Abstract
Study Objectives:
Like other medical branches, the practice of sleep medicine has been affected by the COVID-19 pandemic; however, the actual impact is not known. This study was planned to assess the status of the practice of sleep medicine in India during the COVID-19 pandemic and lockdown.
Methods:
This was an online questionnaire–based descriptive study. A 25-item questionnaire was developed to assess the functioning of sleep laboratories, use of telemedicine, and positive airway pressure therapy during the COVID-19 pandemic in India. The questionnaire was sent to the sleep physicians of 2 major sleep medicine societies of India. Responses were analyzed.
Results:
In this study, the response rate was 64.6%. During this pandemic, 72% of physicians reported that they had closed sleep laboratory, whereas 24% reported shifting to home sleep apnea testing. Only half of the sleep physicians confirmed awareness of the disinfection guidelines proposed by the American Academy of Sleep Medicine to prevent COVID-19 infection in the sleep laboratory. However, almost all of them reported taking preventive measures like the use of protective gear. Sixty-one percent of physicians advised mitigating strategies as a temporary measure to their patients of obstructive sleep apnea. A total of 58.6% opined that auto–positive airway pressure might be used for uncomplicated obstructive sleep apnea without diagnostic polysomnography during the pandemic. Eighty-four percent of physicians reported that they were continuing their services through a telemedicine facility. Physicians reported that consultations for insomnia and circadian rhythm sleep disorders increased during the pandemic.
Conclusions:
Sleep laboratories were reportedly closed during the COVID-19 pandemic, and most of the sleep physicians were providing services through telemedicine. The majority reported that auto–positive airway pressure without diagnostic polysomnography could be an effective option for uncomplicated obstructive sleep apnea. Consultation for insomnia and circadian rhythm sleep disorders reportedly increased during the lockdown.
Citation:
Kanchan S, Saini LK, Daga R, Arora P, Gupta R. Status of the practice of sleep medicine in India during the COVID-19 pandemic. J Clin Sleep Med. 2021;17(6):1229–1235.
Keywords: sleep laboratory, COVID-19 pandemic, health care personnel, guidelines, telemedicine
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep medicine services have been affected during the COVID-19 pandemic; however, its actual magnitude has not been studied systematically.
Study Impact: The present study sheds light on the awareness of sleep physicians on guidelines for conducting sleep studies and managing sleep laboratories during the COVID-19 pandemic in India. It also highlights the measures taken so they could continue to provide clinical services. In addition, this study depicts sleep physicians’ opinions on managing obstructive sleep apnea and reported changes in the category of sleep disorders during the pandemic.
INTRODUCTION
The COVID-19 pandemic has taken the world by surprise. This highly contagious coronavirus has led sleep medicine societies across the globe to frame practice guidelines so that the risk to health care providers, patients, and the general community can be minimized during consultations, sleep study, and other therapeutic procedures.1 The American Academy of Sleep Medicine (AASM) has issued guidelines that cover a wide range of issues such as selection of a patient for sleep studies, screening of patient and the hospital staff, infection control, use of appropriate personal protective equipment, conducting home sleep tests, use of reusable and single-use devices, and stratifying guidelines for conducting polysomnography, based on the degree of community spread.2 Similarly, the European Sleep Society and the British Sleep Society have also issued guidelines for conducting cognitive behavior therapy for insomnia and for the management of obstructive sleep apnea (OSA) during the ongoing COVID-19 pandemic, respectively.3,4 The Indian Society for Sleep Research has recently issued guidelines for sleep medicine practice during the COVID-19 pandemic, which have been framed keeping in mind the practice scenario in the Indian subcontinent.5 The Indian Society for Sleep Research guidelines, in addition to the issues covered in previously mentioned guidelines, also addressed concerns related to telemedicine services for providing medical help to patients with sleep disorders.
Telemedicine has emerged as a capable vehicle for providing treatment to the patients at their doorstep while maintaining physical distancing. AASM released a position statement regarding telemedicine in 2015, emphasizing its use in managing patients with sleep disorders while maintaining standards of care.6 After lockdown in India, the Medical Council of India also issued telemedicine practice guidelines to help the physicians. These guidelines addressed different aspects of telemedicine, such as mode of telecommunication to be used, record keeping during teleconsultation, and medical ethics to be followed.7
Despite available guidelines for general and sleep medicine practice during the pandemic, few issues are still unclear: (1) effect of the pandemic on polysomnography; (2) extent of adherence to the prevailing guidelines during teleconsultation and polysomnography; (3) opinions and changes in the practice of management of sleep disorders, especially OSA during the pandemic; and (4) change, if any, in the categories of sleep disorders approaching for consultation. To the best of our knowledge, this has not been investigated thus far in any geographical area, and this is the first survey addressing these issues.
METHODS
This study was conducted after obtaining approval from the institutional ethics committee. Informed consent was taken from all the participants. A questionnaire was developed to assess the practice of sleep medicine during the COVID-19 pandemic and was sent to the physicians practicing clinical sleep medicine in India.
Questionnaire
The questionnaire contains 25 items, divided into 4 sections. The first section had items related to the impact of COVID-19 on polysomnography. The second section had items related to the practice of sleep medicine using telemedicine facilities. This section had addressed adherence to sleep medicine practice according to Indian guidelines for teleconsultation.7 The third section focused on issues related to home sleep apnea testing (HSAT) and attended polysomnography. Information related to positive airway pressure (PAP) therapy during the pandemic was covered in the fourth section. Last, all the participants were asked whether they have observed a change in patients’ diagnostic categories in their practice. Based on our previous experience with surveys, we kept the questionnaire as brief as possible, and most of the items were close ended. Thus, respondents were requested to pick the best statement that applied to their practice of sleep medicine during COVID-19 (questionnaire (201.2KB, pdf) available in the supplemental material).
Identification of sleep physicians
Two professional societies are engaged in disseminating knowledge related to sleep medicine in India: the Indian Society for Sleep Research and the Indian Sleep Disorders Association. Membership in these societies includes physicians from three categories: physicians exclusively practicing sleep medicine; physicians practicing sleep medicine as a limited part of their primary specialty (pulmonology, neurology, psychiatry, dentistry, pediatrics); and sleep researchers from basic science disciplines. Members of these bodies cater to patients with a variety of sleep disorders. Another organization—the Indian Association of Surgeons for Sleep Apnea—has members working in only a specific area of sleep medicine (ie, surgical management of OSA). Hence, directories of Indian Society for Sleep Research and Indian Sleep Disorders Association were scrutinized, and the members involved in the first 2 categories were identified and approached. Emails of all eligible sleep physicians were collected through the directories, and a questionnaire was sent to them.
Data collection and analysis
The questionnaire was converted into a Google Form. A link to the questionnaire was sent to sleep physicians through an email. Because they were requested to provide their names in the form, nonresponders were easy to identify. Nonresponders were sent a reminder email after 2–3 days that requested that they submit their response. Reminders were sent twice at the interval of 2–3 days. After that, nonresponse was considered as unwillingness to participate in the study. Descriptive analysis was done using SPSS version 23 (IBM SPSS Statistics for Windows, Version 23.0, IBM Corp., Armonk, NY).
RESULTS
A total of 130 sleep physicians were approached, and 84 responded to the survey (response rate of 64.6%). Of 84 responses, 75 were valid responses as 9 responses belonged to members practicing outside India or were duplicate responses. Hence, they were excluded.
Teleconsultation for sleep medicine
Eighty-four percent of physicians reported serving patients of various sleep disorders through teleconsultation. Forty-four percent of these were providing teleconsultation to the new patients: 84% to the patients who have consulted them in-person before lockdown and 28.5% to the patients already using PAP device. There was an overlap of physicians in these 3 categories. Sixty-eight percent of physicians reported using only synchronous mode for the teleconsultation, 17.3% both synchronous and asynchronous modes, and the remaining 5% reported using only asynchronous modes. Thirty percent reported keeping partial records of teleconsultations, whereas 47.6% were keeping complete records. Nearly half (52%) of the respondents opined that telemedicine was useful, and another 42.6% reported that it was useful to some extent.
For the follow-up of patients with a PAP device, only 17% reported using cloud technology to capture data from the PAP device. Nearly half (56%) were aware of cloud technology but not using it, whereas others were not even aware of it. Forty-three percent of physicians reported that cognitive behavior therapy for insomnia (CBT-I) was not applicable to their practice. In the remaining, 50% reported administering CBT-I through telemedicine, whereas a similar proportion discontinued it during the pandemic.
Impact of COVID-19 on polysomnography appointments
Ninety-two percent of the physicians reported cancellation of in-laboratory sleep studies or HSAT after the COVD-19 pandemic. They reported that 84% of patients could understand the reason for the cancellation and were cooperative. Eight percent of the patients wanted to get the study done, whereas another 8% discussed alternative measures as an intermediary option. Sixty-four percent of the physicians reported that they were not aware of the availability of portable sleep labs that could be disposed of after a single use (eg, WatchPAT ONE), whereas a small proportion (5%) were using them to manage patients.
HSAT, in-laboratory testing, and actigraphy
Approximately 72% of the physicians reported that they had closed the sleep laboratory, whereas 20% were conducting HSAT, leaving only 8% who were conducting attended polysomnography (Table 1). Patients who had a low risk for COVID-19 and high risk for OSA without any comorbid illness were preferred by physicians for the attended polysomnography. Interestingly, among the sleep physicians who continued sleep studies during the pandemic (n = 21), only half of them were aware of the guidelines of AASM regarding the disinfection of sleep laboratory to prevent COVID-19 infection among patients. However, almost all the sleep physicians were taking safety measures while conducting sleep studies in the form of personal protective equipment and repeated sanitization of equipment and surface (Table 1). Only 8% were doing actigraphy during the COVID-19 pandemic.
Table 1.
Effect of knowledge and practice of disinfection on polysomnography.
| Serial. No. | Item | Responses | Status of Sleep Study during COVID-19 Pandemic (n = 75) | |||
|---|---|---|---|---|---|---|
| Not Conducting Sleep Study (n = 54) | Conducting Sleep Study during Pandemic (n = 21) | |||||
| Yes, Shifted from Attended Sleep Studies to HSAT Completely (n = 5) | Yes, Mostly HSAT (n = 10) | Yes, Mostly Lab Based (n = 6) | ||||
| 1. | Are you doing COVID test of patients before sleep study? | Only in suspected COVID | NA | 1 (20%) | 6 (60%) | 5 (83%) |
| All patients | NA | 1 (20%) | 1 (10%) | 1 (17%) | ||
| Not advising | NA | 3 (60%) | 3 (30%) | 0 | ||
| 2. | Are you following disinfection guidelines proposed by AASM? | Not aware of guidelines but taking additional preventive measures | NA | 2 (40%) | 7 (70%) | 1 (17%) |
| Yes | NA | 3 (60%) | 3 (30%) | 4 (67%) | ||
| No | 0 | 0 | 1 (16.7%) | |||
AASM = American Academy of Sleep Medicine, HSAT = home sleep apnea test, NA = not applicable.
PAP therapy during COVID-19
Fifty-two percent of the physicians participating in the study opined that viral filters should be used with the interface in all patients (Table 2). More than half (58.6%) opined that auto-titrating continuous PAP could be advised without a sleep study in patients with uncomplicated suspected OSA during the pandemic (Figure 1). Table 2 depicts beliefs regarding PAP therapy among sleep physicians.
Table 2.
Alternatives for management of OSA among groups based on sleep study.
| Serial. No. | Item | Responses | Status of Sleep Study during COVID-19 Pandemic (n = 75) | |||
|---|---|---|---|---|---|---|
| Not Conducting Sleep Study (n = 54) | Yes, Shifted from in Lab Studies to HSAT Completely (n = 5) | Yes, Mostly HSAT (n = 10) | Yes, Mostly Lab Based (n = 6) | |||
| 1. | Aware of disposable sleep labs | Yes | 20 (37%) | 1 (20%) | 3 (30%) | 3 (50%) |
| No | 34 (63% | 4 (80%) | 7 (70%) | 3 (50%) | ||
| 2. | Using disposable sleep labs | Yes | 3 (6%) | 0 (0%) | 0 (0%) | 1 (17%) |
| No | 51 (94%) | 5 (100%) | 10 (100%) | 5 (83%) | ||
| 3. | Do you think nonvented mask with viral filter should be used during pandemic | Yes | 29 (54%) | 2 (40%) | 6 (60%) | 2 (33%) |
| Yes, but only for suspected COVID | 19 (35%) | 1 (20%) | 4 (40%) | 2 (33%) | ||
| Not needed | 6 (11%) | 2 (40%) | 0 (0%) | 2 (33%) | ||
| 4. | Do you think auto-PAP is a viable option for uncomplicated OSA until a sleep study is done? | Yes | 31 (57%) | 3 (60%) | 7 (70%) | 3 (50%) |
| No | 8 (15%) | 2 (40%) | 1 (10%) | 1 (17%) | ||
| Not sure | 12 (22%) | 0 (0%) | 2 (20%) | 2 (33%) | ||
| 5. | Are you advising mitigation/alternative therapy to patients with suspected OSA until a sleep study is done? | Yes | 32 (59%) | 3 (60%) | 7 (70%) | 4 (67%) |
| No | 15 (28%) | 2 (40%) | 3 (30%) | 1 (17%) | ||
HSAT = home sleep apnea test, OSA = obstructive sleep apnea, PAP = positive airway pressure.
Figure 1. Percentage of sleep physicians advocating for auto-PAP for patients with uncomplicated OSA before sleep study.
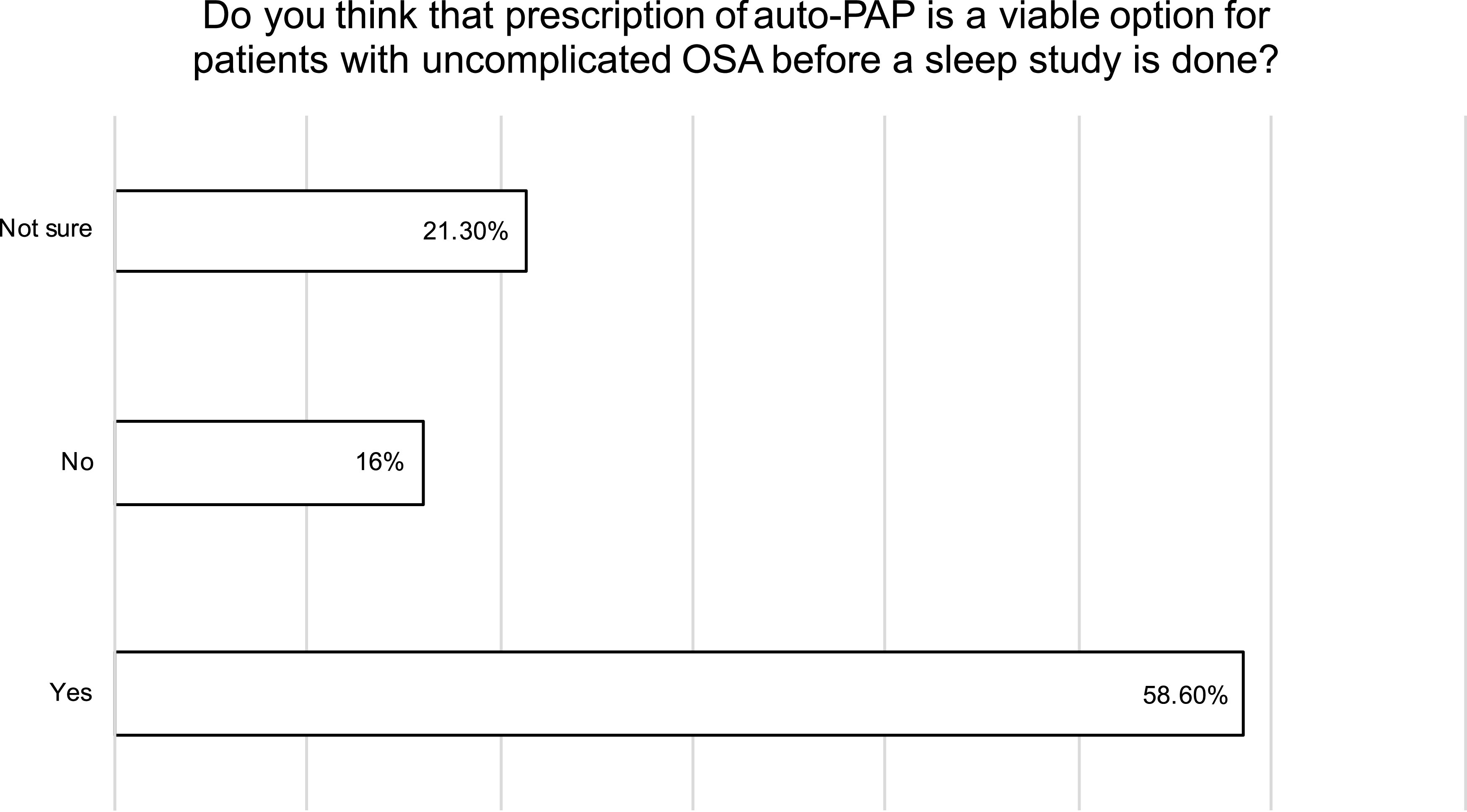
The majority (58.6%) of sleep physicians advocated for using auto-PAP for patients with uncomplicated OSA before a diagnostic polysomnography was done. It shows the urge to start PAP therapy in limited health care access, although this approach is not well studied and advocated by sleep societies. OSA = obstructive sleep apnea, PAP = positive airway pressure.
Ninety-five percent of physicians favored the continuing use of PAP in existing PAP users. Twenty-four percent opined that all PAP users must sleep in a separate room, whereas 55% advocated separation from bed partners only for patients with suspected COVID-19 infection. Sixty-one percent of physicians were advising mitigating strategies to their patients having OSA as an intermediary measure.
Increase in sleep disorders
Sixty-one percent of physicians reported that medications were either totally or partially unavailable during the lockdown. Figure 2 shows physician’s reports regarding the increment of patients with different sleep disorders in their clinics during the pandemic. Seventy-nine percent of physicians believed that insufficient light exposure and increased use of screens emitting light in the blue-range spectrum in the late evening had resulted in an increment of patients with circadian rhythm sleep disorders during the pandemic.
Figure 2. Increase in patients with different sleep disorders during the COVID-19 pandemic.
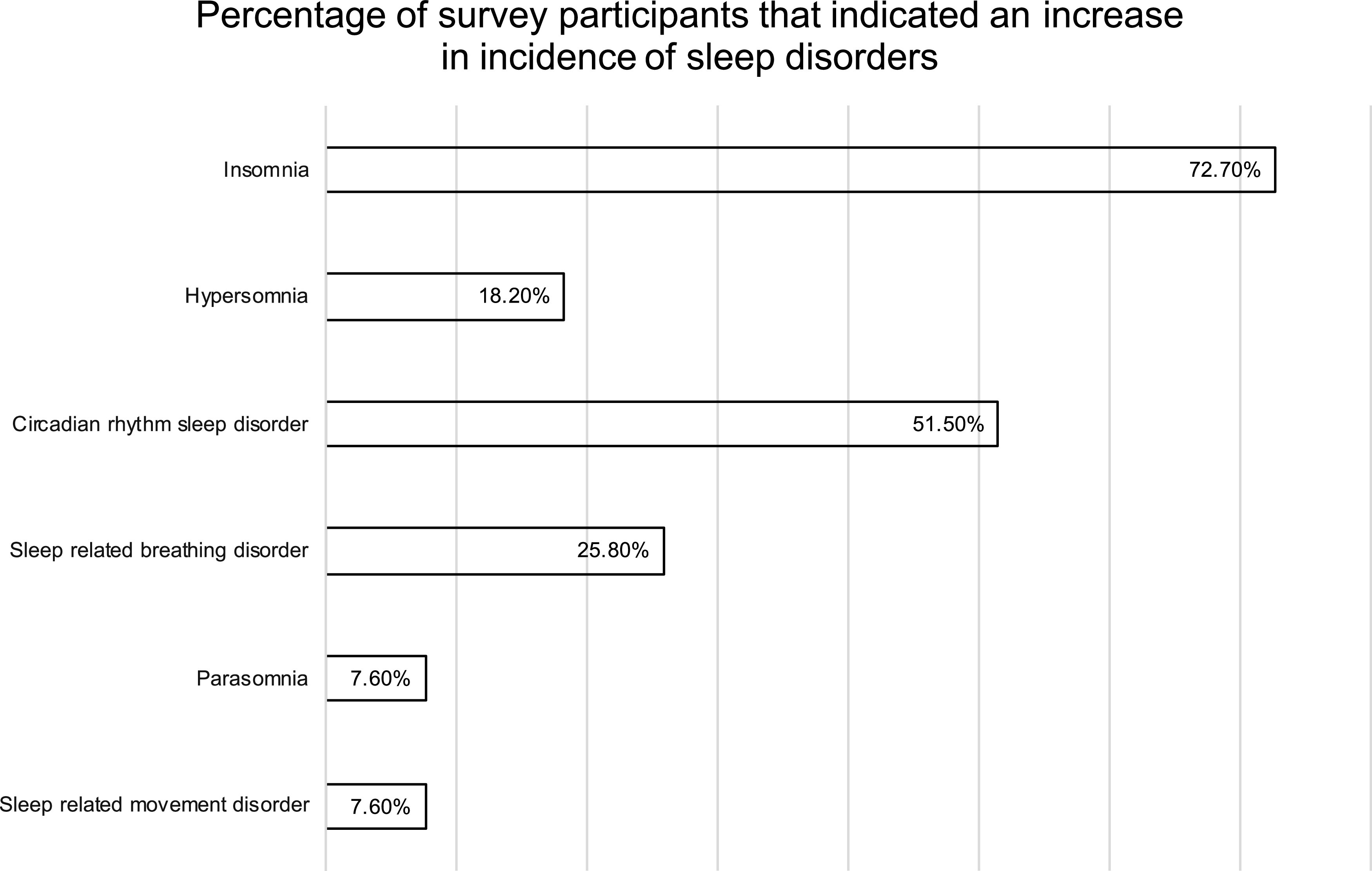
All the sleep-related disorders are on the rise during the pandemic. However, most of the physicians agree on the increasing incidence of insomnia and circadian rhythm sleep disorders. The increasing anxiety, stress, and fear of health seems to be the reason behind this rise.
DISCUSSION
This study provides the status of the practice of sleep medicine and the functioning of sleep laboratories in India during the COVID-19 pandemic. Most of the sleep physicians reported using a telemedicine facility for services to their patients. However, because of the pandemic, most of the sleep laboratories reportedly discontinued polysomnography, whether attended or HSAT. Among the sleep physicians who were conducting sleep studies during the pandemic, only half reported having knowledge about guidelines of AASM for the continuing practice of sleep study during the pandemic. However, adequate safety measures were reportedly adopted by most physicians who continued sleep study during the pandemic to ensure the safety of the patient and staff. More than half of the physicians reported the use of mitigating strategies to provide benefit to patients with OSA as an intermediary measure. A nearly similar number of physicians opined that the prescription of an auto-PAP might be a viable option for patients with a high risk of uncomplicated OSA without the need for diagnostic study. Last, there was an increase in the number of patients with insomnia and circadian rhythm sleep disorders, as reported in the study.
Most of the sleep physicians reportedly chose to discontinue sleep study during the pandemic in India, similar to the observation from the United States.8 In the present study, 84% of the sleep physicians reported providing teleconsultation for sleep disorders, and 22.6% reported online CBT-I during the pandemic. We tried to find out similar studies but could not find any study addressing this issue before the pandemic.
The use of telemedicine services to help patients is a welcoming change in a country of 1.3 billion, where the prevalence of insomnia, restless legs syndrome, and OSA is 10%, 2.3%, and 3.7%–7.5%, respectively.9–12 In such a scenario, teleconsultation should be encouraged to bridge the existing gaps in service delivery and to reduce the health and economic impact of sleep disorders.13,14 Sleep physicians from the United States have shown an inclination toward continuing telemedicine services even after the pandemic would be over, and the same may be followed in India.8 Internet-delivered CBT-I has also been found as an effective management strategy to improve sleep (sleep efficiency, total sleep time, and reduced severity of insomnia) similar to the face-to-face CBT-I among adults with insomnia.15,16 Shifting to the online delivery of CBT-I will help patients with insomnia by reducing the economic burden and improving their productivity and quality of life. This is an important issue, especially in a country where human resources to conduct the CBT-I are limited and available only in large cities.13,17 Similarly, patients with OSA who are using PAP therapy also require periodic follow-ups.18 Usually, patients prefer and are also encouraged by physicians to seek face-to-face consultations in PAP clinics. In the recent past, PAP device manufacturers have started adopting cloud-based technology to generate compliance reports from the PAP devices. This is a welcoming move, which, along with teleconsultation, can be used to reduce the cost of aftercare for patients having OSA.19
Documentation is an important part of medical consultations; hence, at least minimal documentation of the teleconsultations has been emphasized in the Indian guidelines for telemedicine practice.7 However, only half of the sleep physicians in the present study reported maintaining records for the same.7 In this study, reasons for the failure to document teleconsultations were not assessed because it was not anticipated. One possible reason for the same could be the use of synchronous modes of teleconsultation by most physicians, which makes documentation difficult, especially when one is catering to a large number of patients. Irrespective of the reason for failure to document teleconsultations, this finding necessitates a need to make the physicians aware that teleconsultations also have medico-legal implications similar to face-to-face consultations. Hence, the practice of the documentation of every consultation should match with the prepandemic face-to-face consultation period.20
Sleep disorders are rarely life threatening, although their impact on health and the economic burden imposed by them cannot be underestimated.13,14 To address this issue, several professional bodies have come with guidelines, especially targeted to prevent cross-infection during the pandemic.2–5 However, in the present study, nearly half of the sleep physicians reported that they were not aware of AASM guidelines. This could have been a reason for the closure of the sleep laboratory and advising mitigation strategies to the patients having OSA during the pandemic in India, an observation similar to that of the United States.8 It should be noted that mitigation strategies in the form of aerobic exercises, dietary weight loss, and positional therapy have been found inferior to PAP therapy in decreasing the apnea-hypopnea index and oxygen desaturation index.21 It becomes more important considering the recent literature, which suggests that patients with OSA have an 8 times greater risk of contracting the COVID-19 infection than the matched population.22 Besides increasing the risk of infection, OSA also increases the risk of hospitalization and respiratory failure after contracting the COVID-19 infection.22 Hence, an attempt should be made to open the sleep laboratories during the pandemic, although after taking optimal precautions as suggested in various guidelines.2–5 Making sleep physicians aware of the guidelines for reopening of sleep laboratories can be an excellent strategic step in this regard.
Whether to continue the PAP therapy is an important issue considering the proneness of OSA patients to catch the COVID-19 infection and its sequels, as discussed above.22 Although the use of a PAP device is considered an aerosol-generating procedure that can increase the risk of transmission of the SARS-CoV-2 virus, at the same time, another report suggests that it reduces the risk of aspiration pneumonia in patients with OSA.23–25 Moreover, the British Thoracic Society advocates continuing use of PAP therapy unless one has symptoms suggestive of COVID-19 infection.26 Aerosol generation can easily be countered by using a nonvented mask with a viral filter or suggesting the patient with OSA to sleep in a separate room.26–28 Most of the physicians included in this study reported to possess this knowledge, and hence they reported that they were advising continuation of PAP therapy to the existing PAP users and adopting preventive measures to reduce chances of infection through PAP.
The opinion of sleep physicians regarding the use of auto-PAP without diagnostic study for patients with uncomplicated OSA is another issue that requires discussion. Recent guidelines from AASM recommended the use of auto-PAP for the management of OSA. However, it must be followed by diagnostic polysomnography for adults having uncomplicated OSA.18 This recommendation was made to reduce the time lag between diagnosis and treatment initiation, reduce the cost of treatment, and provide care at the patient’s doorstep.18 It is essential to realize that guidelines did not advocate the use of auto-PAP without the diagnostic sleep study either in-lab or HSAT. Moreover, guidelines also identified certain limitations with the initiation of auto-PAP therapy at home, such as failure to identify and rectify problems related to mask fitting, leakage from the mask, and other PAP-related issues that can be efficiently dealt during attended PAP titration (eg, pressure intolerance). Besides the issues related to the interface and pressure intolerance, different auto-PAP machines also follow different algorithms, thus responding to different stimuli to change the pressure, and it ultimately results in difference in the efficacy among auto-PAP devices.29 Last, the difference in cost between auto-PAP and continuous PAP should also be considered, especially in India, where most of the patients have to bear the cost of the PAP device themselves. These issues must be given due consideration, especially when results of a meta-analysis failed to show any difference between auto-PAP and relatively cheaper continuous PAP devices with regard to adherence, improvement in the apnea-hypopnea index, arousal index, and daytime somnolence.30,31
Last, sleep physicians participating in the present study reported that consultations for insomnia and circadian rhythm sleep disorders increased during the pandemic. Whether this finding represents increased rates of these disorders in the population or merely greater access to health professionals during the pandemic is unclear. However, recent evidence suggested that the prevalence of insomnia and poor sleep quality has increased during the pandemic, and bedtimes and waketimes have been delayed during the lockdown.32–34 Several emotional and systemic factors may account for these findings that include perception of stress, absence of social zeitgebers, and increased time spent on mobile or television screen.32,35 Another contributing factor to these findings could be an asymptomatic infection of coronavirus that induces systemic inflammation in addition to infection in areas of the central nervous system that are important for regulation of the sleep-wake cycle.32,35
Like all scientific investigations, this study also had methodologic limitations. This was just a survey, and some of the items had recall bias. Second, the response from nonresponders could have influenced outcomes because this study was based on only 61% response. Third, some pulmonologists and otorhinolaryngologists are practicing sleep medicine as a small part of their clinical practice, and they were not included in this study. Their responses could have been different. Last, this survey provides a cross-sectional view of the practice of sleep medicine during the pandemic, and it may change with time.
In conclusion, the present study showed that most of the sleep laboratories were shut down during the pandemic, although many sleep physicians were reportedly providing patient care through teleconsultation. Most of the physicians reported that they advised existing PAP users to continue therapy. However, this study shows that there is a need to make the physicians aware of 2 important issues: documentation during teleconsultation and rationale use of auto-PAP devices to manage OSA as per prevailing guidelines.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. The authors report no conflicts of interest.
SUPPLEMENTARY MATERIAL
ABBREVIATIONS
- AASM
American Academy of Sleep Medicine
- CBT-I
cognitive behavior therapy for insomnia
- HSAT
home sleep apnea test
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
REFERENCES
- 1. Drummond M . Sleep labs, lung function tests and COVID-19 pandemic: only emergencies allowed! Pulmonology . 2020. ; 26 ( 4 ): 244 – 245 . 10.1016/j.pulmoe.2020.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Sleep Medicine . COVID-19 mitigation strategies for sleep clinics and labs http://www.aptec.pt/media/Recomendacoes_Sleep_Clinics_and_Labs.pdf. Accessed November 17, 2020.
- 3. Altena E , Baglioni C , Espie CA , et al . Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy . J Sleep Res . 2020. ; 29 ( 4 ): e13052 . 10.1111/jsr.13052 [DOI] [PubMed] [Google Scholar]
- 4.Durrant S, Quinnell T, Hare A, et al. BSS Statement on Sleep-Related Advice during the Coronavirus (Covid-19). London: Pandemic; 2020. [Google Scholar]
- 5. Gupta R , Kumar VM , Tripathi M , et al . Guidelines of the Indian Society for Sleep Research (ISSR) for practice of sleep medicine during COVID-19 . Sleep Vigil . 2020. ; 2020 ( July ): 1 – 12 . 10.1007/s41782-020-00097-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Singh J , Badr MS , Diebert W , et al . American Academy of Sleep Medicine (AASM) position paper for the use of telemedicine for the diagnosis and treatment of sleep disorders . J Clin Sleep Med . 2015. ; 11 ( 10 ): 1187 – 1198 . 10.5664/jcsm.5098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Board of Governors, In Supersession of the Medical Council of India; Niti Aayog. Telemedicine Practice Guidelines Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine. New Delhi, India: Medical Council of India; 2020. Accessed March 12, 2021.
- 8. Johnson KG , Sullivan SS , Nti A , Rastegar V , Gurubhagavatula I . The impact of the COVID-19 pandemic on sleep medicine practices . J Clin Sleep Med . 2021. ; 17 ( 1 ): 79 – 87 . 10.5664/jcsm.8830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khan IW , Juyal R , Shikha D , Gupta R . Generalized anxiety disorder but not depression is associated with insomnia: a population based study . Sleep Sci . 2018. ; 11 ( 3 ): 166 – 173 . 10.5935/1984-0063.20180031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gupta R , Ulfberg J , Allen RP , Goel D . Comparison of subjective sleep quality of long term residents at low and high altitudes: SARAHA study . J Clin Sleep Med . 2018. ; 14 ( 1 ): 15 – 21 . 10.5664/jcsm.6870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gupta R , Ulfberg J , Allen RP , Goel D . High prevalence of restless legs syndrome/Willis Ekbom Disease (RLS/WED) among people living at high altitude in the Indian Himalaya . Sleep Med . 2017. ; 35 : 7 – 11 . 10.1016/j.sleep.2017.02.031 [DOI] [PubMed] [Google Scholar]
- 12. Pinto AM , Devaraj U , Ramachandran P , Joseph B , D’Souza GA . Obstructive sleep apnea in a rural population in South India: feasibility of health care workers to administer level III sleep study . Lung India . 2018. ; 35 ( 4 ): 301 – 306 . 10.4103/lungindia.lungindia_433_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wickwire EM , Shaya FT , Scharf SM . Health economics of insomnia treatments: the return on investment for a good night’s sleep . Sleep Med Rev . 2016. ; 30 : 72 – 82 . 10.1016/j.smrv.2015.11.004 [DOI] [PubMed] [Google Scholar]
- 14. Salas RE , Kwan AB . The real burden of restless legs syndrome: clinical and economic outcomes . Am J Manag Care . 2012. 18 ( 9 suppl ): S207 – S212 . [PubMed] [Google Scholar]
- 15. Ye YY , Chen NK , Chen J , et al . Internet-based cognitive-behavioural therapy for insomnia (ICBT-i): a meta-analysis of randomised controlled trials . BMJ Open . 2016. ; 6 ( 11 ): e010707 . 10.1136/bmjopen-2015-010707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Seyffert M , Lagisetty P , Landgraf J , et al . Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-analysis . PLoS One . 2016. ; 11 ( 2 ): e0149139 . 10.1371/journal.pone.0149139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Roach M , Juday T , Tuly R , Chou JW , Jena AB , Doghramji PP . Challenges and opportunities in insomnia disorder . Int J Neurosci . 2020. : 1 – 8 . 10.1080/00207454.2020.1773460 [DOI] [PubMed] [Google Scholar]
- 18. Patil SP , Ayappa IA , Caples SM , Kimoff RJ , Patel SR , Harrod CG . Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Clinical Practice Guideline . J Clin Sleep Med . 2019. ; 15 ( 2 ): 335 – 343 . 10.5664/jcsm.7640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Juarros Martinez SA , Del Olmo Chiches M , Mayoral Aguilera A , et al . Telemonitored CPAP in OSA patient follow-up. Our evidence . Eur Resp J . 2019. ; 54 : PA4162 . 10.1183/13993003.congress-2019.PA4162 [DOI] [Google Scholar]
- 20.Kumar P, Pandey M. Telepsychiatry- boon or bane. In: Srivastava M, Singh NK, Pandey A, eds. Handbook of Mental Helath Issues during COVID-19 Pandemic. 1st ed. Varanasi, India: Department of Psychiatry, Institute of Medical Sciences, Banaras Hindu University; 2020:44–49. [Google Scholar]
- 21. Iftikhar IH , Bittencourt L , Youngstedt SD , et al . Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis . Sleep Med . 2017. ; 30 : 7 – 14 . 10.1016/j.sleep.2016.06.001 [DOI] [PubMed] [Google Scholar]
- 22. Maas MB , Kim M , Malkani RG , Abbott SM , Zee PC . Obstructive sleep apnea and risk of COVID-19 infection, hospitalization and respiratory failure . Sleep Breath . 2020. : 1 – 3 . 10.1007/s11325-020-02203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Barker J , Oyefeso O , Koeckerling D , Mudalige NL , Pan D . COVID-19: community CPAP and NIV should be stopped unless medically necessary to support life . Thorax . 2020. ; 75 ( 5 ): 367 . 10.1136/thoraxjnl-2020-214890 [DOI] [PubMed] [Google Scholar]
- 24. Tran K , Cimon K , Severn M , Pessoa-Silva CL , Conly J . Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review . PLoS One . 2012. ; 7 ( 4 ): e35797 – e35797 . 10.1371/journal.pone.0035797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sullivan CE . Snoring and obstructive sleep apnoea as risk factors in SARS-Cov-2: can nasal CPAP during sleep reduce pneumonia risk? Sleep Biol Rhythms . 2020. ; 1 ( 1 ): 1 – 2 . 10.1007/s41105-020-00295-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.British Thoracic Society . Guidance Regarding Coronavirus (COVID-19) and Obstructive Sleep Apnoea (OSA): For People Who Routinely Use Continuous Positive Airway Pressure (CPAP). Their Families and Health Care Workers. London: British Thoracic Society; 2020. [Google Scholar]
- 27. Baker JG , Sovani M . Case for continuing community NIV and CPAP during the COVID-19 epidemic . Thorax . 2020. ; 75 ( 5 ): 368 . 10.1136/thoraxjnl-2020-214913 [DOI] [PubMed] [Google Scholar]
- 28. Simonds AK , Hanak A , Chatwin M , et al . Evaluation of droplet dispersion during non-invasive ventilation, oxygen therapy, nebuliser treatment and chest physiotherapy in clinical practice: implications for management of pandemic influenza and other airborne infections . Health Technol Assess . 2010. ; 14 ( 46 ): 131 – 172 . 10.3310/hta14460-02 [DOI] [PubMed] [Google Scholar]
- 29. Shi HB , Cheng L , Nakayama M , et al . Effective comparison of two auto-CPAP devices for treatment of obstructive sleep apnea based on polysomnographic evaluation . Auris Nasus Larynx . 2005. ; 32 ( 3 ): 237 – 241 . 10.1016/j.anl.2005.03.007 [DOI] [PubMed] [Google Scholar]
- 30. Nolan GM , Doherty LS , Mc Nicholas WT . Auto-adjusting versus fixed positive pressure therapy in mild to moderate obstructive sleep apnoea . Sleep . 2007. ; 30 ( 2 ): 189 – 194 . 10.1093/sleep/30.2.189 [DOI] [PubMed] [Google Scholar]
- 31. Ip S , D’Ambrosio C , Patel K , et al . Auto-titrating versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: a systematic review with meta-analyses . Syst Rev . 2012. ; 1 ( 1 ): 20 . 10.1186/2046-4053-1-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cellini N , Canale N , Mioni G , Costa S . Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy . J Sleep Res . 2020. ; 29 ( 4 ): e13074 . 10.1111/jsr.13074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pinto J , van Zeller M , Amorim P , et al . Sleep quality in times of Covid-19 pandemic . Sleep Med . 2020. ; 74 : 81 – 85 . 10.1016/j.sleep.2020.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gupta R , Grover S , Basu A , et al . Changes in sleep pattern and sleep quality during COVID-19 lockdown . Indian J Psychiatry . 2020. ; 62 ( 4 ): 370 – 378 . 10.4103/psychiatry.IndianJPsychiatry_523_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Banerjee D , Viswanath B . Neuropsychiatric manifestations of COVID-19 and possible pathogenic mechanisms: Insights from other coronaviruses . Asian J Psychiatr . 2020. ; 54 : 102350 . 10.1016/j.ajp.2020.102350 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


