, Asutifi district to the south, Tano North district to the east, and Dormaa East district to the west. The Municipality has a total land area of 829.3 square kilometres. One-third of the total land area is not inhabited or cultivated which provides arable land for development [9].
The Municipal Health Directorate (MHD) is in charge of health administration in the district. There are 33 health facilities that provide care to inhabitants of the Municipality. The Municipality is zoned into 34 functional Community-based Health Planning and Service (CHPS) zones under six sub-Municipalities. The sub-Municipalities are Abesim, Antwikrom, Newtown/Baakoniaba, New Dormaa, Sunyani central, and Penkwase. The CHPS zones are demarcated areas for the delivery of health services [9].
Childhood vaccines are delivered at health facilities and outreach points within the Municipality. The outreach points serve to deliver vaccines at the doorsteps of beneficiaries so that physical access does not hinder uptake. The outreach points are organized under the various CHPS zones in the 6 sub-Municipalities. The Municipality is noted for being one of the best in terms of vaccine coverage in the country. It is one of the reasons why it was selected as one of the implementing districts under the MVIP [9].
Study design and sampling
The study was an analytical cross-sectional study employing a quantitative approach.
Structured questionnaire and an observation checklist were used to collect data on malaria vaccine uptake and related factors. The assessment was done at a point in time giving a snapshot of the situation. Data was collected from parents/caregivers in Sunyani Municipality about themselves and their children on factors related to malaria vaccine uptake.
Cochrane’s formula was used in to calculate the sample size; where n = sample size; Z = standard normal variate for margin of error; p = proportion of children who take RTS,S vaccine; q = 1-p; d = margin of error.
Since this study was on uptake of a new vaccine, an assumed proportion of uptake of 50% was employed; using a margin of error of 5% and a 10% adjustment for non-response, the calculated sample size was 424.
Stratified sampling technique proportionate to size was used in selecting participants from the six sub-Municipalities which served as strata. There are differences in the characteristics of the sub-Municipalities. Employing stratified sampling technique ensured that all sub-Municipalities were represented in the sample. It also allowed comparison to be made across sub-Municipalities.
In determining the proportionate sample size for each sub-Municipality, the formula below was used:
where A is the sampling fraction, ‘y’ is the sample size = 424, and ‘z’ is the 2019 monthly target coverage for vaccines in Sunyani Municipality = 505.
The sampling fraction was applied to the monthly target of each sub-Municipality to determine the sample size for each sub-Municipality as shown in Table 1.
Table 1.
Sample size determination by sub-Municipality (proportionate to size)
| Sub-Municipality | Monthly target (x) | Sample fraction × x | Sample size |
|---|---|---|---|
| Abesim | 80 | × 80 | 67 |
| Antwikrom | 53 | × 53 | 45 |
| New Dormaa | 122 | × 122 | 102 |
| Newtown/Baakoniaba | 93 | × 93 | 78 |
| Penkwase | 78 | × 78 | 65 |
| Sunyani central | 80 | × 80 | 66 |
| Total | 505 | 424 |
Systematic sampling was then used to select respondents from each stratum. A sampling frame was constructed using the Child Welfare Clinic (CWC) registers at the various CHPS zones. The CWC registers contain the official records of each vaccinated child in a particular CHPS zone. The frame contained the names of children who were eligible to have taken the first 3 doses of the malaria vaccine by December 2019, for each sub-Municipality. A sampling interval was determined for each sampling frame using the formula:
where K = sampling interval, N = the number of children in the sampling frame, and n = sample size for the sub-Municipality. Simple random sampling was used to select the first sample by writing the names of the children from one to the sampling interval, folded and mixed up in a bowl. One piece of paper was selected and the name on the paper represented the first sample. Subsequent samples were drawn by adding the sampling interval to the number of the first drawn sample until all samples required for the sub-Municipality were drawn.
The parents/caregivers of the selected children were contacted and those who agreed to be part of the study were interviewed.
Data collection
Data was collected through the administration of questionnaires to respondents and observation of CWC cards. Parents/caregivers were contacted at CWCs or in their houses depending on where they were available to respond to the questionnaire. Questions centred on socio-demographic factors and other independent variables known to affect vaccine uptake. The other independent variables assessed were: knowledge about malaria vaccine, previous experience with vaccines and vaccination, affordability, and accessibility of vaccines in Sunyani Municipality.
The observation checklist centred on the uptake of malaria vaccine. The CWC card of the children provided this information.
Each questionnaire administration and CWC card observation lasted about 20 min.
To ensure voluntary participation in the study, informed consent was obtained from each parent/caregiver before data collection. None of the parents/caregivers contacted refused to participate in the study, indicating a 100% response rate.
Data analysis
The data was cleaned and entered into Microsoft excel. Entries were double-checked for errors and corrections made. It was then imported to STATA version 15 and analysed. Frequencies and percentages were generated for sociodemographic characteristics such as age, occupation, marital status, religion, and sex. Median and ranges were generated for the continuous variables.
Uptake of the malaria vaccine was measured as levels: no uptake (no dose received), partial uptake (either first or second dose received), and full uptake (all first three doses received). Ordinal logistic regression analysis was done to determine the association between the independent variables and the level of malaria vaccine uptake. The regression was done first at the univariate level. Independent variables with significant p values at the univariate level were used in a multivariate analysis and the model with the best Akaike’s Information Criterion (AIC) and Bayesian’s Information Criterion (BIC) was selected. For all associations, significance level was set at 5%.
Results
Socio-demographic characteristics
A total of 424 parents/caregivers and 424 children participated in the study They were drawn from the six sub-Municipalities in the Sunyani Municipality. The study lasted approximately 10 months.
The median age of parents/caregivers was 29 years (27, 32 years). It ranged from 17 to 45 years. Majority of them (99.3%) were parents with almost all being females (99.5%). Most respondents (60.9%) were married with the rest being either single or cohabiting. Up to 43.2% of respondents had up to secondary education, whiles up to 41.5% of their partners, mostly males had up to tertiary education. Most of the respondents were Christians (75%). Up to 55.2% of respondents were self-employed, whiles 20.5% of respondents were unemployed. However, only 2.6% of their partners were unemployed.
Details of the distribution of the socio-demographic characteristics of respondents are shown in the Table 2.
Table 2.
Distribution of socio-demographic characteristics of study participants, Sunyani Municipal, 2020
| Characteristic (n = 424) | Frequency | Percentage (%) |
|---|---|---|
| Sub-Municipality | ||
| Abesim | 68 | 16.0 |
| Antwikrom | 45 | 10.6 |
| Newtown/Baakoniaba | 78 | 18.4 |
| New Dormaa | 102 | 24.1 |
| Sunyani central | 66 | 15.6 |
| Penkwase | 65 | 15.3 |
| Age (years) | ||
| 15–19 | 11 | 2.6 |
| 20–24 | 46 | 10.9 |
| 25–29 | 171 | 40.3 |
| 30–34 | 151 | 35.6 |
| 35 and above | 45 | 10.6 |
| Parent or caregiver | ||
| Parent | 421 | 99.3 |
| Caregiver | 3 | 0.7 |
| Sex | ||
| Male | 2 | 0.5 |
| Female | 422 | 99.5 |
| Marital status | ||
| Single | 99 | 23.4 |
| Married | 258 | 60.9 |
| Cohabiting | 67 | 15.8 |
| Number of children alive | ||
| 1–3 | 378 | 89.2 |
| More than 3 | 46 | 10.8 |
| Educational status | ||
| No formal education | 28 | 6.6 |
| Primary education | 141 | 33.3 |
| Secondary education | 183 | 43.2 |
| Tertiary education | 72 | 17.0 |
| Educational status of partner | ||
| No formal education | 14 | 3.3 |
| Primary education | 72 | 17.1 |
| Secondary education | 161 | 38.2 |
| Tertiary education | 175 | 41.5 |
| Religion | ||
| Christianity | 318 | 75.0 |
| Islam | 103 | 24.3 |
| Traditionalist | 3 | 0.7 |
| Occupation | ||
| Unemployed | 87 | 20.5 |
| Self-employed | 234 | 55.2 |
| Farming | 32 | 7.6 |
| Civil servant | 71 | 16.8 |
| Religion of partner (n = 421) | ||
| Christianity | 317 | 75.3 |
| Islam | 100 | 23.8 |
| Traditionalist | 4 | 1 |
| Occupation of partner | ||
| Unemployed | 11 | 2.6 |
| Self-employed | 220 | 52.3 |
| Farming | 40 | 9.5 |
| Civil servant | 150 | 35.6 |
Characteristics of children studied, Sunyani Municipality, 2020
Out of the 424 children, 66.3% were aged 15–16 months. Their ages ranged from 13 to 18 months. The median age was 15 months (15, 16 months). Up to 55.4% of them were males. Almost all of them were delivered at a health facility (94.6%).
Details of the characteristics of children studied are shown in Table 3.
Table 3.
Distribution of characteristics of children studied, Sunyani Municipal, 2020
| Characteristic (n = 424) | Frequency | Percentage (%) |
|---|---|---|
| Age (months) | ||
| 13–14 | 79 | 18.6 |
| 15–16 | 281 | 66.3 |
| 17–18 | 64 | 15.1 |
| Sex | ||
| Male | 235 | 55.4 |
| Female | 189 | 44.6 |
| Place of delivery | ||
| Home | 21 | 5.0 |
| Health facility | 401 | 94.6 |
| Unknown | 2 | 0.4 |
Uptake of RTS,S
While 94.1% (95% CI 91.4–96.0%) of the children had been administered the first dose of the malaria vaccine, 90.6% (95% CI 87.4–93.0%) had been administered both the first and the second dose with a reduced percentage of 78.1 (95% CI 73.9–83.8%) having been administered all the three doses.
The reasons given for receiving some but not all the doses of the vaccine were: “did not know when the next one was due” − 45.6%, “was not around”, − 23.5%, and “not comfortable with issues surrounding vaccine” − 13.2%. For those who had received no dose of the vaccine, 60% of the mothers said it was their partner’s (husband) decision not to allow their children to be administered the vaccine whiles the rest said it was their own decision to refuse the vaccine.
Distribution of uptake of malaria vaccine in Sunyani Municipality is shown in Table 4.
Table 4.
Distribution of uptake of malaria vaccine in Sunyani Municipal, 2020
| Characteristic | Frequency | Percentage (%) |
|---|---|---|
| Level of uptake | ||
| No uptake | 25 | 5.9 |
| Partial uptake | 68 | 16.0 |
| Full uptake | 331 | 78.1 |
| RTS,S 1 uptake | ||
| Yes | 399 | 94.1 |
| No | 25 | 5.9 |
| RTS,S 2 uptake | ||
| Yes | 384 | 90.6 |
| No | 40 | 9.4 |
| RTS,S 3 uptake | ||
| Yes | 331 | 78.1 |
| No | 93 | 21.9 |
| Reason for child receiving some but not all doses of RTS,S | ||
| Did not know when next one was due | 31 | 45.6 |
| Was not around | 16 | 23.5 |
| Not comfortable with side effects | 8 | 11.8 |
| Not comfortable with issues surrounding vaccine | 9 | 13.2 |
| Did not take previous one on time | 4 | 5.9 |
| Reason for child receiving none of the doses of RTS,S | ||
| Partner’s (husband) decision to refuse vaccine | 15 | 60.0 |
| Personal decision to refuse vaccine | 7 | 28.0 |
| Did not know child is eligible | 3 | 12 |
Trend of uptake of malaria vaccine in Sunyani Municipality
The uptake of malaria vaccine in Sunyani Municipality shows a declining uptake for the subsequent doses of the vaccine. Whiles uptake for the first dose was 94.1%, it reduced to 90.6% for the second dose and to 78.1% for the third dose. RTS,S 1 and RTS,S 2 uptake met the WHO target of 90% but uptake of RTS,S 3 did not.
A chart of the uptake of the first three doses of malaria vaccine in Sunyani Municipality is shown in Fig. 1.
Fig. 1.
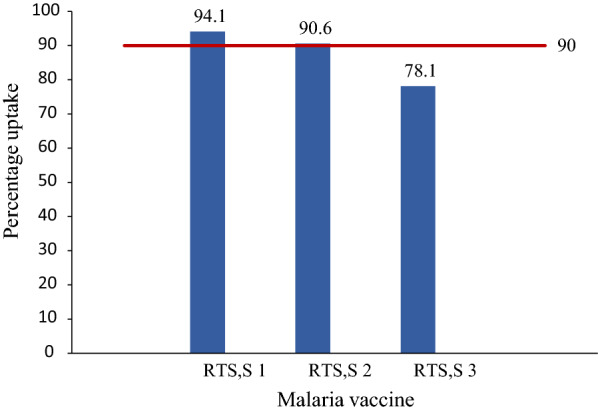
Uptake of malaria vaccine in Sunyani Municipality. Blue bars: uptake (%). Red bars: target
Association between Independent variables and level of malaria vaccine uptake
There was a significant association between the sub-Municipality where one resided and level of uptake. Having a parent who had up to tertiary level education was associated with significantly increased odds of uptake. Details of association between independent variables and level of uptake is shown in Table 5.
Table 5.
Association between independent variables and level of uptake
| Characteristic | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
| Sub-Municipal | 0.79 | 0.69–0.92 | 0.002 |
| Penkwase (base) | 1 | ||
| Abesim | 2.91 | 1.29–6.57 | 0.010 |
| Antwikrom | 5.36 | 1.71–16.79 | 0.004 |
| Newtown/Baakoniaba | 2.28 | 1.08–4.83 | 0.031 |
| New Dormaa | 1.41 | 0.73–2.73 | 0.303 |
| Sunyani central | 2.28 | 1.03–5.08 | 0.043 |
| Age of parent (years) | 1.06 | 0.82–1.37 | 0.616 |
| 20–24 (base) | 1 | ||
| 15–19 | 3.41 | 0.39–29.59 | 0.266 |
| 25–29 | 1.03 | 0.48–2.20 | 0.945 |
| 30–34 | 1.34 | 0.61–2.94 | 0.463 |
| 35 and above | 1.38 | 0.51–3.73 | 0.522 |
| Education level of parent/caregiver | 1.29 | 0.97–1.71 | 0.075 |
| Primary education (base) | 1 | 1 | |
| No formal education | 1.52 | 0.54–4.30 | 0.432 |
| Secondary education | 1.36 | 0.82–2.26 | 0.234 |
| Tertiary education | 2.37 | 1.11–5.08 | 0.026 |
| Education level of partner | 1.02 | 0.78–1.35 | 0.866 |
| Secondary education (base) | 1 | 1 | |
| No formal education | 2.56 | 0.55–11.89 | 0.230 |
| Primary education | 2.46 | 1.19–5.07 | 0.015 |
| Tertiary education | 2.08 | 1.25–3.45 | 0.005 |
| Number of children alive | 0.97 | 0.46–2.04 | 0.940 |
| 1–3 (base) | 1 | 1 | |
| More than 3 | 0.97 | 0.46–2.04 | 0.940 |
| Marital status | 0.80 | 0.55–1.17 | 0.254 |
| Cohabiting (base) | 1 | 1 | |
| Single | 1.60 | 0.78–3.27 | 0.199 |
| Married | 1.68 | 0.91–3.08 | 0.097 |
| Religion of parent/caregiver | 0.73 | 0.44–1.18 | 0.205 |
| Traditionalist (base) | 1 | 1 | |
| Christian | 2.89 | 0.23–35.94 | 0.409 |
| Islam | 2.17 | 0.17–27.63 | 0.551 |
| Religion of partner | 0.73 | 0.45–1.19 | 0.204 |
| Traditionalist (base) | 1 | 1 | |
| Christian | 1.68 | 0.16–17.29 | 0.664 |
| Islam | 1.21 | 0.12–12.85 | 0.872 |
| Occupation of parent/caregiver | 1.34 | 1.03–1.74 | 0.027 |
| Unemployed (base) | 1 | 1 | |
| Self employed | 1.33 | 0.76–2.32 | 0.319 |
| Farmer | 2.66 | 0.85–8.39 | 0.094 |
| Civil servant | 2.21 | 1.00–4.90 | 0.049 |
| Occupation of partner | 1.13 | 0.89–1.43 | 0.305 |
| Self-employed (base) | 1 | 1 | |
| Unemployed | 3.24 | 0.40–26.06 | 0.268 |
| Farmer | 3.07 | 1.05–9.01 | 0.041 |
| Civil servant | 1.365 | 0.84–2.23 | 0.214 |
| Known vaccine preventable diseases | 1.01 | 0.81–1.27 | 0.899 |
| Up to 3 vpds mentioned (base) | 1 | 1 | |
| No correct vpd mentioned | 3.27 | 1.12–9.56 | 0.031 |
| 4–8 correct vpds mentioned | 1.06 | 0.51–2.23 | 0.870 |
| Any correct disease but including malaria | 1.47 | 0.86–2.51 | 0.164 |
| Heard about malaria vaccine | 0.64 | 0.30–1.36 | 0.249 |
| No (base) | 1 | 1 | |
| Yes | 0.64 | 0.30–1.36 | 0.249 |
| Where first heard about malaria vaccine | 0.86 | 0.55–1.35 | 0.510 |
| Friends/relatives (base) | 1 | 1 | |
| CWC | 20.22 | 1.61–253.71 | 0.020 |
| Health facility announcement | 16.78 | 1.18–239.11 | 0.037 |
| Radio | 39.68 | 2.14–737.14 | 0.014 |
| Number of times a child is expected to take the malaria vaccine | 1.26 | 0.67–2.34 | 0.472 |
| Incorrect number (base) | 1 | 1 | |
| Correct number | 1.26 | 0.67–2.34 | 0.472 |
| Schedule of malaria vaccine | 1.26 | 0.55–3.04 | 0.560 |
| Incorrect order (base) | 1 | 1 | |
| Correct order | 1.29 | 0.55–3.04 | 0.560 |
| Heard about any negative report or issue concerning the malaria vaccine | 1.72 | 1.03–2.88 | 0.040 |
| Yes (base) | 1 | 1 | |
| No | 1.72 | 1.03–2.88 | 0.040 |
| Where issue or report was heard | 1.38 | 0.81–2.34 | 0.232 |
| Radio (base) | 1 | 1 | |
| Friends/relatives | 2.75 | 1.37–5.51 | 0.004 |
| Health worker | 2.28 | 0.55–9.44 | 0.255 |
| Other | 1.08 | 0.85–13.60 | 0.954 |
| Did issue/report prevent or delay vaccine acceptance | 8.74 | 4.32–17.70 | < 0.005 |
| Yes (base) | 1 | 1 | |
| No | 8.74 | 4.32–17.70 | < 0.005 |
| Given the option of accepting malaria vaccine at CWC | 1.15 | 0.69–1.93 | 0.591 |
| Yes (base) | 1 | 1 | |
| No | 1.15 | 0.69–1.93 | 0.591 |
| Are vaccines becoming many for children with the introduction of the malaria vaccine | 0.60 | 0.38–0.97 | 0.038 |
| No (base) | 1 | 1 | |
| Yes | 0.60 | 0.38–0.97 | 0.038 |
| Will you recommend malaria vaccine to others | |||
| No (base) | 1 | 1 | |
| Yes | 12.61 | 7.00–22.72 | < 0.005 |
| Child ever suffered an adverse reaction following the administration | 1.14 | 0.72–1.80 | 0.576 |
| No (base) | 1 | 1 | |
| Yes | 1.14 | 0.72–1.80 | 0.576 |
| Reaction child suffered | 0.57 | 0.41–0.81 | 0.001 |
| Abscess (base) | 1 | 1 | |
| Fever | 3.09 | 1.56–6.09 | 0.001 |
| Diarrhoea/vomiting | 5.56 | 0.67–46.00 | 0.111 |
| Did reaction influence acceptance of other vaccines | 1.87 | 0.56–6.27 | 0.311 |
| Yes (base) | 1 | 1 | |
| No | 1.87 | 0.56–6.27 | 0.311 |
| Time taken to reach vaccination centre | 1.09 | 0.69–1.71 | 0.724 |
| Less than 30 min (base) | 1 | 1 | |
| 30–59 min | 1.06 | 0.65–1.74 | 0.820 |
| 1–2 h | 1.51 | 0.18–12.98 | 0.706 |
| Means of getting to vaccination centre | 1.23 | 0.77–1.99 | 0.385 |
| Walking (base) | 1 | 1 | |
| Commercial vehicle | 1.43 | 0.85–2.40 | 0.176 |
| Personal vehicle | 0.411 | 0.07–2.47 | 0.331 |
| Required to pay any money at vaccination centre | 1.24 | 0.62–2.48 | 0.544 |
| Yes (base) | 1 | 1 | |
| No | 1.24 | 0.62–2.48 | 0.544 |
| How to tell when child’s vaccination is due | 0.81 | 0.58–1.12 | 0.195 |
| Visit clinic monthly (base) | 1 | 1 | |
| Check child’d CWC card | 1.57 | 0.97–2.54 | 0.064 |
| Told by nurses | 2.04 | 0.80–5.20 | 0.136 |
| Description of CWC nurses’ attitude | 0.95 | 0.69–1.32 | 0.779 |
| Excellent (base) | 1 | 1 | |
| Very good | 0.50 | 0.22–1.12 | 0.092 |
| Good | 0.61 | 0.27–1.40 | 0.242 |
| Do you think vaccines have long term side effects | 1.01 | 0.33–3.13 | 0.984 |
| Yes (base) | 1 | 1 | |
| No | 1.01 | 0.33–3.13 | 0.984 |
Multivariate analysis showing association between level of uptake and independent variables
Multiple ordered logistic regression analysis using variables that were significant at 5% in the univariate analysis demonstrated that adjusted odds ratio for uptake per sub-Municipality was not significant.
As compared to secondary education, children with a parent who had been educated up to the tertiary level had an increased odds of 4.72 times of completing uptake. Children with parents/caregivers who thought vaccines were becoming too many for them with the addition of the malaria vaccine had 71% reduced odds of full uptake as compared to those who thought otherwise. This association was significant with a p value of 0.001.
Additionally, children who had suffered fever as an adverse reaction had an increased odds of 2.27 of their children completing uptake as compared to those whose children suffered abscess. Details of the multivariate analysis are depicted in Table 6.
Table 6.
Multivariate analysis of association between level of uptake and independent variables
| Characteristic | Crude Odds ratio | 95% Confidence interval | P-value | Adjusted Odds ratio | 95% Confidence interval | P-value |
|---|---|---|---|---|---|---|
| Sub-Municipal | 0.80 | 0.69–0.92 | 0.002 | 0.82 | 0.66–1.02 | 0.076 |
| Penkwase (base) | 1 | 1 | ||||
| Abesim | 2.91 | 1.29–6.57 | 0.010 | 2.21 | 0.53–9.17 | 0.276 |
| Antwikrom | 5.36 | 1.71–16.79 | 0.004 | 2.01 | 0.16–26.03 | 0.593 |
| Newtown/Baakoniaba | 2.28 | 1.08–4.83 | 0.031 | 1.22 | 0.32–4.62 | 0.770 |
| New Dormaa | 1.41 | 0.73–2.73 | 0.303 | 0.36 | 0.10–1.29 | 0.117 |
| Sunyani central | 2.28 | 1.03–5.08 | 0.043 | 0.98 | 0.27–3.50 | 0.971 |
| Education level of partner | 1.02 | 0.78–1.35 | 0.866 | 1.02 | 0.60–1.75 | 0.936 |
| Secondary education (base) | 1 | 1 | ||||
| No formal education | 2.56 | 0.55–11.89 | 0.230 | 0.93 | 0.02–31.06 | 0.970 |
| Primary education | 2.46 | 1.19–5.07 | 0.015 | 4.10 | 1.02–16.47 | 0.047 |
| Tertiary education | 2.08 | 1.25–3.45 | 0.005 | 4.72 | 1.27–17.55 | 0.020 |
| Occupation of partner | 1.13 | 0.89–1.44 | 0.305 | 1.27 | 0.84–1.92 | 0.257 |
| Self-employed (base) | 1 | 1 | ||||
| Unemployed | 3.24 | 0.40–26.06 | 0.268 | 1.74 | 0.17–17.42 | 0.637 |
| Farmer | 3.07 | 1.05–9.01 | 0.041 | 0.97 | 0.08–11.06 | 0.980 |
| Civil servant | 1.365 | 0.84–2.23 | 0.214 | 0.61 | 0.16–2.31 | 0.464 |
| Vaccines becoming many for children with the introduction of the malaria vaccine | 0.60 | 0.38–0.97 | 0.038 | 0.29 | 0.14–0.61 | 0.004 |
| No (base) | 1 | 1 | ||||
| Yes | 0.60 | 0.38–0.97 | 0.038 | 0.29 | 0.14–0.61 | 0.001 |
| Experience with AEFI | 0.57 | 0.41–0.81 | 0.001 | 0.58 | 0.41–0.83 | 0.003 |
| Abscess (base) | 1 | 1 | ||||
| Fever | 3.09 | 1.56–6.09 | 0.001 | 2.27 | 1.13–5.10 | 0.023 |
| Diarrhoea/vomiting | 5.56 | 0.67–46.00 | 0.111 | 6.95 | 0.69–69.77 | 0.099 |
Discussion
Uptake of RTS,S
Findings from this study indicated an uptake of 94.1% for RTS,S 1; 90.6% for RTS,S 2; and 78.1% for RTS,S 3. Uptake of RTS,S 1 and RTS,S 2 thus met the target of 90% coverage for vaccines set by WHO [10]. RTS,S 3 coverage, however, did not meet the set target.
There was a reduction in uptake of subsequent doses of the vaccine. This observed reduction is similar to that observed in Senegal, Cameroun, Nigeria, Togo, Congo, and in the Kwabre East district of Ghana [11–16]. The over 90% uptake recorded for the RTS,S 1 and RTS,S 2 indicates that the anti-vaccine campaigns that greeted the introduction of the malaria vaccine did not impact negatively on the uptake of the vaccine in Sunyani Municipality [6]. This may have been so because the messages were largely on social media and did not really seep down to negatively influence parents/caregivers. It may also have been due to effective public education and other community mobilization strategies employed by the Municipality’s health directorate to create awareness about the vaccine when it was introduced.
Out of the 5.9% of children who had not been administered any dose of the vaccine, most (60%) were attributed to a partner’s decision to refuse the vaccine (Table 4). Almost all the respondents were females indicating that it was the fathers who prevented their children from being administered the vaccine. Fathers play a major role in the family and are usually the decision-makers. Those who prevented their children from being given the vaccine may have been influenced by the anti-vaccine campaigns. Fathers are usually not present at CWCs and so are not likely to benefit from education about vaccines which are usually delivered there.
It may also be the case that mothers were unwilling to admit during the interview that they themselves did not want their children to be vaccinated considering the fact that fathers were not around to respond.
The trend of reduced coverages for subsequent doses of the malaria vaccine may be due to poor knowledge of parent/caregivers about the schedule of the vaccines. This could result in parents/caregivers not presenting their children for the subsequent doses on time or not presenting them at all as was the case of 45.6% of respondents (Table 4). Up to 23.5% of children had not been administered all three doses because their parents/caregivers had travelled when they were due. This can be attributed to the fact that not all districts in the country are administering the vaccine (only districts on the MVIP). Therefore, when parents/caregivers travel to these non-implementing districts, their children may not be administered the vaccine at all or on time.
Factors positively associated with uptake
The findings of higher education and occupation being positive predictors of vaccine uptake are consistent with findings made by Adu, Ofosu, and Mukthar et al. [17–19]. Similarly, the findings of Acharya et al. [15] of higher education being associated with complete uptake was consistent with findings from this study.
Having a higher educated parent was associated with higher odds of complete uptake both in the univariate analysis and the multivariate analysis (AOR: 4.72, 95% CI 1.27–17.55). This could be because highly educated parents have access to more information about the vaccine and were better placed to understand the implementation programme. Since most parents/caregivers who send their wards for vaccination services are women (99.5%), having a partner who has higher education could mean that as the decision-maker, he is more likely to accept the vaccine. Having a higher education is associated with better occupation, the possible reason why civil servants had higher odds of their children completing uptake when compared.
Additionally, having a parent with primary education was also found to be associated with increased odds of full uptake in the multivariate analysis (AOR: 4.10, 95% CI 1.02–16.47) as compared to having a parent with secondary education. This can be attributed to middle level educated parents being more susceptible to misinformation as compared to lower level educated parents. Whiles lower educated parents may rely on official communication such as health education at child welfare clinics and public announcements, middle level educated parents are more likely to be influenced by the anti-vaccine campaigns which were mainly on social media platforms.
Factors negatively associated with uptake
The findings of parents/caregivers having the perception that vaccines are becoming too many for their children is unique to this study per available literature reviewed. Those who thought vaccines for children (32.3%) are becoming many had lower odds of completing uptake (AOR: 0.29, 95% CI 0.14–0.61). This could be that parents/caregivers do not see the benefits of the child being vaccinated overriding the potential adverse effect that could occur when the vaccine is given.
Additionally, parents/caregivers who have children who have ever had fever as an adverse reaction (148/223) following immunization had a higher odds of completing uptake as compared to those who had abscess as an adverse reaction (64/223) (AOR: 3.09, 95% CI 1.56–6.09). This could be related to the fact that most parents/caregivers consider fever to be a minor immediate side effect of vaccines as compared to developing an abscess. They were therefore not likely to ‘risk’ going for a new vaccine the safety of which has been questioned.
Conclusion
Uptake for the first and second doses of the malaria vaccine (RTS,S 1) in the Sunyani Municipality meets WHO’s 90% target. However, uptake of the third dose does not.
Whiles having a higher educated parent is associated with uptake positively, there is a growing perception that vaccines are becoming too many for children and this has a negative impact on uptake.
The Sunyani Municipal Health Directorate and the Ghana Health Service should conduct sustained public education on the malaria vaccine in Sunyani Municipality to further improve upon uptake.
Acknowledgements
Our appreciation goes to all respondents, lecturers of University of Ghana’s School of Public Health and the WHO/TDR project team in Ghana.
Abbreviations
- AEFI
Adverse Event Following Immunization
- ANC
Ante-Natal Care
- AOR
Adjusted odds ratio
- CWC
Child Welfare Clinic
- CHPS
Community-based Health and Planning Service
- EPI
Expanded Programme on Immunization
- GHS
Ghana Health Service
- GVAP
Global Vaccine Action Plan
- MHD
Municipal Health Directorate
- MVIP
Malaria Vaccine Implementation Program
- RTS,S
Malaria vaccine
Appendix
Table 7.
Operational definition and scale of measurement for dependent variable
| Variable | Operational definition | Scale of measurement | Source of data |
|---|---|---|---|
| Uptake of malaria vaccine | Number of doses of malaria vaccine a child has received | Ordinal | Child’s CWC card |
| Full uptake (child has received all 3 doses) | |||
| Partial uptake (child has received either 1st or 2nd dose) | |||
| No uptake (child has not received any dose) |
Malaria vaccine is given in 4 doses at 6, 7, 9 and 24 months of age. Only the first 3 doses were considered in this study
Table 8.
Operational definition and scale of measurement for socio-demographic variables
| Variable | Operational definition | Scale of measurement | Source of data |
|---|---|---|---|
| Age | Age in completed years | Ratio | Interview |
| Sex | Being male or female | Nominal | Observation |
| Place of residence | Sub-Municipality in Sunyani within which parent/caregiver stays | Nominal | Interview |
| Abesim | |||
| Antwikrom | |||
| Sunyani central | |||
| Newtown/Baakoniaba | |||
| New Dormaa | |||
| Penkwase | |||
| Marital status | Legal status of relationship with partner | Nominal | Interview |
| Married | |||
| Single | |||
| Cohabiting | |||
| Religion | Religious denomination | Nominal | Interview |
| Christian | |||
| Muslim | |||
| Traditionalist | |||
| Other | |||
| Religion of partner | Religious denomination | Nominal | Interview |
| Christian | |||
| Muslim | |||
| Traditionalist | |||
| Other | |||
| Educational level | Highest formal education level attained | Ordinal | Interview |
| None | |||
| Primary | |||
| Secondary | |||
| Tertiary | |||
| Educational level of partner | Highest formal education level attained by partner | Ordinal | Interview |
| None | |||
| Primary | |||
| Secondary | |||
| Tertiary | |||
| Occupation | What the individual does for a living (brings him/her regular income) | Nominal | Interview |
| Unemployed | |||
| Self-employed | |||
| Farming | |||
| Civil servant | |||
| Occupation of partner | What the partner does for a living (brings him/her regular income) | Nominal | Interview |
| Unemployed | |||
| Self-employed | |||
| Farming | |||
| Civil servant | |||
| Parity | Number of children alive | Ratio | Interview |
Table 9.
Operational definition and scale of measurement for other independent variables
| Variable | Operational definition | Scale of measurement | Source of data |
|---|---|---|---|
| Knowledge about RTS,S | Whether parent/caregiver has ever heard about the malaria vaccine | Binary | Interview |
| Yes | |||
| No | |||
| Where parent/caregiver first heard about malaria vaccine | Nominal | Interview | |
| CWC | |||
| Health facility announcement | |||
| Radio | |||
| Friend/relative | |||
| Knowledge of the number of times a child is supposed to be administered malaria vaccine | Binary | Interview | |
| Correct number | |||
| Incorrect number | |||
| Knowledge of schedule of malaria vaccine administration | Binary | Interview | |
| Correct order | |||
| Incorrect order | |||
| Perception of vaccines becoming too many | Parent/caregiver thinks vaccines are becoming too many for children with the introduction of malaria vaccine | Binary | Interview |
| Yes | |||
| No | |||
| Concern about vaccine safety | Heard about any negative issue/report concerning malaria vaccine | Binary | Interview |
| Yes | |||
| No | |||
| Previous experience with vaccines | Whether child has ever suffered an adverse reaction following the administration of a vaccine | Binary | Interview |
| Yes | |||
| No | |||
| Accessibility | Minutes spent in reaching nearest CWC | Ratio | Interview |
| Affordability | Payment for vaccination services | Ratio | Interview |
| Perception of quality of vaccination service | Description of CWC nurses’ attitude | Ordinal | Interview |
| Excellent | |||
| Very good | |||
| Good | |||
| Bad | |||
| Very bad | |||
| ANC attendance | Number of times mother attended ANC before delivery of this child | Ratio | Interview |
| Sex of child | Child being male or female | Nominal | Interview |
| Male | |||
| Female | |||
| Place of delivery | Where child was delivered | Nominal | Interview |
| Home delivery | |||
| Health facility | |||
| Time of uptake | Age (in months) at which child was administered any dose of malaria vaccine | Ratio | Child’s CWC card |
Table 10.
EPI schedule In Ghana (without RTS,S)
| Age of administration | Vaccine(s) | Mode of administration |
|---|---|---|
| At birth | BCG, OPV 0 | Intradermal, oral |
| 6 weeks | Penta 1, PCV 1, OPV 1, Rota 1, | Intramuscular, oral |
| 10 weeks | Penta 2, PCV 2, OPV2, Rota 2 | Intramuscular, oral |
| 14 weeks | Penta 3, IPV, PCV 3, OPV 3 | Intramuscular, oral |
| 6 months | Vitamin A | Oral |
| 9 months | Measles-rubella (MR) 1, yellow fever | Sub-cutaneous |
| 12 months | Vitamin A | Oral |
| 18 months | MR 2, Meningococcal ‘A’, Vitamin A | Subcutaneous, intramuscular, oral |
Source: GHS, 2019
Table 11.
EPI schedule with RTS,S for areas on MVIP in Ghana
| Age of administration | Vaccine | Mode of administration |
|---|---|---|
| At birth | BCG, OPV 0 | Intradermal, oral |
| 6 weeks | Penta 1, PCV 1, OPV 1, Rota 1, | Intramuscular, oral |
| 10 weeks | Penta 2, PCV 2, OPV 2, Rota 2 | Intramuscular, oral |
| 14 weeks | Penta 3, IPV, PCV 3, OPV 3 | Intramuscular, oral |
| 6 months | Vitamin A, RTS,S 1 | Oral, intramuscular |
| 7 months | RTS,S 2 | Intramuscular |
| 9 months | Measles-rubella (MR) 1, yellow fever, RTS,S 3 | Subcutaneous, intramuscular |
| 12 months | Vitamin A | Oral |
| 18 months | MR 2, Meningococcal ‘A’, Vitamin A | Subcutaneous, intramuscular, Oral |
| 24 months | RTS,S 4 | Intramuscular |
Source: GHS, 2019
Bolds indicate changes that have occurred in the EPI schedule of MVIP selected areas in Ghana as a result of the introduction of RTS,S
Table 12.
Frequency distribution of responses
| Characteristic | Frequency | Percentage (%) |
|---|---|---|
| Sub-Municipality of residence (n = 424) | ||
| Abesim | 68 | 16.0 |
| Antwikrom | 45 | 10.6 |
| Newtown/Baakoniaba | 78 | 18.4 |
| New Dormaa | 102 | 24.1 |
| Sunyani central | 66 | 15.6 |
| Penkwase | 65 | 15.3 |
| Age (years; n = 424) | ||
| 15–19 | 11 | 2.6 |
| 20–24 | 46 | 10.9 |
| 25–29 | 171 | 40.3 |
| 30–34 | 151 | 35.6 |
| 35 and above | 45 | 10.6 |
| Parent or caregiver (n = 424) | ||
| Parent | 421 | 99.3 |
| Caregiver | 3 | 0.7 |
| Sex (n = 424) | ||
| Male | 2 | 0.5 |
| Female | 422 | 99.5 |
| Marital status (n = 424) | ||
| Single | 99 | 23.4 |
| Married | 258 | 60.9 |
| Cohabiting | 67 | 15.8 |
| Number of children alive (n = 424) | ||
| 1–3 | 378 | 89.2 |
| More than 3 | 46 | 10.8 |
| Educational status (n = 424) | ||
| No formal education | 28 | 6.6 |
| Primary education | 141 | 33.3 |
| Secondary education | 183 | 43.2 |
| Tertiary education | 72 | 17.0 |
| Educational status of partner (n = 424) | ||
| No formal education | 14 | 3.3 |
| Primary education | 72 | 17.1 |
| Secondary education | 161 | 38.2 |
| Tertiary education | 175 | 41.5 |
| Religion (n = 424) | ||
| Christianity | 318 | 75.0 |
| Islam | 103 | 24.3 |
| Traditionalist | 3 | 0.7 |
| Occupation (n = 424) | ||
| Unemployed | 87 | 20.5 |
| Self-employed | 234 | 55.2 |
| Farming | 32 | 7.6 |
| Civil servant | 71 | 16.8 |
| Religion of partner (n = 421) | ||
| Christianity | 317 | 75.3 |
| Islam | 100 | 23.8 |
| Traditionalist | 4 | 1 |
| Occupation of partner (n = 421) | ||
| Unemployed | 11 | 2.6 |
| Self-employed | 220 | 52.3 |
| Farming | 40 | 9.5 |
| Civil servant | 150 | 35.6 |
| Age of child in months (n = 424) | ||
| 13–14 | 79 | 18.6 |
| 15–16 | 281 | 66.3 |
| 17–18 | 64 | 15.1 |
| Sex (n = 424) | ||
| Male | 235 | 55.4 |
| Female | 189 | 44.6 |
| Place of delivery (n = 424) | ||
| Home | 21 | 5.0 |
| Health facility | 401 | 94.6 |
| Unknown | 2 | 0.4 |
| Level of uptake of RTS,S (n = 424) | ||
| No uptake | 25 | 5.9 |
| Partial uptake | 68 | 16.0 |
| Full uptake | 331 | 78.1 |
| RTS,S 1 uptake (n = 424) | ||
| Yes | 399 | 94.1 |
| No | 25 | 5.9 |
| RTS,S 2 uptake (n = 424) | ||
| Yes | 384 | 90.6 |
| No | 40 | 9.4 |
| RTS,S 3 uptake (n = 424) | ||
| Yes | 331 | 78.1 |
| No | 93 | 21.9 |
| Reason for child receiving some but not all doses of RTS,S (n = 68) | ||
| Did not know when next one was due | 31 | 45.6 |
| Did not take previous one on time | 4 | 5.9 |
| Not comfortable with side effects | 8 | 11.8 |
| Not comfortable with issues surrounding vaccine | 9 | 13.2 |
| Was not around | 16 | 23.5 |
| Reason for child receiving none of the doses of RTS,S (n = 25) | ||
| Personal decision to refuse vaccine | 7 | 28.0 |
| Partner’s (husband) decision to refuse vaccine | 15 | 60.0 |
| Did not know child is eligible | 3 | 12 |
| Known vaccine-preventable diseases (n = 424) | ||
| No correct disease mentioned | 41 | 9.7 |
| Up to 3 correct diseases mentioned | 215 | 50.7 |
| 4–8 correct diseases mentioned | 45 | 10.6 |
| Any correct disease mentioned but including malaria | 123 | 29.0 |
| Heard about malaria vaccine (n = 424) | ||
| Yes | 369 | 87.0 |
| No | 55 | 13.0 |
| Where first heard about malaria vaccine (n = 369) | ||
| CWC | 322 | 87.3 |
| Health facility announcement | 28 | 7.6 |
| Radio | 16 | 4.3 |
| Friend/relative | 3 | 0.8 |
| Number of times a child is supposed to receive the malaria vaccine (n = 369) | ||
| Correct number | 73 | 18.8 |
| Incorrect number | 296 | 80.2 |
| Age order of receiving vaccines (n = 369) | ||
| Correct order | 35 | 9.5 |
| Incorrect order | 334 | 90.5 |
| Heard about any negative report or issue concerning the malaria vaccine (n = 369) | ||
| Yes | 225 | 61.0 |
| No | 144 | 39.0 |
| Where negative issue or report was heard (n = 225) | ||
| Radio | 41 | 18.2 |
| Friends/relatives | 168 | 74.7 |
| Health workers | 13 | 5.8 |
| Other | 3 | 1.3 |
| Negative issue/report heard (n = 225) | ||
| Vaccine is not safe | 77 | 34.2 |
| Children are being used for experiment | 140 | 62.2 |
| Vaccine will affect children’s development | 8 | 3.6 |
| Issue/report prevented or delayed vaccine acceptance (n = 225) | ||
| Yes | 46 | 20.4 |
| No | 179 | 79.6 |
| Given the option of accepting malaria vaccine at CWC (n = 369) | ||
| Yes | 247 | 66.9 |
| No | 122 | 33.1 |
| Vaccines becoming many for children with the introduction of the malaria vaccine (n = 424) | ||
| Yes | 137 | 32.3 |
| No | 287 | 67.7 |
| Recommend malaria vaccine to others | ||
| Yes | 357 | 84.2 |
| No | 67 | 15.8 |
| Reason for recommending vaccine (n = 357) | ||
| It is safe | 145 | 40.6 |
| It protects children against malaria | 212 | 59.4 |
| Reason for not recommending vaccine (n = 67) | ||
| Vaccine does not make any difference | 1 | 1.5 |
| No specific reason | 35 | 52.2 |
| Too many issues surrounding vaccine | 2 | 3.0 |
| Do not have much information on the vaccine | 7 | 10.5 |
| It is not safe | 22 | 32.8 |
| Child ever suffered an adverse reaction following the administration (n = 424) | ||
| Yes | 223 | 52.6 |
| No | 201 | 47.4 |
| Reaction child suffered (n = 223) | ||
| Fever | 148 | 66.4 |
| Diarrhoea/vomiting | 11 | 4.9 |
| Abscess | 64 | 28.7 |
| Did reaction influence acceptance of other vaccines (n = 223) | ||
| Yes | 12 | 94.6 |
| No | 211 | 5.4 |
| Time taken to reach vaccination centre (n = 424) | ||
| Less than 30 min | 285 | 67.2 |
| 30–59 min | 132 | 31.1 |
| 1–2 h | 7 | 1.7 |
| Means of getting to vaccination centre (n = 424) | ||
| Walking | 288 | 67.9 |
| Commercial vehicle | 131 | 30.9 |
| Personal vehicle | 5 | 1.2 |
| Required to pay any money at vaccination centre (n = 424) | ||
| Yes | 50 | 11.8 |
| No | 374 | 88.2 |
| How to tell when child’s vaccination is due (n = 424) | ||
| Ask friends | 12 | 2.8 |
| Check child’s CWC card | 218 | 51.4 |
| Visit clinic monthly | 158 | 37.3 |
| Told by nurses | 36 | 8.5 |
| Description of CWC nurses’ attitude (n = 424) | ||
| Excellent | 54 | 12.7 |
| Very good | 191 | 45.1 |
| Good | 175 | 41.3 |
| Bad | 4 | 0.9 |
| Vaccines have long term side effects (n = 424) | ||
| Yes | 17 | 4.0 |
| No | 407 | 96.0 |
Authors’ contributions
DT and PAN made substantial contributions to the conception, design, acquisition of data, interpretation of data, drafting the manuscript and the critical review of the draft article. JCRPO made substantial contribution to the analysis of the study. All authors read and approved the final manuscript.
Funding
The study was Funded by the World Health Organization’s special programme for Research and Training in Tropical Diseases (WHO/TDR), under the WHO/TDR scholarship of the University of Ghana. The funding body played no role in the design of the study, collection, analysis, interpretation of data, and in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Ghana Health Service Ethics Review Committee with approval number GHS-ERC029/12/19. All participants consented to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. World malaria report 2018. Geneva, World Health Organization, 2018. www.who.int/malaria. Accessed 23 Sep 2019.
- 2.District Health Information System. Malaria. 2019. https://dhims.chimgh.org/dhims/dhis-web-pivot/index.html. Accessed 3 Sep 2019.
- 3.WHO. Malaria. Geneva, World Health Organization, 2019. https://www.who.int/news-room/fact-sheets/detail/malaria. Accessed 12 Nov 2019.
- 4.Program for Appropriate Technology in Health . The RTS,S malaria vaccine. Seattle: PATH; 2019. [Google Scholar]
- 5.Ghana Health Service. Ghana starts malaria vaccine implementation. 2019. http://www.ghana.gov.gh/index.php/media-center/news/5513-ghana-starts-malaria-vaccine-implementation. Accessed 20 Oct 2019.
- 6.Myjoyonline. Antimalaria vaccine: children not being used as guinea pigs. 2019. https://www.myjoyonline.com/lifestyle/2019/may-16th/antimalaria-vaccine-children-not-being-used-as-guinea-pigs-ghana-health-service.php. Accessed 20 Oct 2019.
- 7.WHO. Ten years in public health, 2007–2017: report by Dr. Margaret Chan, Director-General. Geneva, World Health Organization. 2017; p. 81–3. www.who.int/malaria. 7 Nov 2019.
- 8.Yawson AE, Bonsu G, Senaya LK, Yawson AO, Eleeza JB, Awoonor-Williams JK, et al. Regional disparities in immunization services in Ghana through a bottleneck analysis approach: implications for sustaining national gains in immunization. Arch Public Health. 2017;75:10. doi: 10.1186/s13690-017-0179-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sunyani Municipal Health Directorate . Annual report, 2018. Sunyani: Sunyani Municipal Health Directorate; 2019. [Google Scholar]
- 10.WHO Global Vaccine Action Plan: decade of vaccine collaboration. Vaccine. 2013;31:5–31. doi: 10.1016/j.vaccine.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Abdou M, Mbengue S, Sarr M, Faye A, Badiane O, Bintou F, et al. Determinants of complete immunization among Senegalese children aged 12–23 months : evidence from the demographic and health survey. BMC Public Health. 2017;17:630. doi: 10.1186/s12889-017-4493-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Russo G, Miglietta A, Pezzotti P, Biguioh RM, Mayaka GB, Sobze MS, et al. Vaccine coverage and determinants of incomplete vaccination in children aged 12–23 months in Dschang, West Region, Cameroon : a cross-sectional survey during a polio outbreak. BMC Public Health. 2015;15:630. doi: 10.1186/s12889-015-2000-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adedire EB, Ajayi I, Fawole OI, Ajumobi O, Kasasa S, Wasswa P, et al. Immunisation coverage and its determinants among children aged 12–23 months in Atakumosa-west district, Osun State Nigeria: a cross-sectional study. BMC Public Health. 2016;16:905. doi: 10.1186/s12889-016-3531-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ekouevi DK, Gbeasor-komlanvi FA, Yaya I, Zida-compaore WI, Boko A, Sewu E, et al. Incomplete immunization among children aged 12–23 months in Togo: a multilevel analysis of individual and contextual factors. BMC Public Health. 2018;18:952. doi: 10.1186/s12889-018-5881-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Acharya P, Kismul H, Mapatano MA, Hatl A. Individual- and community-level determinants of child immunization in the Democratic Republic of Congo : a multilevel analysis. PLoS ONE. 2018;13:e0202742. doi: 10.1371/journal.pone.0202742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wemakor A, Helegbe GK, Abdul-mumin A, Amedoe S, Zoku JA, Dufie AI. Prevalence and factors associated with incomplete immunization of children (12–23 months) in Kwabre East District, Ashanti Region, Ghana. Arch Public Health. 2018;76:9. doi: 10.1186/s13690-018-0315-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adu GA. Determinants of complete vaccination among children 24–35 months in Ga East Municipality of Accra. University of Ghana; 2017. http://ugspace.ug.edu.gh. Accessed 18 Oct 2019.
- 18.Ofosu SK. Factors contributing to immunization coverage in Assin North Municipality. University of Ghana; 2017. http://ugspace.ug.edu.gh. Accessed 18 Oct 2019.
- 19.Mukthar VK, Kulei SJ, Chege M. Determinants of pneumococcal conjugate vaccine uptake among children attending immunisation services at Kenyatta national hospital, Nairobi. Kenya East Afr Med J. 2015;92:348–53. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding on reasonable request.


