Abstract
Objective:
To evaluate the surface of glazed lithium disilicate dental ceramics after irradiation under different irradiation settings of Nd:YAG and Er:YAG lasers using a scanning electron microscope (SEM).
Materials and Methods:
Three glazed-press lithium disilicate ceramic discs were treated with HF, Er:YAG, and Nd:YAG, respectively. The laser-setting variables tested were laser mode, repetition rate (Hz), power (W), time of exposure (seconds), and laser energy (mJ). Sixteen different variable settings were tested for each laser type, and all the samples were analyzed by SEM at 500× and 1000× magnification.
Results:
Surface analysis of the HF-treated sample showed a typical surface texture with a homogenously rough pattern and exposed ceramic crystals. Er:YAG showed no effect on the surface under any irradiation setting. The surface of Nd:YAG-irradiated samples showed cracking, melting, and resolidifying of the ceramic glaze. These changes became more pronounced as the power increased. At the highest power setting (2.25 W), craters on the surface with large areas of melted or resolidified glaze surrounded by globules were visible. However, there was little to no exposure of ceramic crystals or visible regular surface roughening.
Conclusions:
Neither Er:YAG nor Nd:YAG dental lasers exhibited adequate surface modification for bonding of orthodontic brackets on glazed lithium disilicate ceramics compared with the control treated with 9.5% HF.
Keywords: Orthodontic bonding, Lithium disilicate, Er:YAG, Nd:YAG, Dental lasers, Hydrofluoric acid
INTRODUCTION
With the increased popularity of esthetic dentistry, the number of adult orthodontic patients in USA and Canada grew by 14% in the period 2010–2012.1 Orthodontists more frequently encounter patients who have one or more ceramic restorations. Application of 9.5% hydrofluoric acid (HF) for up to 90 seconds can be regarded as a standard technique that provides adequate surface roughening, thus sufficient bond strength for orthodontic bonding.2,3 Nevertheless, there are disadvantages such as lengthy etching time and the risk of severe trauma to soft tissues and tooth substance.4
With advances in technology, the application of lasers in dentistry has increased. Different types of lasers have been used in orthodontics for conditioning enamel before bonding brackets and have shown acceptable results.5 Results with porcelain surfaces are more controversial. Poosti et al. showed that Nd:YAG laser irradiation was an acceptable substitute for hydrofluoric acid; however, the Er:YAG laser was not. Information about laser parameter settings is limited to a laser power of 0.8 W at 10-seconds' duration.6 Hosseini et al. used laser power of 1.5 W, 10-Hz frequency, and 100-μ pulse duration, also showing acceptable results. They concluded that 0.75 W had little potential to promote mechanical porosity.7 Akpinar et al. showed shear bond strength levels that were inadequate for clinical application with an Nd:YAG laser at 4 W.5
All previously reported studies have investigated feldspathic ceramics with little or no data about the effects of Nd:YAG or Er:YAG lasers on lithium disilicate ceramics. Even with the increasing number of these cements compared with feldspathic ceramic prosthetic restorations, the effect of lasers on these types of restorations is still unknown. The aim of this study was to evaluate and compare lithium disilicate ceramic surfaces with different parameters of Nd:YAG and Er:YAG lasers using a scanning electron microscope (SEM) after treatment.
MATERIALS AND METHODS
Three glazed-press lithium disilicate ceramic discs (e.max.Press, Ivoclar Vivadent, Schaan, Lichtenstein) with a diameter of 10 mm and a thickness of 2 mm were produced according to the manufacturer's recommendations.
Sample 1 served as control, treated with 9.5% hydrofluoric acid (porcelain etchant, Bisco Inc, Schaumburg, Ill) for 20 seconds, rinsed under tap water for 20 seconds, and air-dried. On the two remaining samples, a grid was outlined with 16 squares (4 × 4) using a permanent, water-resistant marker pen. The laser-setting variables tested were laser mode, repetition rate (Hz), power (W), length of exposure (seconds), and laser energy (mJ).
Sample 2 was treated with 16 different settings of an Nd:YAG laser (Fotona, Fidelis, Ljubljana, Slovenia) via a sweeping motion at a distance of 4 mm from the surface. The various laser settings are shown in Table 1. The distance between the tip of the laser handpiece and the porcelain surface was adjusted to 4 mm using a special holder attached to the handpiece. Using the same technique, sample 3 was treated with an Er:YAG laser (Fotona; the settings are presented in Table 2). Water cooling was not applied during the laser application.
Table 1.
The 16 different settings of Nd:YAG laser at MSP laser mode and 10-Hz repetition rate (power: 0.5–2.25 W and time: 3–5 s)
| 0.5 W, 3 s | 0.75 W, 3 s | 1 W, 3 s | 1.25 W, 3 s |
| 1.5 W, 3 s | 1.75 W, 3 s | 2 W, 3 s | 2.25 W, 3 s |
| 0.5 W, 5 s | 0.75 W, 5 s | 1 W, 5 s | 1.25 W, 5 s |
| 1.5 W, 5 s | 1.75 W, 5 s | 2 W, 5 s | 2.25 W, 5 s |
Table 2.
Er:YAG laser with 16 different settings (laser mode: QSP, SP, or MAX; energy: 400–1000 mJ; repetition rate: 10 or 15 Hz; and power: 4–15 W). All samples were treated for 20 seconds
| QSP 400 mJ, 10 Hz, 4 W | QSP 450 mJ, 10 Hz, 4.5 W | QSP 500 mJ, 10 Hz, 5 W | QSP 550 mJ, 10 Hz, 5.5 W |
| QSP 600 mJ, 10 Hz, 6 W | QSP 650 mJ, 10 Hz, 6.5 W | QSP 700 mJ, 10 Hz, 7 W | QSP 750 mJ, 10 Hz, 7.5 W |
| SP 400 mJ, 10 Hz, 4 W | SP 500 mJ, 10 Hz, 5W | SP 600 mJ, 10 Hz, 6 W | SP 700 mJ, 10 Hz, 7 W |
| SP 800 mJ, 10 Hz, 8 W | SP 900 mJ, 10 Hz, 9 W | SP 1000 mJ, 10 Hz, 10 W | MAX 1000 mJ, 15 Hz, 15 W |
After surface modifications, the samples were sputter coated with gold for 120 seconds to reduce scanning faults and image artifacts. These were analyzed by a SEM at a magnification of 500× and 1000× (Vega Tescan TS5136LS, Tescan Orsay, Brno-Kohoutovice, Czech Republic).
RESULTS
SEM comparative images are shown in Figures 1 to 5. Figure 1 shows the untreated glazed-lithium disilicate ceramic surface with little or no irregularities. Figure 2 shows the control sample surface-etched with 9.5% hydrofluoric acid. The surface is typical of acid-etched lithium disilicate, with a homogenously rough pattern and exposed ceramic crystals. Figure 3 shows the surfaces that the Er:YAG laser irradiated with increasing power and frequency settings and constant irradiation time. No effect is visible on the sample surfaces. The same surface with no effect was visible when Er:YAG was used to treat the surfaces at varying times, pulse settings, and power; however, the frequency was constant. The Nd:YAG irradiated surfaces with varying time and power settings and constant frequency are shown in Figure 4. The effects became visible as the power and exposure time were increased. The glaze shows fracture formation and melting, with melting and resolidification as the laser power was increased. At the maximum power setting of 2.25 W and 5 seconds' duration, surface craters are visible with large areas of melted and resolidified glaze surrounded by globules (Figure 5). No regular porosity or exposure of ceramic crystals is visible.
Figure 1.
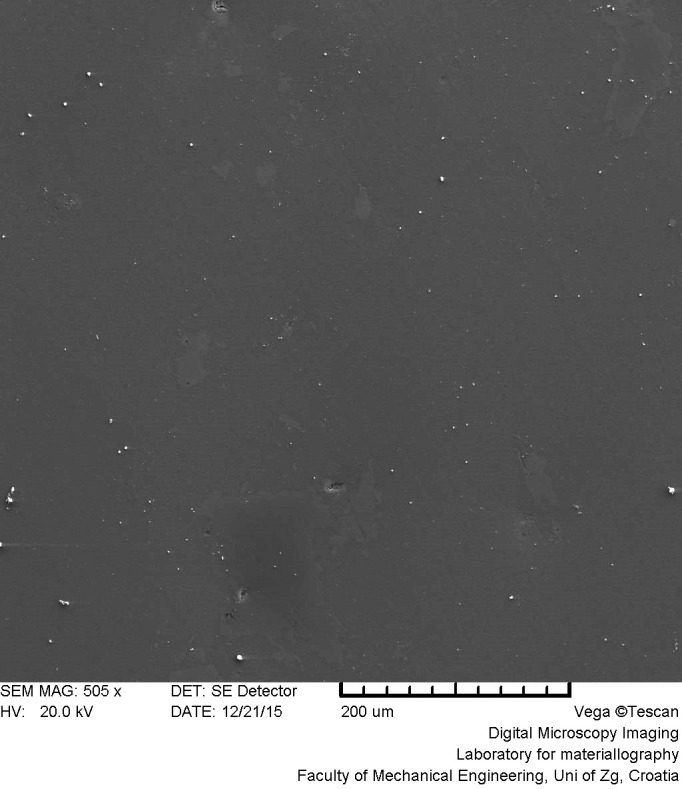
Untreated glazed lithium disilicate ceramic surface.
Figure 5.
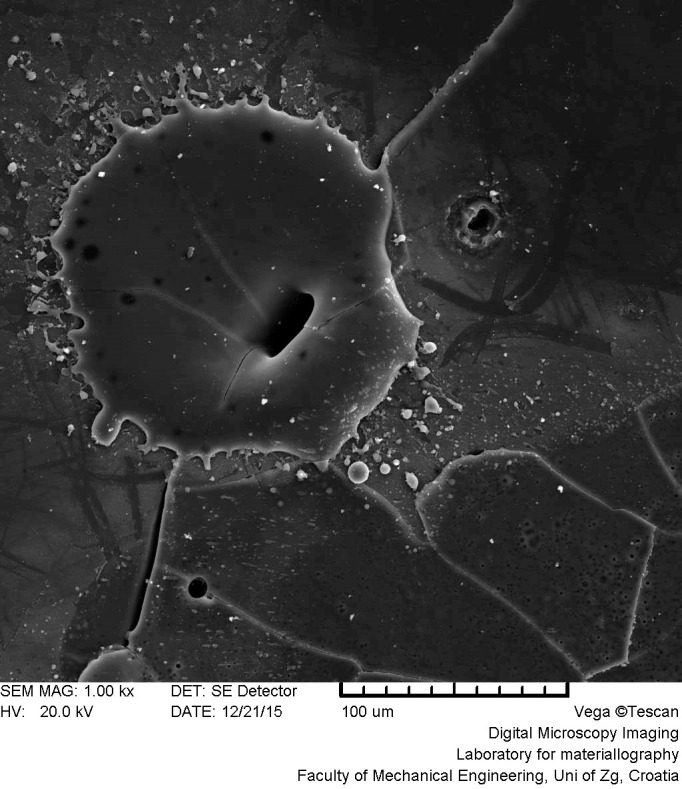
Nd:YAG laser–irradiated lithium disilicate ceramic surface with large areas of cracked, melted, and resolidified glaze surrounded by globules (MSP 2.25 W, 10 Hz, 5 seconds).
Figure 2.
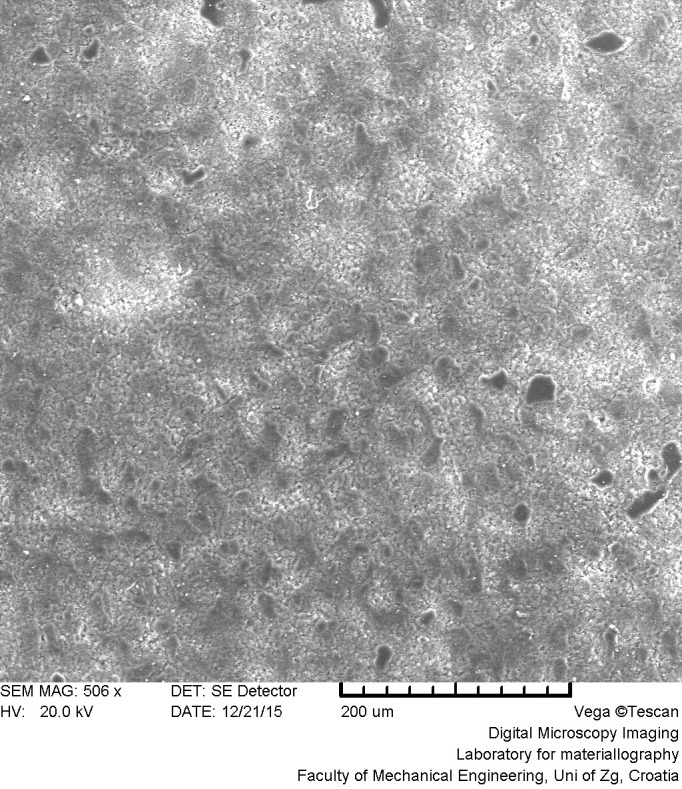
Control sample surface etched with 9.5% hydrofluoric (HF) acid.
Figure 3.
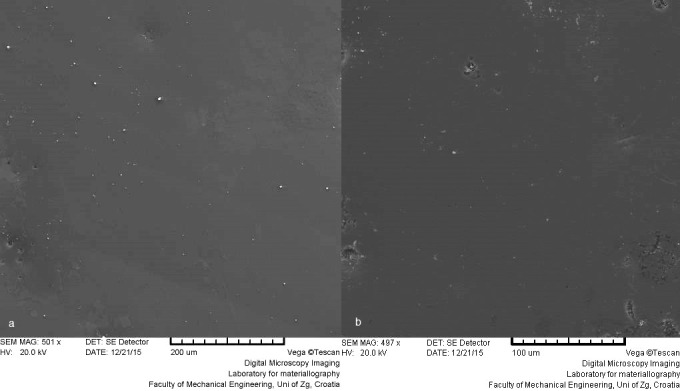
Er:YAG laser–irradiated lithium disilicate ceramic surfaces with increasing power and frequency settings and constant irradiation time: (a) QSP 450 mJ, 10 Hz, 4.5 W ; (b) MAX 1000 mJ, 15 Hz, 15 W.
Figure 4.
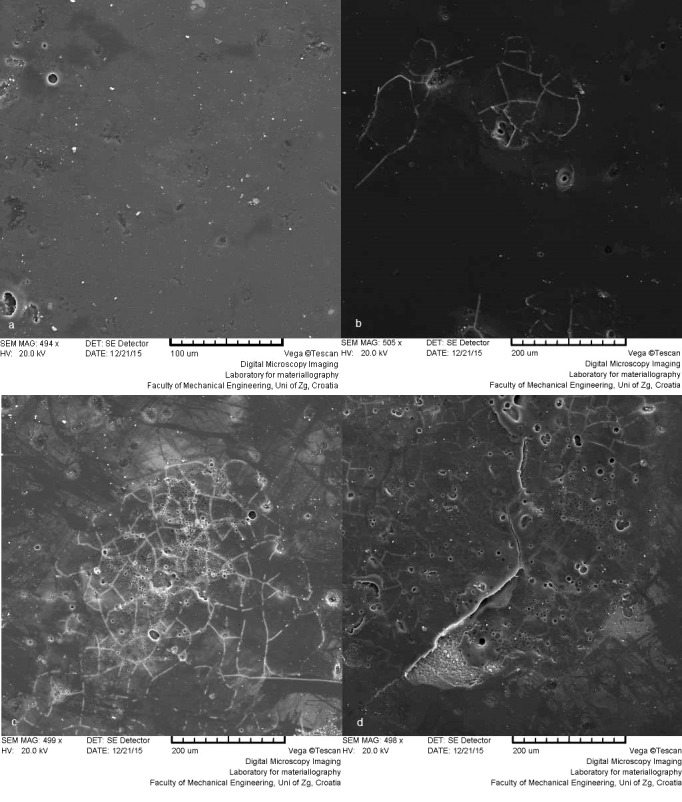
Nd:YAG laser–irradiated lithium disilicate ceramic surfaces with varying time and power settings and constant frequency: (a) MSP 1 W, 10 Hz, 3 seconds; (b) MSP 2 W, 10 Hz, 3 seconds; (c) MSP 1.5 W, 10 Hz, 5 seconds; (d) MSP 2.25 W, 10 Hz, 5 seconds.
DISCUSSION
With patients' increasing esthetic demands, lithium disilicate crowns are emerging as a viable prosthodontic solution for both esthetic and long-term functional problems.8 It is inevitable that orthodontists will encounter these restorations in clinical situations and need to include such restored teeth in orthodontic therapy. So far, etching with HF and sandblasting have been proposed for ceramic surface preparation, with both limitations and inherent risk.9 Etching to composite resin has been shown to result in the most effective surface preparation and the highest bond strengths.10 However, if handled or applied incorrectly in clinical situations, it also carries the highest patient risk due to possible hard or soft tissue damage. It also complicates the orthodontists' workflow with mandatory use of a rubber dam and adequate suction, which can be time consuming and possibly uncomfortable for patients.11,12
However, the above-mentioned concerns with HF can be eliminated by using lasers for ceramic surface preparation. Er:YAG dental lasers emit light at λ = 2940 nm, and the main interaction is with water molecules within hard or soft dental tissues. Energy transfer and subsequent water evaporation result in tissue ablation with little or no heat transfer to the surrounding tissues.13 In the current study, no effect on the surface of the lithium disilicate was visible after Er:YAG laser application. This can be explained on the basis that there is no water in dental ceramics, thus resulting in ineffective energy transfer. Also, it appears that there is no interaction with lithium disilicate crystals as there is with hydroxyapatite in bone or dental hard tissue. However, the absorption of Er:YAG laser light in hydroxyl-apatite has a secondary role in ablation, with water content of irradiated structures being the deciding factor.14
Poosti et al. have stated that Er:YAG-irradiated porcelain was found to be in the lower-than-acceptable range of bracket bond strength for clinical orthodontics, which is consistent with the current findings of no surface effect.6 Their study was, however, on feldspathic dental ceramics, which have no water content in their structure. Topcuoglu et al. also stated that Er:YAG dental lasers were ineffective in creating an adequate bonding surface for orthodontic brackets to feldspathic ceramics; however, their SEM analyses showed ablation and roughening of the surface.15 This might be due to the water irrigation they applied during laser irradiation. Meister et al. have shown that the water component of dental enamel does not contribute to the ablation process when using pulsed erbium lasers and that the ablation process is feasible only if water spray is supplied externally.16 In the current study, water cooling was not applied and that is a possible reason for the discrepancies found in previous studies.
In the recent literature, Er:YAG dental lasers have been proposed for removing lithium disilicate restorations from patients' teeth.17,18 This method is based on the passing of laser light through the restoration without interaction and the consequent ablation of water molecules within the adhesive cement layer beneath the restoration. If such interaction were to occur during laser application for surface preparation before bracket bonding, a catastrophic failure of the restoration would occur, resulting in the need to replace the restoration and postponement of orthodontic treatment. It should also be mentioned that the Er-YAG laser does not significantly affect the mineral composition of dental enamel,19 but no study has evaluated photon interaction parameters of glazed-lithium disilicate ceramics after Er:YAG or Nd:YAG laser treatment.
Nd:YAG dental lasers emit light in the infrared spectrum with λ = 1064 nm and, like any energy transfer in the infrared spectrum, heat transfer occurs on the surface of the irradiated object. Depending on the power of the laser and the surface quality, depth of penetration can vary. When the laser is applied to dentin, melting of the hydroxyapatite and closure or complete obliteration of the dentinal tubules occur.20 Exposure to Nd:YAG laser energy, even for a short time, leads to a glazed, melted, resolidified surface and sometimes even by the formation of globules and cracks.21 These changes were seen on the surface of the irradiated samples in this study, with visible cracks, melting, and resolidifying. With increased laser energy, craters surrounded by globules of erupted glaze appeared on the surface. As the glaze firing temperature is 840°C, it can be assumed that energy transfers at the sample surfaces produced temperatures higher than that.
The idea of this study was to evaluate surface quality prior to bracket bonding. Compared with the surface of the control samples that were treated with HF acid, the Nd:YAG group samples showed a visually different surface. On the SEM images, there was little sign of surface roughening, which would increase the surface area and facilitate better bracket bonding. This conclusion is at odds with the findings of Poosti et al., who stated that the surface was adequate for orthodontic bonding.6 Moreover, the introduction of surface cracks could lead to fracture propagation deeper in the ceramic material and not only debonding, but also chipping and possibly restoration failure and the need for replacement. Akpinar et al. also showed shear bond strength levels that were not adequate for clinical application when using a Nd:YAG laser at 4 W.5 However, both findings are based on visual observations of SEM images, so that further studies investigating surface roughness using confocal microscope analysis of depth22 and bond strength should be conducted before conclusions can be drawn.
CONCLUSIONS
Within the limitations of this study, the following conclusions were made:
Neither Er:YAG nor Nd:YAG dental lasers exhibited adequate surface modification for orthodontic bonding on glazed-lithium disilicate dental ceramic samples compared with the control treated with 9.5% HF acid.
Er:YAG laser showed no effect under any irradiation setting. With Er-YAG, as for Nd:YAG laser, increasing the energy settings resulted in cracking, melting and resolidifying of the surface glaze.
ACKNOWLEDGMENTS
This research was partly supported by a grant from the University of Zagreb for the project Research of Ceramic Systems and Materials in Prosthodontics.
REFERENCES
- 1.American Association of Orthodontists. Smiles are in style. New study says adults are seeking orthodontic treatment in record numbers 2014 Jan 25; . http://mylifemysmile.org/cms/wp-content/uploads/2014/10/Results-of-2012-AAO-Patient-Census-Survey_0.pdf Accessed.
- 2.Lestrade AM, Ballard RW, Xu X, Yu Q, Kee EL, Armbruster PC. Porcelain surface conditioning protocols and shear bond strength of orthodontic brackets. Aust Orthod J. 2016;32:18–22. [PubMed] [Google Scholar]
- 3.Grewal Bach GK, Torrealba Y, Lagravère MO. Orthodontic bonding to porcelain: a systematic review. Angle Orthod. 2014;84:555–560. doi: 10.2319/083013-636.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahrari F, Heravi F, Hosseini M. CO2 laser conditioning of porcelain surfaces for bonding metal orthodontic brackets. Lasers Med Sci. 2013;28:1091–1097. doi: 10.1007/s10103-012-1152-x. [DOI] [PubMed] [Google Scholar]
- 5.Akpinar YZ, Irgin C, Yavuz T, Aslan MA, Kilic HS, Usumez A. Effect of femtosecond laser treatment on the shear bond strength of a metal bracket to prepared porcelain surface. Photomed Laser Surg. 2015;33:206–212. doi: 10.1089/pho.2014.3791. [DOI] [PubMed] [Google Scholar]
- 6.Poosti M, Jahanbin A, Mahdavi P, Mehrnoush S. Porcelain conditioning with Nd:YAG and Er:YAG laser for bracket bonding in orthodontics. Lasers Med Sci. 2012;27:321–324. doi: 10.1007/s10103-010-0878-6. [DOI] [PubMed] [Google Scholar]
- 7.Hosseini MH, Sobouti F, Etemadi A, Chiniforush N, Shariati M. Shear bond strength of metal brackets to feldspathic porcelain treated by Nd:YAG laser and hydrofluoric acid. Lasers Med Sci. 2015;30:837–841. doi: 10.1007/s10103-013-1458-3. [DOI] [PubMed] [Google Scholar]
- 8.Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth–supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs) Dent Mater. 2015;31:603–623. doi: 10.1016/j.dental.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 9.Zarif Najafi H, Oshagh M, Torkan S, Yousefipour B, Salehi R. Evaluation of the effect of four surface conditioning methods on the shear bond strength of metal bracket to porcelain surface. Photomed Laser Surg. 2014;32:694–699. doi: 10.1089/pho.2014.3782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duzyol M, Sagsoz O, Polat Sagsoz N, Akgul N, Yildiz M. The effect of surface treatments on the bond strength between CAD/CAM blocks and composite resin. J Prosthodont. 2016;25:466–471. doi: 10.1111/jopr.12322. [DOI] [PubMed] [Google Scholar]
- 11.Zachrisson YO, Zachrisson BU, Büyükyilmaz T. Surface preparation for orthodontic bonding to porcelain. Am J Orthod Dentofacial Orthop. 1996;109:420–430. doi: 10.1016/s0889-5406(96)70124-5. [DOI] [PubMed] [Google Scholar]
- 12.Hayakawa T, Horie K, Aida M, Kanaya H, Kobayashi T, Murata Y. The influence of surface conditions and silane agents on the bond strength of resin to dental porcelain. Dent Mater. 1992;8:238–240. doi: 10.1016/0109-5641(92)90092-q. [DOI] [PubMed] [Google Scholar]
- 13.Mehl A, Kremers L, Salzmann K, Hickel R. 3D volume-ablation rate and thermal side effects with the Er:YAG and Nd:YAG laser. Dent Mater. 1997;13:246–251. doi: 10.1016/S0109-5641(97)80036-X. [DOI] [PubMed] [Google Scholar]
- 14.Fried D, Featherstone JDB, Visuri SR, Seka WD, Walsh JT., Jr Caries inhibition potential of Er:YAG and Er:YSGG laser radiation. Lasers in Dentistry II. 1996. pp. 73–78.
- 15.Topcuoglu T, Oksayan R, Topcuoglu S, Coskun ME, Isman NE. Effect of Er:YAG laser pulse duration on shear bond strength of metal brackets bonded to a porcelain surface. Photomed Laser Surg. 2013;31:240–246. doi: 10.1089/pho.2012.3463. [DOI] [PubMed] [Google Scholar]
- 16.Meister J, Franzen R, Forner K, et al. Influence of the water content in dental enamel and dentin on ablation with erbium YAG and erbium YSGG lasers. J Biomed Opt. 2006;11:34030. doi: 10.1117/1.2204028. [DOI] [PubMed] [Google Scholar]
- 17.Gurney ML, Sharples SD, Phillips WB, Lee DJ. Using an Er,Cr:YSGG laser to remove lithium disilicate restorations: A pilot study. J Prosthet Dent. 2016;115:90–94. doi: 10.1016/j.prosdent.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Rechmann P, Buu NC, Rechmann BM, Finzen FC. Laser all-ceramic crown removal and pulpal temperature—a laboratory proof-of-principle study. Lasers Med Sci. 2015;30:2087–2093. doi: 10.1007/s10103-015-1738-1. [DOI] [PubMed] [Google Scholar]
- 19.Simsek H, Gurbuz T, Buyuk SK, Ozdemir Y. Evaluation of mineral content and photon interaction parameters of dental enamel after phosphoric acid and Er:YAG laser treatment. Photomed Laser Surg. 2017;35:270–277. doi: 10.1089/pho.2016.4190. [DOI] [PubMed] [Google Scholar]
- 20.Naik SA, Byakod G, Muglikar S. Laser therapy in the management of dentinal hypersensitivity: a critical review. Univ Res J Dent. 2012;2:107–113. [Google Scholar]
- 21.Dilsiz A, Canakci V, Ozdemir A, Kaya Y. Clinical evaluation of Nd:YAG and 685-nm diode laser therapy for desensitization of teeth with gingival recession. Photomed Laser Surg. 2009;27:843–848. doi: 10.1089/pho.2008.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson SM, Lien W, Lee DP, Dunn WJ. Confocal microscope analysis of depth of etch between self-limiting and traditional etchant systems. Angle Orthod. 2017;87:766–773. doi: 10.2319/120816-880.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


