Abstract
Background
Cardiovascular disease is the leading cause of death in China. The aim of this study was to evaluate the levels of cardiovascular health among Chinese adults and to understand the geographic pattern of cardiovascular health.
Methods
In 2015, a total of 74,726 respondents aged ≥ 20 years with no history of cardiovascular disease were randomly sampled from 298 counties/districts of 31 provinces in mainland China and were interviewed. Seven metrics, including smoking, body mass index, physical activity, diet, total cholesterol, blood pressure, and fasting glucose, were determined. Ideal cardiovascular health was defined as the simultaneous presence of all metrics at the ideal level. A score ranging from 0 to 14 was calculated as the sum of all seven metrics for each province. Scores for cardiovascular health behaviors (smoking, body mass index, physical activity and diet) and those for cardiovascular health factors (smoking, total cholesterol, blood pressure, and fasting glucose) were also calculated.
Findings
The mean age was 44.4 ± 15.9 years, and 49.3% were women. The age-sex-standardized prevalence of ideal cardiovascular health was universally poor, ranging from 0.02% [95% confidence interval (CI): 0%, 0.05%] in Tibet to 2.76% (95% CI: 0.45%, 5.07%) in Heilongjiang. Ideal diet (7.1%) was the least common factor of the seven metrics in each province and varied considerably across provinces. Other component metrics of ideal cardiovascular health were also spatially patterned. In all provinces, women had higher scores than men for cardiovascular health, health behaviors and health factors. Differences in cardiovascular health and health behavior scores between urban and rural areas were associated with levels of socio-economic development.
Interpretation
Strategies for addressing poor cardiovascular health require geographic targeting and localized consideration.
Funding
This research was supported by National Key R&D Program, the Shenzhen Strategic Emerging Industry Development Special Fund, and the Fund of "Sanming" Project of Medicine in Shenzhen.
Keywords: Cardiovascular disease, Cardiovascular health, China, Socio-demographic Index, Spatial analysis
Research in context.
Evidence before this study
A detailed analysis of cardiovascular health (CVH) in Chinese adults was reported based on 2010 China Noncommunicable Disease Surveillance. This study has been limited to comparisons of differences between regions crudely defined as north and south. However, China has a geographically diverse landscape with unevenly distributed social-economic development and healthcare resources. In this study, we particularly assessed the status of overall CVH and seven metrics in China at the provincial level.
Added value of this study
This study used data from a large, provincially representative survey of the adult Chinese population to elaborate the general profile of CVH and its spatial patterns. Only 1.06% of Chinese adults had ideal CVH, with substantial variation across provinces. Ideal diet was the least common factor among the seven metrics of CVH in each province and in China as a whole. The overall CVH and each metric demonstrated certain spatial patterns at provincial level. The discrepancy in CVH score between urban and rural residents was associated with local social-economic development.
Implications of all the available evidence
The CVH in all provinces was still extraordinarily poor, implying that majority of Chinese adults were at risk of developing cardiovascular diseases. Both integrated and localized public health strategies are required in China to improve cardiovascular health and to reduce spatial disparities in cardiovascular health.
Alt-text: Unlabelled box
1. Introduction
Cardiovascular disease (CVD) is the largest cause of global mortality and accounts for nearly half of the 36 million annual deaths from non-communicable diseases [1]. A significant reduction in the age-standardized mortality rate of CVD was observed from 1990 to 2016 in mainland China [2]. However, over the same period, the age-standardized prevalence of CVD increased by 14.7% [2] and China still has a high burden of CVD [3].
The American Heart Association (AHA) emphasizes the concept of primordial prevention, or the prevention of cardiovascular risk factors. It has developed seven cardiovascular health metrics to encourage optimal cardiovascular health (CVH) in the population and particularly to prevent risk factors [4]. As an important component of primordial prevention, ideal CVH was reported to be associated with suboptimal health and mental health [5,6]. Several studies have also suggested that ideal CVH has a beneficial effect on CVD events, [7], [8], [9], [10], [11] CVD mortality and all-cause mortality [12], [13], [14], [15], as well as the quality of life [4]. However, there is an extremely low percentage of individuals with ideal CVH in the Chinese adult population [16], [17], [18].
China has a socio-economically and topographically diverse landscape, and healthcare resources are also unevenly distributed. The disease burden of CVD varies across provinces and the gap between provinces has widened over the past two decades [2]. A nationwide survey that investigated overall CVH in China called for strategies addressing both the whole population and those at high risk of CVD to reverse the increasing levels of cardiovascular risk [16]. However, there has been little investigation into the spatial patterning of CVH. Previous efforts have been limited to comparisons of small subgroups in provinces or differences between regions crudely defined as north and south [10,12,[16], [17], [18], [19]]. Decision makers require more detailed information about geographical variation in CVD risk at subnational level to enable them to provide cost-effective local resource allocation and specific preventive health policies that address both CVD and related health inequalities.
This study aimed to use a nationally and provincially representative survey, the 2015 China Chronic Disease and Nutrition Surveillance (CCDNS), to determine the variation of CVH status across provinces, by gender, and between urban and rural areas.
2. Methods
2.1. Study population
The CCDNS was previously known as the China Chronic Disease and Risk Factor Surveillance, and is a periodical cross-sectional survey of non-communicable and chronic diseases and major risk factors. The 2015 CCDNS field survey was conducted in 298 surveillance counties/districts selected from the newly-integrated national mortality surveillance system established in 2013 [20]. Those surveillance counties/districts were located in all 31 provincial-level administrative areas in mainland China, including 22 provinces, 5 autonomous regions and 4 metropolitan cities (thereinafter referred to as provincial units). Urban and rural areas were defined using the latest criteria from the National Bureau of Statistics, which defined them at administrative village or community level. The target population of the CCDNS was adults aged 18 years and above, living in the sample areas for at least six of the past 12 months, not pregnant (for women), and with no mental health issues or other illnesses which might lead to inaccurate responses or impede physical measurement.
2.2. Sampling methods
In 2015, a complex multi-stage sampling design was used to select eligible participants within every district/county. First, two townships or areas were selected using the proportional to population size method. Second, using the same sampling technique, three administrative villages or communities were selected in each chosen township. Third, each administrative village or community was divided into several residential quarters, each with nearly 60 households, from which three quarters were randomly selected. Finally, 45 households were selected to be the target households. The households and eligible family members were invited to participate in the survey. Of the selected households, 20 were randomly chosen to participate in an additional dietary survey. For every selected household, basic information (e.g., sex, birth date) of every family member was recorded. Family members who met the inclusion criteria were invited to participate the individual questionnaire interview, physical measurement, and blood samples. If a chosen household or more than half of its family members refused to participate, or was unavailable, a replacement was selected using the following principles: (a) the whole household should be replaced; (b) a household in the same residential quarter would be chosen as the replacement if possible; (c) the replacement candidate household should have a similar family structure to the original household. In total, of 82,977 eligible participants, 80,902 were interviewed and completed the survey, giving an individual response rate of 97.5%. We excluded 530 participants who were under 20 years old and 5646 with history of stroke or myocardial infarction. This left a total of 74,726 individuals for inclusion in this analysis. The flow diagram of study sample is shown in Fig. 1.
Fig. 1.
Flow diagram of study sample.
2.3. Data collection
All respondents were interviewed using a household questionnaire, to collect economic, environmental, and other family information. Eligible participants were also given an individual questionnaire to obtain information on demographic characteristics, lifestyle factors, and history of chronic diseases. They were invited to attend a community health service station for physical measurements and blood samples. Smoking status was obtained using the questionnaire from the Global Adult Tobacco Survey [21]. The Global Physical Activity Questionnaire was used to assess physical activity [22]. Dietary behavior within the past 12 months was estimated using a food frequency questionnaire [23]. Households participating in the dietary survey completed a 3-day weighed dietary record (including salt consumption) and provided 3-day dietary recalls. Systolic and diastolic blood pressure were measured three times with a one-minute interval using an electronic sphygmomanometer (HEM-1300; OMRON Healthcare Product Development Dalian Co., Ltd., Dalian, China) after the participants had rested for 5 minutes. Three readings of each were recorded and the average of the last two readings was used for data analysis. Blood samples were obtained in the morning after an overnight fast of at least 10 h. Serum samples for glucose and lipids tests were placed in the car refrigerator or box with ice cubes, delivered to the laboratory of local Centers for Disease Control and Prevention (CDC), and stored in refrigerator at -20 °C within 2 h. Then, within one week after sample collection, samples were frozen at −80 °C with dry ice and shipped by air to the central laboratory in Beijing. Serum glucose (hexokinase method) and total cholesterol (cholesterol oxidase method) were tested using a Hitachi 7600 automated clinical chemistry analyzer (Hitachi, Ltd. Japan). Trained interviewers from local CDC carried out all the interviews, measurements, and blood sample collection. The central lab was certificated by the College of American Pathologists and performed all tests using stringent quality control procedures. The details of data collection have also been described in a previous study on the detection of insulin [24]. The survey was authorized by the ethics committee of the Chinese Center for Disease Control and Prevention (201519-A). Written informed consent was obtained from all participants before data collection.
2.4. CVH metrics
In line with AHA guidelines, the seven CVH metrics (smoking, BMI, physical activity, diet, total cholesterol, blood pressure, and fasting glucose) were grouped into cardiovascular health behaviors (smoking, BMI, physical activity and diet) and cardiovascular health factors (smoking, total cholesterol, blood pressure, and fasting glucose). Smoking is included as both a health behavior and a health factor because of its importance in health promotion.
A CVH score was calculated for each participant based on the seven-component metrics. Each metric was classified into three levels (poor = 0 point; intermediate = 1 point; ideal = 2 points). Detailed definitions of “poor,” “intermediate,” and “ideal” levels for all metrics are described in eTable 1 in the Supplement. CVH score ranged from 0 to 14, and the Health Behaviors Score (HBS) and Health Factor Score (HFS) both ranged from 0 to 8. Ideal cardiovascular health is defined as the simultaneous presence of all seven ideal cardiovascular health items among subjects without the history of cardiovascular disease.
2.5. Socio-demographic Index
We used the Socio-demographic Index (SDI), which was developed by the Global Burden of Disease Study, as an indicator of overall socio-economic development status. It is the geometric mean of indices rated from 0 to 1 for total fertility rate under age 25, years of educational attainment in the population over 15 years old, and lag-distributed income per capita [25]. The 2015 SDI data for each province were downloaded from the Global Health Data Exchange tool from the Global Burden of Disease Study.
2.6. Statistical analysis
We described the demographic and socio-economic characteristics of the study population by province. We then determined age-sex-standardized prevalence rate of the seven ideal CVH metrics and overall ideal CVH by province. We also calculated age-sex-standardized mean CVH score, HBS and HFS by province, and showed them using choropleth maps. We used Pearson linear correlation analysis to determine associations between SDI and the prevalence of the seven ideal CVH metrics, overall ideal CVH, and the three scores. Stratified analyses were applied by gender and for urban and rural areas. In male/female group, we calculated the age-standardized prevalence and score. We also evaluated the associations between SDI and the differences in CVH score, HBS and HFS between urban and rural residents, and by gender. Weights were calculated for all the estimation of population weighted indicators. The weights consisted of two components: sampling weights which accounted for the sampling process and equaled to the probabilities of being selected to participate in the survey, and post-stratification weights which harmonized the sample structure of survey with that of 2015 Chinese population estimated by the State Statistics Bureau. Particularly, we considered the age (5-year increments), gender, rural/ urban residency, and provinces simultaneously when doing the post-stratification. These population data were also used in the age-standardization process. Hot-Deck imputation from the US Census Bureau [26] was used to impute all the missing values in CVH metrics, a total of 13.9% of the observations.
All analyses used SAS version 9.4 (SAS Institute, Inc., Cary, North Carolina). We accounted for the complex sample design using Taylor's series method with finite population correction for the primary sampling units, while estimating the sampling error. Comparisons for prevalence were performed with Rao-Scott χ2 tests, while those for means were performed with design-based linear regression [27]. Choropleth maps were generated by JMP 14 (SAS Institute, Inc., Cary, North Carolina). All tests were two-sided, and a P value < 0.05 was considered statistically significant. The present study defines significant differences between any 2 estimates as nonoverlap of their 95% confidence intervals (CIs).
2.7. Role of funding Source
National Key R&D Program (Reference Number 2018YFC1311700) supported the symposiums for this study. The Shenzhen Strategic Emerging Industry Development Special Fund (Reference Number ZDYBH201900000007) and the Fund of "Sanming" Project of Medicine in Shenzhen (Reference Number SZSM201811096) paid the staff costs of data analysis and draft revision.
3. Results
3.1. Characteristics of the study population
The baseline characteristics of the study population by province are shown in eTable 2 in the Supplement. The study included 74,726 participants, and the sample size ranged from 1433 (Ningxia) to 3644 (Guangdong). The mean age was 44.4 ± 15.9 years, and 49.3% were women. The minimum average age was 40.5 years in Tibet, and the maximum was 47.1 years in Chongqing. The lowest proportion (8.7%) of older people (≥ 65 years old) was in Heilongjiang and the highest proportion (15.9%) in Chongqing. The proportion of women ranged from 46.0% in Guangdong to 51.5% in Anhui, and the proportion of married people from 76.1% in Shanghai to 90.3% in Anhui. Substantial variation was observed between provinces in the proportion of high school education or above, ranging from 10.3% in Guizhou to 66.9% in Beijing. The proportion of people living in rural ranged from 8.5% in Shanghai to 78.4% in Guizhou.
3.2. Ideal CVH status and component metrics
In general, only 1.06% (95% CI: 0.88%, 1.24%) of the overall population had ideal CVH in China. The standardized prevalence of all seven CVH metrics and overall ideal CVH by province are shown in Table 1. The prevalence of ideal CVH varied significantly across provinces, ranging from 0.02% (95% CI: 0%, 0.05%) in Tibet to 2.76% (95% CI: 0.45%, 5.07%) in Heilongjiang.
Table 1.
Age-sex-standardized proportions of ideal cardiovascular health among different provinces in Chinese adults in 2015.
| Region | Province a | SDI | ideal smoking | ideal healthy diet | ideal physical activity | ideal body weight | ideal glucose | ideal cholesterol | ideal blood pressure | ideal CVH |
|---|---|---|---|---|---|---|---|---|---|---|
| North | Beijing | 0.84b,c | 73.1(68.9, 77.3)d | 10.0(6.5, 13.5) | 84.4(82.5, 86.4) | 49.4(46.3, 52.6) | 81.5(79.3, 83.7) | 74.8(72.0, 77.6) | 31.1(27.7, 34.5) | 0.30(0.08, 0.52) |
| Tianjin | 0.80 | 71.0(65.2, 76.7) | 8.9(6.1, 11.7) | 75.9(71.5, 80.3) | 51.7(47.3, 56.1) | 77.7(72.3, 83.2) | 72.0(68.0, 76.1) | 25.0(19.6, 30.4) | 1.34(0.67, 2.01) | |
| Hebei | 0.72 | 70.6(65.2, 75.9) | 4.0(0.5, 7.5) | 78.5(74.5, 82.5) | 56.9(54.3, 59.4) | 88.5(86.4, 90.5) | 76.5(74.0, 79.0) | 28.7(24.1, 33.2) | 0.10(0.01, 0.19) | |
| Shanxi | 0.71 | 67.7(65.6, 69.9) | 1.1(0.4, 1.7) | 80.2(75.8, 84.5) | 53.1(47.4, 58.8) | 86.4(83.9, 88.8) | 77.3(73.8, 80.8) | 27.5(25.2, 29.8) | 0.29(0, 0.60) | |
| Inner Mongolia | 0.72 | 65.9(63.9, 67.8) | 2.8(1.1, 4.4) | 81.2(75.2, 87.2) | 55.3(49.7, 60.9) | 87.4(85.4, 89.3) | 69.2(66.1, 72.3) | 27.6(21.7, 33.5) | 0.30(0.03, 0.56) | |
| Northeast | Liaoning | 0.74 | 69.9(63.4, 76.4) | 11.9(6.5, 17.3) | 85.0(80.5, 89.4) | 54.9(52.4, 57.4) | 83.5(80.2, 86.8) | 70.3(67.0, 73.5) | 29.2(25.4, 32.9) | 1.60(0.21, 2.99) |
| Jilin | 0.71 | 75.1(72.1, 78.2) | 4.9(1.7, 8.2) | 84.5(80.5, 88.6) | 53.9(50.7, 57.1) | 88.4(83.9, 92.9) | 78.2(69.1, 87.4) | 28.8(27.3, 30.4) | 0.76(0.04, 1.47) | |
| Heilongjiang | 0.70 | 76.7(71.7, 81.7) | 7.1(4.6, 9.6) | 82.9(80.5, 85.3) | 57.6(54.6, 60.7) | 82.5(80.2, 84.7) | 70.4(67.8, 73.0) | 33.2(28.0, 38.4) | 2.76(0.45, 5.07) | |
| East | Shanghai | 0.82 | 78.4(75.5, 81.3) | 16.1(13.5, 18.8) | 74.7(68.7, 80.7) | 64.3(59.8, 68.9) | 87.4(83.5, 91.4) | 80.9(78.1, 83.8) | 35.0(30.0, 39.9) | 2.14(1.16, 3.11) |
| Jiangsu | 0.75 | 70.8(67.6, 74.1) | 13.5(10.4, 16.6) | 77.4(72.3, 82.5) | 58.4(55.3, 61.4) | 88.0(84.6, 91.3) | 72.6(68.7, 76.4) | 27.4(21.7, 33.0) | 2.11(1.30, 2.91) | |
| Zhejiang | 0.75 | 72.9(69.8, 76.0) | 19.0(16.5, 21.4) | 76.8(73.4, 80.2) | 70.4(65.5, 75.2) | 87.9(84.8, 90.9) | 72.5(64.2, 80.7) | 32.3(27.5, 37.1) | 2.31(1.61, 3.01) | |
| Anhui | 0.65 | 70.9(68.1, 73.8) | 6.4(3.3, 9.4) | 69.5(61.6, 77.4) | 62.9(58.1, 67.8) | 90.1(87.7, 92.5) | 75.7(73.3, 78.1) | 26.9(23.6, 30.2) | 0.59(0.15, 1.03) | |
| Fujian | 0.72 | 72.7(69.3, 76.2) | 12.4(9.3, 15.5) | 77.8(73.9, 81.8) | 71.3(68.9, 73.6) | 90.2(89.6, 90.8) | 58.4(55.9, 60.8) | 33.7(27.6, 39.8) | 2.09(1.01, 3.18) | |
| Jiangxi | 0.66 | 73.8(71.1, 76.4) | 6.8(3.6, 10.0) | 84.3(81.3, 87.4) | 74.3(70.5, 78.1) | 89.4(86.5, 92.4) | 75.3(72.2, 78.3) | 32.4(27.2, 37.5) | 1.40(0, 3.06) | |
| Shandong | 0.74 | 74.6(69.0, 80.3) | 7.2(5.4, 9.0) | 76.9(68.3, 85.4) | 55.3(52.5, 58.2) | 89.1(86.8, 91.3) | 67.0(63.9, 70.1) | 25.9(19.2, 32.6) | 0.74(0.43, 1.05) | |
| Central | Henan | 0.70 | 71.9(69.7, 74.1) | 1.4(0.4, 2.5) | 73.3(68.5, 78.1) | 50.2(44.8, 55.7) | 84.8(78.0, 91.6) | 73.0(66.0, 80.0) | 26.8(22.1, 31.5) | 0.05(0, 0.14) |
| Hubei | 0.70 | 70.8(66.1, 75.6) | 10.5(7.8, 13.3) | 79.4(75.5, 83.2) | 69.9(65.4, 74.4) | 90.5(87.7, 93.2) | 79.5(75.0, 84.1) | 32.5(25.5, 39.5) | 1.81(0.33, 3.29) | |
| Hunan | 0.69 | 64.1(62.9, 65.3) | 4.0(2.7, 5.3) | 79.1(74.4, 83.8) | 73.9(72.2, 75.6) | 89.3(87.5, 91.1) | 71.8(68.4, 75.2) | 33.6(26.3, 41.0) | 0.25(0.06, 0.43) | |
| South | Guangdong | 0.77 | 67(63.6, 70.3) | 16.2(8.2, 24.2) | 78.5(73.8, 83.2) | 71.4(69.2, 73.6) | 88.1(83.1, 93.0) | 60.2(56.8, 63.6) | 41.9(35, 48.7) | 2.04(0.83, 3.25) |
| Guangxi | 0.69 | 71.0(66.3, 75.7) | 7.6(5.4, 9.8) | 77.2(75.2, 79.1) | 74.9(71.2, 78.6) | 85.5(82.5, 88.5) | 54.7(50.8, 58.6) | 32.3(28.2, 36.3) | 1.33(1.03, 1.63) | |
| Hainan | 0.70 | 62.8(58.4, 67.2) | 13.7(10.7, 16.8) | 84.2(79.6, 88.9) | 80.5(75.8, 85.2) | 88.2(86.0, 90.3) | 55.7(51.3, 60.0) | 37.9(34.9, 40.9) | 1.40(0.51, 2.29) | |
| Southwest | Chongqing | 0.69 | 67.1(63.8, 70.3) | 5.9(2.4, 9.4) | 81.8(77.1, 86.5) | 62.2(57.3, 67.2) | 85.9(80.4, 91.5) | 67.3(59.6, 74.9) | 32.9 (25.8, 39.9) | 1.14(0.26, 2.02) |
| Sichuan | 0.67 | 65.5(60.5, 70.4) | 6.6(4.4, 8.7) | 79.8(73.8, 85.9) | 66.7(63.9, 69.6) | 89.2(84.4, 94.0) | 73.5(68.4, 78.6) | 39.0(32.9, 45) | 1.18(0.24, 2.11) | |
| Guizhou | 0.59 | 67.1(61.5, 72.7) | 3.6(1.4, 5.9) | 77.6(64.9, 90.3) | 74.1(64.3, 83.9) | 91.0(87.5, 94.5) | 71.2(66.0, 76.4) | 33.9(24.1, 43.7) | 0.40(0.01, 0.78) | |
| Yunnan | 0.63 | 63.8(61.1, 66.5) | 4.5(3.3, 5.8) | 86.1(82.3, 89.9) | 71.0(67.1, 75) | 92.0(88.6, 95.5) | 70.4(65.8, 75.1) | 35.9(31.1, 40.7) | 0.89(0.42, 1.35) | |
| Tibet | 0.57 | 85.2(81.4, 89) | 0.3(0, 0.7) | 74.0(63.7, 84.2) | 76.2(63.4, 89.1) | 92.0(90.5, 93.5) | 71.5(68.5, 74.6) | 32.2(24.2, 40.2) | 0.02(0, 0.05) | |
| Northwest | Shaanxi | 0.69 | 71.0(66.4, 75.5) | 1.9(0, 4.1) | 80.5(74.2, 86.8) | 65.0(57.6, 72.5) | 91.9(89.1, 94.7) | 79.6(76.5, 82.8) | 32.7(28.2, 37.2) | 0.38(0, 0.81) |
| Gansu | 0.62 | 68.2(66.4, 70.1) | 3.0(1.8, 4.2) | 80.4(73.7, 87.1) | 65.2(61.1, 69.3) | 91.1(89.2, 92.9) | 79.3(78.1, 80.4) | 28.4(25.9, 30.9) | 0.17(0.02, 0.32) | |
| Qinghai | 0.64 | 71.5(64.2, 78.8) | 0.7(0, 1.5) | 83.8(80.5, 87.1) | 67.6(62.2, 73) | 88.7(85.8, 91.7) | 80.3(76.9, 83.7) | 37.2(30.0, 44.3) | 0.07(0, 0.14) | |
| Ningxia | 0.66 | 75.5(73.4, 77.6) | 4.8(0, 9.9) | 82.3(77.4, 87.3) | 67.4(64.8, 69.9) | 94.2(93.3, 95.1) | 85.5(85.4, 85.6) | 37.1(30.1, 44.2) | 2.08(0, 4.40) | |
| Xinjiang | 0.71 | 79.4(73.5, 85.3) | 4.2(1.1, 7.4) | 79.5(71.1, 87.9) | 54.3(49.3, 59.4) | 88.4(85.7, 91.0) | 77.5(72.3, 82.6) | 41.8(37.3, 46.4) | 0.90(0.02, 1.77) | |
| Total | 0.72 | 71.1(70.2, 72.0) | 7.1(6.5, 7.8) | 79.6(78.5, 80.7) | 64.0(62.9, 65.1) | 88.0(87.4, 88.7) | 72.3(71.3, 73.2) | 32.3(31.2, 33.4) | 1.06(0.88, 1.24) |
Not including China Hong Kong, Macao and Taiwan.
Redder color means higher value of point estimation for SDI and individual ideal metrics, bluer means lower value of point estimation.
SDI means social development index.
Proportion and 95% confidence interval.
Ideal fasting glucose was the most common individual factor (88.0%), followed by ideal physical activity (79.6%), ideal cholesterol (72.3%), ideal smoking (71.1%), and ideal BMI (64.0%). However, quite a low proportion had ideal blood pressure (32.3%) and ideal healthy diet (7.1%). For some CVH metrics, there were substantial variations between provinces. For example, the proportion with an ideal healthy diet was 19.0% in Zhejiang, over 60 times greater than in Tibet (0.3%), and the proportion with ideal cholesterol levels ranged from 54.7% in Guangxi to 85.5% in Ningxia.
Table 1 also shows the spatial patterns of CVH metrics in mainland China. There was a higher proportion of people with ideal smoking levels in the east, and fewer in the south and southwest except Tibet. There were also more people with an ideal healthy diet in the east and south, and fewer in the northwest. Ideal physical activity was more common in the northeast and northwest regions. Better fasting glucose levels were seen in the southwest and northwest regions. More people in the northwest had ideal cholesterol levels. There were similar spatial patterns for BMI and blood pressure, which showed higher prevalence in the south and southwest and lower in the north and northeast regions.
3.3. CVH score
In the overall population, the average CVH score, HBS, and HFS were 10.23 (95% CI: 10.18, 10.27), 5.57 (95% CI: 5.54, 5.60), and 6.09 (95% CI: 6.06, 6.13). The standardized mean CVH score ranged from 9.61 (95% CI: 9.36, 9.86) in Inner Mongolia to 10.79 (95% CI: 10.70, 10.89) in Shanghai. HBS ranged from 5.09 (95% CI: 4.91, 5.27) in Inner Mongolia to 5.95 (95% CI: 5.89, 6.02) in Shanghai, and HFS from 5.78 (95% CI: 5.70, 5.87) in Hainan to 6.52 (95% CI: 6.44, 6.60) in Ningxia.
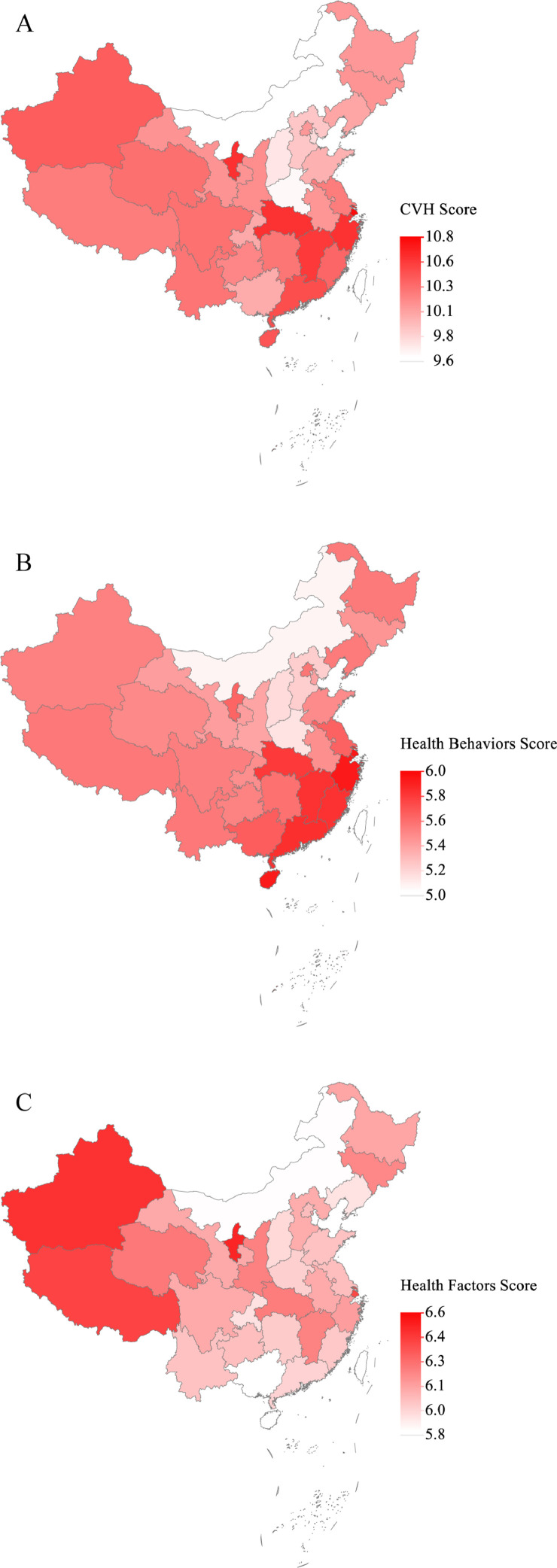
Fig. 2 shows the spatial pattern of the provincial CVH score, HBS, and HFS. The northern region had the lowest CVH score, with higher scores in Shanghai, Hubei, Ningxia, Zhejiang, and Jiangxi. HBS was higher in the southeast, including Shanghai, Zhejiang and Hainan, and lower HBS in the north. Xinjiang, Tibet, and Ningxia had the highest HFS, with lower values in the northern and southern regions.
Fig. 2.
Age- and sex-standardized CVH Score, Health Behaviors Score, and Health Factors Score by 31 provinces in China, 2015. (A) CVH score. (B) Health Behaviors Score. (C) Health Factors Score.
3.4. Urban-rural differences
The distributions of all seven CVH metrics and overall ideal CVH for urban and rural areas are shown in Table 2. The proportion of ideal CVH among urban residents was 1.56% (95% CI: 1.20%, 1.92%), statistically higher than among rural residents [0.62% (95% CI: 0.50%, 0.75%)]. Lower ideal rates were observed in the urban population for physical activity, BMI, and blood glucose. In most provinces, the ideal CVH rate was higher among urban than rural residents. The spatial patterns of ideal diet, body weight, cholesterol and blood pressure were similar between urban and rural areas, while other metrics appears to be fairly different in between.
Table 2.
Age-sex-standardized proportions of ideal cardiovascular health among different provinces in urban and rural residents, 2015.
| Region | Provincea | No. | ideal smoking | ideal healthy diet | ideal physical activity | ideal body weight | ideal glucose | ideal cholesterol | ideal blood pressure | ideal CVH |
|---|---|---|---|---|---|---|---|---|---|---|
| Urban | ||||||||||
| North | Beijing | 1003 | 76.4(70.8, 82.0)b,c | 10.6(6.5, 14.7) | 84.7(82.6, 86.7) | 51.5(48.3, 54.6) | 82.6(79.6, 85.6) | 76.8(75.2, 78.3) | 34.4(30.8, 37.9) | 0.30(0.08, 0.52) |
| Tianjin | 1038 | 77.2(68.9, 85.4) | 11.1(7.8, 14.5) | 79.7(75.6, 83.8) | 52.1(49.3, 54.9) | 78.3(70.4, 86.1) | 69.2(65.2, 73.2) | 24.4(17.1, 31.8) | 2.22(1.09, 3.35) | |
| Hebei | 1183 | 72.5(64.6, 80.5) | 7.5(1.9, 13.1) | 77.7(70.4, 84.9) | 52.2(48.4, 56.0) | 87.4(84.2, 90.6) | 75.8(71.8, 79.9) | 30.6(25.7, 35.5) | 0.13(0, 0.32) | |
| Shanxi | 489 | 71.7(69.3, 74.1) | 1.7(0.1, 3.3) | 78.5(69.1, 88.0) | 49.4(40.3, 58.6) | 77.5(72.0, 82.9) | 71.0(65.7, 76.3) | 30.2(24.4, 35.9) | 0.46(0, 1.15) | |
| Inner Mongolia | 699 | 71.4(69.0, 73.7) | 3.9(0.3, 7.5) | 83.8(76.6, 91.0) | 50.1(39.7, 60.6) | 84.8(82.1, 87.5) | 72.3(67.8, 76.8) | 29.7(15.7, 43.6) | 0.31(0, 0.64) | |
| Northeast | Liaoning | 1278 | 74.9(69.8, 80.1) | 13.3(4.1, 22.5) | 84.9(79.4, 90.3) | 50.7(48.2, 53.3) | 83.0(80.4, 85.5) | 68.9(65.0, 72.8) | 32.3(28.4, 36.3) | 2.01(0, 4.31) |
| Jilin | 784 | 81.4(76.6, 86.1) | 7.5(2.4, 12.6) | 85.8(82.2, 89.3) | 52.4(46.9, 57.9) | 86.9(83.8, 90.0) | 78.1(70.4, 85.9) | 27.5(26.3, 28.7) | 1.29(0.01, 2.57) | |
| Heilongjiang | 610 | 82.8(79.9, 85.7) | 9.4(5.9, 13) | 83.9(79.3, 88.4) | 57.8(55.5, 60.1) | 80.0(78.8, 81.2) | 70.7(69.6, 71.9) | 36.7(33.7, 39.7) | 3.77(0, 7.70) | |
| East | Shanghai | 1405 | 78.6(75.4, 81.8) | 16.4(13.3, 19.4) | 75.1(68.3, 81.8) | 64.5(59.4, 69.5) | 87.5(83.1, 91.8) | 81.1(78.2, 84) | 35.8(29.6, 41.9) | 2.23(1.23, 3.23) |
| Jiangsu | 2122 | 69.2(66.7, 71.6) | 13.0(8.1, 17.9) | 74.6(70.6, 78.6) | 58.7(55.3, 62.0) | 87.6(85.1, 90.1) | 71.4(67.5, 75.3) | 28.0(19.7, 36.2) | 2.34(1.17, 3.52) | |
| Zhejiang | 888 | 75.6(72.7, 78.6) | 26.1(22.6, 29.7) | 78.5(74.3, 82.7) | 69.6(62.7, 76.5) | 87.2(82.2, 92.2) | 72.0(64.9, 79.1) | 30.2(23.0, 37.4) | 3.06(2.31, 3.81) | |
| Anhui | 1141 | 69.8(65.9, 73.7) | 7.2(1.4, 12.9) | 66.9(57.4, 76.3) | 60.7(57.0, 64.3) | 89.0(86.2, 91.8) | 78.3(76.2, 80.4) | 29.9(23.5, 36.3) | 0.53(0, 1.19) | |
| Fujian | 1149 | 71.8(68.6, 75) | 14.9(10.8, 19) | 73.9(69.3, 78.4) | 69.4(64.9, 73.9) | 92.5(91.1, 93.8) | 59.9(57.8, 61.9) | 30.8(27.4, 34.1) | 2.44(1.44, 3.44) | |
| Jiangxi | 1011 | 78.0(72.7, 83.2) | 7.1(0.4, 13.7) | 84.6(80.4, 88.8) | 74.0(67.5, 80.5) | 89.9(87.2, 92.5) | 73.4(67.8, 79.1) | 35.1(31.1, 39.1) | 2.43(0, 5.66) | |
| Shandong | 1342 | 76.6(66.6, 86.7) | 8.3(6.1, 10.6) | 78.2(74.3, 82.1) | 54.8(49.4, 60.3) | 86.6(83.1, 90.1) | 67.6(64.1, 71.1) | 31.9(23.2, 40.6) | 0.91(0.55, 1.26) | |
| Central | Henan | 1920 | 69.4(65.5, 73.2) | 1.9(0.4, 3.5) | 78.1(75.0, 81.1) | 48.0(35.2, 60.7) | 81.8(71.1, 92.5) | 68.7(57.1, 80.4) | 28.8(20.7, 36.9) | 0.11(0, 0.31) |
| Hubei | 1260 | 76.6(71.2, 81.9) | 10.8(6.7, 14.9) | 77.8(73.5, 82.1) | 67.8(63.0, 72.6) | 92.1(87.7, 96.4) | 78.6(72.8, 84.3) | 37.4(26.8, 48.0) | 2.43(0, 5.11) | |
| Hunan | 1183 | 67.2(64.1, 70.3) | 3.2(1.0, 5.4) | 77.9(69.1, 86.8) | 74.5(73.1, 76) | 89.4(87.2, 91.5) | 73.4(67.9, 78.9) | 37.0(25.4, 48.6) | 0.17(0, 0.52) | |
| South | Guangdong | 2001 | 69.8(64.6, 74.9) | 21.5(12.0, 31.0) | 79.1(73.7, 84.4) | 68.6(65.6, 71.6) | 92.2(88.3, 96.2) | 61.9(55.9, 67.9) | 47.1(38.4, 55.7) | 2.87(1.69, 4.06) |
| Guangxi | 791 | 77.9(71.8, 84.0) | 9.3(7.7, 10.8) | 76.1(72.2, 80.0) | 69.1(64.3, 74.0) | 90.6(88.6, 92.5) | 67.6(65.8, 69.5) | 40.8(35.9, 45.6) | 2.16(0.91, 3.42) | |
| Hainan | 322 | 66.9(62.7, 71.0) | 14.4(8.4, 20.3) | 84.6(83.7, 85.6) | 66.4(54.6, 78.2) | 86.5(81.5, 91.5) | 53.5(44.5, 62.5) | 29.6(26.3, 33.0) | 0.96(0, 2.60) | |
| Southwest | Chongqing | 790 | 67.3(60.3, 74.3) | 5.7(2.5, 8.9) | 77.3(70.1, 84.4) | 60.1(53.4, 66.9) | 86.7(79.7, 93.7) | 68.4(59.5, 77.4) | 39.5(27.7, 51.2) | 1.51(0, 3.66) |
| Sichuan | 1059 | 63.4(60.0, 66.7) | 4.8(2.4, 7.2) | 81.0(75.5, 86.4) | 66.8(62.9, 70.7) | 93.3(90.9, 95.6) | 75.3(70.1, 80.5) | 36.6(29.5, 43.7) | 1.25(0.17, 2.34) | |
| Guizhou | 451 | 72.5(62.5, 82.6) | 3.7(0.6, 6.7) | 78.9(70.4, 87.5) | 73.3(60.9, 85.8) | 88.3(83.7, 93.0) | 70.5(68.9, 72.1) | 29.8(22.4, 37.1) | 0.51(0, 1.25) | |
| Yunnan | 647 | 62.9(60.5, 65.3) | 4.6(3.0, 6.2) | 87.2(82.2, 92.2) | 66.8(57.9, 75.6) | 88.5(80.8, 96.1) | 71.6(60.8, 82.4) | 41.0(31.0, 51.0) | 1.58(0.54, 2.61) | |
| Tibet | 347 | 85.3(81.8, 88.8) | 0 | 71.1(58.0, 84.1) | 70.2(53.1, 87.2) | 94.1(91.2, 97.0) | 72.7(64.5, 80.9) | 35.9(33.4, 38.3) | 0 | |
| Northwest | Shaanxi | 978 | 73.1(68.7, 77.4) | 2.4 (0, 5.8) | 77.3(71.3, 83.3) | 64.1(54.2, 73.9) | 90.8(88.3, 93.4) | 78.6(76, 81.3) | 36.9(31.1, 42.8) | 0.59(0, 1.29) |
| Gansu | 356 | 75.2(65.5, 85.0) | 3.1(0, 7.1) | 73.2(57.0, 89.4) | 63.6(56.7, 70.5) | 84.5(81.3, 87.8) | 70.4(63.3, 77.5) | 28.9(21.6, 36.1) | 0.33(0, 1.07) | |
| Qinghai | 322 | 76.2(72.4, 79.9) | 2.2(2.1, 2.2) | 81.6(79.3, 84.0) | 53.8(52.8, 54.7) | 82.5(79.3, 85.7) | 72.7(69.9, 75.6) | 30.0(28.7, 31.2) | 0.31(0.22, 0.40) | |
| Ningxia | 398 | 75.1(73.3, 76.8) | 8.4(0, 17.1) | 82.6(80.4, 84.8) | 63.9(61.2, 66.7) | 93.2(91.6, 94.8) | 84.6(83.0, 86.1) | 36.4(29.5, 43.3) | 3.76(0, 8.05) | |
| Xinjiang | 885 | 75.0(72.7, 77.4) | 6.0(3.7, 8.4) | 82.0(72.0, 92.0) | 51.3(47.6, 55.0) | 86.4(83.5, 89.2) | 74.7(71.0, 78.4) | 41.2(35.5, 47.0) | 1.30(0.47, 2.14) | |
| Total | 29852 | 74.1(72.9, 75.3) | 9.2(8.0, 10.5) | 79.2(77.7, 80.6) | 60.6(59.0, 62.2) | 87.1(86.1, 88.2) | 72.8(71.5, 74.1) | 34.0(32.4, 35.6) | 1.56(1.20, 1.92) | |
| Rural | ||||||||||
| North | Beijing | 653 | 61.8(59.0, 64.7) | 7.7(3.7, 11.7) | 83.7(81.6, 85.7) | 42.4(36.1, 48.7) | 77.5(75.0, 80.0) | 67.9(60.6, 75.2) | 19.8(9.5, 30.2) | 0.30(0, 0.83) |
| Tianjin | 638 | 65.2(59.6, 70.9) | 6.9(3.3, 10.5) | 72.4(67.1, 77.6) | 51.2(44.3, 58.2) | 77.2(73.4, 81.1) | 74.6(69.3, 79.9) | 25.5(21.4, 29.6) | 0.52(0, 1.58) | |
| Hebei | 2117 | 68.8(63.9, 73.7) | 1.0(0.4, 1.6) | 79.3(75.5, 83.0) | 60.9(56.5, 65.3) | 89.3(87.2, 91.4) | 77.0(73.7, 80.4) | 27.0(21.8, 32.2) | 0.08(0, 0.18) | |
| Shanxi | 1298 | 65.3(63.4, 67.1) | 0.7(0.4, 0.9) | 81.2(79.5, 82.9) | 55.3(49.9, 60.7) | 91.9(88.8, 94.9) | 81.2(77.9, 84.5) | 25.9(23.3, 28.4) | 0.19(0.16, 0.22) | |
| Inner Mongolia | 1027 | 61.8(60.5, 63.1) | 1.9(0.5, 3.3) | 79.3(70.7, 87.8) | 59.1(54.9, 63.3) | 89.3(87.3, 91.3) | 66.9(59.4, 74.5) | 26.1(21.9, 30.2) | 0.29(0, 0.70) | |
| Northeast | Liaoning | 1004 | 63.8(53.9, 73.7) | 10.2(4.0, 16.3) | 85.1(78.2, 91.9) | 60.0(57.2, 62.9) | 84.1(78.6, 89.6) | 71.9(67.1, 76.8) | 25.3(21.2, 29.5) | 1.10(0, 2.39) |
| Jilin | 986 | 66.7(64.7, 68.7) | 1.4(0.3, 2.5) | 82.9(76.1, 89.7) | 55.9(53.6, 58.3) | 90.4(82.6, 98.2) | 78.3(65.8, 90.8) | 30.6(28.1, 33.2) | 0.03(0, 0.09) | |
| Heilongjiang | 1667 | 64.2(61.2, 67.2) | 2.2(1.3, 3.1) | 80.8(73.9, 87.8) | 57.4(51.8, 63.0) | 87.5(83.4, 91.5) | 69.7(63.8, 75.6) | 26.0(18.8, 33.2) | 0.71(0, 1.57) | |
| East | Shanghai | 302 | 75.9(66.1, 85.7) | 13.4(6.6, 20.2) | 71.1(58.6, 83.5) | 63.1(58.0, 68.2) | 87.0(82.8, 91.1) | 79.1(73.9, 84.3) | 26.7(21.2, 32.2) | 1.12(0.62, 1.63) |
| Jiangsu | 1140 | 73.2(68.3, 78.1) | 14.2(8.1, 20.3) | 81.2(72.4, 90.0) | 58.0(51.8, 64.1) | 88.5(82.7, 94.3) | 74.2(69.9, 78.5) | 26.5(20.3, 32.7) | 1.77(1.01, 2.53) | |
| Zhejiang | 1704 | 69.1(63.9, 74.3) | 8.9(6.6, 11.1) | 74.5(70.6, 78.4) | 71.4(69.0, 73.8) | 88.8(86.7, 90.8) | 73.1(62.1, 84.1) | 35.2(29.8, 40.6) | 1.26(0, 2.54) | |
| Anhui | 1768 | 72.1(70.3, 73.9) | 5.5(4.4, 6.7) | 72.2(66.2, 78.2) | 65.3(58.8, 71.7) | 91.2(88.4, 94.0) | 73.0(68.8, 77.3) | 23.8(19.9, 27.7) | 0.65(0.23, 1.07) | |
| Fujian | 1545 | 73.8(69.5, 78.2) | 9.3(5.0, 13.6) | 82.8(77.1, 88.5) | 73.6(69.4, 77.7) | 87.3(85.5, 89.1) | 56.5(53.1, 59.8) | 37.3(25.2, 49.3) | 1.67(0, 3.35) | |
| Jiangxi | 1623 | 70.8(68.6, 72.9) | 6.6(4.6, 8.7) | 84.2(81.4, 86.9) | 74.6(70.4, 78.7) | 89.1(85.5, 92.7) | 76.6(72.9, 80.3) | 30.4(24.2, 36.7) | 0.65(0.08, 1.22) | |
| Shandong | 2274 | 73.3(69.7, 76.9) | 6.4(4.0, 8.8) | 76.0(63.6, 88.3) | 55.7(52.2, 59.1) | 90.7(88.5, 92.9) | 66.6(62.2, 70.9) | 22(17.5, 26.4) | 0.63(0.14, 1.11) | |
| Central | Henan | 1351 | 74.1(70.3, 77.8) | 1.0(0, 2.0) | 69.2(64.1, 74.3) | 52.2(46.1, 58.2) | 87.4(82.6, 92.1) | 76.6(73.7, 79.5) | 25.1(18.8, 31.4) | 0 |
| Hubei | 1271 | 64.6(59.3, 69.9) | 10.2(7.6, 12.9) | 81.1(76.3, 85.8) | 72.3(66.4, 78.1) | 88.7(86.6, 90.8) | 80.6(74.6, 86.5) | 27.2(25.2, 29.2) | 1.14(0.35, 1.92) | |
| Hunan | 2265 | 62.2(59.6, 64.9) | 4.5(3.3, 5.7) | 79.8(75.5, 84.1) | 73.6(70.8, 76.4) | 89.3(87.3, 91.3) | 70.8(65.3, 76.4) | 31.6(27.0, 36.2) | 0.29(0.01, 0.57) | |
| South | Guangdong | 1643 | 63.9(58.7, 69.0) | 10.3(5.9, 14.6) | 77.9(70.7, 85) | 74.5(69.3, 79.7) | 83.4(77.9, 89.0) | 58.3(55.0, 61.6) | 36.1(32.4, 39.7) | 1.12(0.48, 1.76) |
| Guangxi | 1940 | 69.0(63.4, 74.6) | 7.1(4.3, 9.9) | 77.5(74.5, 80.5) | 76.6(72.1, 81.1) | 84.0(80.3, 87.8) | 50.9(46.4, 55.4) | 29.8(25.5, 34.0) | 1.09(0.77, 1.41) | |
| Hainan | 1439 | 61.8(57.9, 65.8) | 13.6(10.0, 17.2) | 84.1(78.4, 89.9) | 83.7(81.6, 85.8) | 88.6(86.9, 90.2) | 56.2(50.8, 61.5) | 39.7(38.2, 41.3) | 1.50(0.48, 2.52) | |
| Southwest | Chongqing | 1323 | 66.8(64.3, 69.4) | 6.1(1.2, 11.0) | 85.5(80.2, 90.8) | 64.0(58.6, 69.3) | 85.3(80.3, 90.3) | 66.3(59.3, 73.3) | 27.5(22.7, 32.3) | 0.84(0, 1.83) |
| Sichuan | 2266 | 66.4(60.3, 72.6) | 7.4(4.7, 10.1) | 79.3(71.1, 87.6) | 66.7(61.9, 71.5) | 87.3(81.0, 93.6) | 72.7(66.4, 79) | 40.1(32.3, 47.8) | 1.14(0.07, 2.21) | |
| Guizhou | 1546 | 65.8(60.4, 71.2) | 3.6(1.2, 6.1) | 77.3(62.9, 91.7) | 74.3(63.0, 85.5) | 91.6(87.7, 95.5) | 71.3(65.0, 77.7) | 34.9(23.9, 45.9) | 0.37(0.05, 0.69) | |
| Yunnan | 2189 | 64.4(60.9, 68.0) | 4.5(2.1, 6.8) | 85.4(80.5, 90.3) | 73.7(72.8, 74.7) | 94.3(92.3, 96.2) | 69.7(64.4, 75.0) | 32.8(29.5, 36.0) | 0.46(0.17, 0.74) | |
| Tibet | 1565 | 85.1(80.4, 89.9) | 0.5(0, 1.0) | 76.2(67.5, 84.9) | 80.8(73.1, 88.5) | 90.4(90.0, 90.8) | 70.6(68.3, 73.0) | 29.5(18.6, 40.4) | 0.03(0, 0.09) | |
| Northwest | Shaanxi | 1348 | 67.2(59.4, 75.0) | 0.9(0.5, 1.4) | 86.2(79.4, 92.9) | 66.7(55.5, 78) | 93.8(88.9, 98.7) | 81.4(75.9, 87.0) | 25.2(20.5, 29.9) | 0 |
| Gansu | 1696 | 66.1(64.2, 68.0) | 3.0(2.2, 3.7) | 82.6(78.1, 87.1) | 65.7(61.5, 69.9) | 93.1(92.1, 94.0) | 82.0(79.7, 84.2) | 28.3(26.9, 29.7) | 0.12(0.07, 0.17) | |
| Qinghai | 1181 | 70.3(62.1, 78.4) | 0.4(0, 0.7) | 84.4(80.5, 88.2) | 71.2(67.1, 75.4) | 90.4(86.4, 94.4) | 82.3(78.1, 86.5) | 39.1(29.3, 48.8) | 0 | |
| Ningxia | 1035 | 75.9(71.8, 80.1) | 1.6(0.5, 2.8) | 82.0(74.6, 89.5) | 70.4(64.5, 76.4) | 95.1(92.3, 97.8) | 86.4(84.2, 88.6) | 37.7(29.0, 46.5) | 0.60(0, 1.53) | |
| Xinjiang | 1070 | 87.7(82.7, 92.8) | 0.8(0, 1.7) | 74.7(67.4, 82.1) | 60.1(51.3, 68.9) | 92.2(88.8, 95.5) | 82.7(76.6, 88.9) | 43.0(38.2, 47.8) | 0.12(0, 0.41) | |
| Total | 44874 | 68.5(67.4, 69.6) | 5.3(4.7, 5.9) | 79.9(78.6, 81.3) | 67.0(65.7, 68.3) | 88.9(88.1, 89.6) | 71.8(70.5, 73.2) | 30.9(29.6, 32.1) | 0.62(0.50, 0.75) |
Not including China Hong Kong, Macao and Taiwan.
Redder color means higher value of point estimation for individual ideal metrics, bluer means lower value of point estimation.
Proportion and 95% confidence interval.
In urban areas, mean CVH score ranged from 9.55 (95% CI: 9.45, 9.66) in Shanxi to 10.69 (95% CI: 10.47, 10.92) in Guangdong, while the range for rural areas was from 9.42 (95% CI: 9.32, 9.53) in Beijing to 10.50 (95% CI: 10.21, 10.80) in Ningxia. Fig. 3 shows some differences in CVH score, HBS, and HFS between urban and rural areas. There were higher CVH scores in the urban areas of the southeast and the rural areas of the northwest and southeast. For HBS, similar patterns were observed between urban and rural residents. Both urban and rural residents in the northwest had higher HFS.
Fig. 3.
Age- and sex-standardized CVH score, Health Behaviors Score and Health Factors Score in urban and rural area across China, 2015. (A) CVH score in urban area. (B) CVH score in rural area. (C) Health Behaviors Score in urban area. (D) Health Behaviors Score in rural area. (E) Health Factors Score in urban area. (F) Health Factors Score in rural area.
Differences in CVH score, HBS and HFS between urban and rural areas for 31 provinces was presented in eFig. 1 in the Supplement. Differences in CVH score between urban and rural areas were positively associated with SDI (R2 = 0.266, P = 0.003, Fig. 4). There was a similar association for the differences in HBS (R2 = 0.283, P = 0.002). However, the association between the differences in HFS and SDI was only marginally significant (R2 = 0.088, P = 0.106).
Fig. 4.
The association of Socio-demographic Index with differences in CVH score, Health Behaviors Score, and Health Factors Score for urban and rural areas. (A) CVH score. (B) Health Behaviors Score. (C) Health Factors Score. Each dot shows an individual province. The blue lines indicate the fitting lines. The blue areas show the 95% confidence intervals of the fitting lines.
3.5. Between-gender differences
The prevalence of ideal CVH was 0.45% (95% CI: 0.26%, 0.64%) among men, and 1.68% (95% CI: 1.38%, 1.98%) among women. The distributions of all seven CVH metrics stratified by gender groups are shown in eTable 3 in the Supplement. Except for ideal healthy diet (6.9% in women vs. 7.4% in men), women had higher proportions of ideal levels for all CVH items. They had more than double the proportion of ideal smoking levels than men.
Women had higher mean scores than men for CVH score, HBS, and HFS [10.88 (95% CI: 10.84, 10.93) vs. 9.58 (95% CI: 9.53, 9,64), 6.12 (95% CI: 6.09, 6.15) vs. 5.03 (95% CI: 4.99, 5.07), 6.72 (95% CI: 6.69, 6.75) vs. 5.48 (95% CI: 5.43, 5.53)]. The spatial patterns of CVH score, HBS and HFS were quite similar between genders, although there were some variations in several provinces (eFig. 2 in the Supplement). For example, HBS was lowest for women, but highest for men, in Tibet. Gender differences in CVH score, HBS, and HFS were not significantly associated with SDI (eFig. 3 in the Supplement).
3.6. The relationship between SDI and CVH
We assessed the associations between SDI and CVH score, HBS and HFS (eFig. 4 in the Supplement). The associations of SDI with seven individual CVH metrics and overall ideal CVH for the population, by urban/rural residents, by men/women are shown in eFigs. 5–9 in the Supplement.
4. Discussion
This study used a large, provincially representative survey of the adult Chinese population to describe the general profile of CVH and its spatial patterns in 2015. The overall CVH among Chinese adults in all provinces was extraordinarily poor and there was substantial variation between provinces. Quantifying CVH status in the general population and identifying its spatial pattern is important for public health knowledge and may improve policy development. The difference in CVH between urban and rural residents appears to be associated with local socio-economic development. Better CVH was seen in urban areas of provinces with higher SDI, and in rural areas of provinces with lower SDI. Overall, our findings suggest the importance of geographically targeted strategies for improving CVH.
Several studies have previously found extremely low prevalence of ideal CVH in China [[16], [17], [18],28] and other countries [29], [30], [31], [32], [33]. Based on the 2010 China Noncommunicable Disease Surveillance, one previous study reported that the estimated percentage of ideal CVH was as low as 0.2% in the general population of Chinese adults aged ≥ 20 years [16]. Our estimation (1.13%) was a slight improvement on this figure. This may be partially explained by the ongoing reforms to the primary healthcare system[34], and national health promotion activities, such as China Healthy Lifestyle for All [35]. However, considerable work is still needed to improve CVH in China.
Only a few participants in our study had an ideal diet. This was consistent with the findings of most previous studies from China and other countries [7,13,16,30,31]. The positive association between socio-economic development and the prevalence of ideal diet was consistent with several other studies at individual level [36], [37], [38]. It suggests that there has been increasing demand for a healthier diet linked to rapid economic development in recent decades. Another important finding is that just 31.2% of Chinese adults had an ideal blood pressure level of below 120/80 mm Hg. Uncontrolled blood pressure is the most important risk factor among the CVH metrics, accounting for 33.0–47.2% of atherosclerotic CVD events in China [39]. Our findings further emphasized the importance of promoting good dietary habits and preventing high blood pressure in improving overall CVH status and then reducing the CVD burden in China.
Our study found large geographical variations in ideal CVH, CVH score, HBS, and HFS. The lowest CVH score, HBS, and HFS were in northern China. Although only roughly dividing China into the north and south, Bi et al. [16] also reported that the overall levels of ideal CVH were worse in northern China. We found that in the west, the scores for health factors were better, but the HBS was lower. Better health behaviors but moderate levels of health factors were observed in the south and east of China. It is generally agreed that health behaviors strongly influence healthy factors, including blood pressure, fasting glucose, and total cholesterol, even before the preclinical phase (suboptimal health). Promotion on healthy behaviors owns much merits, in the perspective of primordial prevention. These health behaviors will result in better scores for health factors in these regions in future. Information and knowledge about behaviors associated with CVD prevention is not evenly distributed across different areas in China [35,40], and this probably contributed to the current levels of health behaviors. Our findings suggest that the burden of CVD in specific districts could be partly addressed by regional-level approaches.
In most provinces, the prevalence of ideal CVH and CVH scores was higher in urban than rural areas. Individuals in rural areas tended to have non-ideal CVH, probably because of higher levels of unhealthy lifestyles in rural residents [41,42]. Compared with previous data from 2010 [16], the rate of ideal CVH had increased among both urban and rural residents, but the gap between the two seemed to be widening. Our study further showed that differences between urban and rural areas in CVH score and HBS were associated with socio-economic development, with higher CVH score among urban residents in more developed provinces. In developed areas, there may be greater disparities in the proportion of higher incomes and education levels between urban and rural residents, both of which affect CVH [38,43,44]. This suggests that there will be a gradual transition over time in provinces with lower socio-economic status, as the economy improves, and CVH score in urban areas will eventually overtake that in rural areas. Our study also suggested that the difference in CVH score were mostly attributed to variations in health behaviors between urban and rural areas. This may mean that this could be addressed by timely and targeted implementation of public policies, especially behavioral interventions among rural residents of developing areas.
Our study has several strengths. First, the survey was designed to achieve both national and provincial representativeness under a unified and rigorous sampling scheme, which assured validity of the results. This study has made the first attempt to our knowledge to assess the spatial pattern of CVH at provincial level. A large sample size, standardized survey tools, training and field implementation were all designed to improve the reliability of the analysis. The definition of urban and rural areas was based on the finest microscale at village/community level, which helped capture the true differences between the two. The ideal metrics were also in line with AHA's ideal CVH criteria, which could facilitate the comparison of our findings with other studies. However, our study also had several limitations. Individual history of cardiovascular disease was based on self-reports, and our study might therefore have underestimated the proportion of individuals with a history of cardiovascular disease. This would have resulted in an imprecise estimation of the proportion of ideal CVH in Chinese adults. The information of smoking and diet was collected by questionnaire. But compared to three-day dietary recall survey, quantitative food frequency questionnaire was used to provide more precise and accurate estimates of long-term food intake behavior without being affected by survey season or temporary changes in food composition. Also, considering unaffordable cost of accelerometer in such a large survey, we only relied on self-reports to measure physical activity. Moreover, the effect of ideal CVH on healthy outcome, especially the occurrence of preclinical phase, was not evaluated in this study, which might be further assessed in future studies.
5. Conclusion
Our study indicates that the prevalence of ideal CVH among Chinese adults is extremely low, especially healthy diet and blood pressure. There are also substantial spatial variations across different areas of the country. Both comprehensive and localized health strategies and measurements will be needed to improve the CVH status across the country, and narrow geographical inequities, before it will be possible to reduce the prevalence of CVD in China.
Declaration of Competing Interest
There are no conflicts of interest to declare.
Acknowledgments
Author contribution
LW, YL and XL designed the study. MZ and YS analyzed the data and drafted the manuscript. OS, ZZ, XZ, CL, ZH and LZ critically revised the manuscript. All authors gave final approval for the version to be published.
Acknowledgment
The authors thank the staff of the provincial and regional centers for disease control and prevention for collecting data, and study participants for their participation and contribution.
Data sharing
The study data that underlie the results of this article will be available for investigators after approval by the Chinese Center for Disease Control and Prevention (Beijing, China). Please email the corresponding author for more information.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lanwpc.2020.100033.
Contributor Information
Limin Wang, Email: wanglimin@ncncd.chinacdc.cn.
Yichong Li, Email: yichongli.cvd@139.com.
Xinhua Li, Email: lixinhua@chinacdc.cn.
Appendix. Supplementary materials
References
- 1.Sacco RL, Roth GA, Reddy KS. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American Heart Association and World Heart Federation. Glob Heart. 2016;11(2):251–264. doi: 10.1016/j.gheart.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Liu S, Li Y, Zeng X. Burden of cardiovascular diseases in China, 1990–2016. JAMA Cardiol. 2019;4(4):342–352. doi: 10.1001/jamacardio.2019.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute for Health Metrics and Evaluation (IHME) IHME, University of Washington; Seattle, WA: 2017. GBD compare data visualization.http://vizhub.healthdata.org/gbd-compare [Google Scholar]
- 4.Lloyd-Jones DM, Hong Y, Labarthe D. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 5.Wang Y, Liu X, Qiu J. Association between Ideal cardiovascular health metrics and suboptimal health status in Chinese population. Sci Rep. 2017;7(1):14975. doi: 10.1038/s41598-017-15101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Z, Yang X, Wang A. Association between Ideal cardiovascular health metrics and depression in Chinese population: a cross-sectional study. Sci Rep. 2015;5:11564. doi: 10.1038/srep11564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaye B, Canonico M, Perier M-C. Ideal cardiovascular health, mortality, and vascular events in elderly subjects. J Am Coll Cardiol. 2017;69(25):3015–3026. doi: 10.1016/j.jacc.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Dong C, Rundek T, Wright CB, Anwar Z, Elkind MSV, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics. Circulation. 2012;125(24):2975–2984. doi: 10.1161/CIRCULATIONAHA.111.081083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu S, Huang Z, Yang X. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5(4):487–493. doi: 10.1161/CIRCOUTCOMES.111.963694. [DOI] [PubMed] [Google Scholar]
- 11.Miao C, Bao M, Xing A. Cardiovascular health score and the risk of cardiovascular diseases. PLoS One. 2015;10(7) doi: 10.1371/journal.pone.0131537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Y, Chi HJ, Cui LF. The ideal cardiovascular health metrics associated inversely with mortality from all causes and from cardiovascular diseases among adults in a Northern Chinese industrial city. PLoS One. 2014;9(2):e89161. doi: 10.1371/journal.pone.0089161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang Q, Cogswell ME, Flanders WD. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125(8):987–995. doi: 10.1161/CIRCULATIONAHA.111.049122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corlin L, Short MI, Vasan RS, Xanthakis V. Association of the duration of ideal cardiovascular health through adulthood with cardiometabolic outcomes and mortality in the framingham offspring study. JAMA Cardiol. 2020;5(5):1–8. doi: 10.1001/jamacardio.2020.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bi Y, Jiang Y, He J. Status of cardiovascular health in Chinese adults. J Am Coll Cardiol. 2015;65(10):1013–1025. doi: 10.1016/j.jacc.2014.12.044. [DOI] [PubMed] [Google Scholar]
- 17.Chang Y, Guo X, Chen Y. Prevalence and metrics distribution of ideal cardiovascular health: a population-based, cross-sectional study in rural China. Heart Lung Circ. 2016;25(10):982–992. doi: 10.1016/j.hlc.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 18.Wu HY, Sun ZH, Cao DP, Wu LX, Zeng Q. Cardiovascular health status in Chinese adults in urban areas: analysis of the Chinese Health Examination Database 2010. Int J Cardiol. 2013;168(2):760–764. doi: 10.1016/j.ijcard.2012.09.235. [DOI] [PubMed] [Google Scholar]
- 19.Chung J, Wong B, Yan V, Chung L, So H, Chan A. Cardiovascular health of construction workers in Hong Kong: a cross-sectional study. Int J Environ Res Public Health. 2018;15(6):1251. doi: 10.3390/ijerph15061251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu S, Wu X, Lopez AD. An integrated national mortality surveillance system for death registration and mortality surveillance, China. Bull World Health Organ. 2016;94(1):46–57. doi: 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prevention CCfDCa. Global Adult Tobacco Survey (GATS) China 2010 CountryReport.https://www.who.int/tobacco/surveillance/survey/gats/chn/en/.
- 22.Orgnization WH. Global Physical Activity Questionnaire (GPAQ). https://www.who.int/ncds/surveillance/steps/GPAQ_EN.pdf.
- 23.Zhao WH, Huang ZP, Zhang X. Reproducibility and validity of a Chinese food frequency questionnaire. Biomed Environ Sci. 2010;23:1–38. [Google Scholar]
- 24.Pang SJ, Man QQ, Song S. Relationships of insulin action to age, gender, body mass index, and waist circumference present diversely in different glycemic statuses among chinese population. J Diabetes Res. 2018;2018 doi: 10.1155/2018/1682959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou M, Wang H, Zeng X. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Altmayer L. Proceedings of the 2002 Northeast SAS user's group. 2002. Hot-deck imputation: a simple DATA step approach; pp. 773–780. [Google Scholar]
- 27.Steven GH, Brady TW, Patricia AB. CRC Press; 2010. Applied Survey Data Analysis: [Google Scholar]
- 28.Zeng Q, Dong SY, Song ZY, Zheng YS, Wu HY, Mao LN. Ideal cardiovascular health in Chinese urban population. Int J Cardiol. 2013;167(5):2311–2317. doi: 10.1016/j.ijcard.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 29.Benziger CP, Zavala-Loayza JA, Bernabe-Ortiz A. Low prevalence of ideal cardiovascular health in Peru. Heart. 2018;104(15):1251–1256. doi: 10.1136/heartjnl-2017-312255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Machado LBM, Silva BLS, Garcia AP. Ideal cardiovascular health score at the ELSA-Brasil baseline and its association with sociodemographic characteristics. Int J Cardiol. 2018;254:333–337. doi: 10.1016/j.ijcard.2017.12.037. [DOI] [PubMed] [Google Scholar]
- 31.Graciani A, Leon-Munoz LM, Guallar-Castillon P, Rodriguez-Artalejo F, Banegas JR. Cardiovascular health in a southern Mediterranean European country: a nationwide population-based study. Circ Cardiovasc Qual Outcomes. 2013;6(1):90–98. doi: 10.1161/CIRCOUTCOMES.112.967893. [DOI] [PubMed] [Google Scholar]
- 32.Kim JY, Ko Y-J, Rhee CW. Cardiovascular health metrics and all-cause and cardiovascular disease mortality among middle-aged men in Korea: the Seoul male cohort study. J Prev Med Public Health. 2013;46(6):319–328. doi: 10.3961/jpmph.2013.46.6.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shay CM, Ning H, Allen NB. Status of cardiovascular health in US adults. Circulation. 2012;125(1):45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li X, Lu J, Hu S. The primary health-care system in China. Lancet. 2017;390(10112):2584–2594. doi: 10.1016/S0140-6736(17)33109-4. [DOI] [PubMed] [Google Scholar]
- 35.Wang J, Ma J, Yang Y, Shi W. Analysis on the work status of the instructors of China healthy lifestyle for all. Chin J Prev Contr Chron Dis. 2019;27(10):736–739. in Chinese. [Google Scholar]
- 36.Manios Y, Kourlaba G, Kondaki K. Diet quality of preschoolers in Greece based on the Healthy Eating Index: the GENESIS study. J Am Diet Assoc. 2009;109(4):616–623. doi: 10.1016/j.jada.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 37.Kant AK, Graubard BI. Secular trends in the association of socio-economic position with self-reported dietary attributes and biomarkers in the US population: National Health and Nutrition Examination Survey (NHANES) 1971–1975 to NHANES 1999–2002. Public Health Nutr. 2007;10(2):158–167. doi: 10.1017/S1368980007246749. [DOI] [PubMed] [Google Scholar]
- 38.Mullie P, Clarys P, Hulens M, Vansant G. Dietary patterns and socioeconomic position. Eur J Clin Nutr. 2010;64(3):231–238. doi: 10.1038/ejcn.2009.145. [DOI] [PubMed] [Google Scholar]
- 39.Han C, Liu F, Yang X. Ideal cardiovascular health and incidence of atherosclerotic cardiovascular disease among Chinese adults: the China-PAR project. Sci China Life Sci. 2018;61(5):504–514. doi: 10.1007/s11427-018-9281-6. [DOI] [PubMed] [Google Scholar]
- 40.Yang Y, Wang J, Shi W, Ma J. The trend analysis of healthy settings development for China healthy lifestyle for all from 2013 to 2018. Chin J Prev Contr Chron Dis. 2019;27(10):732–735. in Chinese. [Google Scholar]
- 41.WHO Report on the Global Tobacco Epidemic 2011. 2011.
- 42.Yang G, Kong L, Zhao W. Emergence of chronic non-communicable diseases in China. Lancet. 2008;372(9650):1697–1705. doi: 10.1016/S0140-6736(08)61366-5. [DOI] [PubMed] [Google Scholar]
- 43.Mistry R, McCarthy WJ, de Vogli R, Crespi CM, Wu Q, Patel M. Adolescent smoking risk increases with wider income gaps between rich and poor. Health Place. 2011;17(1):222–229. doi: 10.1016/j.healthplace.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Foraker RE, Bush C, Greiner MA. Distribution of cardiovascular health by individual- and neighborhood-level socioeconomic status: findings from the Jackson heart study. Glob Heart. 2019;14(3):241–250. doi: 10.1016/j.gheart.2019.04.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.