Abstract
Objective
The prevalence of atherosclerotic cardiovascular disease (ASCVD) in younger adults has increased over the past decade. However, it is less well established whether patient reported outcomes differ between younger and older adults with ASCVD. We sought to evaluate age-specific differences in patient reported outcomes among adults with ASCVD.
Methods
This was a retrospective cross-sectional survey study. We used data from the 2006–2015 Medical Expenditure Panel Survey (MEPS), a nationally representative sample of the United States population. Adults ≥18 years with a diagnosis of ASCVD, ascertained by ICD9 codes or self-reported data, were included. Logistic regression was used to compare self-reported patient-clinician communication, patient satisfaction, perception of health, emergency department (ED) visits, and use of preventive medications (aspirin and statins) by age category [Young: 18–44, Middle: 45–64, Older: ≥65 years]. We used two-part econometric modeling to evaluate age-specific annual healthcare expenditure.
Results
There were 21,353 participants included. Over 9000 (42.6%-weighted) of the participants were young or middle aged, representing ~9.9 million adults aged <65 years with ASCVD nationwide. Compared with older adults, middle-aged and young adults with ASCVD were more likely to report poor patient-clinician communication [OR 1.73 (95% CI 1.28–2.33) and 2.49 (1.76–3.51), respectively], poor healthcare satisfaction, and poor perception of health status, have increased ED utilization and were also less likely to be using aspirin and statins. The mean annual healthcare expenditure was highest among middle-aged adults [$10,798 (95% CI, $10,012 to $11,583)].
Conclusion
Compared with older adults, younger adults with ASCVD were more likely to report poor patient experience and poor health status and less likely to be using preventive medications. More effort needs to be geared towards understanding the age-specific differences in healthcare quality and delivery to improve outcomes among high-risk young adults with ASCVD.
Keywords: Communication, Satisfaction, Age-differences, Statin use, Aspirin use, Healthcare expenditure, Atherosclerotic cardiovascular disease
Highlights
-
1
In a sample of US adults with ASCVD we compared young & middle-age to older adults.
-
2
Young adults were more likely to report poor healthcare communication & satisfaction.
-
3
Young adults at a higher risk for depression and have poorer health perception.
-
4
Young adults with ASCVD were less likely to be using aspirin and statins.
-
5
More effort needed to understanding age-specific differences in patient experience.
1. Introduction
Although advanced age is the most significant risk factor for atherosclerotic cardiovascular disease (ASCVD), the prevalence of ASCVD in younger adults has increased over the past decade [1,2]. Despite the overall decrease in mortality from ASCVD in the United States (U.S.) over the last few decades, this trend has not been seen in younger adults [[3], [4], [5], [6]]. Hospitalizations from acute myocardial infarction (MI) among younger adults have not declined [7], and an increase in cardiometabolic risk factors has been suggested to contribute to the growing incidence of ASCVD in the younger population [1,7,8]. Furthermore, young adults with ASCVD are at high risk of recurrent cardiovascular events and require aggressive secondary prevention management, which is facilitated by good clinician-patient partnerships in optimizing health care delivery [9,10].
Even though age is thought to influence an individual’s perception about healthcare communication [11], it is less well established whether patient reported outcomes (PROs) differ between younger and older adults with established ASCVD. This provides an opportunity for more research and intervention among this understudied population. In this study, we used a nationally representative dataset to compare age-specific differences in PROs among individuals with ASCVD.
2. Methods
2.1. Study design and sampling
The Medical Expenditure Panel Survey (MEPS) database was used to conduct this retrospective study. The MEPS is cosponsored by the Agency for Healthcare, Research and Quality (AHRQ) and the National Center for Health and Statistics [12]. It is released annually and contains nationally representative information on sociodemographic characteristics, medical conditions, prescribed medicines, healthcare expenditure, and payer sources in different data files, with every participant having a unique person identifier [[13], [14], [15]]. To account for survey non-response, person-weight and variance estimation stratum are assigned to each MEPS participant, as described elsewhere [12]. Further description of the MEPS is discussed in the Supplementary Online Brief.
To carry out this study, we merged three different yearly MEPS files: full-year consolidated data files (contains information on sociodemographic characteristics, health resource utilization and patient experience), medical conditions files (contains International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) diagnoses of medical conditions), and the prescription medication files, using a unique person identifier, to provide specific information on each respondent. Per the Department of Health and Human Services guidelines, this study was exempt from Institutional Review Board review because it was conducted using a de-identified publicly available dataset.
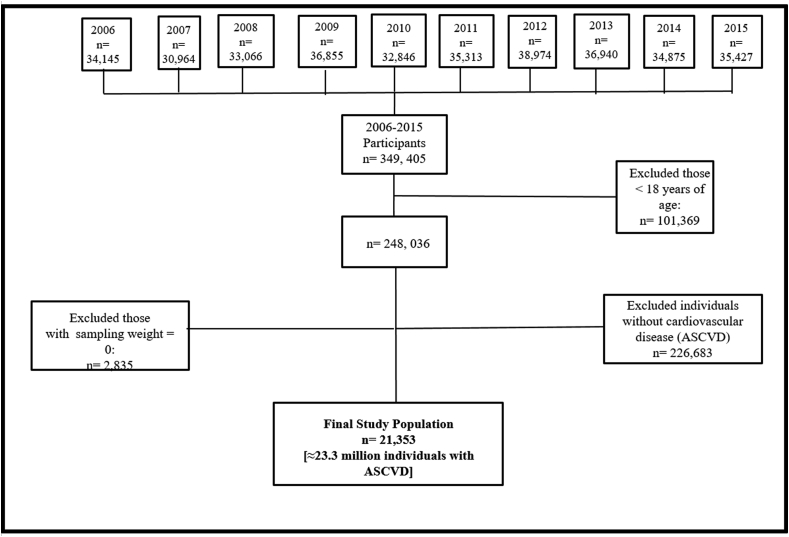
To generate more robust estimates, we pooled information from 2006 to 2015 MEPS data (Fig. 1) and included individuals ≥18 years of age with a diagnosis of ASCVD (coronary artery disease, stroke, and/or peripheral artery disease, ascertained by self-report or any of the following ICD-9-CM codes: 410, 413, 414, 433–437, 440 and 443, respectively) and had assigned weights, so as to generate nationally representative results.
Fig. 1.
Flow chart of the patient selection process, MEPS 2006–2015.
2.2. Study variables
2.2.1. Patient-clinician communication
Incorporated in the MEPS questionnaires is the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey, which assesses questions related to patient healthcare experience. As described in prior studies, we used the responses to the four communication-related questions recommended by the CAHPS consortium to evaluate patient-clinician communication (PCC): (a) How often health providers explained things in a way that was easy to understand? (b) How often providers showed respect for what you had to say? (c) How often providers spent enough time with you? (d) How often providers listened carefully to you? [[16], [17], [18]]
Using a 4-point Likert scale system, the responses were graded as: 1-never, 2-sometimes, 3-usually, and 4-always. As recommended by the CAHPS group, we combined “never” and “sometimes” responses into a single variable “never/sometimes” [16]. Hence, the responses were relabeled as 1-never/sometimes, 2-usually, and 3-always (Supplemental eTable 1). These responses were totaled to give a communication score ranging from 4 to 12 and a weighted average response from 1 to 3 was generated, labeled as 1 - “Poor PCC”, 2 - “Average PCC”, 3 - “Optimal PCC”. Subsequently, “Average” and “Optimal” PCC were combined to yield a binary variable (Poor PCC vs. Average/Optimal PCC), with poor PCC being the outcome of interest. Similar methodology have been used in prior studies [13,[17], [18], [19]].
2.2.2. Patient satisfaction
The question “Rating of healthcare from all doctors and other health providers”, from the MEPS questionnaire was used to assess patient satisfaction with healthcare. It is graded from 0 (worst health care possible) to 10 (best health care possible). As shown in prior studies, this variable was classified into two categories: “Poor Patient Satisfaction” (scores ≥0 to ≤3) or “Excellent/Good Patient Satisfaction” (scores ≥4 to ≤10), with poor patient satisfaction as the outcome of interest [13].
2.2.3. Secondary preventive medication usage
Aspirin and statin therapy have a well-established role for the secondary prevention of ASCVD. The variation in reporting of medication usage across the various age brackets was used as a quality of care indicator [13]. Information such as prescribed medicines, and pharmacy/drug stores from which these medications were obtained were collected from the MEPS respondents. With the consent of the MEPS participants, the collected information was verified and additional information on medications, were collected from the drug stores and pharmacies [17]. This information is available in the MEPS Prescribed Medicine Files [12]. Statins were coded as 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors and lipid lowering medications containing a 3-hydroxy-3-methylglutaryl coenzyme A agent [13,17]. For aspirin usage, an individual’s response (Yes/No) to the question: “does the person take aspirin frequently?” was used [13].
2.2.4. Perception of health status
MEPS participants were asked to evaluate their general health, with the responses provided on a 5-point Likert scale: 1-excellent, 2-very good, 3-good, 4-fair, and 5-poor. We divided these responses to give a binary variable: fair and poor responses combined as a single variable labeled as “Poor”, and excellent, very good and good responses combined and labeled as “Good. “Poor” perception of general health was used as the outcome of interest.
2.2.5. Depression risk
We also evaluated risk for depression among study participants without a diagnosis of depression (ICD-9 code 311). We used the responses to the questions on the Patient Health Questionnaire-2 scale to assess an individual’s risk of depression. The MEPS provides a summary of the PHQ-2, with responses on a scale ranging from 0 to 6, where higher values indicate an increased risk for depression [18]. As in prior studies, we used a cut of >3 to signify a high risk for depression [18]. See Supplemental Online eMethods for details.
2.2.6. Healthcare expenditure and ED utilization
The MEPS full year consolidated file contains information on the total number of Emergency Department (ED) visits per survey year. As described in prior studies, we used two or more ED visits per survey year as a measure of increased ED utilization [13,17,18].
To obtain an estimate of the annual healthcare expenditure, MEPS participants reported their yearly incurred medical expenditures, which included amounts spent on health services and prescription medication filled within the year. This information is available in the MEPS full year consolidated file. Total, as well as out-of-pocket, expenditures were calculated and reported for each participant. Payment source and amount contributed were also confirmed by follow-up surveys with healthcare professionals and pharmacies [20]. Data on healthcare expenses were adjusted using the gross domestic product (GDP) deflator to adjust yearly expenditures from 2004 to 2015 to constant 2015 U S. dollars [14,15,20].
2.2.7. Age group and other covariates
We used the respondents’ age as the primary predictor variable. Participant age was grouped into 3 categories [Young adults: 18–44, Middle-aged adults: 45–64, Older adults: ≥65 years]. Other variables included in this study include level of income, sex, race/ethnicity, insurance status, education, region, marital status, employment status, comorbid conditions, and cardiovascular risk factors. See Supplemental Online eMethods for details.
Comorbid conditions were estimated using the standardized Charlson comorbidity index, which was modified to exclude the cardiovascular component. Details have been described elsewhere [21,22]. Cardiovascular risk factor profile was determined based on the number of unfavorable risk factors an individual possesses, with higher number of risk factors representing a poor cardiovascular risk factor profile (Supplemental eTable 2).
We also looked at the 10-year trend of the proportion of individuals with ASCVD, stratified by age categories. For ease of analysis, we combined 2 years into cycles: 2006–2007, 2008–2009, 2010–2011, 2012–2013, and 2014–2015 (Supplemental Fig. 1).
2.3. Statistical analysis
Stata®, version 13.1 (StataCorp, LP, College Station, Texas, USA), was used for all statistical analyses with a p value of <0.05 considered statistically significant. Chi-square test was used to examine the differences in the demographic characteristics of the study population. Logistic regression models were applied for all binary outcomes, with age group of the respondents as the primary predictor. In all logistic regression models, we accounted for sex, race/ethnicity, region, level of income, level of education, health insurance, comorbid conditions and cardiovascular risk factors.
To analyze cost data, we used the two-part econometric model because healthcare expenditures are mostly right skewed (i.e. the bulk of expenditures is incurred by only a small proportion of the population) [23]. Two-part models are the product of the probability that any given individual had any expenditure, and their mean expenditures [24,25]. The distribution of the glm was determined using the modified park test which is typically employed in analyzing cost data to select the most appropriate modeling method [26].
3. Results
3.1. Sample characteristics
The study sample consisted of 21,353 MEPS participants from 2006 to 2015, which represents 23.3 million U.S. adults with ASCVD (mean [SD] age, 64 [14.7] years) (Fig. 1). The sociodemographic characteristics of the study population are described in Table 1. Overall, 57.4% of the population were ≥65 years, 34.6% between 45 and 64 years of age and 8.0% of the participants were between the ages of 18–44 years. Over 42% of U.S. adults with ASCVD are young and middle-aged, which translates into 9.9 million non-elderly U.S. adults with ASCVD. The majority of older adults with ASCVD in the study population were males (52% men), non-Hispanic white (83%), of higher socioeconomic strata (62% high or middle income), insured (primarily Medicare) and lived in the southern region of the country (Table 1). In contrast, young adult patients were about 60% non-Hispanic whites, 44% high or middle income, and 51.5% insured.
Table 1.
Weighted sample characteristics of non-institutionalized US adults aged ≥18 years with ASCVD, categorized by age group, MEPS 2006–2015.
| Older adults (≥65 yrs) | Middle-aged adults (45–64 yrs) | Young adults (18–44yrs) | P-value | |
|---|---|---|---|---|
| N = 21,353 | 12,257 (57.4%) | 7388 (34.6%) | 1708 (8.0%) | |
| Weighted sample = 23,277,253 | ||||
| Level of income (%) | <0.001 | |||
| High income | 32.3 | 34.8 | 19.9 | |
| Middle income | 30.4 | 27.3 | 29.0 | |
| Low income | 19.4 | 13.3 | 16.4 | |
| Very low income | 17.9 | 24.6 | 34.7 | |
| Sex (%) | <0.001 | |||
| Female | 48.1 | 44.0 | 51.5 | |
| Male | 51.9 | 56.0 | 48.5 | |
| Race/Ethnicity (%) | <0.001 | |||
| Non-Hispanic Whites | 82.6 | 71.9 | 60.4 | |
| African Americans/Blacks | 8.4 | 14.8 | 16.8 | |
| Asians | 2.4 | 2.6 | 1.8 | |
| Hispanics | 6.6 | 10.7 | 21.0 | |
| Insurance status (%) | <0.001 | |||
| Uninsured | 0.3 | 59.6 | 48.5 | |
| Private | 0.3 | 12.2 | 21.5 | |
| Medicaid | 3.1 | 21.8 | 26.5 | |
| Medicare | 99.3 | 6.4 | 34.5 | |
| Education (%) | 0.002 | |||
| Less than high school | 27.2 | 23.3 | 23.9 | |
| High school/GED | 50.0 | 51.6 | 53.6 | |
| Some college or Higher | 22.8 | 25.1 | 22.5 | |
| Marital status (%) | <0.001 | |||
| Married | 53.2 | 58.7 | 41.1 | |
| Widowed | 30.9 | 5.4 | 0.9 | |
| Divorced | 11.4 | 21.2 | 15.1 | |
| Separated | 1.1 | 4.3 | 6.1 | |
| Never married | 3.4 | 10.4 | 36.8 | |
| Region (%) | <0.001 | |||
| Northeast | 19.7 | 16.6 | 17.3 | |
| Midwest | 22.5 | 23.1 | 23.0 | |
| South | 38.3 | 42.7 | 41.9 | |
| West | 19.5 | 17.6 | 17.8 | |
While the proportion of older adults with ASCVD remained stable at about 58% over the study period, the proportion of young adults with ASCVD increased from 5.5% in 2006–2007 to 8.5% in 2014–2015, although the increase was not statistically significant (p for trend = 0.49) (Supplemental Fig. 1).
3.2. Patient experience
Compared with older adults with ASCVD, middle-aged and young adults were more likely to report poor communication with their clinicians [middle-aged adults: (adjusted OR 1.73, 95% CI 1.28–2.33), young adults: (adjusted OR 2.49, 95% CI 1.76–3.51)] (Table 2).
Table 2.
Patient reported outcomes among individuals with ASCVD, based on age group, MEPS 2006–2015.
| Older adults (≥65 yrs) | Middle-aged adults (45–64 yrs) | Young adults (18–44yrs) | |
|---|---|---|---|
| Patient Healthcare Experience | |||
| Proportion with poor patient-clinician communication (p < 0.001) | 9.7% | 17.6% | 23.7% |
| Poor patient-clinician communication (OR, 95%CI) | Ref | 1.73 (1.28–2.33) | 2.49 (1.76–3.51) |
| Proportion with poor patient satisfaction (p < 0.001) | 17.6% | 30.2% | 36.7% |
| Poor patient satisfaction (OR, 95%CI) | Ref | 1.73 (1.36–2.19) | 2.19 (1.63–2.95) |
| Patient perception of General Health | |||
| Proportion with poor perception of health (p < 0.001) | 31.7% | 43.7% | 33.8% |
| Poor perceived health status (OR, 95%CI) | Ref | 4.57 (3.43–6.09) | 3.35 (2.39–4.67) |
| Proportion with high risk for depression (p < 0.001) | 6.7% | 10.5% | 11.9% |
| ∗∗High risk for depression (OR, 95%CI) | Ref | 2.77 (1.96–3.92) | 3.34 (2.23–5.00) |
| Medication Usage | |||
| Proportion not on a statin (p < 0.001) | 37.4% | 48% | 80.9% |
| Not on a Statin (OR, 95%CI) | Ref | 1.64 (1.25–2.17) | 5.39 (3.84–7.59) |
| Proportion not on aspirin (p < 0.001) | 32.3% | 39.1% | 74.8% |
| Not on Aspirin (OR, 95%CI) | Ref | 1.57 (1.24–1.98) | 5.78 (4.38–7.62) |
| Emergency Department Utilization | |||
| Proportion with 2 or more ED visits/year (p = 0.02) | 9.6% | 10.4% | 12.1% |
| 2 or more ED visits/year (OR, 95%CI) | Ref | 1.57 (1.16–2.12) | 2.20 (1.55–3.14) |
| Annual Healthcare expenditure | |||
| US dollars (95% CI)] | US dollars (95% CI)] | US dollars (95% CI)] | |
| Adjusted mean annual healthcare expenditures | $9435 (8257 to 10,611) | $10,798 (10,012 to 11,583) | $8000 (6717 to 9282) |
∗Odds ratios (OR) were adjusted for income level, race, sex, region, health insurance, educational status, modified Charlson comorbidity index (without the cardiovascular component), cardiovascular risk factors.
∗∗Depression risk among US adults with ASCVD, without a diagnosis of depression.
Abbreviations; CI, confidence interval; ASCVD, atherosclerotic cardiovascular disease; ED, Emergency Department.
Middle-aged adults with ASCVD had a 1.73 times higher adjusted odds of reporting poor satisfaction with healthcare received, when compared with older adults (OR 1.73, 95% CI 1.36–2.19). Younger adults were over two times more likely to report dissatisfaction with the overall healthcare received when compared with older adults (OR 2.19, 95% CI 1.63–2.95) (Table 2).
The Supplemental eTable 3 shows the different components of PCC and the proportion of respondents dissatisfied with their PCC, by age groups. While 7.9% of U.S. older adults with ASCVD report that their clinicians did not spend enough time with them, a much higher proportion (20.5%) of younger adults with ASCVD reported the same. Similarly, a higher proportion of younger adults with ASCVD report that their clinicians never or only sometimes listen to what they had to say (5.7% for U.S. adults ≥65 years vs. 16.9% of U.S. adults 18–44 years).
Although the focus in this study was on individuals with ASCVD, in Supplemental eTable 4, we show PCC and patient satisfaction among individuals without ASCVD, based on age category, for comparison with the ASCVD population. Younger individuals in the general population also report poor PCC and were more likely to be dissatisfied with their healthcare services, when compared with older adults.
3.3. Patient perception of health and depression risk
Age was also significantly associated with an individual’s perception of their health status among patients with ASCVD. Compared with older adults, middle-aged adults were over 4 times more likely to perceive their general health as being poor (OR 4.57, 95% CI 3.43–6.09). Young adults also had higher odds of perceiving their health status as being poor, when compared with older adults (OR 3.35, 95% CI 2.39–4.67) (Table 2).
Risk for depression (among individuals with ASCVD who were without a diagnosis of depression) was higher at younger ages. Compared with older adults, the middle-aged and young adults were ~2.8 times (OR 2.77, 95% CI 1.96–3.92) and ~3.3 times (OR 3.34, 95% CI 2.23–5.00) more likely to be at a high risk for depression, respectively (Table 2).
3.4. Medication usage, ED utilization & healthcare expenditure
Statin and aspirin use were used as a measure of adherence to guideline directed medical therapy for secondary prevention among individuals with ASCVD. Compared with adults ≥65 years, those between the ages of 45–64 years had higher odds of not using a statin (OR 1.64, 95% CI 1.25–2.17). Adults aged 18–44 years were over 5 times more likely to not be using a statin (OR 5.39, 95% CI 3.84–7.59), when compared with adults ≥65 years. Similarly, younger participants with ASCVD had higher odds of not using aspirin when compared with their older counterparts; middle-aged adults (OR 1.57, 95% CI 1.24–1.98), young adults (OR 5.78, 95% CI 4.38–7.62) (Table 2).
Young and middle-aged adults with ASCVD had increased ED utilization, when compared with older adults. Those aged 45–64 years were ~1.5 times more likely to utilize the ED 2 or more times/year when compared with adults ≥65 years (OR 1.57, 95% CI 1.16–2.12). Young adults had over 2-fold higher odds of two or more ED visits per year, when compared with older adults (OR 2.20, 95% CI 1.55–3.14) (Table 2).
Among these adults with ASCVD, the mean annual healthcare expenditure was highest among middle-aged adults [$10,798 (95% CI, $10,012 to $11,583)] and lowest among young adults [$8000 (95% CI, $6717 to $9282)]. Older adults had an average annual healthcare expenditure of $9435 (95% CI, $8257 to $10,611) (Table 2).
Sex and race appeared to modify the effect of age on some of the PROs among U.S. adults with ASCVD. We therefore stratified by these variables as displayed in (Supplementary eTables 5-10). Compared with women 65 years and older with ASCVD, young women 18–44 years were more likely to report poor healthcare satisfaction (OR 1.84, 95% CI 1.22–2.78), were at a higher risk for depression (OR 3.09, 95% CI 1.60–5.97), and more likely to report not using a statin (OR 4.98, 95% CI 3.10–8.01) or aspirin (OR 5.37, 95% CI 3.55–8.13) (eTable 5). Among Black adults, compared with individuals ≥65 years with ASCVD, those 18–44 years were more likely to report not using a statin (OR 7.34, 95% CI 4.09–13.18) or aspirin (OR 4.28, 95% CI 2.65–6.92) (eTable 8).
4. Discussion
In this study, which was nationally representative of over 23 million U.S. adults with ASCVD, we found that young and middle-aged adults with ASCVD were more likely to report poor PCC, poor satisfaction, and were at a higher risk for depression when compared with older adults [Fig. 2]. They were also more likely to report under-utilization of guideline directed medical therapy for secondary prevention, poorer perception of health, and higher ED utilization. Annual healthcare expenditure was highest among the middle-aged population with ASCVD.
Fig. 2.
Age specific differences in patient reported outcomes among US adults with ASCVD, Medical Expenditure Panel Survey 2006–2015 (reference group – older adults).
Optimal patient experience is important in promoting patient-centered care. Patient-clinician communication and patient satisfaction are important pillars of patient experience and studies have shown the association between optimal patient experience and improved health outcomes [13,17,19]. It has been suggested that individuals <65 years were less likely to report adequate and effective communication with their clinicians when compared with those ≥65 years [11]. In our study, we focused on individuals with established ASCVD, who warrant aggressive secondary prevention management to reduce their residual risk, where effective communication is perhaps even more critical than in the primary prevention setting. However in supplemental analysis, we report similar age-related disparities in the general non-ASCVD population, as had been noted in other studies [11]. This current study showed that young and middle-aged adults with ASCVD were more likely to be dissatisfied and report poor PCC when compared with older adults.
It is unclear how exactly age influences patient experience. Optimizing PCC and patient satisfaction may not entirely be within the sphere of influence of the healthcare system. This current study showed a higher proportion of younger adults reporting dissatisfaction with their PCC in terms of being listened to, showing respect to what they had to say, spending enough time with them and explaining things in ways easy enough for them to understand, when compared with older adults with ASCVD. The patient’s social, behavioral and psychological condition may affect the evaluation of their patient experience. We speculate that these matrices rely heavily on patient expectations of what their healthcare experience should be like and patient perceptions of the care and attention they have received from their clinicians, which may differ by age [11,27]. For example, older patients may be more tolerant of the inadequacies of the healthcare delivery process, given their familiarity with the system over time and also the long standing relationships and interaction they might have had with their clinicians.
On the other hand, younger patients, who might be more likely to focus on the ease and promptness of healthcare access, wait time, and their involvement in the health decision making process, might be less pleased with any short-comings of the healthcare delivery process [11]. Older patients with ASCVD may also require more comprehensive care, by virtue of having a protracted past medical history and other comorbidities, hence influencing the clinician’s approach during health encounters and the amount of time spent with patients in clinic visits. Societal norms and expectations that clinicians will pay more attention to older adults could also be playing a role in the age-specific differences noted in patient experience.
Statins and aspirin are guideline directed medical therapy indicated for secondary prevention among individuals with ASCVD. Evidence on the association between age and medication compliance among adults with chronic medical conditions have been conflicting [[28], [29], [30]]. This current study shows that older adults with ASCVD are more likely to report statin and aspirin use, when compared with their younger counterparts. It is possible that while younger patients may be in denial pertaining to their medical condition, older patients with ASCVD are more likely to have accepted their diagnoses, hence be more willing to comply with suggested medical therapies. Alternatively, clinicians may not treat younger adults as aggressively with preventive strategies due to perceived lower risk, as has been shown in general populations [31,32]; although all patients in our sample had established ASCVD with a class I indication for both aspirin and statins.
Self-perception of health has been shown to be highly correlated with an individual’s sense of well-being and overall life satisfaction and less so with health-related factors [33,34]. Among the general population, it is suggested that older adults were more likely to describe their overall health as being poor [35]. Decline in physical activity, comorbid conditions and quality of life are factors that might explain this association noted among the aging population. In this study, after adjusting for sociodemographic factors and comorbid conditions, we found young and middle-aged adults with ASCVD were more likely to perceive their health as being poor, when compared with older adults. The discrepancy in our findings versus prior studies may be due to the study population, as the current study included only individuals with ASCVD. A young individual diagnosed with a disease largely attributable to aging may perceive his or her health as being very poor, compared with an older adult. Furthermore, an individual’s view of their health compared to that of their peers within the same age group probably influences the self-rating of their health. This could also explain the higher risk of depression among younger adults with ASCVD, demonstrated in this study.
We demonstrated an increased ED utilization among young and middle-aged adults with ASCVD compared with older adults. The lower ED utilization observed among older adults with ASCVD could be a result of higher medication compliance, and better patient experience which would also encourage more routine outpatient follow up visits in older vs. younger adults, hence reducing the risk and frequency of cardiovascular emergencies.
Cardiovascular disease is one of the major contributors to the significant healthcare expenditure noted among U.S. adults. The distribution of healthcare cost is age dependent with most healthcare spending occurring in middle-aged and older adults [36]. This is similar to what we found in our study showing higher annual average expenditures among older and middle-aged adults, with young adults with ASCVD contributing the least to healthcare spending annually. Some factors influencing higher healthcare expenditure among middle-aged and older adults include greater number of comorbid conditions, longer hospital stays, increasing long-term care and disease complications with age [37].
4.1. Strengths and limitations
Given the cross sectional design of the MEPS, causality cannot be established between age and health outcomes among individuals with ASCVD. We defined ASCVD to include ICD-9 and self-reported diagnosis; hence, there is a risk of under-estimation of the actual burden of ASCVD. Also, there are many other factors that might be contributing to the age-specific differences in patient reported outcomes among adults with ASCVD that we could not account for such as no-show rates, age of diagnosis, duration of relationship between the clinician and the patient, and contraindications to medical therapy. Furthermore, there are significant differences between the young and older ASCVD population in terms type of insurance, level of income, and racial composition. Although we adjusted for these variables in the regression analyses, these sociodemographic differences could also be markers of unmeasured confounders that we could not account for. Finally, some conditions such as hemorrhagic stroke may not warrant the uses of medications such as aspirin. Although we could not account for the types of stroke in the study or other conditions like carotid artery dissection, when we restricted the analyses to only individuals with MI, younger individuals with MI were much more likely to report not being on a statin or aspirin when compared with older adults with MI.
However, this study also has many strengths, including the overlapping survey design of the MEPS, the multi-level approach to verification of obtained information, and the application of weights making the results obtained from this study generalizable to U.S. non-institutionalized civilian adults living with ASCVD.
5. Conclusions
Compared with older adults, young and middle-aged adults with ASCVD were more likely to report poorer patient experience and perception of their health, less likely to be using established secondary prevention medications, were at an increased risk for depression, and had higher ED utilization. More effort needs to be geared towards understanding the age-specific differences in healthcare quality and delivery to improve health outcomes among younger individuals with ASCVD.
Disclosures
None of the authors reported any conflicts of interest.
Funding
Dr. Michos is supported by the Blumenthal Scholars Fund for Preventive Cardiology at Johns Hopkins.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajpc.2020.100083.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Virani S.S., Alonso A., Benjamin E.J., Bittencourt M.S., Callaway C.W., Carson A.P. Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Robinson J.G., Gidding S.S. Curing atherosclerosis should be the next major cardiovascular prevention goal. J Am Coll Cardiol. 2014;63(25 Pt A):2779–2785. doi: 10.1016/j.jacc.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 3.Wilmot K.A., O’Flaherty M., Capewell S., Ford E.S., Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation. 2015;132(11):997–1002. doi: 10.1161/CIRCULATIONAHA.115.015293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta A., Wang Y., Spertus J.A., Geda M., Lorenze N., Nkonde-Price C. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64(4):337–345. doi: 10.1016/j.jacc.2014.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khan SU, Bashir ZS, Khan MZ, Khan MS, Gulati M, Blankstein R. Trends in Cardiovascular Deaths Among Young Adults in the United States, 1999 to 2018. Am J Cardiol. 2020;128:216–217. doi: 10.1016/j.amjcard.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtin S.C. Trends in cancer and heart disease death rates among adults aged 45–64: United States, 1999–2017. Natl Vital Stat Rep. 2019;68(6):1–8. [PubMed] [Google Scholar]
- 7.Arora S., Stouffer G.A., Kucharska-Newton A.M., Qamar A., Vaduganathan M., Pandey A. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139(8):1047–1056. doi: 10.1161/CIRCULATIONAHA.118.037137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang J., Biery D.W., Singh A., Divakaran S., DeFilippis E.M., Wu W.Y. Risk factors and outcomes of very young adults who experience myocardial infarction: the partners YOUNG-MI registry. Am J Med. 2020;133(5):605–612. doi: 10.1016/j.amjmed.2019.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collet J.P., Zeitouni M., Procopi N., Hulot J.S., Silvain J., Kerneis M. Long-term evolution of premature coronary artery disease. J Am Coll Cardiol. 2019;74(15):1868–1878. doi: 10.1016/j.jacc.2019.08.1002. [DOI] [PubMed] [Google Scholar]
- 10.Michos E.D., Choi A.D. Coronary artery disease in young adults: a hard lesson but a good teacher. J Am Coll Cardiol. 2019;74(15):1879–1882. doi: 10.1016/j.jacc.2019.08.1023. [DOI] [PubMed] [Google Scholar]
- 11.DeVoe J.E., Wallace L.S., Fryer G.E., Jr. Patient age influences perceptions about health care communication. Fam Med. 2009;41(2):126–133. [PMC free article] [PubMed] [Google Scholar]
- 12.Medical Expenditure Panel Survey 2019. http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp Retrieved July 20th.
- 13.Okunrintemi V., Valero-Elizondo J., Patrick B., Salami J., Tibuakuu M., Ahmad S. Gender differences in patient-reported outcomes among adults with atherosclerotic cardiovascular disease. J Am Heart Assoc. 2018;7(24) doi: 10.1161/JAHA.118.010498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okunrintemi V., Benson E.A., Tibuakuu M., Zhao D., Ogunmoroti O., Valero-Elizondo J. Trends and costs associated with suboptimal physical activity among US women with cardiovascular disease. JAMA Netw Open. 2019;2(4) doi: 10.1001/jamanetworkopen.2019.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tibuakuu M., Okunrintemi V., Jirru E., Echouffo Tcheugui J.B., Orimoloye O.A., Mehta P.K. National trends in cessation counseling, prescription medication use, and associated costs among US adult cigarette smokers. JAMA Netw Open. 2019;2(5) doi: 10.1001/jamanetworkopen.2019.4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hardee J.T., Kasper I.K. A clinical communication strategy to enhance effectiveness and CAHPS scores: the ALERT model. Perm J. 2008;12(3):70–74. doi: 10.7812/tpp/07-066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okunrintemi V., Spatz E.S., Di Capua P., Salami J.A., Valero-Elizondo J., Warraich H. Patient-provider communication and health outcomes among individuals with atherosclerotic cardiovascular disease in the United States: medical expenditure panel survey 2010 to 2013. Circ Cardiovasc Qual Outcomes. 2017;10(4) doi: 10.1161/CIRCOUTCOMES.117.003635. [DOI] [PubMed] [Google Scholar]
- 18.Okunrintemi V., Valero-Elizondo J., Michos E.D., Salami J.A., Ogunmoroti O., Osondu C. Association of depression risk with patient experience, healthcare expenditure, and health resource utilization among adults with atherosclerotic cardiovascular disease. J Gen Intern Med. 2019;34(11):2427–2434. doi: 10.1007/s11606-019-05325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen Q., Beal E.W., Schneider E.B., Okunrintemi V., Zhang X.F., Pawlik T.M. Patient-provider communication and health outcomes among individuals with hepato-pancreato-biliary disease in the USA. J Gastrointest Surg. 2018;22(4):624–632. doi: 10.1007/s11605-017-3610-z. [DOI] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality MEPS-HC panel design and data collection process. https://meps.ahrq.gov/mepsweb/survey_comp/hc_data_collection.jsp
- 21.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.de Groot V., Beckerman H., Lankhorst G.J., Bouter L.M. How to measure comorbidity. a critical review of available methods. J Clin Epidemiol. 2003;56(3):221–229. doi: 10.1016/s0895-4356(02)00585-1. [DOI] [PubMed] [Google Scholar]
- 23.Mihaylova B., Briggs A., O’Hagan A., Thompson S.G. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20(8):897–916. doi: 10.1002/hec.1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Belotti F., Deb P., Manning W., Norton E. two pm: two-part models. STATA J. 2015;15(1):3–20. [Google Scholar]
- 25.Hardin J.W., Hilbe J. third ed. StataCorp LP; 2012. Generalized linear models and extensions. [Google Scholar]
- 26.Manning W.G., Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 27.DeVoe J.E., Wallace L.S., Fryer G.E., Jr. Measuring patients’ perceptions of communication with healthcare providers: do differences in demographic and socioeconomic characteristics matter? Health Expect. 2009;12(1):70–80. doi: 10.1111/j.1369-7625.2008.00516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smilowitz S., Aftab A., Aebi M., Levin J., Tatsuoka C., Sajatovic M. Age-related differences in medication adherence, symptoms, and stigma in poorly adherent adults with bipolar disorder. J Geriatr Psychiatr Neurol. 2019 doi: 10.1177/0891988719874116. 891988719874116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fernandez-Lazaro C.I., Garcia-Gonzalez J.M., Adams D.P., Fernandez-Lazaro D., Mielgo-Ayuso J., Caballero-Garcia A. Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study. BMC Fam Pract. 2019;20(1):132. doi: 10.1186/s12875-019-1019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nanna M.G., Navar A.M., Wang T.Y., Mi X., Virani S.S., Louie M.J. Statin use and adverse effects among adults >75 Years of age: insights from the patient and provider assessment of lipid management (PALM) registry. J Am Heart Assoc. 2018;7(10) doi: 10.1161/JAHA.118.008546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thanassoulis G., Williams K., Altobelli K.K., Pencina M.J., Cannon C.P., Sniderman A.D. Individualized statin benefit for determining statin eligibility in the primary prevention of cardiovascular disease. Circulation. 2016;133(16):1574–1581. doi: 10.1161/CIRCULATIONAHA.115.018383. [DOI] [PubMed] [Google Scholar]
- 32.Singh A., Collins B.L., Gupta A., Fatima A., Qamar A., Biery D. Cardiovascular risk and statin eligibility of young adults after an MI: partners YOUNG-MI registry. J Am Coll Cardiol. 2018;71(3):292–302. doi: 10.1016/j.jacc.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Osibogun O., Ogunmoroti O., Spatz E.S., Burke G.L., Michos E.D. Is self-rated health associated with ideal cardiovascular health? The Multi-Ethnic Study of Atherosclerosis. Clin Cardiol. 2018;41(9):1154–1163. doi: 10.1002/clc.22995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schneider G., Driesch G., Kruse A., Wachter M., Nehen H.G., Heuft G. What influences self-perception of health in the elderly? The role of objective health condition, subjective well-being and sense of coherence. Arch Gerontol Geriatr. 2004;39(3):227–237. doi: 10.1016/j.archger.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 35.Kaleta D., Polanska K., Dziankowska-Zaborszczyk E., Hanke W., Drygas W. Factors influencing self-perception of health status. Cent Eur J Publ Health. 2009;17(3):122–127. doi: 10.21101/cejph.b0017. [DOI] [PubMed] [Google Scholar]
- 36.Alemayehu B., Warner K.E. The lifetime distribution of health care costs. Health Serv Res. 2004;39(3):627–642. doi: 10.1111/j.1475-6773.2004.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang P., Imai K. The relationship between age and healthcare expenditure among persons with diabetes mellitus. Expet Opin Pharmacother. 2007;8(1):49–57. doi: 10.1517/14656566.8.1.49. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.