Summary
In emergency departments (EDs), demand for care often exceeds the available resources. Triage addresses this problem by sorting patients into categories of urgency.
The Interagency Integrated Triage Tool (IITT) is a novel triage system designed for resource-limited emergency care (EC) settings. The system was piloted by two EDs in Papua New Guinea as part of an EC capacity development program.
Implementation involved a five-hour teaching program for all ED staff, complemented by training resources including flowcharts and reference guides. Clinical redesign helped optimise flow and infrastructure, and development of simple electronic registries enabled data collection. Local champions were identified, and experienced EC clinicians from Australia acted as mentors during system roll-out.
Evaluation data suggests the IITT, and the associated change management process, have high levels of acceptance amongst staff. Subject to validation, the IITT may be relevant to other resource-limited EC settings.
Summary box
-
•
The Interagency Integrated Triage Tool, developed collaboratively by the World Health Organization, International Committee of the Red Cross and Médecins Sans Frontières, is a novel, three-tier triage system designed for resource-limited emergency care (EC) settings
-
•
The pilot version of the tool was implemented by two emergency departments in Papua New Guinea as part of an EC development project that aimed to improve triage, patient flow and data management at both sites
-
•
Implementation strategies included a collaborative partnership between Australian and Papua New Guinean EC clinicians, identification of clinical champions and recruitment of experienced EC clinicians to act as mentors during establishment of the system
-
•
Evaluation data suggests the tool has high levels of acceptance amongst staff, and the change management process was able to meet their clinical and learning needs
Emergency departments (EDs) fulfil a critical role in health systems. They are a primary access point to healthcare for patients with acute illness, provide an interface between hospital and community-based health services, and fill gaps in care for vulnerable populations [1,2].
Demand for emergency care (EC) often exceeds the available resources. It is important, therefore, that EDs have systems for prioritising patients based on the urgency of their condition. This process is referred to as triage, and has been widely implemented across EDs in high-income countries [3].
Although a large number of triage tools have been developed, few have been purpose-designed for resource-limited settings [3], [4], [5], [6], [7]. The evidence underpinning ED triage in low- and middle-income countries (LMICs) is limited, but the value of simple and context-specific approaches is widely recognised [6], [7], [8], [9], [10], [11], [12].
This article describes the implementation of a novel, three-tier triage system in two resource-limited EDs in Papua New Guinea (PNG). It discusses challenges and solutions in the change management process, and reports initial evaluation data from both sites.
1. Emergency department triage
Grounded in the ethical principles of equity and justice, triage aims to maximise the impact of EC by identifying and prioritising patients with time-critical care needs. Typical models involve a healthcare worker (often a nurse) assigning a category of urgency to each patient that presents to the ED [3].
Globally, a large number of triage scales are in operation. These differ in terms of structure (number of categories or tiers) and composition (assessment criteria) [3], [4], [5], [6], [7]. High-resource settings tend to utilise five-tier tools, which may also function to stream patients and predict resource utilisation [3]. These systems are less efficient because of the time taken to differentiate between category three and four patients [3,13].
Very few tools have been purpose-designed for resource-limited environments [6,7]. The most widely studied is the four-tier South African Triage Scale (SATS), which has demonstrated acceptable reliability and validity in a number of settings [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24]. A recent systematic review of adult triage scales in LMICs found that the evidence supporting any particular scale was moderate at best [6].
In the Pacific region, triage has been identified as a priority for EC development [25]. Amongst respondents to a survey of EC clinicians in Pacific Island Countries (PICs), only 18% reported consistent use of a recognised triage tool [25]. An exception is Solomon Islands, which has developed a simple three-tier system (the Solomon Islands Triage Scale [SITS]) based on SATS [8]. Tools with three categories are well-suited to resource-constrained EDs because they are intuitive and efficient [8,12].
2. Integrated Interagency Triage Tool
The Integrated Interagency Triage Tool (IITT), developed collaboratively by the World Health Organization (WHO), International Committee of the Red Cross (ICRC) and Médecins Sans Frontières (MSF), is a three-tier system designed for EC settings with limited resources. A four-tier adaptation of the system is planned but not yet available.
The IITT has been initially released as one of WHO's recommended tools for the COVID-19 pandemic [26,27]. Full release, accompanied by a training manual, is anticipated in late 2020. This project forms part of the field testing and validation process, and has taken on increased relevance in the context of an escalating burden of COVID-19, and an urgent need for simple tools to identify patients with time-sensitive care needs [28], [29], [30].
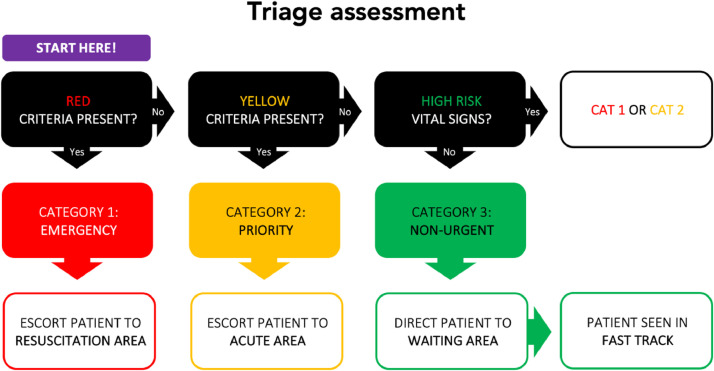
The IITT is designed to be applied at the point of ED arrival. It allocates patients into one of three, colour-coded categories based on the presence of specific signs and symptoms (categories one and two) or the absence of high-risk vital signs (category three) [27]. The IITT triage assessment flow chart, as adapted for this pilot, appears in Fig. 1. The rationale for the implementation of this system, as opposed to SATS or SITS, is discussed below.
Fig. 1.
IITT triage assessment process, as adapted for the PNG context.
3. Emergency care in Papua New Guinea
PNG, a PIC with a population of approximately 8 million, faces significant challenges in healthcare delivery. These include under-resourcing, a limited health workforce, a high burden of communicable disease and an increasing prevalence of non-communicable illness and injury [31].
Despite an expanding number of emergency physicians (EPs), most provinces have under-developed primary and secondary care systems to facilitate EC [31,32]. There is little data on the epidemiology of emergency presentations, and most EDs do not have formalised triage processes.
The IITT was piloted by two sentinel PNG EDs: Gerehu General Hospital (GGH) in the National Capital District and Mount Hagen Provincial Hospital (MHPH) in the Highlands region. These sites were selected because they are broadly representative of urban and regional contexts, and have strong leadership from locally-trained EPs.
3.1. Gerehu General Hospital, Port Moresby
Port Moresby is PNG's capital, with a population of approximately 365,000. GGH is the city's secondary public hospital. The ED receives approximately 60 presentations per day, and is staffed by four EPs, seven registrars (specialists-in-training), seven health extension officers (HEOs) and approximately 24 nurses and community health workers (CHWs). The role of HEOs is akin to clinical officers in other developing settings [33].
Prior to the clinical redesign process described below, the ED included one resuscitation bay and six acute beds. Basic pathology services are available. There are inpatient units for medicine and paediatrics, but patients requiring critical care or admission under another service are transferred to Port Moresby General Hospital (PMGH).
At the time of this project, GGH was utilising a bespoke four-tier triage system adapted from the Australasian Triage Scale. Few staff had received any formal training in triage. In the context of limited resources, GGH clinicians had identified that a three-tier tool would better suit the context.
3.2. Mount Hagen Provincial Hospital, Mount Hagen
Mount Hagen is the third largest city in PNG. It is the capital of the Western Highlands Province (population approximately 400,000), and a major administrative centre for the region.
MHPH is the city's major health facility. There is limited primary care infrastructure within the province, so patients rely on MHPH for many of their healthcare needs. The ED receives approximately 150 presentations per day, and is staffed by one EP, three registrars, five HEOs and approximately thirty nurses and CHWs. It includes four resuscitation bays, 16 acute beds and five short-stay beds. Basic pathology and radiology services are available.
Prior to implementation of the IITT, the ED had no triage system and most patients were seen on a ‘first come, first served’ basis. A large proportion of cases were receiving definitive management by a ‘screening nurse’ at the point of arrival. Only selected patients would proceed to assessment by a HEO or doctor.
Major challenges for the ED include understaffing, suboptimal data recording, a large burden of primary care patients and access block. The ED leadership team at MHPH had identified that structured processes for triage, flow and data management could address these challenges [34].
4. Needs assessment and governance
In the context of a longstanding partnership between PNG and Australian EC clinicians [2,35,36], a collaborative project was instigated to pilot a new triage model at GGH and MHPH. A needs assessment, undertaken by two Australian EPs, was informed by a strengths-based approach employed in other Pacific EC settings [37]. This process focussed on the building blocks of functional EC systems, with a view to identifying the processes, infrastructure, human resources, data systems and governance arrangements necessary for effective triage and flow [25].
The needs assessment also facilitated identification of an appropriate triage tool, and following consultation with local clinicians, the IITT was selected as the system of choice. There were several reasons for this decision. First, the four-tier SATS was thought to be too complex, mainly owing to its early warning score component [38]. Second, there were concerns that SITS would not be sufficiently sensitive for certain time-sensitive presentations, primarily because of its shorter list of category one signs and symptoms [8]. In addition, the experience of SITS in Honiara demonstrated significant delays to the assessment of category two patients [8]. PNG clinicians considered that, in the higher acuity and resource-limited settings of GGH and MHPH, a more conservative approach to triage categorisation was warranted. Third, there was a unique opportunity to pilot a new triage instrument endorsed by three well regarded organisations (WHO, MSF and ICRC). At a time of renewed enthusiasm for global EC development, collaborators were keen to make a contribution to the evidence base underpinning triage in LMICs [1,2].
Key stakeholders were identified and engaged throughout the project. These included the health services (MHPH and GGH), Ministry (National Department of Health), project manager (Australasian College for Emergency Medicine), research institute (Monash University), funding body (Australian Government) and IITT custodian (WHO). All stakeholders agreed that the IITT represented an appropriate triage tool for the context.
4.1. Patient and public involvement
Patients were informed about the project through signage in both EDs and public health messaging from health services. An example is available on the Western Highlands Provincial Health Authority website [39]. At the time of implementation, local clinicians led briefings in the ED reception area, and PNG media outlets were engaged to raise community awareness of the updated triage processes [40,41].
5. Project design and delivery
The project used a capacity development approach embedded within a research framework [42]. Data related to the impact of the IITT on ED processes and clinical outcomes, along with assessment of the tool's predictive validity and inter-rater reliability, will be reported separately. Ethics approval for the research components of the project were obtained from Monash University (MUHREC 19,106/22,581) and endorsed by the PNG Medical Research Advisory Committee (MRAC 19.08/20.12).
Although triage was the focus of the project, the needs assessment identified that a range of other ED processes would need to be updated to facilitate the system. The workplan therefore incorporated clinical redesign and data components, with the overall aim of improving triage, patient flow and data management capacity. Development, implementation and evaluation of the project occurred over a 12-month period.
During the development phase, a series of site visits facilitated planning for the clinical redesign process and infrastructure improvements; identification of local champions; and design of an electronic ED registry at both locations. In order to test the system in a smaller ED with pre-existing triage experience, implementation was undertaken at GGH in advance of MHPH.
5.1. Resource development
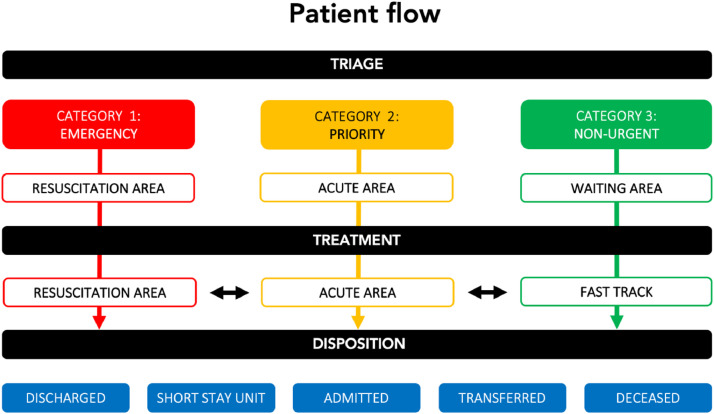
A number of resources were developed to facilitate the operation of the IITT. These included colour-coded flowcharts for triage assessment (Fig. 1) and patient flow (Fig. 2). The terms ‘emergency’, ‘priority’ and ‘non-urgent’ were assigned to the tiers to ensure consistency with other WHO tools [12]. Laminated cards for category one (emergency) signs and symptoms, category two (priority) signs and symptoms, vital sign parameters, high-risk trauma criteria and locally recommended time targets were also developed. These resources were introduced during the modular teaching program and mentoring period described below.
Fig. 2.
Patient flow process, linking triage category with key stages in the ED patient journey.
5.2. Clinical redesign and infrastructure improvements
The IITT defines three streams of care based on the urgency of the patient's condition (Fig. 2). In both EDs, designated areas were developed for emergency (resuscitation/red zone), priority (acute/yellow zone) and non-urgent patients (fast track [FT]/green zone). These were demarcated using coloured signage and duct tape (placed on the floor).
In both facilities, changes in layout were required to ensure that FT areas were in close proximity to the waiting room. This was an important strategy to minimise crowding. At GGH, the former resuscitation room was converted into a FT treatment space, and a new, two-bed ‘red zone’ established in the high visibility area of the department.
At MHPH, the existing ‘screening’ area was deemed inadequate for triage due to its small size and sub-optimal ventilation. With minimal renovation, a protected triage area was established, incorporating bench space for two triage officers and ward clerks (Fig. 3A). At both sites, vital signs monitors were installed to facilitate observation measurement, and the waiting rooms expanded to allow sufficient capacity for all category three patients to be seated in view of the triage desk.
Fig. 3.
Pictures from Mount Hagen Provincial Hospital demonstrating various strategies for effective triage and flow within the ED
A = renovated triage area to accommodate two triage officers and two ward clerks; B = staff allocations whiteboard linked to streams of care; C = colour-coded patient tracking whiteboard; and D = simple box system for organising patient charts, to ensure that patients are seen in the correct order.
A number of other systems were implemented to improve flow and ED functioning. For instance, whiteboards were marked with coloured tape to facilitate staff allocations (Fig. 3B) and patient tracking (Fig. 3C) across the different care streams. At GGH, an additional consultation room was incorporated into the ED's allocated physical space to expand FT capacity.
5.3. Operationalisation
A clear process was required to operationalise the IITT. Based on a strategy employed elsewhere [8], a manual sorting system, linked with the triage assessment workflow, was developed.
Under this process, all patients presenting to triage are allocated a clipboard. After completion of the triage assessment, the clipboard (and associated paperwork) is placed at the back of a designated, category-specific box (Fig. 3D). To ensure that patients are seen in the correct order, clinicians select a clipboard from the front of the box and prioritise ‘red before yellow’ and ‘yellow before green’. At the conclusion of a patient's episode of care, clipboards are placed in a designated ‘discharge’ box and returned to triage for re-use.
5.4. Documentation and data management
To facilitate the new system, a patient registration and triage form (PRTF) was developed for both sites (supplementary file). The form was designed to facilitate clinical care as well as data capture.
Simple, electronic registries, an important tool to drive EC quality improvement [43], were developed at both sites. At GGH, a Microsoft Excel database was built with the functionality to automatically calculate key time intervals and tally presentation frequencies. At MHPH, a registry linked to the existing hospital information system was designed by a local developer. This incorporates functionality for performance indicator and disease surveillance reporting, including auto-populated frequency tables for the country's National Health Information System [44].
At both sites, data entry occurs at the conclusion of the patient's episode of care. Ward clerks collect the completed PTRFs and enter relevant data into the registry. If data entry is maintained, the registries can report ED summary statistics in close to real-time.
5.5. Training process
A multi-disciplinary team of experienced Australian EC clinicians was recruited to assist with training. Ideally, the faculty would have included experienced triage officers from other PICs, but limited regional experience with triage and human resource shortages were barriers to recruitment [25,45].
At both sites, the training process comprised a five-hour classroom session consisting of three modules. Experience elsewhere has shown the feasibility of brief educational interventions [46]. Content was developed by the Australian team (inspired by established triage training programs) [8,12,38,47] but reviewed by local collaborators. Sessions were conducted in multi-disciplinary groups of up to 20 participants, and co-facilitated by local EPs. Local leaders decided that all ED staff should undertake the training, such that doctors, HEOs, nurses and CHWs would all have capacity to undertake the triage officer role.
Each module comprised a range of educational strategies linked with specific learning outcomes. These included multiple choice questions, case-based scenarios and role plays, with a strong emphasis on triage assessment (Fig. 1) and patient flow (Fig. 2) components of the system. Facilitators took an active role in observing participants and providing feedback on their performance.
5.6. Mentoring and implementation support
At both sites, the new system went live within 48 h of the classroom teaching sessions. Roll-out was supported by the visiting Australian clinicians. Nurses provided one-on-one mentoring at the triage desk and to senior nursing staff managing flow within the ED. This intense mentoring was utilised for all day shifts for one week following implementation. Changes to flow and ED design were also initiated during this period.
Given the extent of the changes at MHPH, the new model was presented to all hospital clinicians at a ‘grand round’. This provided an opportunity to educate non-ED staff about the updated processes. To help patients navigate the system, security staff, stationed at ED entrances, provided directions.
6. Monitoring and evaluation
At both sites, follow-up visits were undertaken within three months of implementation. These enabled evaluation of the change management processes, provided a further opportunity for mentoring and allowed training of local champions to provide ongoing, in-house education. The evaluation visits also facilitated assessment of the IITT's reliability (using inter-rater agreement), but these data will be reported separately.
6.1. Survey findings
In review meetings at both sites, staff were invited to complete a voluntary, anonymous survey regarding the system and change management process. This utilised a five-point Likert scale (strongly disagree – strongly agree). There were 24 respondents from GGH (50% of those trained) and 15 from MHPH (41.6% of those trained).
6.2. Triage and flow system
The proportion of respondents who agreed or strongly agreed with the statements regarding the triage and flow process is described in Table 1A. There was 100% agreement that “the new triage and flow system helps identify and prioritise the most urgent patients”.
Table 1.
Evaluation survey responses.
| Statement | GGH (n = 24) | MHPH (n = 15) |
|---|---|---|
| A: TRIAGE AND FLOW PROCESS | ||
|
100% | 100% |
|
79% | 100% |
|
96% | 100% |
|
88% | 100% |
|
56% | 93% |
| B: IMPLEMENTATION PROCESS | ||
|
100% | 100% |
|
100% | 100% |
|
100% | 91% |
|
100% | 100% |
|
100% | 100% |
The figures denote the proportion of survey respondents that agreed or strongly agreed with the relevant statement, based on a five-point Likert scale (strongly disagree – strongly agree).
Staff were asked if they would change anything about the triage criteria. None provided recommendations. More than two thirds of respondents explicitly stated that no changes were required, citing reasons such as, “the process is very clear to follow”, “the current system is very flexible” and “the triage criteria summarises all the specific details we need to categorise the patient”.
The survey also asked respondents how they thought the system could be improved. Staff suggested that more clinicians were required to address an ongoing high workload; diversion of lower acuity patients to alternate facilities would help address crowding; and ongoing training may assist with knowledge retention.
6.3. Training and education process
The proportion of respondents who agreed or strongly agreed with the statements regarding the training process is described in Table 1B. There was 100% agreement that “the training program adequately supported implementation of the triage and flow system”, “the duration of the training session was sufficient” and “the reference materials (eg, triage flowcharts) helped me to understand the new system”.
Staff were asked if they would change anything about the implementation process. Respondents suggested that periodic refresher training would be valuable, and involvement of ambulance drivers and security staff would help ensure understanding across all disciplines.
6.4. Limitations
A degree of caution is required in interpreting these survey findings. The response rate was sub-optimal and there is a possibility of sampling bias. This reflects the voluntary nature of the survey, and a deliberate strategy to allow clinicians to complete the form in their own place and time. There are also implicit power imbalances in development projects involving external advisors, and despite the best efforts of the visiting Australian clinicians to create an egalitarian learning environment, local staff may have felt compelled to rate the system highly.
7. Reflections and lessons learned
Notwithstanding these limitations, survey responses were overwhelmingly positive about the system and change management process. These findings speak to the face validity of the IITT and the implementation strategy as a whole. Beneficial structural elements included a multisectoral, collaborative governance model; an effective partnership between PNG and Australian EC clinicians built on mutual trust and respect; strong local leadership; and a motivated team of Australian EC clinicians who donated their time to the project.
Some of the challenges encountered, and lessons learned, are described in Table 2. A key message was the need for flexibility and innovation in addressing issues associated with poor ED design and infrastructure, and the value of local clinicians identifying solutions to unforeseen problems. In addressing these challenges, a successful strategy was making the process collaborative and enjoyable for all participants. Highlights included applying coloured duct tape to the floor, role-playing during classroom training and assembling fans to keep the triage and learning areas cool! These lessons will be of relevance to other settings considering implementation of the IITT.
Table 2.
Challenges, solutions and lessons learned during implementation of the new triage and flow processes.
| Challenge | Solution |
| Congestion at the triage desk | Security staff trained in the new triage and flow processes, and called upon to assist with crowd control and provide directions to patients |
| Temperature overwhelming in the triage area during peak periods | Fans purchased to help ensure a safe and comfortable work environment |
| Uncertainty about the staff member responsible for the triage officer role | Whiteboard established for the clear allocation of staff members to all clinical areas |
| Long delays to triage at commencement of morning shift (as hospital gates locked overnight) | Night shift staff encouraged to commence triage of patients at first light to manage workload for the morning team |
| Delays to review of patients returning for results review | Establishment of separate queue for ‘same day reviews’, allowing prioritisation of these returning patients ahead of new category three cases |
| Insufficient triage staff (due to overwhelming workload) to allow review of waiting room patients in peak times | EP and senior nurses encouraged to undertake or delegate waiting room reviews in order to monitor for potentially deteriorating patients |
| Difficulty calling for assistance when a lone triage officer was working at the triage desk | Doorbell system implemented to allow triage officer to signal for help from clinicians working in main area of the ED |
| Asthma patients bypassing triage area to access nebuliser station for ‘self-service’ | All staff, including security officers, encouraged to ensure these patients enter via main entrance and are assessed by triage staff prior to medication administration |
| Fast track patients with ongoing care needs initially had delays to follow-up/discharge, as they would be seen in an assessment room prior to being transferred to the fast track treatment zone | Designation of a specific HEO or doctor responsible for the follow-up and ongoing management of patients in the fast track treatment zone |
| Access block hindering patient flow through the ED | Senior ED staff encouraged to review ED patients and assist facilitation of ward transfers/discharges as promptly as possible, and hospital flow managers actively engaged in IITT training process |
| Inaccurate time reporting on PRTF | Clocks purchased for the ED to ensure accurate documentation of time stamps |
| Difficulties maintaining data entry into new, electronic clinical registries | Additional ward clerks recruited, and working hours expanded, to maximise capacity for data entry and accurate performance indicator reporting |
Ultimately, the success of this project reflects the enthusiasm of PNG clinicians for quality improvement in their departments. Strong local leadership and ownership were essential to the change management process. EDs lacking these attributes may find it difficult to embark on projects of this nature.
8. Future directions
Assessment of the IITT's validity and reliability is currently underway. Protocols to test the impact of triage implementation on process measures (eg, time to assessment) and clinical outcomes (eg, mortality) have also been developed (clinicaltrials.gov reference NCT04098705).
In the interim, early results from the pilot have been considered by local clinicians at PNG's Medical Symposium [48]. On the back of positive experience to date, plans are being developed to extend the system to PNG's two largest EDs (including PMGH) and trial a train-the-trainer model. This will allow the implementation process to become self-sustaining.
Beyond PNG, the IITT model is being considered for adaptation in other Pacific settings. In the context of significant labour mobility amongst PICs, there may be advantages to a uniform, three-tier triage scale across the region [25,45].
Outcomes from this pilot will have important implications beyond the Pacific. Advantages of the IITT include simplicity, efficiency and low resource utilisation. If validated, the tool is likely to have applicability in a variety of LMIC contexts.
The project has demonstrated that triage implementation is a vehicle for a range of process improvements, including patient flow and data management. Consistent with experience elsewhere [10,49,50], the combination of these systems changes is likely to improve ED performance, with the potential to reduce morbidity and mortality.
Conclusion
The IITT is a novel, three-tier triage tool. This project piloted the system in two resource-limited EDs in PNG, and was accompanied by clinical redesign, infrastructure improvement and data management enhancements to improve ED functioning.
Implementation was achieved through a partnership model involving Australian and PNG clinicians. Essential strategies included strong local leadership, such as EP champions at both sites, and recruitment of experienced EC clinicians to act as mentors.
The IITT, and the change management process described here, appear to have high levels of acceptance amongst staff. Subject to further field testing and assessment of predictive validity, the tool is likely to be relevant to other resource-limited EDs.
Contribution statement
RM led the project and was primarily responsible for manuscript preparation. JM, OB, GN, JT and SKa were essential local collaborators and played important roles in IITT implementation. CB, SB, TC, TH and JPM participated in the training and mentoring process. TR contributed to project design, SKo assisted with project management, and GOR and PC provided research advice. All co-authors reviewed the manuscript.
Data sharing statement
All data referred to in this paper are available, in de-identified format, from the corresponding author upon reasonable email request.
Declaration of Competing Interest
None to declare
Acknowledgments
Acknowledgements
The authors would like to acknowledge all of the EC clinicians at GGH and MHPH who participated in the IITT training and implementation process. Thanks also go to the Executive of the Western Highlands Provincial Health Authority, including Hospital Manager Jane Holden, and the staff on the Global EC Desk at the Australasian College for Emergency Medicine, including Sally Reid, for actively supporting and championing the project. The authors also acknowledge the efforts of those WHO, MSF and ICRC staff who contributed to development of the IITT.
Funding
The project was funded through a Friendship Grant from the Australian Government Department of Foreign Affairs and Trade and an International Development Fund Grant from the Australasian College for Emergency Medicine Foundation. RM is supported by a National Health and Medical Research Council Postgraduate Scholarship and a Monash Graduate Excellence Scholarship.
Footnotes
Provenance: Not commissioned
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2020.100051.
Appendix. Supplementary materials
References
- 1.World Health Assembly. Resolution 72.16. Emergency care systems for universal health coverage: ensuring timely care for the acutely ill and injured. https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R16-en.pdf. Published 2019. Accessed January 20, 2020.
- 2.Mitchell R., Phillips G., O’Reilly G., Creaton A., Cameron P. World Health Assembly resolution 72.16: what are the implications for the Australasian College for Emergency Medicine and emergency care development in the Indo‐Pacific? Emerg Med Australas. 2019;31(5):696–699. doi: 10.1111/1742-6723.13373. [DOI] [PubMed] [Google Scholar]
- 3.FitzGerald G., Jelinek G.A., Scott D., Gerdtz M.F. Emergency department triage revisited. Emerg Med J. 2010;27(2):86–92. doi: 10.1136/emj.2009.077081. [DOI] [PubMed] [Google Scholar]
- 4.Farrokhnia N., Castren M., Ehrenberg A. Emergency department triage scales and their components: a systematic review of the scientific evidence. Scand J Trauma Resusc Emerg Med. 2011;19(1):42. doi: 10.1186/1757-7241-19-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hinson J.S., Martinez D.A., Cabral S. Triage performance in emergency medicine: a systematic review. Ann Emerg Med. 2019;74(1):140–152. doi: 10.1016/j.annemergmed.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Jenson A., Hansoti B., Rothman R., de Ramirez S.S., Lobner K., Wallis L. Reliability and validity of emergency department triage tools in low- and middle-income countries. Eur J Emerg Med. 2018;25(3):154–160. doi: 10.1097/MEJ.0000000000000445. [DOI] [PubMed] [Google Scholar]
- 7.Hansoti B., Jenson A., Keefe D. Reliability and validity of pediatric triage tools evaluated in low resource settings: a systematic review. BMC Pediatr. 2017;17(1):37. doi: 10.1186/s12887-017-0796-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wanefalea L.E., Mitchell R., Sale T., Sanau E., Phillips G.A. Effective triage in the Pacific region: the development and implementation of the Solomon Islands Triage scale. Emerg Med Australas. 2019;31(3):451–458. doi: 10.1111/1742-6723.13248. [DOI] [PubMed] [Google Scholar]
- 9.Wallis L., Gottschalk S., Wood D., Bruijns S., de Vries S., Balfour S. The Cape Triage score - a triage system for South Africa. South African Med J. 2006;96(1):53–56. [PubMed] [Google Scholar]
- 10.Molyneux E., Ahmad S., Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bull World Health Organ. 2006;84(4):314–319. doi: 10.2471/blt.04.019505. doi:/S0042-96862006000400016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duke T. New WHO guidelines on emergency triage assessment and treatment. Lancet. 2016;387(10020):721–724. doi: 10.1016/S0140-6736(16)00148-3. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Emergency Triage assessment and treatment (ETAT) course. https://www.who.int/maternal_child_adolescent/documents/9241546875/en/. Accessed September 13, 2020.
- 13.Health Policy Priorities Principal Committee . Adelaide; 2011. Australian Triage process review - report. [Google Scholar]
- 14.Meyer G.D., Meyer T.N., Gaunt C.B. Validity of the South African Triage Scale in a rural district hospital. Afr J Emerg Med. 2018;8(4):145–149. doi: 10.1016/j.afjem.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wangara A.A., Hunold K.M., Leeper S. Implementation and performance of the South African Triage scale at Kenyatta National Hospital in Nairobi, Kenya. Int J Emerg Med. 2019;12(1) doi: 10.1186/s12245-019-0221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Uwamahoro C., Aluisio A.R., Chu E. Evaluation of a modified South African Triage score as a predictor of patient disposition at a tertiary hospital in Rwanda. African J Emerg Med. 2020;10(1):17–22. doi: 10.1016/j.afjem.2019.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dalwai M., Valles P., Twomey M. Is the South African Triage scale valid for use in Afghanistan, Haiti and Sierra Leone? BMJ Glob Heal. 2017;2(2) doi: 10.1136/bmjgh-2016-000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sunyoto T., Van Den Bergh R., Valles P. Providing emergency care and assessing a patient triage system in a referral hospital in Somaliland: a cross-sectional study. BMC Health Serv Res. 2014;14(1) doi: 10.1186/s12913-014-0531-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bruijns S.R., Wallis L.A., Burch V.C. Effect of introduction of nurse triage on waiting times in a South African emergency department. Emerg Med J. 2008;25(7):395–397. doi: 10.1136/emj.2007.049411. [DOI] [PubMed] [Google Scholar]
- 20.Bruijns S.R., Wallis L.A., Burch V.C. A prospective evaluation of the Cape triage score in the emergency department of an urban public hospital in South Africa. Emerg Med J. 2008;25(7):398–402. doi: 10.1136/emj.2007.051177. [DOI] [PubMed] [Google Scholar]
- 21.Lowsby R., Kamara C., Kamara M. An assessment of nurse-led triage at Connaught Hospital, Sierra Leone in the immediate post-Ebola period. African J Emerg Med. 2017;7(2):51–55. doi: 10.1016/j.afjem.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Massaut J., Valles P., Ghismonde A. The modified south African triage scale system for mortality prediction in resource-constrained emergency surgical centers: a retrospective cohort study. BMC Health Serv Res. 2017;17(1):594. doi: 10.1186/s12913-017-2541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dalwai M.K., Twomey M., Maikere J. Reliability and accuracy of the South African Triage Scale when used by nurses in the emergency department of Timergara Hospital, Pakistan. South African Med J. 2014;104(5):372. doi: 10.7196/SAMJ.7604. [DOI] [PubMed] [Google Scholar]
- 24.Rominski S., Bell S.A., Oduro G., Ampong P., Oteng R., Donkor P. The implementation of the South African Triage Score (SATS) in an urban teaching hospital, Ghana. Afr J Emerg Med. 2014;4(2):71–75. doi: 10.1016/j.afjem.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phillips G., Creaton A., Airdhill-Enosa P. Emergency care status, priorities and standards for the Pacific region: a multiphase survey and consensus process across 17 different Pacific Island Countries and Territories. Lancet Reg Heal - West Pacific. 2020;1 doi: 10.1016/j.lanwpc.2020.100002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed July 3, 2020.
- 27.World Health Organization. Clinical care of severe acute respiratory infections - tool kit. https://www.who.int/publications/i/item/clinical-care-of-severe-acute-respiratory-infections-tool-kit. Accessed October 1, 2020.
- 28.Woodruff I.G., Mitchell R.D., Phillips G. COVID‐19 and the Indo-Pacific: implications for resource‐limited emergency departments. Med J Aust. 2020;213(8):345. doi: 10.5694/mja2.50750. [DOI] [PubMed] [Google Scholar]
- 29.Ayebare R.R., Flick R., Okware S., Bodo B., Lamorde M. Adoption of COVID-19 triage strategies for low-income settings. Lancet Respir Med. 2020;8(4):e22. doi: 10.1016/S2213-2600(20)30114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker T., Schell C.O., Petersen D.B. Essential care of critical illness must not be forgotten in the COVID-19 pandemic. Lancet. 2020;6736(20):19–20. doi: 10.1016/S0140-6736(20)30793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization . Health service delivery profile Papua New Guinea 2012. Port Moresby; 2012. Papua New Guinea Department of Health. [Google Scholar]
- 32.Howes S., Mako A.A., Swan A., Walton G., Webster T., Wiltshire C. Canberra; 2012. A lost decade? Service delivery and reforms in Papua New Guinea 2002-2012. [Google Scholar]
- 33.Mullan F., Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. Lancet. 2007;370(9605):2158–2163. doi: 10.1016/S0140-6736(07)60785-5. [DOI] [PubMed] [Google Scholar]
- 34.Mitchell R. The road to paradise: developing emergency medicine in the highlands of Papua New Guinea. Your ED. May 2019:28–30. [Google Scholar]
- 35.Curry C., Annerud C., Jensen S., Symmons D., Lee M., Sapuri M. The first year of a formal emergency medicine training programme in Papua New Guinea. Emerg Med Australas. 2004;16(4):343–347. doi: 10.1111/j.1742-6723.2004.00612.x. [DOI] [PubMed] [Google Scholar]
- 36.Phillips G.A., Hendrie J., Atua V., Manineng C. Capacity building in emergency care: an example from Madang, Papua New Guinea. Emerg Med Australas. 2012;24(5):547–552. doi: 10.1111/j.1742-6723.2012.01597.x. [DOI] [PubMed] [Google Scholar]
- 37.Phillips G., Bowman K., Sale T., O'Reilly G. A Pacific needs analysis model: a proposed methodology for assessing the needs of facility-based emergency care in the Pacific region. BMC Health Serv Res. 2020;20(1):560. doi: 10.1186/s12913-020-05398-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Emergency Medicine Society of South Africa. The South African Triage scale (SATS). https://emssa.org.za/special-interest-groups/the-south-african-triage-scale-sats/. Accessed September 12, 2020.
- 39.Western Highlands Provincial Health Authority. New emergency care system for Mt Hagen hospital. https://www.whhs.gov.pg/2019/05/new-emergency-care-system-for-mt-hagen-hospital/. Accessed September 1, 2019.
- 40.EMTV. New emergency care system trialed at Mt Hagen hospital. https://emtv.com.pg/new-emergency-care-system-trialed-at-mt-hagen-general-hospital/. Accessed November 1, 2019.
- 41.Peki R. Mt Hagen hospital pioneers new system. Post-Courier. November 6, 2019.
- 42.Rhodes D., Antoine E.Practitioners’ handbook for capacity development: a cross-cultural approach. Melbourne: Leadership Strategies. 2013.
- 43.Mowafi H., Ngaruiya C., O'Reilly G. Emergency care surveillance and emergency care registries in low-income and middle-income countries: conceptual challenges and future directions for research. BMJ Glob Heal. 2019;4:1–12. doi: 10.1136/bmjgh-2019-001442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cibulskis R., Hiawalyer G. Information systems for health sector monitoring in Papua New Guinea. Bull World Health Organ. 2002;80(9):752–758. [PMC free article] [PubMed] [Google Scholar]
- 45.Yamamoto T.S., Sunguya B.F., Shiao L.W., Amiya R.M., Saw Y.M., Jimba M. Migration of health workers in the Pacific islands. Asia Pacific J Public Heal. 2012;24(4):697–709. doi: 10.1177/1010539512453259. [DOI] [PubMed] [Google Scholar]
- 46.Worster A., Gilboy N., Fernandes C.M. Assessment of inter-observer reliability of two five-level triage and acuity scales: a randomized controlled trial. CJEM. 2004;6(04):240–245. doi: 10.1017/S1481803500009192. [DOI] [PubMed] [Google Scholar]
- 47.Australian Government Department of Health. Emergency Triage Education Kit. https://www1.health.gov.au/internet/main/publishing.nsf/Content/casemix-ED-Triage Review Fact Sheet Documents. Accessed April 1, 2019.
- 48.Mitchell R. PNG Medical Symposium Emergency Medicine Specialty Meeting. Port Moresby; 2019. Triage in Papua New Guinea: a collaborative development project. [Google Scholar]
- 49.Clark M., Spry E., Daoh K., Baion D., Skordis-Worrall J. Reductions in inpatient mortality following interventions to improve emergency hospital care in Freetown, Sierra Leone. Morgan D, editor. PLoS ONE. 2012;7(9):e41458. doi: 10.1371/journal.pone.0041458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dekker-Boersema J., Hector J., Jefferys L.F. Triage conducted by lay-staff and emergency training reduces paediatric mortality in the emergency department of a rural hospital in Northern Mozambique. Afr J Emerg Med. 2019;9(4):172–176. doi: 10.1016/j.afjem.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.