Abstract
Recovery stepping in response to forward slips has the potential to not only rebuild the base of support to prevent backward falling, but also provide extra limb support to prevent downward falling. Hence, recovery stepping is often necessary for fall prevention following an unexpected slip. However, less is known about whether recovery foot placement could affect the likelihood of recovery following a slip. The purpose of this study was to determine whether there is an optimal recovery landing zone within which older adults have a higher likelihood of recovery. 195 participants experienced a novel, unannounced forward slip while walking on a 7-meter walkway. The center of mass (COM) stability (computed from its position and velocity), vertical limb support (computed from change in hip kinematics), and recovery limb joint moments (from joint kinematics and ground reaction force) in the sagittal plane were analyzed. The results showed that a longer distance between recovery foot landing position and the projected COM position at recovery foot touchdown (relative recovery step placement) was conducive to stability improvement but adverse to limb support enhancement, and vice versa for a shorter distance. Relative recovery step placement could predict the recovery likelihood with an accuracy of 67.3%, and the recovery rate was greater than 50% when the distance between recovery foot and COM is less than 0.3 × foot length. This study also found more posterior stepping could be attributed to insufficient ankle plantar flexor and hip flexor moments in the pre-swing phase, while more anterior stepping was induced by insufficient hip and knee extensor moments in the following swing phase.
Keywords: optimal landing zone, recovery step, stability, limb support, joint moment
Introduction:
A recovery (compensatory) step often used after experiencing a loss of balance.21, 22 Previous studies stated that one could successfully avert a fall by taking an effective recovery step,4, 42 as recovery stepping could not only restore stability by rebuilding the base of support (BOS), but could also provide extra limb support to retard hip descent, therefore decreasing fall risk and slip severity.35, 42 Increased fall rates were also linked to an inability to recover one’s balance by taking a recovery step.23 Previous studies found that a longer forward recovery step or a greater distance between the center of mass (COM) and the recovery foot could increase individuals’ ability to recover their balance upon experiencing a trip,12, 15, 31 however, it is unclear whether the same is true for backwards step3 to recover from a forward slip.
Both instability and limb collapse are known to account for forward slip-induced falls.36 Stability can be defined as the ability to maintain and regulate the projected COM within the limits of the BOS during both static and dynamic tasks.28 Previous theoretical work has led to computation of stability limits or margins which are postulated to be internal representations or boundaries within which the body COM state can be stable or resistant to change from perturbations without having to resort to changing the BOS. A COM state (its position and velocity) outside the stability limits is considered as unstable.20 Limb support is defined as the reactive vertical force generated from the stance limb in order to resist the downward falling of the pelvis during perturbation induced loss of balance30. Previous evidence has demonstrated a linear relationship between change in this reactive force [measured by vertical ground reaction force (GRF)] and change in hip kinematics. When the body is unable to generate sufficient vertical supporting force against the force of gravity (GRF < body weight), limb collapse ensues with associated downward movement of the pelvis, and can be easily measured by the change in hip kinematics.32 It has been previously demonstrated that both limb support and stability rapidly deteriorate following a slip,36, 42 and thus execution of the recovery step (taken by the trailing foot) becomes necessary to regain stability and enhance limb support. A longer recovery step is useful to maximize the vertical supporting force to reverse COM vertical descent, according to the bipedal inverted pendulum model.14, 25, 39 But, this longer recovery step would bring the recovery foot landing position closer behind the COM during locomotion, leading to a smaller BOS with worse stability against backward balance loss.4, 9 Conversely, a shorter recovery step would cause a longer distance between the recovery foot and the COM, which could generate a larger landing impulse in the anteroposterior (AP) direction,16 slowing the body’s backward rotation upon experiencing an unexpected perturbation.31 But, this longer distance between the recovery foot and the COM also lowers the vertical component of the ground reaction force during walking, resulting in decreased enhancement of limb support (Figure 1). Thus, there may be some tradeoff between enhancing limb support and regaining stability, as a longer distance between the recovery foot and the COM is conducive to improving stability but adverse to enhancing limb support, and vice versa for a shorter distance. Therefore, we speculated that an appropriate recovery step should be neither too long nor too short in order to limit both instability and limb collapse and, hence, improve the likelihood of recovery.
Figure 1.
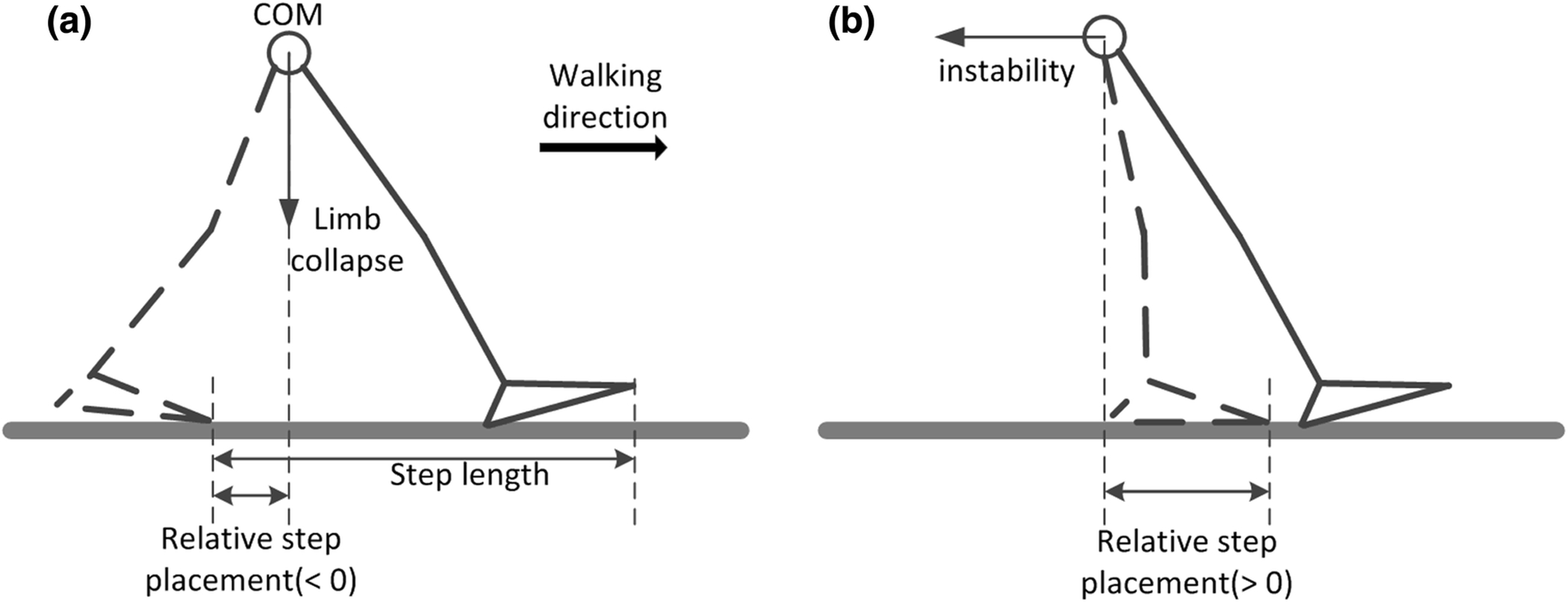
Schematic of typical recovery steps following a novel slip. a) When participants take a negative recovery step, they may experience limb collapse, b) when participants take a positive recovery step, they may experience instability.
Recovery stepping upon gait-slip perturbations reflects triggered responses initiated by the CNS to restore stability.4 Previous studies have postulated that the motor program for triggering the recovery step might be modulated by the central pattern generator, as recovery step length is often scaled to one’s overall step length during gait. 9, 17 Moreover, excessive hip descent prior to recovery stepping could restrict recovery step length,32 and a lower stability at recovery step liftoff could also shorten recovery step length.18 However, it remains to be examined if recovery step placement to large-scale unannounced slips can be modulated by kinematic and kinetic factors.
The purpose of this study was to first chart a recovery rate curve (which plots the recovery rate for different recovery step placements relative to the COM) for gait-slips and then subsequently investigate and determine the optimal recovery zone in the AP plane, in which the landing of the recovery step would lead to the greatest chance of recovery, demonstrated by a significant improvement in both COM stability and limb support. We postulated that the post-slip changes in stability and limb support would be correlated with the relative recovery step placement (recovery step landing position relative to the COM) but with opposing slopes. Specifically, stability would improve with shorter recovery step due to the larger BOS. Limb support, however, would improve with longer recovery step due to the larger supporting force reversing vertical descent of the COM. Further we hypothesized that there would be an optimal landing zone for the recovery step which should neither be too posterior nor too anterior to the COM, but instead at a certain proximity to the COM where recovery rates would be the greatest. In this case, individuals who stepped inside this zone would not only regain their stability, but would also enhance their limb support, leading to the highest recovery likelihood. Further, this study attempted to investigate the motor program (in terms of joint moments) that affects recovery step placement. Knowledge of the specific joint moments that modulate step landing could assist in designing intervention strategies for optimal recovery foot landing upon experiencing a novel slip.
Method:
Subjects
195 community-dwelling older adults (≥ 65 years) participated in this study (age: 72.3 ± 5.3 years; height: 165.5 ± 8.8 cm; mass: 75.5 ± 14.1 kg). Included participants were part of a previously conducted study and only the first novel slip trial data was included for the purpose of this study.29, 35 Out of 195 subjects, 19 were excluded from the analysis as they stepped out of the force plate zone and therefore the calculated joint moments in these trials would be inaccurate. All included participants were prescreened via a questionnaire to exclude those with neurological, musculoskeletal, cardiopulmonary, or any other systemic disorders. All participants provided written informed consent, approved by the Institutional Review Board in the University of Illinois at Chicago.
Experimental setup
The slip was induced by releasing a pair of side-by-side, low-friction movable platforms embedded near the middle of a 7-meter walkway. The platforms were firmly locked in place for the first ten walking trials. During the slip trial, the platforms (friction coefficient < 0.05) could slide freely in the AP direction for up to 90 cm forward or 58 cm backward. Once a subject’s right (slipping) foot was detected in contact with the right platform, 29 a computer controlled triggering mechanism would release the right platform. Then, the left platform was automatically released after the left (recovery) foot landed on it. Subjects were told that a slip may or may not happen during any of the trials. Only the first slip trial for each subject was analyzed.
The subjects wore their own athletic shoes and a full-body safety harness which was connected by shock-absorbing ropes to a loadcell (Transcell Technology Inc., Buffalo Grove, IL). The loadcell was mounted on an overhead trolley on a track over the walkway. Four force plates (AMTI, Newton, MA) were installed beneath the walkway to record the ground reaction force. The harness enabled subjects to walk freely while providing protection against body impact with the floor. Kinematics for a full body marker set (28 retro-reflective markers) were recorded by an eight-camera motion capture system (Motion Analysis Corporation, Santa Rosa, CA). Marker co-ordinates were low-pass filtered using a fourth-order Butterworth filter, the optimal cutoff frequency for each marker (ranging from 4.5 to 9 Hz) was determined based on equation developed by Yu et al.42, 45 Kinematic data were sampled at 120 Hz and synchronized with the force plate and loadcell data, which were collected at 600 Hz.
Outcome variables
Relative recovery step placement:
As the initial contact area of the recovery foot was always around the toe (head of the 1st metatarsal) in this study, the relative recovery step placement was calculated by subtracting the COM position from the toe position of the recovery foot in the AP direction at the instant of recovery foot touchdown (LTD, always left and the trailing one). The COM was calculated using a 13-segment rigid body model with gender-dependent segmental inertial parameters.7 Step length was determined to be the distance between the toe of the slipping foot (always right and the leading one) and that of the recovery foot at LTD (Figure 1).
Stability:
The COM position and its velocity relative to the BOS were computed to assess a person’s instantaneous dynamic stability.27 First, the relative position and velocity of the COM were calculated using the motion state (position and velocity) of the rear edge of the BOS (the right heel) as a reference. Then, relative COM position was normalized by foot length (FL) and relative velocity was normalized by the quantity , where g is the gravitational acceleration and BH is body height. Finally, the COM stability was computed as the shortest distance from the COM state (position and velocity) to the computational limits of stability under slip conditions and during walking in the AP directions.40 These limits which have been derived theoretically (via human model simulations) have since been validated empirically to accurately predict risk of backward and forward falling.41, 43
Limb Support:
The vertical hip velocity normalized by body height was used to represent limb support.42 Hip velocity was obtained by taking the derivative of the midpoint of the left and right hip joint centers. This measure has been previously demonstrated to correlate with the vertical ground reaction force and a change in vertical COM.42 For example, a reduced limb support value indicates an insufficient vertical ground reaction force against the gravity of human body and a vertical downward (towards the ground) acceleration of the COM.
Joint moments:
The joint position data collected via 3D motion analysis and the ground reaction force were used to compute the joint moments of the recovery limb. Joint moment was calculated using subject-specific musculoskeletal sagittal-plane models (7-link, 9-degree-of-freedom) in OpenSim version 3.38 with inverse-dynamics formulation.41 The individual models were scaled according to each subject’s anthropometric measurements.10 As the joint moments applied on the recovery foot could directly affect its acceleration, hence the acceleration of the recovery foot (ankle marker) in AP and vertical directions were also calculated.
The events of step time used in this study, including slip foot touchdown (RTD), recovery foot liftoff (LLO), and LTD, were detected from force plate data (vertical force decent below 10N).11 The whole recovery stepping period could be divided into a pre-swing phase (RTD to LLO) and a swing phase (LLO to LTD). In the pre-swing phase, the push off force reaches its peak at around 100ms prior to LLO (pre-LLO), hence this instant was chosen was analysis in this phase.37 While in the swing phase, the instant when the foot (ankle marker) reached its maximum height was defined as pre-descent. After this instant, as seen in normal gait participants start lowering their limb to prepare for the next step touchdown by increasing the hip extensor moment.34, 38 However, upon slip the lowering strategy could be different based on reaction initiation post-perturbation.24 Hence the variables of interest (joint moments and foot accelerations) were analyzed at the pre-descent instant of the swing phase.
Relationship between recovery rate and landing position
A fall was identified if the peak loadcell force during a slip exceeded 30% of the participant’s body weight,44 otherwise the trial was a recovery. As recovery step placement ranged from −2 to 2 × FL in AP direction,35 40 subranges with the same width (0.5 × FL) were selected in this zone, with the distance between adjacent subranges being 0.1 × FL (i.e. subrange 1 is from −2.25 to −1.75, subrange 2 is from −2.15 to −1.65, subrange 3 is from −2.05 to −1.55, etc.). Within each subrange, the recovery rate was calculated by dividing the recovery trial number by the total trial numbers in this subrange. To guarantee both sensitivity and accuracy, the width of 0.5 × FL was used for each subrange in this study. However, the recovery rate curves were highly consistent with different subrange widths (0.2, 0.4, 0.6, and 0.8 × FL), and these curves are shown in the Appendix.
If there is an optimal recovery zone as we expected, the whole landing zone could be divided into three parts based on the recovery rate. These smaller zones are the optimal landing zone (OPT, recovery rate > 50%), the backward landing zone posterior to the OPT (BWD, recovery rate < 50%), and the forward landing zone anterior to the OPT (FWD, recovery rate < 50%).
In addition, the relationship between recovery rate and landing placement in ML direction was also analyzed. Similarly, the landing placement was normalized by foot width (FW), and 40 subranges with the same width (0.5 × FW) were selected with the distance between adjacent subranges being 0.1 × FW. The recovery rate was calculated for each subrange.
Statistical analysis
In order to examine the effect of recovery step on stability and limb support, correlation analyses were conducted between the relative recovery step placement and both the change in stability and change in limb support from pre-LTD (LTD − 10ms, when the recovery foot has no contact with the ground) to post-LTD (LTD + 150ms, when the recovery foot fully comes into contact with the ground). The relationship between stability and limb support at pre-LTD was also analyzed to verify whether instability was correlated with limb collapse.
To determine the optimal landing zone, logistic regression was firstly used to verify whether relative recovery step placement (the absolute value, Table 1) could affect slip outcome (fall or not), and whether relative recovery step placement would have a higher predictive capacity compared to recovery step length, which was also proposed as a fall risk predictor.15 Next, backward stepwise logistic regression was conducted for fall prediction based on these variables along with the stability and limb support variables at LTD. Further, the relationship between recovery rate and recovery foot placement was analyzed based on the recovery rate curves mentioned above.
Table 1.
Predictive validity of relative recovery step placement and step length using logistic regression. FL denotes foot length, FW denotes foot width.
| Model | Independent variable(s) | Accuracy | B value | P value |
|---|---|---|---|---|
| 1 | | (Toe − COM) / FL | in AP* | 67.3% | 2.30 | <0.001 |
| 2 | Step length | 53.2% | −0.18 | 0.304 |
| 3 | | (Toe − COM) / FL | in AP | 70.5% | 2.95 | <0.001 |
| Hip vertical velocity at LTD | −8.55 | <0.001 | ||
| 4 | | (Toe − COM) / FW | in ML | 56.6% | 0.71 | 0.112 |
denoting absolute value
Stepwise multi-linear regression was used to confirm whether or not the recovery step placement could be modulated by the joint moments of the recovery limb at pre-LLO and pre-descent. If it could, then one-way ANOVA was conducted to compare the differences in joint moments among the three stepping zones (BWD, OPT, and FWD) for pre-LLO and pre-descent. This was subsequently followed-up with independent t-tests with Bonferroni corrections applied. Similarly, one-way ANOVA and post hoc analyses were used to compare the recovery foot (ankle) acceleration in the AP and vertical directions among the three zones for pre-LLO and pre-descent. In addition, backward stepwise logistic regression was used to further verify whether or not the recovery step zone could be predicted based on these joint moments. All statistical analyses were performed using SPSS 22 (IBM Corp, Armonk, NY). For multiple comparisons, an adjusted significance level at α = 0.02 was used to avoid type two errors. All other statistical analyses had a significance level of α = 0.05.
Results:
Relationship between recovery rate and recovery foot placement
A significant negative relationship was detected between relative recovery foot placement [(Toe - COM) / FL] and stability (r = −0.78, p < 0.001. Fig. 2). Conversely, recovery step placement was positively correlated with limb support (r = 0.47, p < 0.001). Additionally, limb support was positively correlated with stability at pre-LTD (r = 0.72, p < 0.001).
Figure 2.
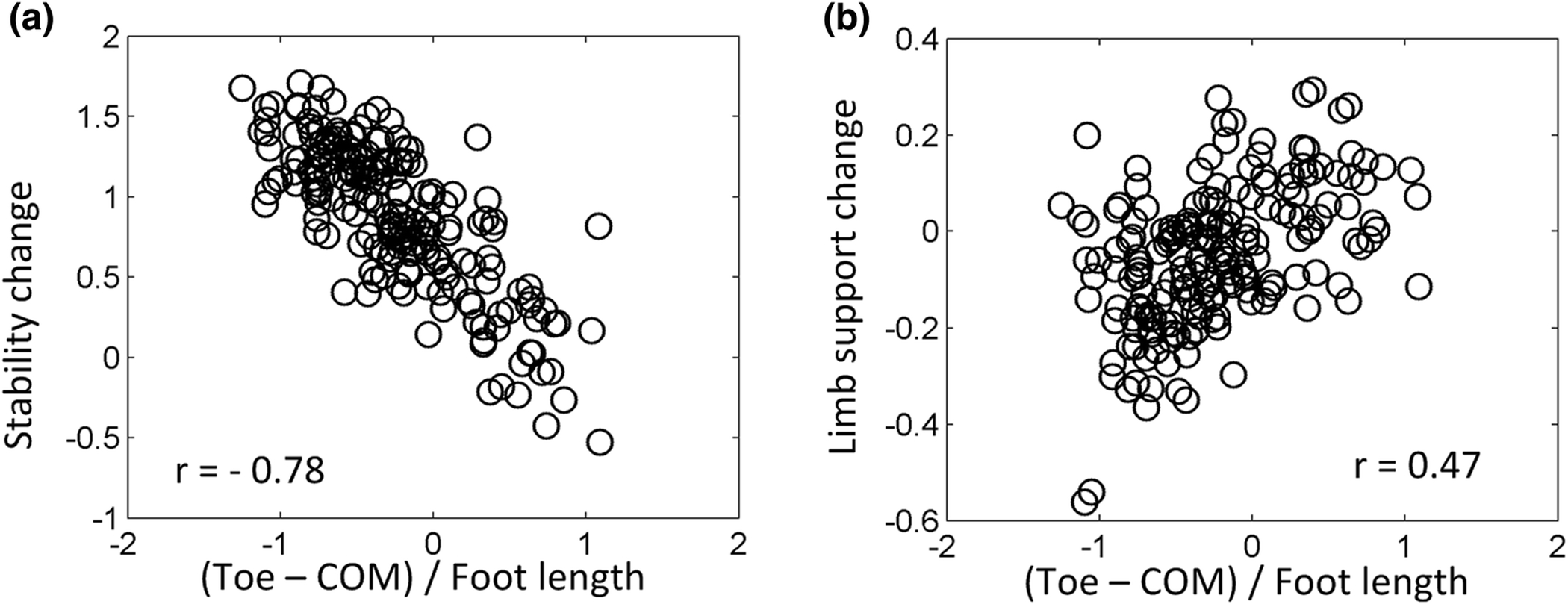
a) Relationship between relative recovery step placement (with reference to the COM) and the change of stability from pre-LTD (LTD − 10ms) to post-LTD (LTD + 150ms), b) relationship between relative recovery step placement and the change of limb support from pre-LTD to post-LTD.
Recovery step length did not contribute to fall prediction (p > 0.05. Table 1), but relative recovery step placement was a key determinant for fall prediction (accuracy = 67.3%, p < 0.001). After combining this variable with hip vertical velocity at LTD, the predictive accuracy could be improved by 3.2%.
The recovery rate was calculated for each subrange from −2 to 2. The recovery rate was as high as 60% when the recovery foot landed close to the COM (Fig. 4), and it dropped all the way to 0% when the recovery landing position was too anterior or posterior to the COM (distance between the toe and COM > FL). According to the distribution of recovery rates, there was an optimal recovery step zone (between −0.3 and 0.3 × FL, trial number = 60), also there was a backward (< −0.3 × FL, trial number = 86) and forward step zones (> 0.3 × FL, trial number = 30). Inconsistent with the recovery step placement in AP direction, there was no optimal recovery step zone in ML direction, and it was found that recovery step placement in ML direction did not contribute to fall prediction (p > 0.05. Table 1).
Figure 4.
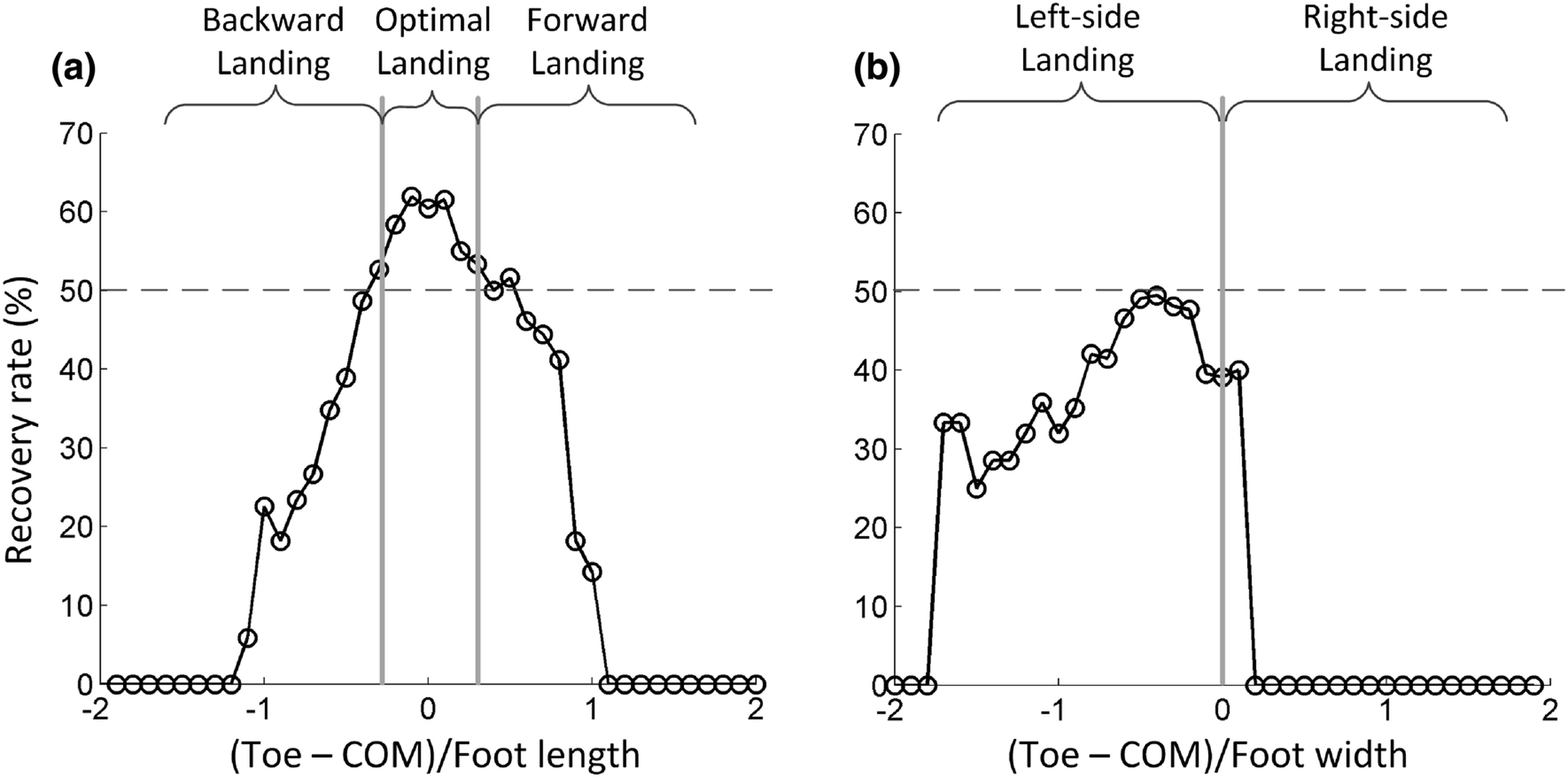
a) Recovery rate at each foot landing subrange in AP direction from −2 to 2 × FL (foot length), the step size between the subranges is 0.1× FL. Based on this recovery rate, the whole foot landing zone could be divided into three groups: backward landing (N = 86); optimal landing (N = 60); and forward landing (N = 30). b) Recovery rate at each foot landing subrange in ML direction from −2 to 2 × FW (foot width), the step size between the subranges is 0.1 × FW.
Relationship between recovery foot placement and joint moments
According to multiple linear regression, recovery step placement was determined by only four variables (ankle and hip moments at pre-LLO and knee and hip moments at pre-descent) (r = 0.65, p < 0.01 for all variables. Table 2). Consistently, one-way ANOVA demonstrated that only ankle moment [F (3, 142) = 8.44, p < 0.001. Fig. 5], and hip moment [F (3, 142) = 5.82, p = 0.004] at pre-LLO were significantly affected by step zone (BWD, OPT, and FWD). At pre-descent, a significant effect of step zone was found for knee moment [F (3, 142) = 7.18, p = 0.001] and hip moment [F (3, 142) = 6.24, p = 0.002], but not for ankle moment (p > 0.05).
Table 2.
Stepwise linear multi-regression model on recovery step landing location. Pre-LLO is LLO-100ms, and pre-descent denotes the instant when the recovery foot starts descending towards the ground.
| Independent variables | B value | P value | r value |
|---|---|---|---|
| Hip moment at pre-LLO | 2.86 | <0.001 | 0.65 |
| Ankle moment at pre-LLO | 2.73 | 0.009 | |
| Hip moment at pre-descent | −20.79 | 0.003 | |
| Knee moment at pre-descent | −8.42 | <0.001 |
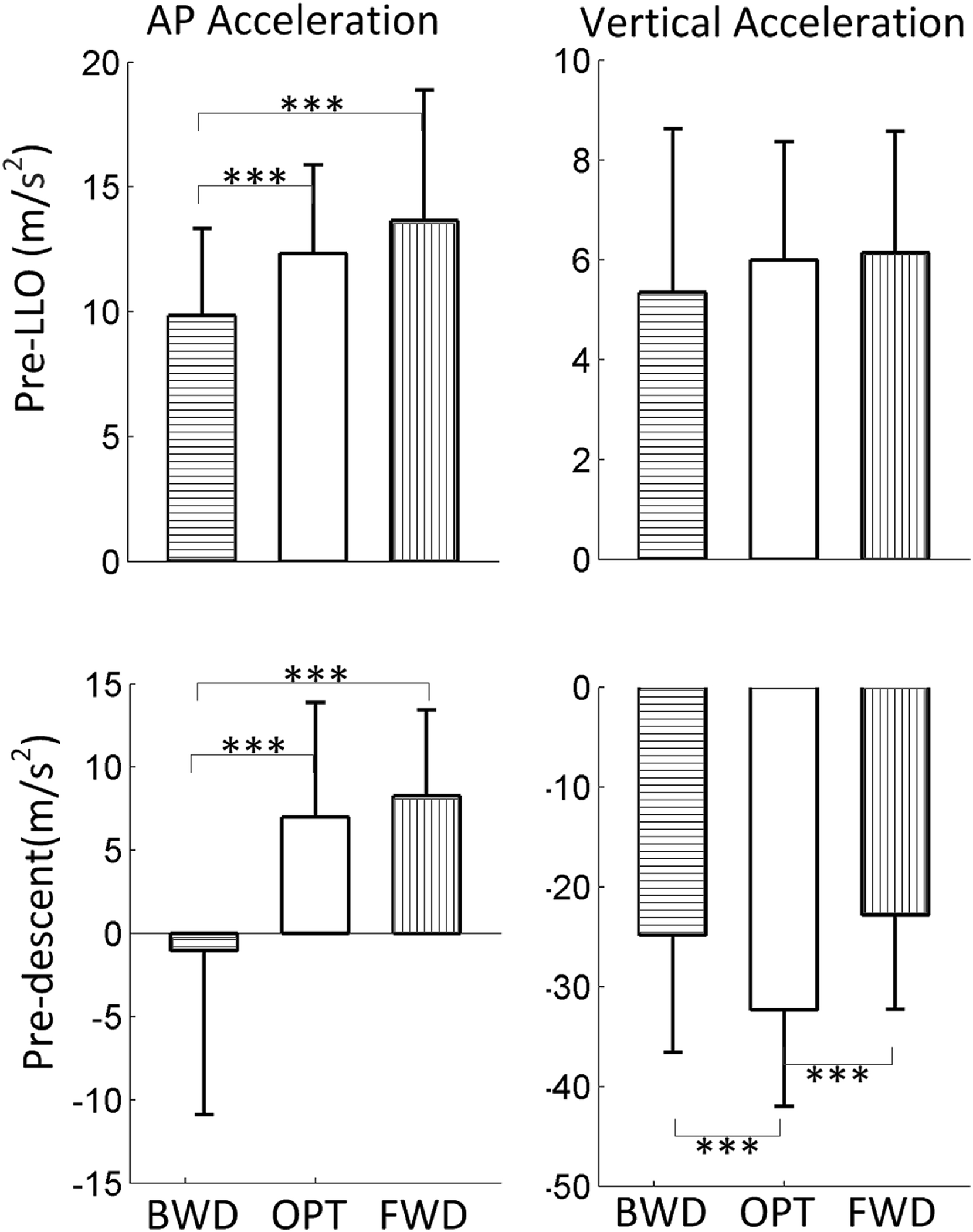
Figure 5.
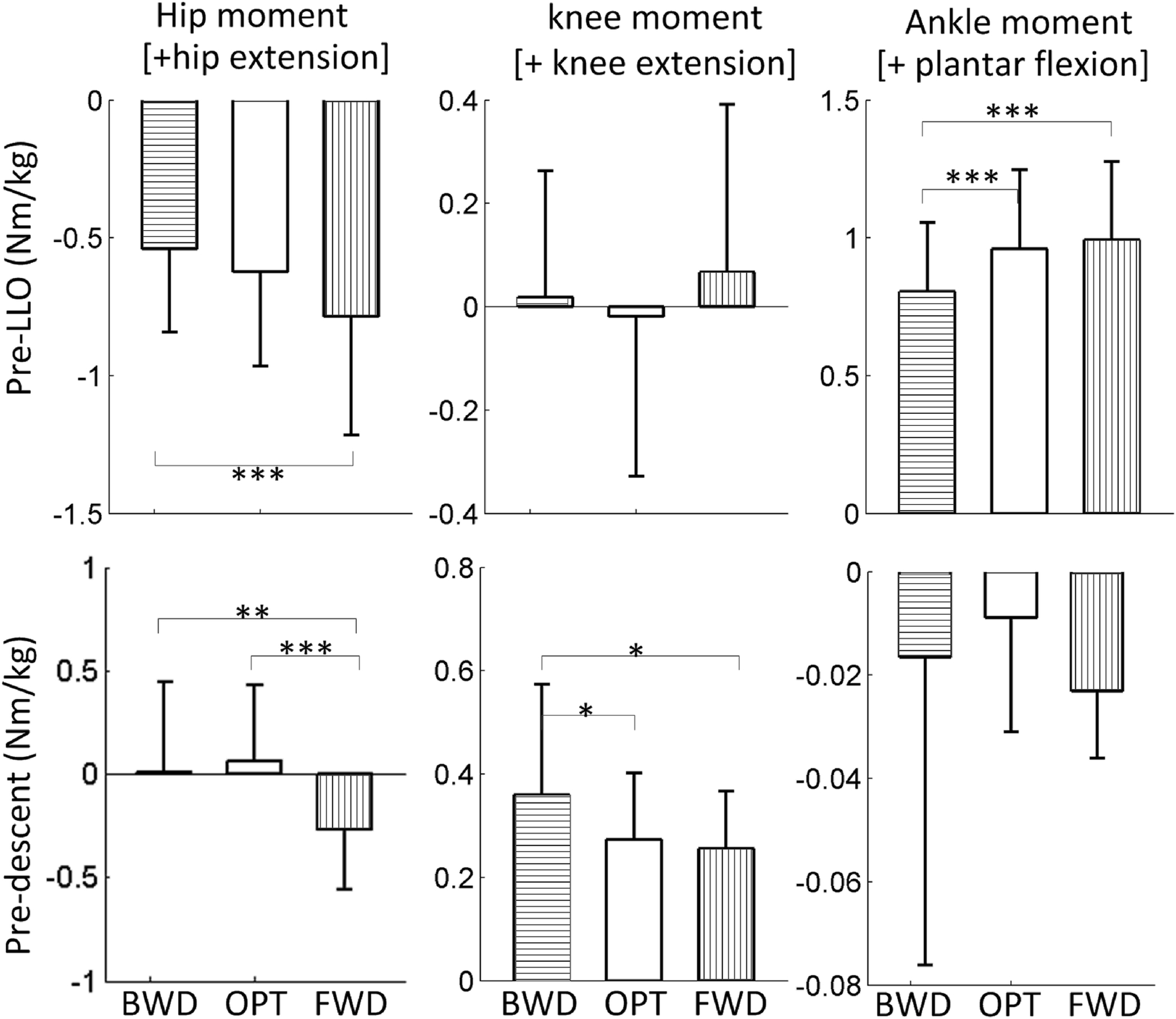
Joint moment comparisons across three groups (BWD, OPT, and FWD) at pre-LLO (LLO − 100ms) and pre-descent instants.
Post hoc analysis indicated that ankle moment at pre-LLO in the BWD was significantly smaller than in the OPT and FWD (p < 0.001 for both. Fig. 5), while hip moment at pre-LLO in the OPT was significantly smaller than in the FWD (p < 0.001). However, no differences in knee moments were found at pre-LLO among these groups (p > 0.05 for all). At pre-descent, hip moment in the FWD was significantly smaller than in the OPT and BWD (p < 0.001 for both. Fig. 5), while knee moment in the BWD was significantly larger than in the OPT and FWD (p < 0.05 for both). However, there were no significant differences in ankle moment among these groups (p > 0.05 for all). Among all of the joint moments at pre-LLO and pre-descent, ankle moment (p < 0.001. Table. 3) and hip moment (p = 0.002) at pre-LLO could predict whether the recovery foot would land in the BWD with an accuracy of 67.6%, hip moment (p < 0.001) and knee moment (p < 0.001) at pre-descent could predict whether the recovery foot would land in the FWD with an accuracy of 86.3%, and the ankle moment (p = 0.02) at pre-LLO and hip moment (p = 0.05) at pre-descent could predict whether the relative recovery step placement would be in the OPT with an accuracy of 65.9%.
Table 3.
Backward stepwise logistic regression for recovery step placement prediction using joint (ankle, knee and hip) moments at pre-LLO and pre-descent. BWD denotes backward landing zone; FWD denotes forward landing zone; OPT denotes optimal landing zone; pre-LLO is LLO-100ms; and pre-descent denotes the instant when the recovery foot starts descending towards the ground.
| Model | Independent variables | Accuracy | B value | P value |
|---|---|---|---|---|
| Whether in BWD | Ankle moment at pre-LLO | 67.6% | −2.67 | <0.001 |
| Hip moment at pre-LLO | 1.54 | 0.002 | ||
| Whether in FWD | Hip moment at pre-descent | 86.3% | −6.04 | <0.001 |
| Knee moment at pre-descent | −12.09 | <0.001 | ||
| Whether in OPT | Ankle moment at pre-LLO | 65.9% | 1.37 | 0.02 |
| Hip moment at pre-descent | 0.79 | 0.05 |
Relationship between recovery foot placement and foot accelerations
Foot accelerations in the AP [at pre-LLO: F (3, 142) = 13.81, p < 0.001; at pre-descent: F (3, 142) = 23.03, p < 0.001. Fig. 6] and vertical directions [at pre-LLO: p > 0.05; at MR: F (3, 142) = 11.48, p < 0.001] were also affected by step zone. At pre-LLO, the foot acceleration in the AP direction in the BWD was significantly smaller than that in the OPT (p < 0.001. Fig. 6) and FWD (p < 0.001). While at pre-descent, the AP acceleration was significantly smaller in the BWD (BWD vs. OPT: p < 0.001; BWD vs. FWD: p < 0.001) and the vertical acceleration was significantly smaller in the OPT (OPT vs. BWD: p < 0.001; OPT vs. FWD: p < 0.001) compared to in the other zones.
Figure 6.
Acceleration (in AP or vertical direction) comparisons across three groups (BWD, OPT, and FWD) at pre-LLO (LLO − 100ms) and pre-descent instants.
Discussion:
As postulated, recovery foot placement could not only impact individuals’ ability to regain stability but it could also impact limb support. A more posterior recovery foot placement (relative to the COM) at LTD could improve stability but weaken limb support, while a more anterior recovery foot placement could enhance limb support but lead to a shorter BOS with worse stability against backward loss of balance (Fig. 2). Hence, the optimal recovery step placement should be neither too posterior nor too anterior relative to the COM, but should be right around the COM (from − 0.3 to 0.3 × FL. Fig. 4). As shown in Figure 2, both instability and limb collapse could be reversed for individuals who stepped in this optimal recovery step placement zone. Subjects whose recovery foot landed in this zone had a higher recovery rate (> 50%), which was consistent with our hypothesis. Additionally, slip outcomes could be predicted with a certainty of 67.3% based on recovery foot placement only, while this prediction strength was even higher (70.5%, Table. 1) when combined with limb support at LTD, indicating that an appropriate foot landing position together with sufficient limb support could greatly decrease the likelihood of fall following a slip.
Unlike recovery from a trip,31 the outcome (fall or not) of a slip during locomotion was not affected by recovery step length but was instead affected by the relative recovery step placement, which might be due to differences in mechanisms between slip and trip perturbations. Unlike for a slip, the velocity of the BOS following a trip is always around zero due to the higher friction coefficient, and hence, the larger horizontal ground reaction force on the recovery foot as a result of the longer step length,6, 15 which could retard the body’s forward rotation after recovery touchdown.13 For a slip, however, although the larger horizontal (propulsive) force due to the shorter step length could rebuild a larger BOS and increase COM velocity, hence improve stability, this force might also accelerate the slipping foot due to its lower friction coefficient, leading to a higher perturbation intensity.3
Besides affecting slip intensity, a more posterior recovery landing position would increase the distance between the slipping foot and the recovery foot, thus the vertical support force would decrease according to the bipedal inverted pendulum model, resulting in a split fall.35 Conversely, a more anterior landing could provide a larger vertical support force, which could prevent limb collapse by providing sufficient support (Fig. 2b). However, there might not be enough propulsive force with a more anterior landing to prevent the COM from moving out of the backward boundary of the BOS, and, hence, this shorter distance between the COM and the backward boundary could worsen stability (Fig. 2a), especially when the recovery foot lands more than one foot length anterior to the COM (increment is ~0). Therefore, because recovery step placement is so important for recovery from a slip, the modulation of this stepping response is crucial for improving recovery outcomes, and this could potentially be done through the modulation of specific joint moments.
Besides the recovery step placement in AP direction, the lateral landing placement was also analyzed in this study. Conversely, it was found that the recovery step placement in ML direction could not affect the risk of fall. This could be because the slip perturbation in this study was always in AP direction, and our previous study have assessed on the cause of falls, and reported that only 8% of slip-related laboratory falls36 could be attributed to ML instability, and other falls were induced by either AP instability and/or limb collapse. Similarly, only about 12% of slip-related real-life falls were found to be correlated with lateral instability.19 Correspondingly, the recovery step placement in ML direction was not a key factor affecting the fall risk. These findings indicate that ML stability might play a minimal role for predominantly AP perturbations such as real-life slips.
It is quite likely that during a novel, unannounced slip, recovery landing (reactive posture adjustment) is not simply due to local reflexes but rather an activation of a motor pattern to prevent a fall, and the recruitment of muscle synergies corresponding to this specific motor pattern can be modulated to change the motor behavior.5 Our results indicate that recovery step placement could be affected by adjustments of corresponding joint moments at pre-LLO (proactive) and pre-descent (reactive) instants (Table. 2). More posterior stepping resulted from insufficient plantar flexor and hip flexor moments at pre-LLO (Table. 3 and Fig. 5), as plantar flexor and hip flexor moments in the pre-swing phase initiate the swing and increase the energy level of the recovery leg, which could accelerate the leg segments through the pre-swing phase.26 Thus, insufficient plantar flexor and hip flexor moments in this phase would result in a smaller foot acceleration in the AP direction (Fig. 6), leading to more posterior stepping. More anterior stepping, however, was induced by insufficient hip extensor and knee extensor moments at pre-descent, which contributed to foot touching the ground (Fig. 6). A greater foot acceleration during its descent to the ground could shorten the duration from pre-descent to its touchdown to avoid a more anterior stepping. Together, the plantar flexor moment in the pre-swing phase and the hip extensor moment in the swing phase were the key determinants affecting whether the recovery foot would land in the optimal zone (Table. 3). These joint moment adjustments could be attributable to modulation of specific movement patterns. Therefore, it might be possible for individuals to improve their reactive actions by modulating their movement patterns.
There are many other factors that might affect the recovery foot placement. Previous studies have demonstrated that recovery step length is often scaled to one’s step length during regular walking. 9, 17 However, the gait kinematic factors could be perceived as the “downstream” factors, which were determined by corresponding preceding lower limb joint moments.1, 33 Hence, this study mainly focused on the kinetic factors.
One limitation of this study was that all the slips were delivered to the right leg and if leg dominance affects recovery responses, the results could be different. However, leg dominance has not shown to impact recovery responses.2 Further, only the joint moments of the compensatory limb were compared in this study, and it is possible that the joint moments of the slipping limb might also affect the recovery step placement. Therefore, future studies could investigate contribution of slipping limb kinetics on recovery step placement, although it is expected to be small.
The present study findings could have clinical applications for fall prevention. Knowledge of the optimal landing zone could help clinicians specifically design interventions during volitional step training or reactive step training to target optimal relative recovery foot placement. It was postulated that individuals’ fall types were determined by the recovery step placement.35 For example a shorter recovery step (backward landing zone) would lead to a split fall, while a longer recovery step (forward landing zone) would lead to a feet-forward fall. Hence, individuals prone to split fall could benefit from targeting of specific neuromuscular training related to motor strategies recruiting plantar flexion and hip extension that might improve relative recovery step placement and recovery rates. While for repeated feet-forward fallers, neuromuscular training related to motor strategies recruiting knee and hip extension might be helpful. However, the postulations require further investigation.
In summary, this study investigated the relationship between recovery step placement and fall likelihood upon experiencing a slip. This paper was the first to postulate the notion of an optimal recovery step zone within which the recovery rate following a slip would be higher than for other zones. The results showed that a more posterior recovery step placement would improve stability but weaken limb support, and vice versa for a more anterior step placement. It was also found that the recovery step placement was related to the plantar flexor and hip flexor moments in pre-swing phase, and the knee and hip extensor moments in the swing phase. The findings from this study could assist clinicians in developing step training paradigms for fall prevention in older adults.
Figure 3.
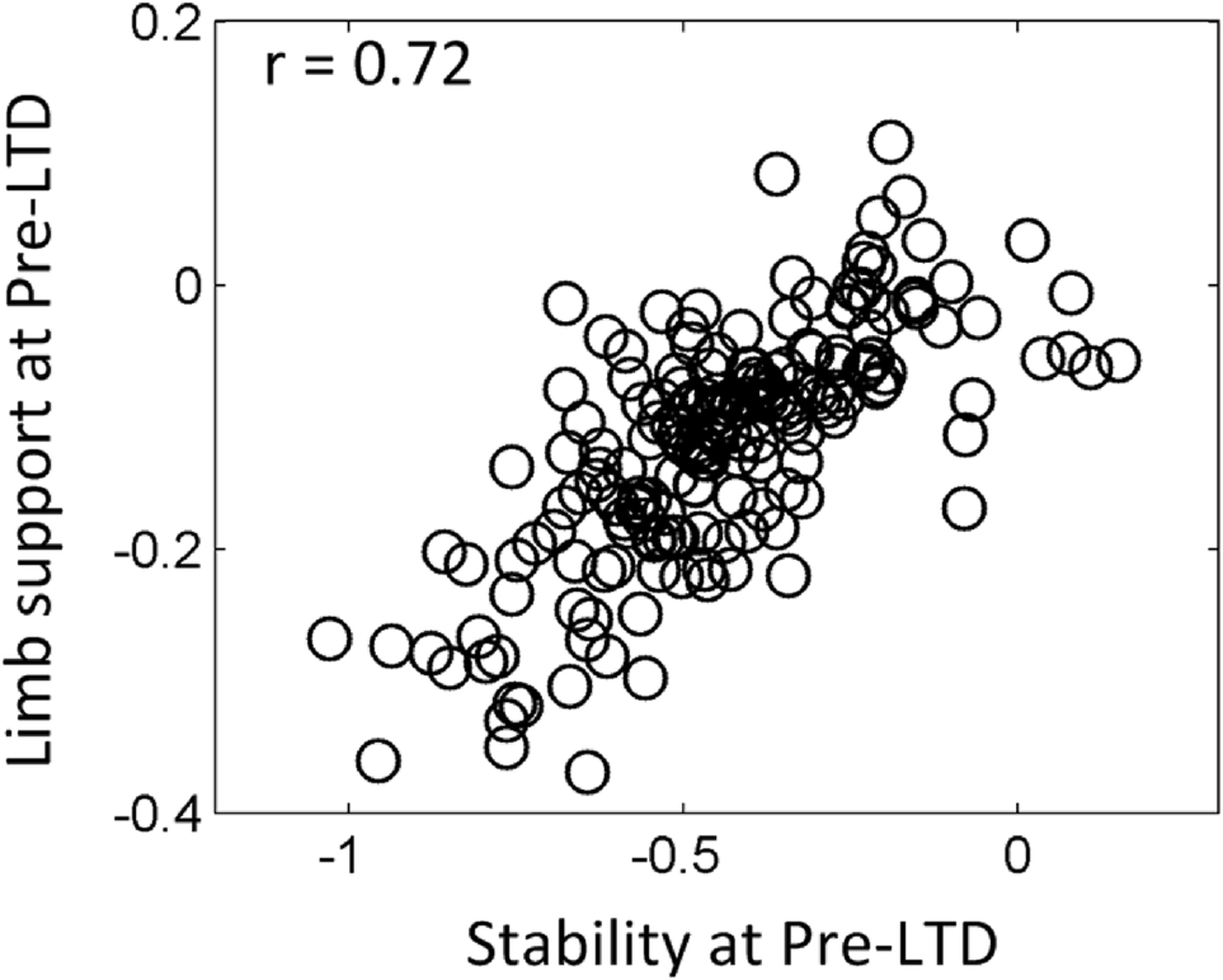
Relationship between stability and limb support at pre-LTD (LTD − 10ms).
Acknowledgements
This work was supported by NIH R01-AG050672-02 (to Tanvi Bhatt) and NIH R01-AG044364 (to Tanvi Bhatt & Yi-Chung Pai). We thank Ms. Alison Schenone for helpful edits.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of interest
None
References:
- 1.Beschorner K and Cham R. Impact of joint torques on heel acceleration at heel contact, a contributor to slips and falls. Ergonomics 51: 1799–1813, 2008. [DOI] [PubMed] [Google Scholar]
- 2.Bhatt T and Pai YC. Immediate and latent interlimb transfer of gait stability adaptation following repeated exposure to slips. Journal of Motor Behavior 40: 380–390, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatt T, Wening JD and Pai YC. Adaptive control of gait stability in reducing slip-related backward loss of balance. Experimental Brain Research 170: 61–73, 2006. [DOI] [PubMed] [Google Scholar]
- 4.Bhatt T, Wening JD and Pai YC. Influence of gait speed on stability: recovery from anterior slips and compensatory stepping. Gait & Posture 21: 146–156, 2005. [DOI] [PubMed] [Google Scholar]
- 5.Cheung VCK, d’Avella A and Bizzi E. Adjustments of Motor Pattern for Load Compensation Via Modulated Activations of Muscle Synergies During Natural Behaviors. Journal of Neurophysiology 101: 1235–1257, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper RC, Prebeau-Menezes LM, Butcher MT and Bertram JEA. Step length and required friction in walking. Gait & Posture 27: 547–551, 2008. [DOI] [PubMed] [Google Scholar]
- 7.de Leva P Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. Journal of Biomechanics 29: 1223–1230, 1996. [DOI] [PubMed] [Google Scholar]
- 8.Delp SL, Anderson FC, Arnold AS, Loan P, Habib A, John CT, Guendelman E and Thelen DG. OpenSim: open-source software to create and analyze dynamic Simulations of movement. Ieee Transactions on Biomedical Engineering 54: 1940–1950, 2007. [DOI] [PubMed] [Google Scholar]
- 9.Espy DD, Yang F, Bhatt T and Pai YC. Independent influence of gait speed and step length on stability and fall risk. Gait & Posture 32: 378–382, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaffney BM, Harris MD, Davidson BS, Stevens-Lapsley JE, Christiansen CL and Shelburne KB. Multi-Joint Compensatory Effects of Unilateral Total Knee Arthroplasty During High-Demand Tasks. Annals of Biomedical Engineering 44: 2529–2541, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghoussayni S, Stevens C, Durham S and Ewins D. Assessment and validation of a simple automated method for the detection of gait events and intervals. Gait & Posture 20: 266–272, 2004. [DOI] [PubMed] [Google Scholar]
- 12.Grabiner MD, Bareither ML, Gatts S, Marone J and Troy KL. Task-Specific Training Reduces Trip-Related Fall Risk in Women. Medicine and Science in Sports and Exercise 44: 2410–2414, 2012. [DOI] [PubMed] [Google Scholar]
- 13.Grabiner MD, Koh TJ, Lundin TM and Jahnigen DW. Kinematics of Recovery from a Stumble. Journals of Gerontology 48: M97–M102, 1993. [DOI] [PubMed] [Google Scholar]
- 14.Hof AL The ground reaction vector in walking passes always (almost) through the same point. Journal of Biomechanics 46: 631–632, 2013. [DOI] [PubMed] [Google Scholar]
- 15.Hsiao-Wecksler ET and Robinovitch SN. The effect of step length on young and elderly women’s ability to recover balance. Clinical Biomechanics 22: 574–580, 2007. [DOI] [PubMed] [Google Scholar]
- 16.King GW, Luchies CW, Stylianou AP, Schiffman JM and Thelen DG. Effects of step length on stepping responses used to arrest a forward fall. Gait & Posture 22: 219–224, 2005. [DOI] [PubMed] [Google Scholar]
- 17.Lacquaniti F, Grasso R and Zago M. Motor patterns in walking. News in Physiological Sciences 14: 168–174, 1999. [DOI] [PubMed] [Google Scholar]
- 18.Liu X, Reschechtko S, Wang SJ and Pai YC. The recovery response to a novel unannounced laboratory-induced slip: The “first trial effect” in older adults. Clinical Biomechanics 48: 9–14, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacLean JGB and Reddy SK. The contralateral slip - An avoidable complication and indication for prophylactic, pinning in slipped upper femoral epiphysis. Journal of Bone and Joint Surgery-British Volume 88b: 1497–1501, 2006. [DOI] [PubMed] [Google Scholar]
- 20.Mak MKY, Yang F and Pai YC. Limb Collapse, Rather Than Instability, Causes Failure in Sit-to-Stand Performance Among Patients With Parkinson Disease. Physical Therapy 91: 381–391, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maki BE and McIlroy WE. The role of limb movements in maintaining upright stance: The “change-in-support” strategy. Physical Therapy 77: 488–507, 1997. [DOI] [PubMed] [Google Scholar]
- 22.Maki BE, McIlroy WE and Fernie GR. Change-in-support reactions for balance recovery. Ieee Engineering in Medicine and Biology Magazine 22: 20–26, 2003. [DOI] [PubMed] [Google Scholar]
- 23.Mansfield A, Inness EL, Wong JS, Fraser JE and McIlroy WE. Is Impaired Control of Reactive Stepping Related to Falls During Inpatient Stroke Rehabilitation? Neurorehabilitation and Neural Repair 27: 526–533, 2013. [DOI] [PubMed] [Google Scholar]
- 24.Martelli D, Aprigliano F, Tropea P, Pasquini G, Micera S and Monaco V. Stability against backward balance loss: Age-related modifications following slip-like perturbations of multiple amplitudes. Gait & Posture 53: 207–214, 2017. [DOI] [PubMed] [Google Scholar]
- 25.Maus HM, Lipfert SW, Gross M, Rummel J and Seyfarth A. Upright human gait did not provide a major mechanical challenge for our ancestors. Nature Communications 1: 2010. [DOI] [PubMed] [Google Scholar]
- 26.Neptune RR, Kautz SA and Zajac FE. Contributions of the individual ankle plantar flexors to support, forward progression and swing initiation during walking. Journal of Biomechanics 34: 1387–1398, 2001. [DOI] [PubMed] [Google Scholar]
- 27.Pai Y-C and Patton JL. Center of mass velocity-position predictions for balance control. Journal of Biomechanics 30: 347–354, 1997. [DOI] [PubMed] [Google Scholar]
- 28.Pai YC Movement termination and stability in standing. Exercise and Sport Sciences Reviews 31: 19–25, 2003. [DOI] [PubMed] [Google Scholar]
- 29.Pai YC, Yang F, Bhatt T and Wang E. Learning from laboratory-induced falling: long-term motor retention among older adults. Age 36: 1367–1376, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pai YC, Yang F, Wening JD and Pavol MJ. Mechanisms of limb collapse following a slip among young and older adults. Journal of Biomechanics 39: 2194–2204, 2006. [DOI] [PubMed] [Google Scholar]
- 31.Pavol MJ, Owings TM, Foley KT and Grabiner MD. Mechanisms leading to a fall from an induced trip in healthy older adults. Journals of Gerontology Series a-Biological Sciences and Medical Sciences 56: M428–M437, 2001. [DOI] [PubMed] [Google Scholar]
- 32.Pavol MJ and Pai YC. Deficient limb support is a major contributor to age differences in falling. Journal of Biomechanics 40: 1318–1325, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Piazza SJ and Delp SL. The influence of muscles on knee flexion during the swing phase of gait. Journal of Biomechanics 29: 723–733, 1996. [DOI] [PubMed] [Google Scholar]
- 34.Prilutsky BI, Gregor RJ and Ryan MM. Coordination of two-joint rectus femoris and hamstrings during the swing phase of human walking and running. Experimental Brain Research 120: 479–486, 1998. [DOI] [PubMed] [Google Scholar]
- 35.Wang S, Liu X, Lee A and Pai Y-C. Can Recovery Foot Placement Affect Older Adults’ Slip-Fall Severity? Annals of Biomedical Engineering 1–8, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang SJ, Liu X and Pai YC. Limb Collapse or Instability? Assessment on Cause of Falls. Annals of Biomedical Engineering 47: 767–777, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Winter DA CNS strategies in human gait: implication for FES control. Automedica 11: 163–174, 1989. [Google Scholar]
- 38.Winter DA Foot trajectory in human gait: a precise and multifactorial motor control task. Physical Therapy 72: 45–53; discussion 54–46, 1992. [DOI] [PubMed] [Google Scholar]
- 39.Yamaguchi T and Masani K. Contribution of center of mass–center of pressure angle tangent to the required coefficient of friction in the sagittal plane during straight walking. Biotribology 5: 16–22, 2016. [Google Scholar]
- 40.Yang F, Anderson FC and Pai YC. Predicted threshold against backward balance loss following a slip in gait. Journal of Biomechanics 41: 1823–1831, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang F, Anderson FC and Pai YC. Predicted threshold against backward balance loss in gait. Journal of Biomechanics 40: 804–811, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang F, Bhatt T and Pai YC. Role of stability and limb support in recovery against a fall following a novel slip induced in different daily activities. Journal of Biomechanics 42: 1903–1908, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang F, Espy D and Pai YC. Feasible Stability Region in the Frontal Plane During Human Gait. Annals of Biomedical Engineering 37: 2606–2614, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang F and Pai YC. Automatic recognition of falls in gait-slip training: Harness load cell based criteria. Journal of Biomechanics 44: 2243–2249, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu B, Gabriel D, Noble L and An KN. Estimate of the optimum cutoff frequency for the Butterworth low-pass digital filter. Journal of Applied Biomechanics 15: 318–329, 1999. [Google Scholar]


