Abstract
Background
While optimal cardiovascular risk factor (CRF) profile is associated with lower mortality, morbidity, and healthcare expenditures among individuals with atherosclerotic cardiovascular disease (ASCVD), less is known regarding its impact on financial hardship from medical bills. Therefore, we assessed whether an optimal CRF profile is associated with a lower burden of financial hardship from medical bills and a reduction in cost-related barriers to health.
Methods
We used a nationally representative sample of adults between 18 and 64 years from the National Health Interview Survey between 2013 and 2017. We assessed ASCVD status and the number of risk factors to categorize the study population into 4 mutually exclusive categories: ASCVD (irrespective of CRF profile) and non-ASCVD with poor, average, and optimal CRF profile. Adjusted logistic regression model was used to determine the association of ASCVD/CRF profile with financial hardship from medical bills and cost-related barriers to health (cost-related medication non-adherence (CRN), foregone/delayed care, and high financial distress).
Results
We included 119,388 non-elderly adults, representing 189 million individuals annually across the United States. Non-ASCVD/optimal CRF profile individuals had a lower prevalence of financial hardship and an inability paying medical bills when compared with individuals with ASCVD (24% vs 45% and 6% vs 19%, respectively). Among individuals without ASCVD and an optimal CRF profile, the prevalence of each cost-related barrier to health was <50% compared with individuals with ASCVD. Poor/low income and uninsured individuals within non-ASCVD/average CRF profile strata had a lower prevalence of financial hardship and an inability paying medical bills when compared with middle/high income and insured individuals with ASCVD. Non-ASCVD individuals with optimal CRF profile had the lowest odds of all barriers to health.
Conclusion
Optimal CRF profile is associated with a lower prevalence of financial hardship from medical bills and cost-related barriers to health despite lower income and lack of insurance.
Keywords: Cardiovascular disease, Cost, Financial hardship, Outcomes, Risk factors
Highlights
-
•
Nearly 1 in 5 individuals with ASCVD reported an inability to pay medical bills.
-
•
Only 6% of those with optimal CRF profile were unable to pay medical bills.
-
•
Optimal CRF profile had the lowest odds of all outcomes like high financial distress.
-
•
Worse outcomes among individuals with poor/low income and lack of insurance.
-
•
Optimal CRF profile was protective despite poor/low income and lack of insurance.
1. Introduction
Atherosclerotic cardiovascular disease (ASCVD) remains a leading cause of morbidity and mortality in the United States and around the world. Patients with ASCVD endure significant financial burden from direct and indirect medical costs, life-years lost, and diminished quality of life related to their condition [1]. In 2010, the American Heart Association launched the 2020 Strategic Impact Goals, which defined the concept of ideal cardiovascular health (CVH), including adequate management of hypertension, diabetes, and total cholesterol, smoking abstinence, maintaining a healthy weight and diet, and engaging in physical activity [2]. It is now well established that an optimal cardiovascular risk factor (CRF) profile, as a measure of CVH, is associated with favorable cardiovascular outcomes, including lower mortality and morbidity rates [[3], [4], [5], [6]], as well as decreased healthcare expenditures and cardiovascular costs later in life, regardless of ASCVD status [[7], [8], [9]]. To date, however, less is known whether an optimal CRF profile is associated with lower financial hardship among affected individuals. Therefore, in this study we sought to describe financial hardship from medical bills across the spectrum of varying CRF profiles and an ASCVD status from a nationally representative sample of adults in the United States (US). Additionally, we analyzed cost-related consequences and barriers affecting individuals’ health, such as cost-related medication non-adherence (CRN), foregone/delayed care, and high financial distress.
2. Materials & methods
2.1. Study design
We utilized pooled, cross-sectional data from the National Health Interview Survey (NHIS) between 2013 and 2017. The NHIS is a National Center for Health Statistics/Center for Disease Control and Prevention database constructed from annual surveys, which incorporates complex, multi-stage sampling to provide estimates on the noninstitutionalized US population. This study was based on the Sample Adult Core files, which were supplemented with demographic and socioeconomic characteristics, health status, healthcare services, and health-related behaviors from the US adult population. Since NHIS data is publicly available as de-identified data, this study was exempt from the Institutional Review Board Committee. We limited our study to focus on non-elderly (18–64 years of age) adults with ASCVD status and CRF profile information to capture the population without universal public insurance, which may provide enhanced protection from the financial-related outcomes of interest.
2.2. Study variable
2.2.1. ASCVD and CRF profiles
Individuals who self-reported having coronary artery disease (answered “yes” to any of the following 3 questions: “Have you ever been told by a doctor or other health professional that you had … coronary heart disease? or … angina, also called angina pectoris? or … a heart attack (also called myocardial infarction)?”) and/or stroke disease (answered “yes” to the following question: “Have you ever been told by a doctor or other health professional that you had a stroke?”), were established as having ASCVD.
CRF profile was ascertained based on the presence of 1 or more of the following self-reported clinical characteristics: diagnosis of hypertension, diabetes mellitus, or high cholesterol, current smoker, obesity (body mass index ≥ 30 kg/m2), or insufficient physical activity (≥75 min/week of vigorous-intensity activity or ≥150 min/week moderate-intensity activity or combination) [2]. The sum of the risk factors an individual accrued was used to determine the CRF profile: “poor/unfavorable” (≥4 CRFs) and “favorable” (<4 CRFs) (“average” [2–3 CRFs] or “optimal” [0–1 CRF]).
2.3. Outcome variables
2.3.1. Financial hardship from medical bills
Individuals were classified as having “financial hardship from medical bills” if they answered “yes” to either of the following questions: “In the past 12 months did you/anyone in your family have problems paying or were unable to pay any medical bills? Include bills for doctors, dentists, hospitals, therapists, medication, equipment, nursing home or home care” and “Do you/anyone in your family currently have any medical bills that are being paid off over time? This could include medical bills being paid off with a credit card, through personal loans, or bill paying arrangements with hospitals or other providers. The bills can be from earlier years as well as this year.” Individuals who answered “yes” to having any problems paying bills were then asked a follow-up question: “Do you/Does anyone in your family currently have any medical bills that you are unable to pay at all?” Those who answered “yes” to the follow-up question were classified as “unable to pay medical bills at all”, a proxy of the most vulnerable individuals.
2.3.2. Cost-related barriers to health
Individuals who reported money-saving behaviors in the past 12 months as described in Table 1, were defined to have CRN. Individuals who reported to have delayed care or have not sought out care because they could not afford it or because they were worried about the costs in the past 12 months were defined to have foregone/delayed care (Table 1) [10]. Financial distress was derived from 6 questions addressing “worry” regarding several financial matters in the past 12 months as mentioned in Table 1. All questions were answered on a 4-point scale, ranging from 0 (not worried at all) to 4 (very worried). An aggregate score was created, ranging from 6 to 24, with a higher score translating into higher stress [11], which was divided into quartiles. Individuals among the highest quartile (i.e. those with the highest scores) were then classified as having high financial distress.
Table 1.
Itemized questions for Cost-related Barriers to Health.
| Cost-related Medication Non-adherence |
|---|
During the past 12 months, were any of the following true for you? (Yes/No)
|
|
Forgone/Delayed Care |
During the past 12 months, were any of the following true for you? (Yes/No)
|
|
High Financial Distress |
How worried (very worried, moderately worried, not too worried, not worried at all) are you right now about
|
2.4. Covariates
Other covariates included in this study were age (18–39 and 40–64 years), sex, family size (0, 1, and ≥2), family income (middle/high income [≥200% federal poverty limit] and low/poor-income [<200% federal poverty limit]), race/ethnicity (non-Hispanic white, non-Hispanic black, non-Hispanic Asian, and Hispanic), insurance status (insured and uninsured), education (at least some college education and less than college education), region (Northeast, Midwest, South, and West), and number of chronic comorbidities. Chronic comorbidities were self-reported and included emphysema, chronic obstructive pulmonary disease, asthma, gastrointestinal ulcer, cancer (any), arthritis (including arthritis, gout, fibromyalgia, rheumatoid arthritis, and systemic lupus erythematosus), any kind of liver condition, and “weak/failing” kidneys, were aggregated and categorized as having 0, 1, or ≥ 2.
2.5. Statistical analysis
We utilized data from the Integrated Public Use Microdata Series (http://www.ipums.org) to correctly calculate variance estimation for nationally representative results, since 5 years of pooled data were used for analysis. We divided the study population into 4 mutually exclusive groups based on the ASCVD status and CRF profile: ASCVD (irrespective of the CRF profile), non-ASCVD with poor CRF profile, non-ASCVD with average CRF profile, and non-ASCVD with optimal CRF profile. We compared the baseline characteristics of the study population using χ2 analysis across the pre-specified ASCVD/CRF profile groups and studied the prevalence using weighted proportions. We used logistic regression model adjusted for age, sex, family size, family income, race/ethnicity, insurance status, education, comorbidities, and region to calculate odds ratios to determine the association of ASCVD/CRF profile on financial hardship from medical bills, and cost-related barriers to health (CRN, foregone/delayed care, and high financial distress). Additionally, we conducted a sub-analysis among participants with ASCVD stratified by CRF profile status to ascertain unadjusted and adjusted associations with financial hardship from medical bills, an inability to pay bills at all, along with the aforementioned barriers to health. We performed all statistical analyses using Stata®, version 15.1 (StataCorp, LP, College Station, Texas, USA). A two-tailed p-value of <0.05 was considered statistically significant for all analyses. All analyses were survey-specific and considered the complex NHIS survey design.
3. Results
Our study population consisted of 119,388 individuals (between 18 and 64 years), representing 72% of total cohort surveyed by NHIS from 2013 to 2017. This sample represented 189 million non-elderly US adults annually. Mean age was 41 ± 7.7 years and 49% were men. Overall, 4.6% (95% CI: 4.4%, 4.8%) of the weighted study population had ASCVD. Among those without ASCVD, 6% had a poor CRF profile, 31.8% average CRF profile, and 57.6% optimal CRF profile. General characteristics of the study population are displayed in Table 2. Non-ASCVD/optimal CRF profile individuals were younger (18–39 years old), from middle/high income families, with a lower comorbidity count, and were more likely to have at least some college education when compared to individuals with ASCVD.
Table 2.
General characteristics of the study population by ASCVD and non-ASCVD/CRF profile status.
| Total | ASCVD | No ASCVD |
p-value | |||
|---|---|---|---|---|---|---|
| Poor CRF Profile |
Average CRF Profile |
Optimal CRF Profile |
||||
| Sample (N) | 119,388 | 6160 | 7878 | 38,768 | 66,582 | |
| Weighted sample, (weighted %) | 188,861,117 | 8,696,486 (4.6) | 11,381,648 (6.0) | 60,102,341 (31.8) | 108,680,642 (57.6) | |
| Age Category, n (weighted %) | <0.001 | |||||
| 18-39 | 54,192 (47.6) | 684 (12.4) | 1061 (13.9) | 14,010 (37.9) | 38,437 (59.3) | |
| 40-64 | 65,196 (52.4) | 5476 (87.6) | 6817 (86.1) | 24,758 (62.1) | 28,145 (40.7) | |
| Sex, n (weighted %) | <0.001 | |||||
| Male | 55,045 (49.0) | 3317 (57.5) | 3445 (47.7) | 17,661 (49.3) | 30,622 (48.3) | |
| Female | 64,343 (51.0) | 2843 (42.5) | 4433 (52.3) | 21,107 (50.7) | 35,960 (51.7) | |
| Race/Ethnicity, n (weighted %) | <0.001 | |||||
| Non-Hispanic White | 73,736 (63.4) | 3945 (67.1) | 4844 (65.8) | 23,632 (63.1) | 41,315 (62.9) | |
| Non-Hispanic Black | 16,316 (12.9) | 1118 (16.4) | 1583 (17.3) | 6207 (14.8) | 7408 (11.2) | |
| Non-Hispanic Asian | 7219 (6.2) | 159 (2.8) | 197 (2.8) | 1571 (4.5) | 5292 (7.7) | |
| Hispanic | 20,466 (17.5) | 799 (13.7) | 1093 (14.1) | 6725 (17.5) | 11,849 (18.1) | |
| Family Size, n (weighted %) | <0.001 | |||||
| 1 | 36,025 (17.0) | 2423 (22.9) | 2768 (19.6) | 10,970 (15.7) | 19,864 (17.0) | |
| 2 | 33,903 (28.8) | 2095 (38.1) | 2682 (37.5) | 11,775 (30.6) | 17,351 (26.2) | |
| ≥3 | 49,460 (54.2) | 1642 (39.0) | 2428 (42.9) | 16,023 (53.7) | 29,367 (56.8) | |
| Family Income, n (weighted %) | <0.001 | |||||
| Middle/High-Income | 71,353 (68.6) | 2690 (53.8) | 4001 (59.8) | 21,843 (64.5) | 42,819 (73.0) | |
| Poor/Low-Income | 41,033 (31.4) | 3137 (46.2) | 3474 (40.2) | 14,561 (35.5) | 19,861 (27.0) | |
| Insurance Status, n (weighted %) | <0.001 | |||||
| Insured | 100,559 (85.5) | 5407 (88.2) | 6908 (88.3) | 31,890 (83.5) | 56,354 (86.2) | |
| Uninsured | 18,268 (14.5) | 731 (11.8) | 944 (11.7) | 6724 (16.5) | 9869 (13.8) | |
| Education, n (weighted %) | <0.001 | |||||
| Some College or Higher | 76,488 (64.2) | 3057 (51.1) | 3902 (50.3) | 21,988 (56.8) | 47,541 (70.8) | |
| HS/GED or Less than HS | 42,513 (35.8) | 3081 (48.9) | 3939 (49.7) | 16,613 (43.2) | 18,880 (29.2) | |
| Region, n (weighted %) | <0.001 | |||||
| Northeast | 18,904 (17.4) | 907 (15.2) | 1154 (15.8) | 5943 (16.7) | 10,900 (18.1) | |
| Midwest | 25,812 (22.4) | 1370 (24.4) | 1810 (24.1) | 8872 (23.7) | 13,760 (21.4) | |
| South | 42,569 (36.5) | 2588 (42.4) | 3228 (41.5) | 14,602 (38.8) | 22,151 (34.3) | |
| West | 32,103 (23.7) | 1295 (18.0) | 1686 (18.6) | 9351 (20.7) | 19,771 (26.3) | |
| Comorbidities, n (weighted %) | <0.001 | |||||
| 0 | 76,882 (66.2) | 1880 (32.7) | 2886 (38.4) | 22,891 (61.0) | 49,225 (74.6) | |
| 1 | 29,432 (24.1) | 1862 (31.0) | 2755 (35.1) | 10,878 (27.4) | 13,937 (20.6) | |
| ≥2 | 13,074 (9.7) | 2418 (36.3) | 2237 (26.5) | 4999 (11.6) | 3420 (4.8) | |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor; HS, high school; GED, general equivalency diploma.
3.1. Burden of ASCVD and non-ASCVD/CRF profile on financial hardship
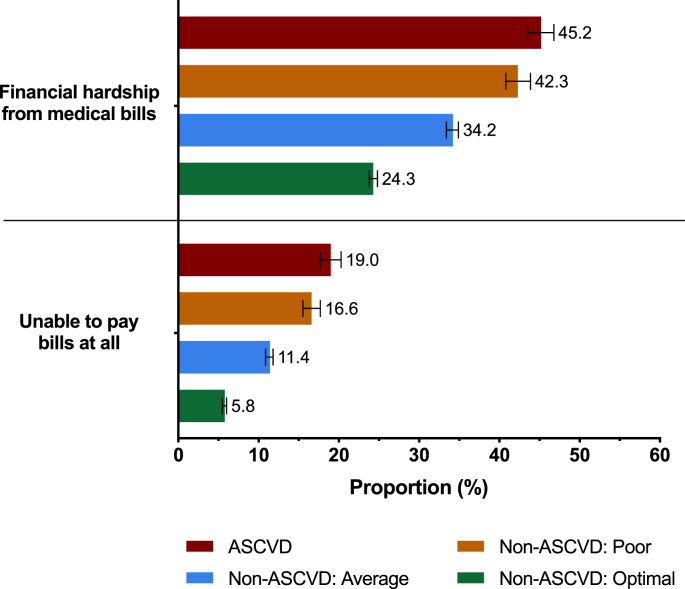
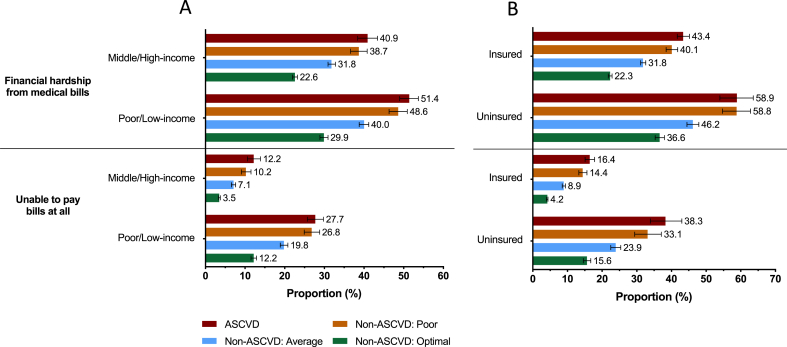
Fig. 1 depicts the prevalence of financial hardship from medical bills and an inability to pay bills. Nearly half (45.2%) of the individuals with ASCVD had financial hardship from medical bills and 19% were unable to pay medical bills at all. In contrast, individuals without ASCVD and an optimal CRF profile had a lower prevalence of financial hardship from medical bills (24.3%) and an inability paying medical bills (5.8%). Among ASCVD and non-ASCVD/poor CRF profile individuals, the prevalence of being unable to pay medical bills at all was 40% of those with financial hardship from medical bills when compared to only 24% among non-ASCVD/optimal CRF profile individuals. There was a stepwise decrease in the prevalence of financial hardship measures with improving CRF among those without ASCVD. These differences persisted among specific subpopulations as shown in Fig. 2. We found a higher prevalence of financial hardship and an inability to pay bills at all among those with lower income and without insurance coverage across ASCVD/CRF profile strata. Furthermore, individuals with ASCVD among middle/high income and insured strata, reported a higher prevalence of financial hardship from medical bills and an inability paying medical bills compared to non-ASCVD/average CRF profile individuals among poor/low income and uninsured strata.
Fig. 1.
Title: Prevalence of Financial Hardship from Medical Bills among Non-Elderly Adults by ASCVD and Non-ASCVD/CRF Profile Status.
There was a stepwise increase in the prevalence of financial hardship from medical bills and an inability to pay bills at all with worsening CRF profile.
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor.
Fig. 2.
Title: Prevalence of Financial Hardship from Medical Bills by (A), family income (B), insurance status among Non-Elderly Adults by ASCVD and Non-ASCVD/CRF Profile Status.
Within each CRF profile strata, individuals with lower income and lack of insurance had a higher prevalence of financial hardship from medical bills and an inability to pay bills at all when compared with individuals with higher income and insurance coverage.
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor.
Table 3 details the adjusted odds ratios for financial hardship from medical bills across the spectrum of ASCVD and CRF profile. Individuals without ASCVD but with a favorable CRF profile (optimal CRF profile: OR 0.44, 95% CI [0.41, 0.48]; average CRF profile: OR 0.66, 95% CI [0.61, 0.72]) had significantly lower odds of having financial hardship from medical bills when compared to individuals with ASCVD; the association was similar for being unable to pay medical bills (Table 3). On the other hand, those without established ASCVD and poor CRF profile had similar odds of experiencing financial hardship from medical bills (OR 0.90, 95% CI [0.82, 0.99]) or an inability paying medical bills (OR 0.89, 95% CI [0.78, 1.01]) as that of ASCVD individuals. This trend of lower odds of financial hardship and an inability to pay medical bills in association with a more favorable CRF profile persisted among all patient and disease-related covariates (Tables S1 & S2).
Table 3.
Odds ratios of financial hardship among non-elderly adults by ASCVD and non-ASCVD/CRF profile status.
| ASCVD |
No ASCVD |
|||
|---|---|---|---|---|
| Poor CRF Profile |
Average CRF Profile |
Optimal CRF Profile |
||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Financial Hardship from Medical Bills | ||||
| Model 1 | Reference | 0.89 (0.81, 0.97) | 0.63 (0.59, 0.68) | 0.39 (0.36, 0.42) |
| Model 2 | 0.90 (0.82, 0.99) | 0.66 (0.61, 0.72) | 0.44 (0.41, 0.48) | |
| Unable to Pay Medical Bills at All | ||||
| Model 1 | Reference | 0.83 (0.74, 0.93) | 0.50 (0.45, 0.55) | 0.22 (0.20, 0.24) |
| Model 2 | 0.89 (0.78, 1.01) | 0.56 (0.49, 0.63) | 0.30 (0.26, 0.34) | |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor; OR, odds ratios; CI, confidence interval.
Model 1: unadjusted model.
Model 2: adjusted for age, sex, race/ethnicity, geographic region, comorbidities, family size, family income, education, and insurance status.
3.2. Burden of ASCVD and non-ASCVD/CRF profile on cost-related barriers to health
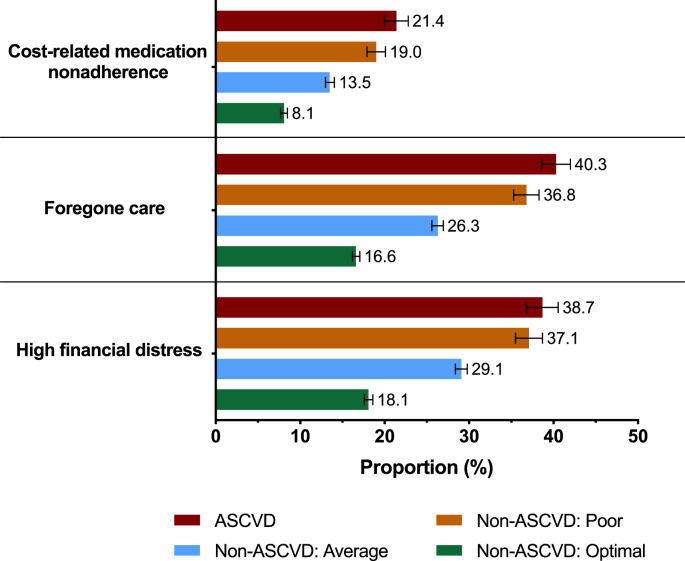
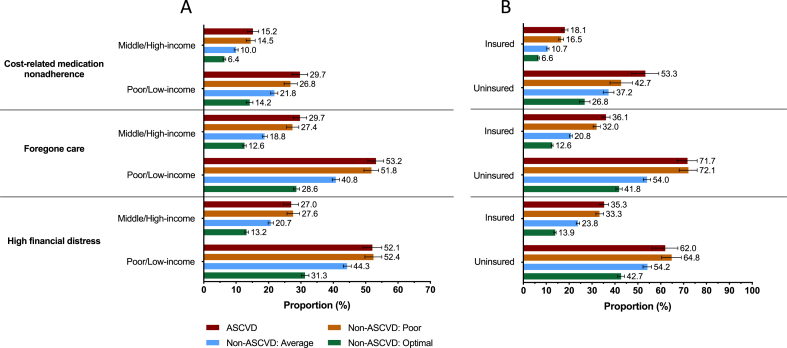
Overall, all cost-related barriers to health measures were most prevalent among individuals with ASCVD followed by non-ASCVD individuals with poor CRF profile (Fig. 3). These differences persisted among specific subpopulations (Fig. 4), with a higher prevalence among those with lower income and without insurance coverage. After accounting for demographic and social risk factors, those without ASCVD and optimal CRF profile individuals had the lowest odds of having CRN (OR 0.42, 95% CI [0.38, 0.48]), foregone/delayed care (OR 0.41 95% CI [0.37, 0.45]), and high financial distress (OR 0.52, 95% CI [0.47, 0.58]), when compared to individuals with ASCVD. Conversely, those without ASCVD and poor CRF had similar odds of experiencing all cost-related barriers to health when compared to individuals with ASCVD (Table 4).
Fig. 3.
Title: Prevalence of Cost-Related Barriers to Health among Non-Elderly Adults by ASCVD and Non-ASCVD/CRF Profile Status.
There was a stepwise increase in cost-related medication non-adherence, foregone/delayed care, and high financial distress with worsening CRF profile.
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor.
Fig. 4.
Title: Prevalence of Cost-Related Barriers to Health by (A), family income (B), insurance status among Non-Elderly Adults by ASCVD and Non-ASCVD/CRF Profile Status.
Within each CRF profile strata, individuals with lower income and lack of insurance had a higher prevalence of cost-related medication non-adherence, foregone/delayed care, and high financial distress when compared with individuals with higher income and insurance coverage.
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor.
Table 4.
Odds ratios of cost-related barriers to health among non-elderly adults by ASCVD and non-ASCVD/CRF profile status.
| ASCVD |
No ASCVD |
|||
|---|---|---|---|---|
| Poor CRF Profile |
Average CRF Profile |
Optimal CRF Profile |
||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Cost-Related Medication Non-Adherence | ||||
| Model 1 | Reference | 0.86 (0.77, 0.97) | 0.58 (0.52, 0.63) | 0.32 (0.29, 0.36) |
| Model 2 | 0.91 (0.80, 1.03) | 0.66 (0.59, 0.73) | 0.42 (0.38, 0.48) | |
| Foregone/Delayed care | ||||
| Model 1 | Reference | 0.86 (0.78, 0.95) | 0.53 (0.49, 0.57) | 0.30 (0.27, 0.32) |
| Model 2 | 0.94 (0.84, 1.04) | 0.63 (0.58, 0.69) | 0.41 (0.37, 0.45) | |
| High Financial Distress | ||||
| Model 1 | Reference | 0.94 (0.85, 1.03) | 0.65 (0.60, 0.71) | 0.35 (0.32, 0.38) |
| Model 2 | 1.02 (0.91, 1.14) | 0.79 (0.72, 0.87) | 0.52 (0.47, 0.58) | |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CRF, cardiovascular risk factor; OR, odds ratios; CI, confidence interval.
Model 1: Unadjusted Model.
Model 2: adjusted for age, sex, race/ethnicity, geographic region, comorbidities, family size, family income, education, and insurance status.
3.3. Burden of CRF profile within ASCVD on financial hardship and cost-related barriers to health
In a sub-analysis among those with ASCVD, we noticed a stepwise decrease in the prevalence of all measures of financial hardship and cost-related barriers to health with improving CRF profile. Notably, the prevalence of being unable to pay medical bills at all and CRN were 50% lower among individuals with ASCVD and optimal CRF profile when compared with individuals with ASCVD and poor CRF profile (unable to pay medical bills at all: 11.5% vs 23.4%; CRN: 14.8% vs 27.3%). Figures S1 & S2 illustrate the prevalence the outcomes by ASCVD and CRF profile status. These differences persisted after accounting for demographic and socioeconomic determinants of health (Table S3).
4. Discussion
In a nationally representative sample of US non-elderly adults, we demonstrated that a favorable CRF profile was associated with lower financial hardship from medical bills along with a reduction in previously described barriers to health including CRN, foregone/delayed care, and high financial distress. Notably, we found that these results persisted among all family income and insurance strata. Finally, our results showed that an optimal CRF profile was inversely associated with financial hardship from medical bills and an inability to pay medical bills at all despite a lower income level and lack of insurance coverage.
In recent years with rising healthcare costs, financial burden incurred by patients and their families from medical bills has drawn significant national attention. It is now well established that individuals with ASCVD face a particularly high healthcare-related financial burden [12,13], with 1 in 10 families that have a member with ASCVD spending more than one-third of their income on health-related expenses [13]. These expenses can represent major financial challenges to patients, regardless of their insurance status, and can lead to a reduction in overall quality of health and psychological well-being along with other cost-related consequences and tradeoffs such as high financial distress, medication non-adherence, and foregone/delayed medical care [14,15]. The burden of financial hardship among individuals with ASCVD is worsened in the presence of other comorbid conditions such as diabetes mellitus [16], [29].
Established risk factors of cardiovascular disease – many of which can be effectively modified, treated, or controlled – are important drivers of death and disability. Due to their significance and overall burden, the AHA’s 2020 Strategic Impact Goals emphasized the importance of optimizing these risk factors as part of a national goal, to reduce CVD morbidity, mortality, and economic burden. In recent years, multiple reports have attempted to estimate the potential economic impact of a favorable CRF profile. Notably, Willis et al. studied the relationship between cardiovascular status, ideal cardiovascular metrics and healthcare utilization in middle-aged individuals, and later-life healthcare costs [8]. They found that overall healthcare expenditures were significantly lower among those with a favorable CV health status. Similarly, Sullivan et al. demonstrated that individuals without cardiometabolic risk factor clusters, on average, spent $5477 less on healthcare when compared with those with cardiometabolic risk factor clusters [17]. In a nationally representative US adult population, Valero-Elizondo et al. demonstrated lower out-of-pocket costs among those with optimal CRF profile irrespective of ASCVD status [7]. Importantly, these benefits were noted across all socioeconomic groups including those <65 years old.
Our current study adds to the existing literature by documenting significantly lower financial hardship measures among those with a favorable CRF status. Findings from our study reiterate the advantages conferred by an optimal CRF profile beyond lower incidence and mortality from chronic diseases (including diabetes [18], cancer [19,20], end-stage renal disease [21], and cardiovascular disease [22,23]) and lower healthcare expenditures and resource utilization [[7], [8], [9],24]. Our results further emphasize the importance of preventing and managing modifiable risk factors, irrespective of underlying CVD status for the overall health at individual, family, and community levels, in addition to the economic benefits at the national level.
Our findings also provide insights that secondary prevention among individuals with ASCVD is equally important as primordial prevention in protecting one’s family from financial burden and other cost-related barriers to accessing healthcare services. In our study, we demonstrated that, among individuals with ASCVD, those with optimal CRF profile had significantly lower odds of these cost-related consequences than those with poor CRF profile. These findings underscore the importance of closely managing cardiovascular risk factors and behaviors among those with ASCVD to improve the overall cardiovascular health and financial stability of an individual and his or her family.
The management costs of ASCVD are substantial and constitute a major source of concern at both the national and individual level. While, attainment of an optimal CRF profile is associated with an overall relative reduction in financial hardship, we noted greater burden among those who lacked health insurance and those with lower family income. In fact, uninsured and lower income individuals with optimal CRF reported similar burden of financial hardship such as an inability to pay medical bills, CRN, foregone medical care, and financial distress as compared to insured and middle/high incomes individuals with established ASCVD. Our study results provide an impetus for health policy advocates and other stakeholders on the benefits of an upfront investment in ASCVD primordial and primary prevention. However, the significant risk of financial hardship cannot be fully addressed without widening the scope of insurance coverage and further limiting out-of-pocket expenditures for the most vulnerable segments of our society. Further, it is critical to carefully evaluate the complex, multidirectional interplay between financial hardship, cardiovascular risk factors, and social determinants of health. Considering the heightened risk of cardiovascular risk factors, comorbidities, and adverse cardiac events and outcomes among individuals experiencing financial hardship from medical bills, it is imperative to not only strive to improve CRF profiles in the general population and particularly in low-resource settings, but also to concurrently address the sociodemographic inequities themselves through focused public health interventions and effective public policy reform.
Developing and sustaining effective, patient-centered public health interventions is critical for alleviating the burden and consequences of cardiovascular risk factors in vulnerable and low-resource communities. In recent years, community-based health workers (CBHW) have gained attention for their ability promote healthy behaviors and positive outcomes in underserved settings. Notably, a systematic review conducted by Kim and colleagues found that the utilization of CMHW interventions was associated with significant cardiovascular risk reduction and that the roles of CMHW’s included health education, counseling, case management, social services, and support [25]. Another review of the current literature found that the most commonly implemented community-based cardiovascular interventions included education followed by counseling or support and exercise classes, with more than half of interventions having multiple components [26]. Behavior change interventions were found to be the most challenging to implement while programs developed to decrease blood pressure were the most effective. Future research studies and public health interventions may derive benefit from integrating components of the conceptual framework on patient centered access to healthcare produced by Khanassov et al. describing core tenants of improving healthcare access in low-resource settings such as approachability, acceptability, availability, and affordability [27].
Our results should be interpreted given the following limitations. The cross-sectional nature of our study precludes the establishment of causal relationship between our studied outcomes and ASCVD or poor CRF profile status. For example, poor cardiovascular health can predispose a family to overall financial hardship due to excessive out-of-pocket healthcare costs, while similarly financial hardship from medical bills may be a contributor to financial difficulties for any given individual or family, predisposing to poor cardiovascular health. Therefore, a bilateral causal relationship is plausible, and it is crucial to note that financial hardship and poor cardiovascular health can cause and progressively worsen each other with poor social determinants of health serving as the root cause for either of them. This can be explained by the higher prevalence of ASCVD, poor CRF profile as well as financial hardship from medical bills and other cost-related barriers to health among lower socio-economic (lower education and income) and uninsured families in our study. Second, since all the information regarding the study variables was obtained through self-reported surveys, there is a potential for recall bias. Therefore, underestimation of the true national prevalence of ASCVD and modifiable risk factor status is likely, as described previously, especially in chronic conditions [28]. Third, we were unable to calculate the ideal CVH status as defined by American Heart Association due to lack of dietary information and clinical values of other relevant health factors.
In conclusion, we found that a favorable CRF profile is directly associated with a significantly lower prevalence of financial hardship from medical bills and other cost-related barriers to health, findings that support nationwide policies focusing on preventing and managing modifiable risk factors, irrespective of underlying CVD status.
Disclosures
The authors declare that they have no conflicts of interest relevant to the content of this manuscript.
Declaration of competing interest
Dr. Khera is supported by the National Heart, Lung, and Blood Institute (grant 5T32HL125247-02) and the National Center for Advancing Translational Sciences (grant UL1TR001105) of the National Institutes of Health. Dr. Virani has received research grants from the Department of Veterans Affairs, American Heart Association, American Diabetes Association, and World Heart Federation; and has received honoraria from the American College of Cardiology (Associate Editor for Innovations, acc.org). Dr. Desai is supported by grant K12 HS023000-01 from the Agency for Healthcare Research and Quality; has received research funding from the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are used for public reporting; and support from Johnson & Johnson and Medtronic, through Yale University, to develop methods of clinical trial data sharing. Dr. Nasir has received support from the Katz Academy for Translational Research. All other authors have reported that they have no relationships relative to the contents of this paper to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajpc.2020.100034.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Benjamin E.J., Blaha M.J., Chiuve S.E. Heart disease and stroke statistics-2017 update: a report from the American heart association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd-Jones D.M., Hong Y., Labarthe D. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 3.Berry J.D., Dyer A., Cai X. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329. doi: 10.1056/NEJMoa1012848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lloyd-Jones D.M., Leip E.P., Larson M.G. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 Years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 5.Stampfer M.J., Hu F.B., Manson J.E., Rimm E.B., Willett W.C. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343:16–22. doi: 10.1056/NEJM200007063430103. [DOI] [PubMed] [Google Scholar]
- 6.Wilkins J.T., Ning H., Berry J., Zhao L., Dyer A.R., Lloyd-Jones D.M. Lifetime risk and years lived free of total cardiovascular disease. J Am Med Assoc. 2012;308:1795–1801. doi: 10.1001/jama.2012.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valero-Elizondo J., Salami J.A., Ogunmoroti O. Favorable cardiovascular risk profile is associated with lower healthcare costs and resource utilization: the 2012 medical expenditure panel survey. Circ Cardiovasc Qual Outcomes. 2016;9:143–153. doi: 10.1161/CIRCOUTCOMES.115.002616. [DOI] [PubMed] [Google Scholar]
- 8.Willis B.L., DeFina L.F., Bachmann J.M. Association of ideal cardiovascular health and long-term healthcare costs. Am J Prev Med. 2015;49:678–685. doi: 10.1016/j.amepre.2015.03.034. [DOI] [PubMed] [Google Scholar]
- 9.Singh J., Valero-Elizondo J., Salami J.A. Favorable modifiable cardiovascular risk profile is associated with lower healthcare costs among cancer patients: the 2012-2013 medical expenditure panel survey. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.007874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kent E.E., Forsythe L.P., Yabroff K.R. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119:3710–3717. doi: 10.1002/cncr.28262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel M.R., Piette J.D., Resnicow K., Kowalski-Dobson T., Heisler M. Social determinants of health, cost-related nonadherence, and cost-reducing behaviors among adults with diabetes: findings from the national health Interview survey. Med Care. 2016;54:796–803. doi: 10.1097/MLR.0000000000000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khera R., Hong J.C., Saxena A. Burden of catastrophic health expenditures for acute myocardial infarction and stroke among uninsured in the United States. Circulation. 2018;137:408–410. doi: 10.1161/CIRCULATIONAHA.117.030128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khera R., Valero-Elizondo J., Okunrintemi V. Association of out-of-pocket annual health expenditures with financial hardship in low-income adults with atherosclerotic cardiovascular disease in the United States. JAMA Cardiol. 2018;3:729–738. doi: 10.1001/jamacardio.2018.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Annapureddy A., Valero-Elizondo J., Khera R. Association between financial burden, quality of life, and mental health among those with atherosclerotic cardiovascular disease in the United States. Circ Cardiovasc Qual Outcomes. 2018;11 doi: 10.1161/CIRCOUTCOMES.118.005180. [DOI] [PubMed] [Google Scholar]
- 15.Valero-Elizondo J., Khera R., Saxena A. Financial hardship from medical bills among nonelderly U.S. Adults with atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2019;73:727–732. doi: 10.1016/j.jacc.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Mszar R., Grandhi G.R., Valero-Elizondo J. Cumulative burden of financial hardship from medical bills across the spectrum of diabetes mellitus and atherosclerotic cardiovascular disease among non-elderly adults in the United States. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.119.015523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sullivan P.W., Ghushchyan V., Wyatt H.R., Hill J.O. The medical cost of cardiometabolic risk factor clusters in the United States. Obesity (Silver Spring) 2007;15:3150–3158. doi: 10.1038/oby.2007.375. [DOI] [PubMed] [Google Scholar]
- 18.Joseph J.J., Echouffo-Tcheugui J.B., Carnethon M.R. The association of ideal cardiovascular health with incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Diabetologia. 2016;59:1893–1903. doi: 10.1007/s00125-016-4003-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foraker R.E., Abdel-Rasoul M., Kuller L.H. Cardiovascular health and incident cardiovascular disease and cancer: the women’s health initiative. Am J Prev Med. 2016;50:236–240. doi: 10.1016/j.amepre.2015.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rasmussen-Torvik L.J., Shay C.M., Abramson J.G. Ideal cardiovascular health is inversely associated with incident cancer: the Atherosclerosis Risk in Communities study. Circulation. 2013;127:1270–1275. doi: 10.1161/CIRCULATIONAHA.112.001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rebholz C.M., Anderson C.A., Grams M.E. Relationship of the American heart association’s impact goals (Life’s Simple 7) With Risk of Chronic Kidney Disease: results From the Atherosclerosis Risk in Communities (ARIC) Cohort Study. J Am Heart Assoc. 2016;5 doi: 10.1161/JAHA.116.003192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Folsom A.R., Yatsuya H., Nettleton J.A. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ford E.S., Greenlund K.J., Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feldman D.I., Valero-Elizondo J., Salami J.A. Favorable cardiovascular risk factor profile is associated with lower healthcare expenditure and resource utilization among adults with diabetes mellitus free of established cardiovascular disease: 2012 Medical Expenditure Panel Survey (MEPS) Atherosclerosis. 2017;258:79–83. doi: 10.1016/j.atherosclerosis.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Kim K., Choi J.S., Choi E. Effects of Community-Based Health Worker Interventions to Improve Chronic Disease Management and Care Among Vulnerable Populations: A Systematic Review. Am J Public Health. 2016;106:e3–e28. doi: 10.2105/AJPH.2015.302987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walton-Moss B., Samuel L., Nguyen T.H., Commodore-Mensah Y., Hayat M.J., Szanton S.L. Community-based cardiovascular health interventions in vulnerable populations: a systematic review. J Cardiovasc Nurs. 2014;29:293–307. doi: 10.1097/JCN.0b013e31828e2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khanassov V., Pluye P., Descoteaux S. Organizational interventions improving access to community-based primary health care for vulnerable populations: a scoping review. Int J Equity Health. 2016;15 doi: 10.1186/s12939-016-0459-9. 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Evaluation of National Health Interview Survey diagnostic reporting. Vital Health Stat. 1994;2 1-116. [PubMed] [Google Scholar]
- 29.Caraballo C., Valero-Elizondo J., Khera R. Burden and Consequences of Financial Hardship From Medical Bills Among Nonelderly Adults With Diabetes Mellitus in the United States. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.119.006139. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.