Abstract
Objectives
Patients with severe hyperlipidemia (low-density lipoprotein-cholesterol (LDL-C) ≥190 mg/dL) have a significantly increased risk of cardiovascular disease (CVD) and are more likely to have familial hypercholesterolemia (FH). We sought to determine how often health care providers recognize the implications of and adjust therapy for an LDL-C ≥190 mg/dL.
Methods
We conducted a retrospective review of patients with an LDL-C measurement in the medical record of a large health care system between November 2015 and June 2016. Patients were restricted to those with LDL-C ≥190 mg/dL and without secondary causes of dyslipidemia, with sensitivity analyses for those with LDL-C ≥220 mg/dL.
Results
Of 27,963 patients, 227 had LDL-C ≥190 mg/dL. Only 21% were on a statin at the time of LDL-C measurement. More than 90% had a follow-up clinic visit, but 41% had no change in treatment. FH was only included in the differential for 14%. The presence/absence of a family history of dyslipidemia, myocardial infarction, and premature CVD were documented in 26%, 29%, and 31%. Only 20.7% and 22.1% had documentation of the presence or absence of tendinous xanthomas or corneal arcus, respectively. Among those without prior specialist care (cardiologist or endocrinologist), only 13% were referred. These measures were only slightly better for those with LDL-C ≥220 mg/dL.
Conclusion
In a large health care system, the possibility of FH was rarely acknowledged in those with residual LDL-C ≥190 mg/dL, few were referred to specialists, and therapeutic adjustments were suboptimal. Additional efforts are required to understand barriers to improving the evaluation and management of patients with LDL-C ≥190 mg/dL.
Keywords: Hyperlipidemia, Familial hypercholesterolemia, Prevention
Introduction
Severe hyperlipidemia, defined as having a low-density lipoprotein-cholesterol (LDL-C) ≥190 mg/dL, is a major risk factor for coronary heart disease (CHD) and other cardiovascular diseases (CVD). One study demonstrated that such individuals have up to a 5 fold increased risk of CHD in their lifetimes and developed CHD 10–20 years earlier [1]. Current cholesterol guidelines recommend high-intensity statin treatment for patients with an LDL-C ≥190 mg/dL [2], as this lipid-lowering therapy can significantly reduce morbidity and mortality [3].
An important consideration in those with an LDL-C ≥190 mg/dL is the potential diagnosis of familial hypercholesterolemia (FH) [4,5]. FH is an autosomal dominant disorder that causes premature CVD due to lifelong elevated LDL-C [5,6]. The heterozygous form of FH is estimated to occur in 1 in 250 to 1 in 500 people, while the incidence of the homozygous form is 1 in 250,000 to 1 in 1 million [5,7,8]. There are at least 20 million people with FH worldwide, but 80% are unaware of their diagnosis, and only a small proportion of those diagnosed receive optimal therapy [5,9].
It is estimated that approximately 7% of those with LDL-C ≥190 mg/dL would meet diagnostic criteria for FH, with an increasing prevalence at higher LDL-C thresholds (i.e. LDL-C ≥220) [10]. Current society recommendations encourage consideration for FH in those with LDL-C ≥190 mg/dL [4,5], both due to the higher likelihood of FH in this group and because earlier treatment in those with FH can abrogate the cardiovascular effects. Further, identification of FH facilitates cascade screening of family members allowing for earlier diagnosis.
It remains unclear the extent to which health care providers recognize the implications of an LDL-C ≥190 mg/dL and adjust therapy in response to residual LDL-C ≥190 mg/dL. In order to improve the diagnosis and treatment of FH, there needs to be an increased awareness and a better understanding of current practice patterns in regards to the evaluation and management of patients with an LDL-C ≥190 mg/dL.
Methods
Study population
We conducted a retrospective review of patients with a lipid panel recorded in the University of Texas Southwestern Medical Center electronic medical record (EMR) between November 2015 and June 2016. The study was approved by the Institutional Review Board of the University of Texas at Southwestern Medical Center, Dallas, TX with waiver of informed consent. A flow diagram of patient selection method is displayed in Supplemental Fig. S1. Patients were restricted to those with an LDL-C ≥190 mg/dL. Those with an LDL-C <190 (treated or untreated) were not included. Those with extensive missing chart information (medical record numbers that did not correspond to a patient chart or charts without any notes, medications, or lab values) and those with secondary causes of LDL-C elevation were excluded. Secondary causes included: 1) nephrotic syndrome, 2) cholestasis, 3) hypothyroidism, 4) treatment with cyclosporine, 5) treatment with tacrolimus, sirolimus, or everolimus, 6) treatment with Accutane, and 7) ketogenic diet [11].
Clinical data
A detailed review of the EMR was conducted for patients with an LDL-C ≥190 mg/dL who met inclusion criteria to identify variables of interest. We manually extracted clinical data directly from patient charts by reviewing outpatient clinic notes, admission, progress, and discharge notes, laboratory values, as well as medication lists through August 2017.
For patients with more than one LDL-C measurement within the period of interest, the highest LDL-C value was used. Demographic data such as sex and age at the time of the elevated LDL-C value were also recorded. Charts were reviewed to determine whether patients had a clinic appointment within the year prior to the abnormal LDL-C. If so, the provider’s specialty was documented in addition to whether or not the patient’s dyslipidemia was acknowledged or managed during the visit. Charts were also reviewed to determine whether patients had a clinic appointment during the period of time after the elevated LDL-C was measured until charts were reviewed in August 2017. If so, the provider’s specialty was documented in addition to whether or not the patient’s dyslipidemia was acknowledged or managed during the visit.
To determine whether patients were currently taking a statin or another lipid lowering medication (PCSK9 inhibitors, ezetimibe, niacin, fibrates, or bile acid binding resins) at the time of the abnormal LDL-C value or whether they had ever taken any medications in the past, provider notes and medication lists were carefully reviewed, and the EMR search function was utilized. Charts were also reviewed to determine whether any medication recommendations, prescriptions, or adjustments were made in response to the documented LDL-C ≥190 mg/dL and whether providers considered referral to a cardiologist or endocrinologist to help manage the patient’s dyslipidemia within 3 months of the lab draw.
Lastly, documentation of patient and family history of premature cardiovascular diseases, physical exam findings, and whether or not FH was considered in the differential diagnosis was assessed by reviewing provider notes and by searching for key phrases including but not limited to: “familial hypercholesterolemia,” “FH,” “family history,” “premature,” “genetic,” “xanthoma,” or “arcus”. Family history was documented for: 1) high cholesterol or lipid problems in a first or second degree relative, 2) premature myocardial infarction (Simon Broome criteria), or 3) premature coronary or other vascular disease (Dutch Lipid Clinic Network criteria).
Statistical analysis
Continuous data were reported using median ± interquartile range for non-normal distributions. Sensitivity analyses for baseline characteristics, physical exam findings, family history, treatment patterns, and referral patterns were performed at LDL-C thresholds ≥190 mg/dL and ≥220 mg/dL, since patients with this more extreme phenotype are more likely to have FH. All statistical analyses were performed using STATA 14.2 (StataCorp, College Station, Texas).
Results
Baseline characteristics
During the 8-month study period, there were 27,963 patients with a recorded LDL-C value. Of these patients, 388 had an LDL-C ≥190 mg/dL (1.4%). After excluding 119 patients with extensive missing clinical data and 42 patients with secondary causes of LDL-C elevation, there were 227 patients with an LDL-C ≥190 mg/dL of whom 53 had an LDL-C ≥220 mg/dL. Baseline characteristics of the study population are summarized in Table 1. The median age was 57 years, and 66% were women. Only 21% were currently on a statin at the time LDL-C was recorded, while 36% had never taken a statin. Almost 90% of patients had not been prescribed another lipid lowering medication, such as PCSK9 inhibitors, ezetimibe, niacin, fibrates, or bile acid binding resin, and only 5% were currently on one of these medications. Among those with an LDL-C ≥220 mg/dL, results were comparable. Only 26% were currently taking a statin, while only 8% were currently taking another lipid lowering medication.
Table 1.
Baseline characteristics.
| Characteristic | LDL-C ≥ 190 |
LDL-C ≥ 220 |
|---|---|---|
| n = 227 | n = 53 | |
| Age (yrs), median (IQR) | 57 (48,66) | 55 (50,67) |
| Female, n (%) | 149 (65.6) | 37 (69.8) |
| History of Statin Use, n (%) | ||
| Current | 47 (20.7) | 14 (26.4) |
| Prior But Not Current | 99 (43.6) | 24 (45.3) |
| Never | 81 (35.7) | 15 (28.3) |
| History of Other Lipid Lowering Drug Use, n (%) | ||
| Current | 11 (4.9) | 4 (7.6) |
| Prior But Not Current | 16 (7.0) | 7 (13.2) |
| Never | 200 (88.1) | 42 (79.2) |
Abbreviations: IQR = interquartile range; LDL-C = low-density lipoprotein-cholesterol.
Documentation of family history, physical exam, and the possibility of FH
Provider documentation of family history is reported in Fig. 1. Overall, only 26% of patients with an LDL-C ≥190 mg/dL had specific documentation of the presence or absence of a family history of high cholesterol or dyslipidemia. Only 29% of patients had documentation of the presence or absence of a family history of myocardial infarction, and only 31% of patients had documentation about whether or not they had a first degree relative with known premature coronary and vascular disease. Among those with an LDL-C ≥220 mg/dL, documentation of relevant family history was still less than 50% for each of these three components.
Fig. 1.
Provider documentation of presence/absence of family history (CVD: cardiovascular disease; LDL-C: low-density lipoprotein-cholesterol; MI: premature myocardial infarction).
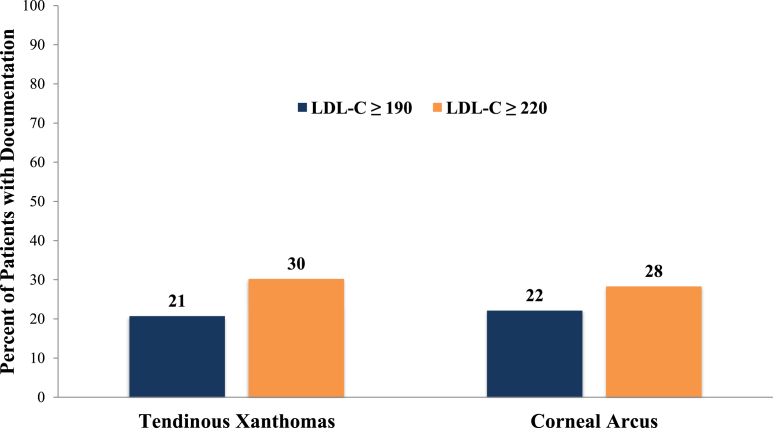
Documentation of clinical findings such as tendinous xanthomas and corneal arcus is presented in Fig. 2. Overall, only 21% of patients with an LDL-C ≥190 mg/dL had documentation of the presence or absence of tendinous xanthomas, while only 22% had documentation of the presence or absence of corneal arcus. Even when patients had an LDL-C ≥220 mg/dL, the presence or absence of each these two physical exam findings was undocumented in around 70% of patient charts.
Fig. 2.
Provider documentation of presence/absence of physical examination findings (LDL-C: low-density lipoprotein-cholesterol).
Lastly, for those with an LDL-C ≥190 mg/dL, FH was only considered in the differential diagnosis for 14% of patients. Even with an LDL-C ≥220 mg/dL, only 30% of patients had charts noting FH as a possibility.
Practice patterns, changes in treatment, and referrals
Following the laboratory test with LDL-C ≥190 mg/dL, more than 90% of patients had a follow-up clinic visit with a provider. In 41% of those with an LDL-C ≥190 mg/dL, neither a statin nor another lipid lowering medication was prescribed, recommended, or adjusted by a provider within 3 months of the abnormal LDL-C. For 51.5% of patients, either a statin or a statin plus another lipid lowering medication was recommended, while for 7.5% of patients, only a non-statin lipid lowering medication was recommended (Fig. 3a). Even among those with an LDL-C ≥220 mg/dL, the results were similar, and 40% of patients had no change in treatment (Fig. 3b).
Fig. 3.
(a) Changes in treatment among those with LDL-C ≥190 mg/dL. (b) Changes in treatment among those with LDL-C ≥220 mg/dL (LDL-C: low-density lipoprotein-cholesterol)
∗Prescribed, recommended, or adjusted (including change in medication type or dose) within 3 months of abnormal LDL-C.
Of all 227 patients with an LDL-C ≥190 mg/dL, 79% had never seen a cardiologist or endocrinologist who acknowledged or managed their LDL-C prior to the abnormal value. Of these patients, only 13% were referred to a specialist within 3 months after the abnormal LDL-C (Fig. 4a). Even at a higher threshold of LDL-C ≥220 mg/dL, results were comparable, and only 16% of those who had not previously seen a specialist were then referred to one (Fig. 4b).
Fig. 4.
(a) Referral pattern among those with LDL-C ≥190 mg/dL. (b) Referral pattern among those with LDL-C ≥220 mg/dL (LDL-C: low-density lipoprotein-cholesterol)
∗Patient had seen a cardiologist or endocrinologist who acknowledged or managed their LDL-C prior to the abnormal value.
∗∗Referral was mentioned or recommended within 3 months of abnormal LDL-C.
Discussion
In a large health care system, individuals with an untreated or residual LDL-C ≥190 mg/dL infrequently had FH considered as a potential diagnosis. Further, they were not adequately managed with statins, or other lipid lowering medications, despite the fact that current lipid guidelines recommend high-intensity statins for all patients with an LDL-C ≥190 mg/dL [2]. Most of these patients were not referred to specialists in the management of lipid disorders. These data highlight important treatment gaps in the care of patients with LDL-C ≥190 mg/dL.
Individuals with an LDL-C ≥190 mg/dL are at significantly increased lifetime risk of CVD. One study involving over 68,000 subjects followed for up to 30 years found that those with LDL-C ≥190 mg/dL had a 2–5 fold increased risk of CHD compared to those with LDL-C <130 mg/dL [1]. Further, CHD occurred 10–20 years earlier in men and 20–30 years earlier in women with LDL-C ≥190 mg/dL than in people with LDL-C<130. Given the higher long-term risks, the 2013 ACC/AHA Cholesterol Guidelines recommended high intensity statin therapy in all those ages 20 years and older with LDL-C ≥190 mg/dL, without calculation of estimated 10-year risk of atherosclerotic cardiovascular disease.
At our institution, 36% of patients with an LDL-C ≥190 mg/dL had no record of having ever been prescribed a statin. Our findings are similar to an analysis of a general practice electronic health record in Australia that found that 44% of patients with an LDL-C ≥190 mg/dL had never taken a statin [12] as well as an analysis of statin prescription rates from a national clinical registry that showed that 34% of patients with an LDL-C ≥190 mg/dL did not have a statin prescription [13]. Surprisingly, after a documented LDL-C ≥190 mg/dL, 41% of patients in our study had no recommended change in treatment. While it is possible that there may have been a reluctance to prescribe statins due to a history of adverse effects such as myalgias, only ~20% of patients in our study reported a history of myalgias, and of those who had an LDL-C ≥190 mg/dL and no prior history of statin use, 47% still had no change in treatment. The study period of the current analysis began 2 years after the release of the 2013 Cholesterol Guidelines, which was an adequate timeframe to disseminate treatment recommendations in this group. The reasons for the therapeutic inertia for statin therapy in those with LDL-C ≥190 mg/dL are not clear, but mirror broader gaps in statin prescriptions in other groups [14].
An important consideration in those with an LDL-C ≥190 mg/dL is the potential for FH. Estimates vary, but studies using genetic testing for diagnosis report a 2% prevalence of FH in those with LDL-C ≥190 mg/dL [15], while an analysis from the NHANES study using clinical criteria reported 7% prevalence [10]. The prevalence of FH increases progressively at higher LDL-C thresholds. Both the Simon Broome and AHA diagnostic criteria delineate an LDL-C level above 190 mg/dL as raising the potential for FH, which should then be supported and confirmed by additional clinical criteria [4]. Similarly, the National Lipid Association Guidelines also state that an LDL-C ≥190 mg/dL should raise suspicion for FH, and that a detailed family history should be collected in all such individuals [5].
Unfortunately, the results of our study indicate that there is poor documentation of the possibility of FH, relevant family history, and corresponding physical exam features in those with LDL-C ≥190 mg/dL, which likely reflects a lack of recognition that these patients may have FH. Interestingly, the proportion of those with documentation of the presence or absence of physical exam findings (20%) was comparable to the proportion with prior specialist management, suggesting the possibility that only a small proportion were assessed for physical exam findings by non-specialists. Even in those with an LDL-C ≥220 mg/dL with a higher likelihood of FH, consideration of family history features relevant for an FH diagnosis were documented in less than half of such cases. Identifying FH patients is essential not only for prompt treatment of the individual, but also because it provides an opportunity to cascade screen family members to identify younger relatives who may not have been detected otherwise [7]. In fact, the 2018 Cholesterol Guidelines specify that lipid testing is indicated in children as early as 2 years of age for those with a family history of LDL-C ≥190 mg/dL, as identifying children and young individuals with FH is a priority. Although it is well known that most individuals with FH are not formally diagnosed [16], there are very few data evaluating consideration of FH criteria in those with LDL-C ≥190 mg/dL, particularly using individual medical chart review.
Various machine learning and electronic health record algorithms are being developed to better identify those with FH [17,18]. In terms of an LDL-C threshold algorithm, a study in the UK described an electronic health record audit tool that identified patients with diagnosed FH or possible FH, and flagged those with an LDL-C >190 mg/dL or those with a total cholesterol >290 mg/dL for further assessment. Over a 2-year period, electronic prompts appeared in the charts of flagged patients to prompt physicians to consider FH. Nurses also reviewed flagged patients to help assemble additional FH diagnostic criteria. After implementation of this two-part initiative, the recorded prevalence of FH increased from 1 in 750 at baseline to 1 in 357 [19]. The development of a similar system within other healthcare networks could enhance additional investigations in those with LDL-C ≥190 mg/dL to increase the diagnosis of FH. With patients now having greater access to their medical records and test results, specifically highlighting within the lab report the need for additional evaluation and treatment in those with LDL-C ≥190 mg/dL may help prompt not only providers but also patients to seek out further management.
Although our study is one of the first to perform a detailed evaluation of care processes from medical records of those with LDL-C ≥190 mg/dL, it has several limitations. First, current practice patterns were only assessed within one health care system. Nonetheless, we believe that our results are still generalizable, as it is known that there is undertreatment in those with LDL-C ≥190 mg/dL and FH is widely underrecognized. In addition, our study did not capture those who were treated to an LDL-C <190 mg/dL. Therefore, the proportion of patients ever having had an LDL-C ≥190 mg/dL who were on statin therapy is likely higher. Furthermore, although patient records were thoroughly and carefully reviewed, patient charts may not be comprehensive as patients may obtain additional health care from outside care providers. Lastly, poor documentation may not always reflect a lack of consideration of FH or a failure to assess the corresponding family history or physical exam findings. Nonetheless, appropriate and accurate documentation is still an important component of patient care, and our findings suggest that there is significant room for improvement.
Conclusions
Even after untreated or residual LDL-C measurements of 190 mg/dL and higher were recorded in this large, academic health care institution, most health care providers did not document the possibility of FH, relevant family history, and corresponding physical exam findings. A large proportion of patients did not receive any adjustments in treatment, and few were referred to specialists. Additional steps are necessary to further understand current practice patterns in order to improve the evaluation and management of patients with LDL-C ≥190 mg/dL.
Funding source
None.
Disclosures
Dr Ahmad reports grants from Regeneron Pharmaceuticals Inc, personal fees from Regeneron Pharmaceuticals Inc, personal fees from Amgen, personal fees from Akcea, grants from the National Institutes of Health–National Heart, Lung, and Blood Institute, and grants from the Familial Hypercholesterolemia Foundation.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Dr Ahmad reports grants from Regeneron Pharmaceuticals Inc, personal fees from Regeneron Pharmaceuticals Inc, personal fees from Amgen, personal fees from Akcea, grants from the National Institutes of Health–National Heart, Lung, and Blood Institute, and grants from the Familial Hypercholesterolemia Foundation.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajpc.2020.100002.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Patient selection method. (LDL-C: low-density lipoprotein-cholesterol)
References
- 1.Perak A.M., Ning H., de Ferranti S.D., Gooding H.C., Wilkins J.T., Lloyd-Jones D.M. Long-term risk of atherosclerotic cardiovascular disease in US adults with the familial hypercholesterolemia phenotype. Circulation. 2016;134(1):9–19. doi: 10.1161/CIRCULATIONAHA.116.022335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stone N.J., Robinson J.G., Lichtenstein A.H. ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;129(25 Suppl 2):S1–S45. doi: 10.1161/01.cir.0000437738.63853.7a. 2014. [DOI] [PubMed] [Google Scholar]
- 3.Vallejo-Vaz A.J., Robertson M., Catapano A.L. Low-density lipoprotein cholesterol lowering for the primary prevention of cardiovascular disease among men with primary elevations of low-density lipoprotein cholesterol levels of 190 mg/dL or above: analyses from the WOSCOPS (west of scotland coronary prevention study) 5-year randomized trial and 20-year observational follow-up. Circulation. 2017;136(20):1878–1891. doi: 10.1161/CIRCULATIONAHA.117.027966. [DOI] [PubMed] [Google Scholar]
- 4.Gidding S.S., Champagne M.A., de Ferranti S.D. The agenda for familial hypercholesterolemia: a scientific statement from the American heart association. Circulation. 2015;132(22):2167–2192. doi: 10.1161/CIR.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg A.C., Hopkins P.N., Toth P.P. Familial hypercholesterolemia: screening, diagnosis and management of pediatric and adult patients: clinical guidance from the National Lipid Association Expert Panel on Familial Hypercholesterolemia. J Clin Lipidol. 2011;5(3 Suppl):S1–S8. doi: 10.1016/j.jacl.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Marks D., Thorogood M., Neil H.A., Humphries S.E. A review on the diagnosis, natural history, and treatment of familial hypercholesterolaemia. Atherosclerosis. 2003;168(1):1–14. doi: 10.1016/s0021-9150(02)00330-1. [DOI] [PubMed] [Google Scholar]
- 7.Langslet G., Ose L. Screening methods in the diagnosis and assessment of children and adolescents with familial hypercholesterolemia. Expert Rev Cardiovasc Ther. 2013;11(8):1061–1066. doi: 10.1586/14779072.2013.814851. [DOI] [PubMed] [Google Scholar]
- 8.de Ferranti S.D., Rodday A.M., Mendelson M.M., Wong J.B., Leslie L.K., Sheldrick R.C. Prevalence of familial hypercholesterolemia in the 1999 to 2012 United States national health and nutrition examination surveys (NHANES) Circulation. 2016;133(11):1067–1072. doi: 10.1161/CIRCULATIONAHA.115.018791. [DOI] [PubMed] [Google Scholar]
- 9.Watts G.F., Gidding S., Wierzbicki A.S. Integrated guidance on the care of familial hypercholesterolaemia from the International FH Foundation: executive summary. J Atheroscler Thromb. 2014;21(4):368–374. [PubMed] [Google Scholar]
- 10.Bucholz E.M., Rodday A.M., Kolor K., Khoury M.J., de Ferranti S.D. Prevalence and predictors of cholesterol screening, awareness, and statin treatment among US adults with familial hypercholesterolemia or other forms of severe dyslipidemia (1999-2014) Circulation. 2018;137(21):2218–2230. doi: 10.1161/CIRCULATIONAHA.117.032321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stone N.J. Secondary causes of hyperlipidemia. Med Clin North Am. 1994;78(1):117–141. doi: 10.1016/s0025-7125(16)30179-1. [DOI] [PubMed] [Google Scholar]
- 12.Vickery A.W., Ryan J., Pang J., Garton-Smith J., Watts G.F. Increasing the detection of familial hypercholesterolaemia using general practice electronic databases. Heart Lung Circ. 2017;26(5):450–454. doi: 10.1016/j.hlc.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 13.Al-Kindi S.G., DeCicco A., Longenecker C.T., Dalton J., Simon D.I., Zidar D.A. Rate of statin prescription in younger patients with severe dyslipidemia. JAMA Cardiol. 2017;2(4):451–452. doi: 10.1001/jamacardio.2016.5162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pokharel Y., Tang F., Jones P.G. Adoption of the 2013 American College of cardiology/American heart association cholesterol management guideline in cardiology practices nationwide. JAMA Cardiol. 2017;2(4):361–369. doi: 10.1001/jamacardio.2016.5922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khera A.V., Won H.H., Peloso G.M. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J Am Coll Cardiol. 2016;67(22):2578–2589. doi: 10.1016/j.jacc.2016.03.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nordestgaard B.G., Chapman M.J., Humphries S.E. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease Consensus Statement of the European Atherosclerosis Society. Eur Heart J. 2013;34(45):3478–3490. doi: 10.1093/eurheartj/eht273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Banda J.M., Sarraju A., Abbasi F. Finding missed cases of familial hypercholesterolemia in health systems using machine learning. NPJ Digit Med. 2019;2:23. doi: 10.1038/s41746-019-0101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Safarova M.S., Liu H., Kullo I.J. Rapid identification of familial hypercholesterolemia from electronic health records: the SEARCH study. J Clin Lipidol. 2016;10(5):1230–1239. doi: 10.1016/j.jacl.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green P., Neely D., Humphries S.E., Committee M.F.A.S. Improving detection of familial hypercholesterolaemia in primary care using electronic audit and nurse-led clinics. J Eval Clin Pract. 2016;22(3):341–348. doi: 10.1111/jep.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient selection method. (LDL-C: low-density lipoprotein-cholesterol)