Abstract
Objective
To assess the prevalence, temporal trends and sex- and racial/ethnic differences in the burden of mental health disorders (MHD) and outcomes among patients with myocardial infarction (MI) in the United States.
Methods
Using the National Inpatient Sample Database, we evaluated a contemporary cohort of patients hospitalized for acute MI in the United States over 10 years period from 2008 to 2017. We used multivariable logistic regression analysis for in-hospital outcomes, yearly trends and estimated annual percent change (APC) in odds of MHD among MI patients.
Results
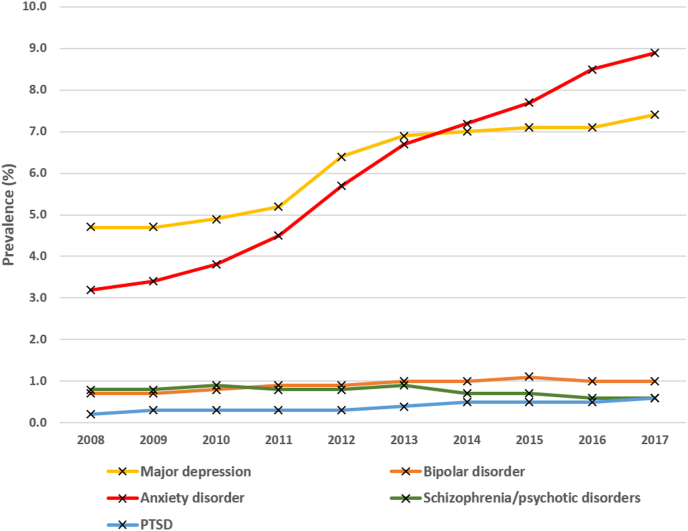
We included a total sample of 6,117,804 hospitalizations for MI (ST elevation MI in 30.4%), with a mean age of 67.2 ± 0.04 years and 39% females. Major depression (6.2%) and anxiety disorders (6.0%) were the most common MHD, followed by bipolar disorder (0.9%), schizophrenia/psychotic disorders (0.8%) and post-traumatic stress disorder (PTSD) (0.3%). Between 2008 and 2017, the prevalences significantly increased for major depression (4.7%–7.4%, APC +6.2%, p < .001), anxiety disorders (3.2%–8.9%, APC +13.5%, p < .001), PTSD (0.2%–0.6%, +12.5%, p < .001) and bipolar disorder (0.7%–1.0%, APC +4.0%, p < .001). Significant sex- and racial/ethnic-differences were also noted. Major depression, bipolar disorder or schizophrenia/psychotic disorders were associated with a lower likelihood of coronary revascularization.
Conclusion
MHD are common among patients with acute MI and there was a concerning increase in the prevalence of major depression, bipolar disorder, anxiety disorders and PTSD over this 10-year period. Focused mental health interventions are warranted to address the increasing burden of comorbid MHD among acute MI.
1. Introduction
Mental health is often given less priority in medicine, where the main focus is often on treating the disease rather than the whole patient [1]. The increasing evidence supporting the association of mental health disorders (MHD) and cardiovascular disease (CVD) has prompted the American Heart Association to include major depression and bipolar disorder as moderate-risk conditions associated with accelerated atherosclerosis and early CVD [2]. However, there is a paucity of data on the burden of MHD among patients with acute CVD.
Understanding sex- and racial/ethnic-differences and trends in the prevalence of MHD among patients presenting with acute CVD are necessary for healthcare teams and policymakers to identify vulnerable groups that need attention, and formulate appropriate strategies for comprehensive care to simultaneously address mind and body disorders to achieve better outcomes. In this study, we assessed the temporal trends and the sex- and racial/ethnic-differences in the prevalence of major forms of MHD, and the association of MHD and in-hospital outcomes among a contemporary cohort of patients hospitalized for acute myocardial infarction (MI) in the United States (US) over a decade from 2008 through 2017.
2. Methods
2.1. Data source
We utilized the National Inpatient Sample (NIS) developed by the Healthcare Cost and Utilization Project (HCUP) for this study [3]. We analyzed the most contemporarily available data for a period of 10 years from 2008 through 2017. More details about the NIS and data extraction are provided as Supplemental Methods. Institutional research board approval and informed patient consent for study participation were not required, as the NIS contains de-identified patient information that is publicly available for analysis.
2.2. Inclusion/exclusions and definitions
We included all adult (age ≥18 years) hospitalizations with a principal diagnosis of acute ST-elevation MI or non-ST elevation MI using appropriate International Classification of Diseases (ICD) diagnoses codes (eTable 1). Major depression, bipolar disorder, anxiety disorder, post-traumatic stress disorder (PTSD), and schizophrenia/psychotic disorders were the MHD included in this study. We assessed the average and yearly prevalence of comorbid diagnosis of MHD stratified by sex and race/ethnicity. The race/ethnicity groups included are Non-Hispanic Blacks (NHB), Non-Hispanic Whites (NHW), Hispanics, Asian or Pacific Islander (PI) and Native American (NA) [4].
2.3. Statistical analysis
All analyses were performed using STATA-16 (StataCorp, TX), and stratified weighted data were utilized to obtain nationwide estimates. Continuous variables were reported as mean with standard deviation and compared using the Student t-test, and the categorical variables were reported as proportions and compared using the Chi-square test. We used multiple logistic regression analysis for yearly trends with the year of admission as the independent variable along with specific MHD of interest as the dependent variable. The yearly prevalence of MHD was obtained using marginal effects following multiple regression analysis. The annual percent change (APC) in the Odds of the MHD was estimated as equal to (Odds ratio-1) x 100 and reported along with Ptrend to provide a quantitative estimation. Trends in the prevalence of various MHD between various subgroups of interest were compared using a subgroup-year interaction term in the regression model and reported as Pinteraction. Similarly, the yearly trends in coronary revascularization and in-hospital mortality were assessed.
We performed a further analysis with 3 falsification endpoints which are presumed to be unrelated to the primary outcome of temporal trends in the prevalence of MHD among acute MI hospitalizations to validate that the annual trends in MHD are not just because of better diagnostic coding strategies. The falsification endpoints assessed were the trends in the prevalence of hyperlipidemia, anemia and peripheral arterial disease among acute MI hospitalizations in the US over the same time period.
The association of various types of MHD and odds of coronary revascularization and in-hospital mortality were analyzed using multivariable logistic regression analysis adjusted for demographic (age, sex, race/ethnicity), social (income, rural residential location, insurance status), hospital characteristics (teaching hospital status, urban hospital location, bed size) and clinical characteristics (comorbidities including obesity, anemia, diabetes mellitus, hypertension, hyperlipidemia, chronic liver disease, chronic kidney disease, dialysis dependence, pulmonary vascular disease, chronic obstructive pulmonary disease, prior MI/coronary revascularization and prior stroke).
3. Results
3.1. Baseline characteristics
We included a total of 6,117,804 patients with MI hospitalization during 2008–2017 (STEMI 30.4%, NSTEMI 69.6%); the study sample had a mean age of 67.2 ± 0.04 years and 39% were females. The baseline demographic, clinical and hospital characteristics of the study population stratified by MHD are provided in Table 1.
Table 1.
Baseline characteristics of study population stratified by mental health disorders: the National Inpatient Sample of patients with acute myocardial infarction from 2008 to 2017.
| Patient characteristics | No mental health disorders (n = 4,088,062) | Mental health disorders |
∗p value | ||||
|---|---|---|---|---|---|---|---|
| Major depression (n = 269,641) | Bipolar disorder (n = 40,738) | Anxiety disorders (n = 358,885) | Schizophrenia and other psychotic disorders (n = 46,577) | Post-traumatic stress disorder (n = 18,168) | |||
| Mean age (years)±SD | 70.52 ± 0.1 | 67.6 ± 0.1 | 58.8 ± 0.1 | 65.1 ± 0.1 | 66.8 ± 0.2 | 59.7 ± 0.2 | <.001 |
| Female (%) | 40.0 | 53.2 | 45.2 | 56.0 | 43.2 | 21.2 | <.001 |
| Race | |||||||
| White (%) | 77.6 | 83.8 | 83.0 | 86.2 | 68.7 | 82.2 | <.001 |
| Black (%) | 10.7 | 8.1 | 11.2 | 6.2 | 21.5 | 11.4 | |
| Hispanic (%) | 8.7 | 6.7 | 5.0 | 6.5 | 7.9 | 5.2 | |
| Asian (%) | 3.0 | 1.3 | 0.8 | 1.1 | 1.8 | 1.2 | |
| Rural residential location (%) | 21.2 | 21.6 | 19.1 | 22.2 | 20.6 | 22.0 | <.001 |
| Type of insurance | |||||||
| Medicare (%) | 66.4 | 64.4 | 55.3 | 57.4 | 72.4 | 56.9 | <.001 |
| Medicaid (%) | 5.2 | 8.6 | 19.6 | 10.2 | 17.0 | 15.1 | |
| Private (%) | 24.7 | 23.0 | 18.9 | 27.3 | 7.9 | 23.0 | |
| Uninsured/self-paid (%) | 3.6 | 3.9 | 6.2 | 5.1 | 2.7 | 5.1 | |
| Teaching hospital (%) | 53.7 | 55.5 | 55.9 | 55.8 | 54.0 | 60.7 | <.001 |
| Urban hospital location (%) | 90.3 | 89.7 | 91.1 | 89.3 | 88.8 | 91.1 | <.001 |
| Income quartile for the residential ZIP code | |||||||
| 0-25th percentile | 28.1 | 28.6 | 34.3 | 30.5 | 39.2 | 31.4 | <.001 |
| 26th-50th percentile | 27.0 | 27.5 | 27.2 | 27.6 | 26.7 | 30.0 | |
| 51st-75th percentile | 24.0 | 24.3 | 22.1 | 23.4 | 20.4 | 24.2 | |
| 76th-100th percentile | 20.8 | 19.6 | 16.4 | 18.5 | 13.7 | 14.8 | |
| Anemia (%) | 3.0 | 3.4 | 2.6 | 2.9 | 3.4 | 2.5 | <.001 |
| Obesity (%) | 3.5 | 4.3 | 4.1 | 5.6 | 2.5 | 6.2 | <.001 |
| Diabetes mellitus (%) | 39.8 | 40.9 | 40.6 | 33.6 | 38.9 | 35.4 | <.001 |
| Hyperlipidemia (%) | 56.8 | 62.3 | 57.2 | 62.8 | 46.2 | 63.0 | <.001 |
| Hypertension (%) | 74.0 | 76.3 | 70.4 | 75.9 | 72.4 | 74.0 | <.001 |
| Liver disease (%) | 2.7 | 2.5 | 3.8 | 2.0 | 3.4 | 4.0 | <.001 |
| Chronic kidney disease (%) | 22.6 | 19.2 | 14.0 | 14.0 | 17.6 | 11.2 | <.001 |
| Hemodialysis dependence (%) | 0.6 | 0.5 | 0.3 | 0.4 | 0.4 | 0.2 | <.001 |
| Pulmonary vascular disease (%) | 4.9 | 4.2 | 3.0 | 3.8 | 4.2 | 2.8 | <.001 |
| COPD (%) | 18.8 | 26.5 | 30.9 | 27.9 | 29.4 | 29.1 | <.001 |
| Peripheral arterial disease (%) | 10.0 | 11.0 | 7.2 | 9.4 | 8.4 | 9.3 | <.001 |
| Dementia (%) | 1.9 | 2.9 | 1.9 | 2.1 | 3.9 | 1.1 | <.001 |
| Prior MI (%) | 10.4 | 11.8 | 11.6 | 11.4 | 9.2 | 13.9 | <.001 |
| Prior CABG (%) | 8.0 | 7.1 | 5.6 | 5.8 | 4.3 | 6.2 | <.001 |
| Prior PCI (%) | 11.4 | 11.4 | 11.4 | 10.9 | 6.9 | 12.6 | <.001 |
| Prior stroke (%) | 5.2 | 6.3 | 5.1 | 5.1 | 5.6 | 4.0 | <.001 |
| STEMI (%) | 28.1 | 24.6 | 28.0 | 24.1 | 24.9 | 26.8 | <.001 |
| NSTEMI (%) | 71.8 | 75.4 | 72.0 | 75.8 | 75.0 | 73.2 | <.001 |
| PCI (%) | 42.7 | 40.5 | 39.2 | 43.3 | 30.5 | 42.8 | <.001 |
| CABG (%) | 8.6 | 6.1 | 5.7 | 7.2 | 7.1 | 9.8 | <.001 |
| Duration of hospitalization (days) ± SD | 4.94 ± 0.02 | 4.46 ± 0.02 | 4.47 ± 0.06 | 4.09 ± 0.02 | 5.7 ± 0.1 | 4.0 ± 0.1 | <.001 |
Abbreviations: CABG: coronary artery bypass grafting; COPD: chronic obstructive pulmonary disease; NSTEMI: non-ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction; SD: standard deviation.
∗p-value represents the comparison of the distribution of various demographic variables and other medical comorbidities among the study population stratified by the presence of various mental health disorders.
3.2. The overall prevalence and temporal trends of various types of MHD
Over the 10-year study period, major depression (6.2%) and anxiety disorder (6.0%) were the most common MHD, followed by bipolar disorder (0.9%), schizophrenia/psychotic disorders (0.8%) and PTSD (0.3%). From 2008 to 2017, the prevalences significantly increased for major depression (4.7%–7.4%, APC +6.2%), anxiety (3.2%–8.9%, APC +13.5%), PTSD (0.2%–0.6%, +12.5%) and bipolar disorder (0.7%–1.0%, APC +4.0%), while the schizophrenia/psychotic disorders showed a downtrend (0.8%–0.6%, APC -2.6%) (Fig. 1, eTable 2). These findings were further substantiated with the stable trends in the prevalence of specific falsification endpoints during the same period of study [hyperlipidemia (58.0%–59.0%, APC +2.5%, p = 0.1), anemia (2.8%–2.8%, APC -0.01%, p = 0.2) and peripheral arterial disease (9.8%–9.6%, APC -0.02, p = 0.1) (eFigure 1, eTable 2)].
Fig. 1.
Temporal trends in the prevalence of mental health disorders among patients with acute myocardial infarction.
Figure shows the trends in the yearly prevalence of major depression, bipolar disorder, anxiety disorders, schizophrenia/psychotic disorders and PTSD from 2008-2017 among patients hospitalized with acute MI.
Abbreviations: PTSD = post-traumatic stress disorder
3.3. Sex differences
All categories of MHD were more prevalent among females compared to males except PTSD which was more prevalent among males (eFigure 2, A-B, eTable 3). The prevalence of major depression and anxiety disorders showed a larger increase among females compared to males, whereas the prevalence of bipolar disorder and PTSD increased among both sexes similarly (eFigure 2, A-B, eTable 3). While the females experienced a decline in the prevalence of schizophrenia/psychotic disorders it did not change significantly among males (eFigure 2, A-B, eTable 3).
3.4. Racial/ethnic differences
The prevalence of major depression was largest among NHW; however, the largest increase was seen among NA (eFigure 3, A-E, eTable 4). Bipolar disorder was more common among NHW and NHB with a steady increase in the prevalence across the study period. Anxiety disorders were most common among NHW with all races having a significant increase in the prevalence of anxiety disorders with the largest increase among NHB. The NHB groups had the highest overall prevalence of schizophrenia/psychotic disorders (1.5%) whereas PTSD was most common among NA (0.5%); however, NHB groups had the largest increase in the prevalence of PTSD among all races (0.1%–0.5%, APC +18.5%, p < .001) (eFigure 3, A-E, eTable 4).
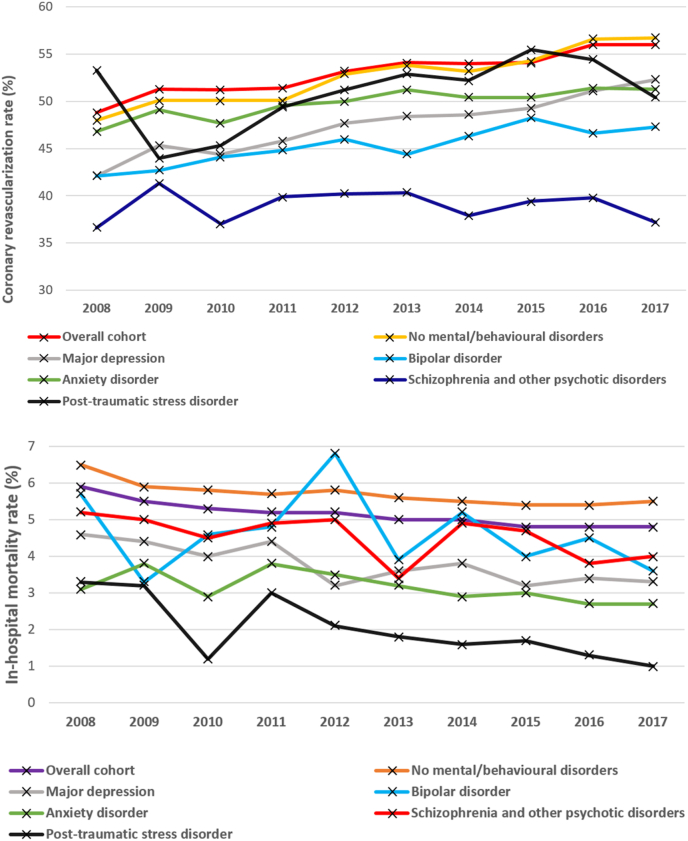
3.5. MHD and index hospital coronary revascularization
Patients with schizophrenia/psychotic disorders had the lowest average coronary revascularization rate (37.6%) (Table 2) (Fig. 2A). Over the study period, the coronary revascularization rate increased across all categories of MHD except among patients with schizophrenia/psychotic disorders and PTSD (eTable 5). In adjusted analyses, a comorbid diagnosis of major depression [adjusted OR 0.80 (95% confidence interval (CI) 0.72–0.88)], bipolar disorder [0.69 (0.65–0.72)] and schizophrenia/psychotic disorders [0.50 (0.47–0.52)] were significantly associated with lower odds of coronary revascularization for acute MI compared to those without any MHD (Table 2). These findings were consistent in age-stratified regression analysis (eTable 6).
Table 2.
Multivariable-adjusted logistic regression analysis of the association of mental health disorders and coronary revascularization and in-hospital mortality among acute myocardial infarction patients from 2008 to 2017 in United States.
| In-hospital mortality |
|||||||
|---|---|---|---|---|---|---|---|
| Overall, % | Unadjusted OR | 95% CI | p value | ∗Adjusted OR | 95% CI | p value | |
| No mental health disorders | 6.4 | Ref | ref | ref | ref | ref | ref |
| Major depression | 3.4 | 0.56 | 0.54–0.59 | <.001 | 0.64 | 0.61–0.67 | <.001 |
| Bipolar disorder | 4.3 | 0.47 | 0.41–0.53 | <.001 | 0.68 | 0.59–0.78 | <.001 |
| Anxiety disorders | 2.6 | 0.39 | 0.37–0.41 | <.001 | 0.50 | 0.48–0.53 | <.001 |
| Schizophrenia and other psychotic disorders | 4.5 | 0.77 | 0.70–0.84 | <.001 | 0.80 | 0.72–0.88 | <.001 |
| Post-traumatic stress disorder | 2.6 | 0.24 | 0.19–0.31 | <.001 | 0.36 | 0.26–0.50 | <.001 |
| Coronary revascularization | |||||||
| Overall, % |
Unadjusted OR |
95% CI |
p value |
∗Adjusted OR |
95% CI |
p value |
|
| No mental health disorders | 50.6 | Ref | ref | ref | ref | ref | ref |
| Major depression | 46.1 | 0.86 | 0.84–0.88 | <.001 | 0.80 | 0.78–0.82 | <.001 |
| Bipolar disorder | 44.9 | 0.90 | 0.85–0.94 | <.001 | 0.69 | 0.65–0.72 | <.001 |
| Anxiety disorders | 50.5 | 1.02 | 1.00–1.04 | 0.01 | 1.00 | 0.95–1.04 | 0.9 |
| Schizophrenia and other psychotic disorders | 37.6 | 0.54 | 0.51–0.56 | <.001 | 0.50 | 0.47–0.52 | <.001 |
| Post-traumatic stress disorder | 52.6 | 1.18 | 1.08–1.27 | <.001 | 1.08 | 0.97–1.17 | <.001 |
Abbreviations: CI: confidence interval; OR: odds ratio.
Fig. 2.
A and B. Differences in the temporal trends of the coronary revascularization (A) and in-hospital mortality (B) among patients with acute myocardial infarction stratified by mental health disorders.
Figure shows the differences in the temporal trends of the coronary revascularization and in-hospital mortality among patients with acute myocardial infarction stratified by various types of mental health disorders.
3.6. MHD and in-hospital mortality
The average in-hospital mortality of the entire study cohort was 5.1%. The average in-hospital mortality rate was highest among patients without any MHD (6.4%) and lowest among patients with comorbid anxiety disorders (2.6%) and PTSD (2.6%) (Table 2) Fig. 2B). The in-hospital mortality following acute MI decreased across the study period among all categories of MHD except among those with a co-morbid diagnosis of bipolar disorder and schizophrenia/psychotic disorders (eTable 7). Compared to patients with no diagnosis of MHD, patients with various types of MHD had lower odds of in-hospital mortality (Table 2). The odds of lower in-hospital mortality among patients with MHD compared to those without any MHD weakened with increasing age on age-stratified regression analysis (eTable 6).
4. Discussion
In this study, we report certain key findings in regards to the sex- and racial/ethnic-differences in the temporal trends and prevalence of MHD, and their in-hospital outcomes, among a contemporary cohort of patients hospitalized for acute MI in the US from 2008 through 2017. First, major depression and anxiety were the predominant MHD among patients hospitalized with acute MI. Second, there was a consistent but variable degree of increase in the prevalence of MHD. Notably, the prevalence of major depression, anxiety disorders and PTSD almost doubled during the study period. Third, there were significant sex- and racial/ethnic-differences in the burden and temporal trends in the prevalence of MHD among patients with acute MI. Fourth, a comorbid diagnosis of major depression, bipolar, or schizophrenia/psychotic disorders were significantly associated with a lower likelihood of index hospital coronary revascularization, even though a co-diagnosis of MHD was associated with a lower risk of in-hospital mortality.
4.1. Overall burden and trends in MHD
We found that major depression and anxiety disorders followed by bipolar disorder are the major MHD among patients hospitalized with acute MI. The prevalence of major depression and anxiety disorders has almost doubled among acute MI patients; also, bipolar disorder showed a consistent and significant increase (42%) over the decade. While the general prevalence of depression among US adults remains unchanged over the recent years [5], there are consistent reports of a significant increase in the community prevalence of the bipolar disorder among adults, particularly youths [6,7], which is thought to be likely due to increased awareness among medical providers about this previously under-recognized diagnosis [6]. This concerning increase in the prevalence of major depression and bipolar disorder among patients with acute MI needs special attention as they are important but often under-estimated as risk factors for CVD [8]. Depression and bipolar disorder have been upgraded as moderate risk factors for early CVD because of a strong association between these diseases [2]. Adults with major depression are at 3-fold higher prevalence of CVD and those with bipolar are at 5-fold increased risk of CVD at an age 7.5–14 years younger than the adults without mood disorders [2,9,10]. Often mood disorders tend to be under-recognized among young adults and lead to inadequate treatment and adverse outcomes [2,9]. Our study findings corroborate with other reports that anxiety disorders are increasingly been found as a co-morbid diagnosis along with other medical and MHD over time due to increased awareness and screening for stress disorders [11]. Even though the isolated impact of anxiety disorders on CVD is not well established, the rising prevalence of anxiety disorders among patients with acute MI is concerning as few studies suggest a strong association between CVD and anxiety disorders [12]. A recent study showed that women with anxiety disorders but no prior CVD were more likely to have myocardial ischemia compared to those without anxiety [13]. It is plausible that anxiety symptoms could overlap or mask symptoms of CVD leading to delays in referral and optimal treatment [13].
4.2. Sex and race/ethnic trends in MHD
Our study found significant sex- and racial/ethnic-differences in the prevalence of MHD among acute MI patients. Females suffer from major depression, anxiety disorders and bipolar disorder disorders almost twice as often as males. Even though the uptrend in the prevalence was noted across all subgroups, the females had the largest increase in the prevalence of these disorders. NHW followed by Hispanics and NA were the most affected with mood disorders and anxiety disorders, and they constituted a significant share of the rising trends in these disorders. Although all races experienced a significant increase in the prevalence of major depression, NA experienced that largest increase. The health needs and mental health of NA have historically been understudied, underfunded and understaffed [14]. Interestingly, Asians/PI had the lowest prevalence of MHD when compared to other races/ethnicities. This finding is consistent with prior reports of lower rates of utilization of mental health services by Asians; however, it is unclear whether this is truly due to the lower prevalence of the disorders because of better psychological resilience of people of Asian descent or under-diagnosis of these disorders among Asian descendants [15]. It could also be due to the fact that the expression of emotional distress may be different in Asians and other racial-ethnic minority groups [16]. The prevalence of PTSD was highest among NA and the largest increase was seen among NHB. NA and NHB are the two racial/ethnic groups that have experienced ‘historical trauma’ among other social injustices [17,18]. Interventions to address the mental health of these groups should be rooted in trauma-informed and culturally responsive care [19].
4.3. Impact of specific types of MHD
It is concerning that patients with major depression and bipolar disorder were less likely to receive coronary revascularization during an index hospitalization for acute MI. Few other studies have shown similar findings among patients with major depression [[20], [21], [22]]. Provider biases, possible late presentation and logistical challenges in providing optimal invasive care (such as if severely depressed or bipolar patients decline an offered option of coronary revascularization) are possible reasons for a lower rate of coronary revascularization among these cohorts. Also, we found that the in-hospital mortality among patients with bipolar disorder with acute MI remained unchanged over the decade while it had a consistent decline among other cohorts. Together with these facts and an alarming increase in the prevalence of major depression and bipolar disorder among patients with acute MI, it is vitally important for comprehensive care of these patients with a goal to achieve optimal revascularization rates.
Schizophrenia/psychotic disorders and PTSD were the least prevalent MHD among patients with acute MI. Schizophrenia is associated with a higher risk of acute MI among younger adults [23]. Consistent with prior reports [24,25], in our study, we found that the patients with schizophrenia/psychotic disorders were the least likely to get coronary revascularization following acute MI and there was no increase in coronary revascularization rate unlike other cohorts. While other data from the NIS from an earlier time from (2004–2014) found that patients with schizophrenia with acute MI were at increased odds of in-hospital mortality [OR 1.10 (95% CI 1.04–1.16) [25], we found that schizophrenia was associated with lower in-hospital mortality (OR 0.80 (0.72–0.88) during the years 2008–2017, compared to those without MHD. This apparent mortality paradox is discussed more below; however, our findings were notable that the in-hospital mortality following acute MI in this group has not declined over the decade. Our study findings are important for prompt recognition of comorbid schizophrenia/psychotic disorders among adults with acute MI and provide appropriate care without any treatment bias for optimal outcomes in this small, but vulnerable group.
PTSD is a well-recognized condition found to be common among acute MI survivors as well as a risk factor for acute MI [26,27]. Poorer health care and lifestyle [28], abnormal autonomic response [29,30] and heightened inflammatory state [31] are some of the mechanisms suggested to explain the association of PTSD and CVD. We found a 3-fold increase in the prevalence of PTSD among acute MI patients over the 10-year period. It is crucial to address PTSD as a risk factor and an outcome among acute MI survivors.
4.4. In-hospital mortality among patients with MHD
There was a seemingly paradoxical lower risk of in-hospital mortality among patients with MHD compared to those without MHD among our study population. These differences in the mortality risks were less apparent with increasing age on age-stratified analysis signifying a short-term survival advantage that the younger age adds to patients with MHD. Similar findings have been demonstrated among other studies examining short-term outcomes (up to 30-days) among patients with MHD [[20], [21], [22],32]. However, it is intriguing that those patients who suffer from MHD have developed acute MI at an early age compared to their non-MHD counterparts and this seems to be likely due to premature CVD associated with various MHD [2,33]. Also, multiple studies examining the long-term (≥1 year) outcomes of acute coronary syndromes among patients with MHD have found significantly lower survival compared to those with no MHD [[34], [35], [36], [37], [38]]. The lower rates of coronary revascularization and poor after-care among patients with MHD [37] could have been the reason for poor long-term survival among these patients.
4.5. Clinical and public health implications
The increasing burden of MHD among acute MI patients in the US signifies the importance of comprehensive assessment of CVD risk factor profile including the psychological, mental, social and ethnic risks of the individual rather than just traditional atherosclerotic risk factors. Moreover, MHD are often ignored when it comes to cardiovascular prevention strategies because of a lack of awareness about the implications of MHD among patients with CVD like lesser odds of coronary revascularization and consequent poorer long-term outcomes due to factors like inadequate self-care, non-adherence to medications and follow-ups, as well as unfamiliarity with the potential psychological interventions that could potentially improve overall outcomes. Our findings are particularly important in the light of recent evidence suggestive of interventions like exercise training and cardiac rehabilitation to help improve psychological risk factors and reduces stress-related mortality among patients with CVD [39,40]. While clinicians may feel inadequately trained to address MHD themselves, it is worthwhile to utilize a team-based approach to care and involve psychologists, psychotherapists, and other behavioral therapists as indicated.
4.6. Strengths and limitations
Our study adds significantly to the knowledge of the MHD and CVD by comprehensively reporting the overall prevalence and trends with detailed sex- and racial/ethnic-differences in the prevalence of major MHD and in-hospital outcomes in a nationally representative contemporary cohort of acute MI patients. Our findings will enable cardiovascular clinicians, psychiatrists, policymakers and preventive experts to identify the types of MHD which need immediate attention, racial/ethnic groups which need special care, and implement policies to tackle the hostile combination of MHD and CVD to improve the holistic health of the individual as well as further risk reduction in cardiovascular mortality and morbidity.
Our study has certain limitations. Our study findings apply to hospitalized adults with acute MI. This could underestimate the true prevalence of MHD among patients with stable CVD. The increase in the prevalence of MHD could be because of more frequent coding in recent years when compared to previous years. However, we further validated our analysis with falsification endpoints which reinforces the trueness of our study findings of rising burden of MHD among acute MI patients as we did not find a corresponding increase in the prevalence of 3 falsification endpoints. In addition, it is possible that the increased awareness about MHD in the community and the providers to screen for MHD among inpatients would have contributed to increased diagnosis and hence the rising prevalence of various types of MHD. Nevertheless, our study provides a detailed assessment of the burden of MHD among acute MI hospitalizations and it emphasizes the importance of clinicians to address the mental health comorbidities for overall improved outcomes. Reliance on administrative data to extract MHD diagnosis can potentially lead to miscoding errors; however, we have used accurate ICD-9 and ICD-10 codes with appropriate statistical tools as recommended by HCUP to enable a longitudinal analysis of comorbid diagnoses to obtain national estimates limiting any such errors. ICD-9 and ICD-10 CM codes are the most comprehensive classification system of MHD to date. Prior systematic reviews have found that use of administrative dataset for analyzing MHDs are fairly accurate with an average positive predictive value of 76% [41]. Also, the NIS database has been extensively used to identify sex- and race/ethnicity-based differential outcomes and prevalence of diseases over time in other reports [42]. Lastly, we were unable to assess the impact of MHD on the long-term outcomes following acute MI because of the nature of the dataset which tracks only the in-hospital events and outcomes.
5. Conclusion
Mental health disorders are common among patients hospitalized with acute MI. Over this 10-year period, there was a concerning increase in the prevalence of most forms of MHD, mainly the prevalence of major depression, bipolar disorder, anxiety disorders and PTSD. A comorbid diagnosis of major depression, bipolar disorder and schizophrenia/psychotic disorders was associated with a lower likelihood of index hospital coronary revascularization. Acute MI patients with comorbid MHD should be provided with comprehensive care for better long-term outcomes even though the evidence behind the use of various behavioral interventions to improve survival and quality of life among patients with MHD is still limited.
Funding sources
Erin D. Michos is supported by the Amato Fund for Women’s Cardiovascular Health Research at Johns Hopkins University.
Conflicts of interest
All authors have no relevant conflicts of interest.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajpc.2020.100133.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Levine G.N. The mind-heart-body connection. Circulation. 2019;140:1363–1365. doi: 10.1161/CIRCULATIONAHA.119.041914. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein B.I., Carnethon M.R., Matthews K.A., McIntyre R.S., Miller G.E., Raghuveer G., Stoney C.M., Wasiak H., McCrindle B.W. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: a scientific statement from the American heart association. Circulation. 2015;132:965–986. doi: 10.1161/CIR.0000000000000229. [DOI] [PubMed] [Google Scholar]
- 3.Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: December 2019. National Inpatient Sample (NIS) . 2012. [Google Scholar]
- 4.Mays V.M., Ponce N.A., Washington D.L., Cochran S.D. Classification of race and ethnicity: implications for public health. Annu. Rev. Publ. Health. 2003;24:83–110. doi: 10.1146/annurev.publhealth.24.100901.140927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brody D.J., Pratt L.A., Hughes J.P. 2018. Prevalence of Depression Among Adults Aged 20 and over: United States, 2013-2016. NCHS Data Brief; pp. 1–8. [PubMed] [Google Scholar]
- 6.Moreno C., Laje G., Blanco C., Jiang H., Schmidt A.B., Olfson M. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch. Gen. Psychiatr. 2007;64:1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- 7.Harpaz-Rotem I., Leslie D.L., Martin A., Rosenheck R.A. Changes in child and adolescent inpatient psychiatric admission diagnoses between 1995 and 2000. Soc. Psychiatr. Psychiatr. Epidemiol. 2005;40:642–647. doi: 10.1007/s00127-005-0923-0. [DOI] [PubMed] [Google Scholar]
- 8.Gan Y., Gong Y., Tong X., Sun H., Cong Y., Dong X., Wang Y., Xu X., Yin X., Deng J., Li L., Cao S., Lu Z. Depression and the risk of coronary heart disease: a meta-analysis of prospective cohort studies. BMC Psychiatr. 2014;14:371. doi: 10.1186/s12888-014-0371-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldstein B.I., Fagiolini A., Houck P., Kupfer D.J. Cardiovascular disease and hypertension among adults with bipolar I disorder in the United States. Bipolar Disord. 2009;11:657–662. doi: 10.1111/j.1399-5618.2009.00735.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant B.F., Stinson F.S., Hasin D.S., Dawson D.A., Chou S.P., Ruan W.J., Huang B. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the national epidemiologic survey on alcohol and related conditions. J. Clin. Psychiatr. 2005;66:1205–1215. doi: 10.4088/jcp.v66n1001. [DOI] [PubMed] [Google Scholar]
- 11.Ruscio A.M., Hallion L.S., Lim C.C.W., Aguilar-Gaxiola S., Al-Hamzawi A., Alonso J. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiatr. 2017;74:465–475. doi: 10.1001/jamapsychiatry.2017.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frasure-Smith N., Lespérance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch. Gen. Psychiatr. 2008;65:62–71. doi: 10.1001/archgenpsychiatry.2007.4. [DOI] [PubMed] [Google Scholar]
- 13.Paine N.J., Bacon S.L., Pelletier R., Arsenault A., Diodati J.G., Lavoie K.L. Do women with anxiety or depression have higher rates of myocardial ischemia during exercise testing than men? Circ Cardiovasc Qual Outcomes. 2016;9:S53–S61. doi: 10.1161/CIRCOUTCOMES.115.002491. [DOI] [PubMed] [Google Scholar]
- 14.Office of the Surgeon General. Substance Abuse and Mental Health Services Administration (US); 2001. Center for Mental Health Services and the National Institute of Mental Health. Publications and Reports of the Surgeon General Mental Health: Culture, Race, and Ethnicity: A Supplement To Mental Health: A Report Of the Surgeon General Rockville (MD) [PubMed] [Google Scholar]
- 15.Lee S.Y., Martins S.S., Keyes K.M., Lee H.B. Mental health service use by persons of Asian ancestry with DSM-IV mental disorders in the United States. Psychiatr. Serv. 2011;62:1180–1186. doi: 10.1176/appi.ps.62.10.1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsumoto D. Ethnic differences in affect intensity, emotion judgments, display rule attitudes, and self-reported emotional expression in an American sample. Motiv. Emot. 1993;17:107–123. [Google Scholar]
- 17.Ehlers C.L., Gizer I.R., Gilder D.A., Ellingson J.M., Yehuda R. Measuring historical trauma in an American Indian community sample: contributions of substance dependence, affective disorder, conduct disorder and PTSD. Drug Alcohol Depend. 2013;133:180–187. doi: 10.1016/j.drugalcdep.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gone J.P. A community-based treatment for Native American historical trauma: prospects for evidence-based practice. J. Consult. Clin. Psychol. 2009;77:751–762. doi: 10.1037/a0015390. [DOI] [PubMed] [Google Scholar]
- 19.Brave Heart M.Y. The historical trauma response among natives and its relationship with substance abuse: a Lakota illustration. J. Psychoact. Drugs. 2003;35:7–13. doi: 10.1080/02791072.2003.10399988. [DOI] [PubMed] [Google Scholar]
- 20.Schulman-Marcus J., Shah T., Swaminathan R.V., Feldman D.N., Wong S.C., Singh H.S., Minutello R.M., Bergman G., Kim L.K. Comparison of recent trends in patients with and without major depression and acute ST-elevation myocardial infarction. Am. J. Cardiol. 2016;118:779–784. doi: 10.1016/j.amjcard.2016.06.051. [DOI] [PubMed] [Google Scholar]
- 21.Schulman-Marcus J., Goyal P., Swaminathan R.V., Feldman D.N., Wong S.C., Singh H.S., Minutello R.M., Bergman G., Kim L.K. Comparison of trends in incidence, revascularization, and in-hospital mortality in ST-elevation myocardial infarction in patients with versus without severe mental illness. Am. J. Cardiol. 2016;117:1405–1410. doi: 10.1016/j.amjcard.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Druss B.G., Bradford D.W., Rosenheck R.A., Radford M.J., Krumholz H.M. Mental disorders and use of cardiovascular procedures after myocardial infarction. J. Am. Med. Assoc. 2000;283:506–511. doi: 10.1001/jama.283.4.506. [DOI] [PubMed] [Google Scholar]
- 23.Wu S.I., Chen S.C., Liu S.I., Sun F.J., Juang J.J., Lee H.C., Kao K.L., Dewey M.E., Prince M., Stewart R. Relative risk of acute myocardial infarction in people with schizophrenia and bipolar disorder: a population-based cohort study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0134763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Attar R., Berg Johansen M., Valentin J.B., Aagaard J., Jensen S.E. Treatment following myocardial infarction in patients with schizophrenia. PLoS One. 2017;12 doi: 10.1371/journal.pone.0189289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohamed M.O., Rashid M., Farooq S., Siddiqui N., Parwani P., Shiers D., Thamman R., Gulati M., Shoaib A., Chew-Graham C., Mamas M.A. Acute myocardial infarction in severe mental illness: prevalence, clinical outcomes, and process of care in U.S. Hospitalizations. Can. J. Cardiol. 2019;35:821–830. doi: 10.1016/j.cjca.2019.04.021. [DOI] [PubMed] [Google Scholar]
- 26.Lima B.B., Hammadah M., Pearce B.D., Shah A., Moazzami K., Kim J.H., Sullivan S., Levantsevych O., Lewis T.T., Weng L., Elon L., Li L., Raggi P., Bremner J.D., Quyyumi A., Vaccarino V. Association of posttraumatic stress disorder with mental stress-induced myocardial ischemia in adults after myocardial infarction. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.2734. e202734-e202734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Remch M., Laskaris Z., Flory J., Mora-McLaughlin C., Morabia A. Post-traumatic stress disorder and cardiovascular diseases. Circ Cardiovasc Qual Outcomes. 2018;11 doi: 10.1161/CIRCOUTCOMES.117.004572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zen A.L., Whooley M.A., Zhao S., Cohen B.E. Post-traumatic stress disorder is associated with poor health behaviors: findings from the heart and soul study. Health Psychol. 2012;31:194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shah A., Vaccarino V. Heart rate variability in the prediction of risk for posttraumatic stress disorder. JAMA Psychiatr. 2015;72:964–965. doi: 10.1001/jamapsychiatry.2015.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shah A.J., Lampert R., Goldberg J., Veledar E., Bremner J.D., Vaccarino V. Posttraumatic stress disorder and impaired autonomic modulation in male twins. Biol. Psychiatr. 2013;73:1103–1110. doi: 10.1016/j.biopsych.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Passos I.C., Vasconcelos-Moreno M.P., Costa L.G., Kunz M., Brietzke E., Quevedo J. Inflammatory markers in post-traumatic stress disorder: a systematic review, meta-analysis, and meta-regression. Lancet Psychiatr. 2015;2:1002–1012. doi: 10.1016/S2215-0366(15)00309-0. [DOI] [PubMed] [Google Scholar]
- 32.Pino E.C., Zuo Y., Borba C.P., Henderson D.C., Kalesan B. Clinical depression and anxiety among ST-elevation myocardial infarction hospitalizations: results from Nationwide Inpatient Sample 2004-2013. Psychiatr. Res. 2018;266:291–300. doi: 10.1016/j.psychres.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 33.Lichtman J.H., Froelicher E.S., Blumenthal J.A., Carney R.M., Doering L.V., Frasure-Smith N., Freedland K.E., Jaffe A.S., Leifheit-Limson E.C., Sheps D.S., Vaccarino V., Wulsin L. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014;129:1350–1369. doi: 10.1161/CIR.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 34.Abrams T.E., Vaughan-Sarrazin M., Rosenthal G.E. Psychiatric comorbidity and mortality after acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:213–220. doi: 10.1161/CIRCOUTCOMES.108.829143. [DOI] [PubMed] [Google Scholar]
- 35.Druss B.G., Bradford W.D., Rosenheck R.A., Radford M.J., Krumholz H.M. Quality of medical care and excess mortality in older patients with mental disorders. Arch. Gen. Psychiatr. 2001;58:565–572. doi: 10.1001/archpsyc.58.6.565. [DOI] [PubMed] [Google Scholar]
- 36.Laursen T.M., Munk-Olsen T., Agerbo E., Gasse C., Mortensen P.B. Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Arch. Gen. Psychiatr. 2009;66:713–720. doi: 10.1001/archgenpsychiatry.2009.61. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell A.J., Lawrence D. Revascularisation and mortality rates following acute coronary syndromes in people with severe mental illness: comparative meta-analysis. Br. J. Psychiatr. : J. Ment. Sci. 2011;198:434–441. doi: 10.1192/bjp.bp.109.076950. [DOI] [PubMed] [Google Scholar]
- 38.Petersen L.A., Normand S.L., Druss B.G., Rosenheck R.A. Process of care and outcome after acute myocardial infarction for patients with mental illness in the VA health care system: are there disparities? Health Serv. Res. 2003;38:41–63. doi: 10.1111/1475-6773.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lavie C.J., Menezes A.R., De Schutter A., Milani R.V., Blumenthal J.A. Impact of cardiac rehabilitation and exercise training on psychological risk factors and subsequent prognosis in patients with cardiovascular disease. Can. J. Cardiol. 2016;32:S365–s373. doi: 10.1016/j.cjca.2016.07.508. [DOI] [PubMed] [Google Scholar]
- 40.Lavie C.J., Pack Q.R., Levine G.N. Expanding traditional cardiac rehabilitation in the 21st century. J. Am. Coll. Cardiol. 2020;75:1562–1564. doi: 10.1016/j.jacc.2020.02.038. [DOI] [PubMed] [Google Scholar]
- 41.Davis K.A.S., Sudlow C.L.M., Hotopf M. Can mental health diagnoses in administrative data be used for research? A systematic review of the accuracy of routinely collected diagnoses. BMC Psychiatr. 2016;16 doi: 10.1186/s12888-016-0963-x. 263-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yandrapalli S., Nabors C., Goyal A., Aronow W.S., Frishman W.H. Modifiable risk factors in young adults with first myocardial infarction. J. Am. Coll. Cardiol. 2019;73:573–584. doi: 10.1016/j.jacc.2018.10.084. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.