Abstract
Objectives:
To determine the relative effects of Herbst appliance therapy in hypo- and hyperdivergent patients.
Materials and Methods:
The treated group included 45 growing Class II, division 1, patients treated with stainless steel crown Herbst appliances, followed by fixed edgewise appliances. The untreated control group consisted of 45 Class II, division 1, subjects, matched to the treated sample based on Angle classification, age, sex, and pretreatment mandibular plane angle (MPA). Subjects were categorized as hypo- or hyperdivergent based on their MPAs. Pre- and posttreatment cephalograms were traced and superimposed on cranial base and mandibular structures.
Results:
The primary effect of the Herbst in terms of maxillomandibular correction was in the maxilla. It significantly restricted maxillary growth, producing a “headgear effect.” Mandibular treatment changes depended on divergence. Hyperdivergent patients experienced a deleterious backward true mandibular rotation with Herbst treatment. Hypodivergent patients, as well as untreated hypo- and hyperdivergent controls, underwent forward true mandibular rotation. However, hypodivergent chins did not advance any more than expected for untreated hypodivergent Class II patients.
Conclusions:
Hypo- and hyperdivergent patients benefit from the Herbst's headgear effect. While the mandibular growth of hypodivergent patients overcomes the negative rotational effects, hyperdivergent patients undergo a deleterious backward mandibular rotation and increases in facial height.
Keywords: Hyperdivergent, Hypodivergent, Herbst therapy, Growing children
INTRODUCTION
Bilateral Class II dental malocclusion is a common orthodontic problem, occurring in approximately 15% of the US population.1 Of these, approximately 75% have Class II skeletal malocclusion.2,3 A consistent finding among subjects with Class II dental malocclusion is mandibular retrusion and facial convexity.4,5 To improve patients' facial convexity, significant anteroposterior (AP) positional changes of the chin would be needed. Chin advancement would create straighter profiles and improve facial esthetics.5–7
Common nonsurgical treatment methods to correct Class II skeletal malocclusions include headgear and functional appliances. Fixed functional appliances offer the advantage of not requiring patient compliance. The Herbst appliance was designed to alter the sagittal position of the mandible by continuously posturing it forward, with the goal of stimulating or redirecting condylar growth.8 The Herbst exerts a posterior force on the maxillary teeth and an anterior force on the mandibular teeth, which should produce proclination of the mandibular incisors and improve the first molar relationship. Other reported dental effects include retroclination of the maxillary incisors, distalization and intrusion of the maxillary molars, and backward rotation of the occlusal plane.
The skeletal effects produced with the Herbst remain controversial. Various studies have reported maxillary growth restriction, described as a “headgear effect,”5,9–14 A recent systematic review, which excluded most studies due to methodological limitations, found minimal maxillary skeletal and no significant headgear effects.8 It also disputed improvements in mandibular position and increases in mandibular length previously reported.4,9,10,15 While the amounts of condylar growth and fossa modeling that occur with the Herbst remain controversial,9,10,16–20 significant posterior redirection of condylar growth has been repeatedly demonstrated.10,16–18
The Herbst literature typically does not specify mandibular divergence.5,10,17,21,22 Of the studies that do, two focused exclusively on hyperdivergent patients,5,10 and the other three did not have well-matched controls.16,23,24 Divergence is important because true mandibular rotation plays the primary role in determining changes in chin position,5,25,26 condylar growth direction, and mandibular shape.26–28 It cannot be assumed that posteriorly directed condylar growth and associated increases in overall mandibular length produced with the functional appliances will improve AP chin position. In fact, posterior condylar growth is related to backward mandibular rotation, which displaces the chin down and back. As such, any possible gains in overall mandibular length produced with the Herbst could be negated by backward mandibular rotation, especially in hyperdivergent patients.
The purpose of the present study was to distinguish the effects of Herbst treatment in hypo- and hyperdivergent patients and compare those differences to well-matched, untreated controls.
MATERIALS AND METHODS
Sample Description
The sample included consecutive patients previously treated (ie, within the past 7 years) with the Herbst and fixed appliances by one private practice orthodontist who met the following criteria: (1) ANB angle greater than age- and sex-specific norms29; (2) Class II division 1 malocclusion with greater than or equal to half-step molar and canine relationships; (3) finished treatment with Class I molar and canine relationships, 2- to 3-mm overbite, and 1- to 2-mm overjet; and (4) between the ages of 11 and 14 years.
The treated group included 45 patients (23 boys, 22 girls) treated with stainless steel crown Herbst appliances. The pretreatment age (T1) was 12.6 ± 1.1 years, Herbst treatment continued until 14.4 ± 4.3 years, and the Herbst and fixed edgewise appliances were removed (T2) at 15.1 ± 1.2 years. All patients were treated using a standard cantilever Herbst appliance with full-coverage stainless steel crowns on the maxillary and mandibular first molars, telescopic cantilever arms from the mandibular first molars, and a 0.040-mm stainless steel lower lingual arch with occlusal rests on the mandibular first premolars.
The untreated control group was composed of children drawn from three school districts in Montreal representing the socioeconomic strata of the larger population.30 They consisted of 45 Class II division 1 subjects matched to the treated sample based on age, sex, and pretreatment mandibular plane angle (MPA).
The control sample was initially (T1) 12.4 ± 0.8 years of age and followed for 2.2 ± 0.5 years. This study was approved by the Texas A&M University Baylor College of Dentistry Institutional Review Board (IRB2015-0040).
Cephalometric Methods
Seven skeletal and dental landmarks were identified (Table 1) and digitized by one investigator using Dolphin Imaging Software. The linear measurements were adjusted to eliminate magnification; angular measurements were used to quantify the anteroposterior changes (SNA, SNB, ANB), mandibular plane angle (S-N/Go-Me), and skeletal convexity (NAPg).
Table 1.
Cephalometric Landmarks and Definitions
| Abbreviation |
Definition |
| S | Sella: the geometric center of the pituitary fossa |
| N | Nasion: the most anterior point on the frontonasal suture |
| Pg | Pogonion: the most anterior point on the chin |
| Me | Menton: the lowest point on the symphyseal shadow of the mandible |
| Go | Gonion: the point on the curvature of the angle of the mandible located by bisecting the angle formed by lines tangent to the posterior ramus and the inferior border of the mandible |
| A | A Point (subspinale): the most posterior midline point in the concavity between ANS and prosthion |
| B | B Point (supramentale): the most posterior midline point in the concavity between infradentale and pogonion |
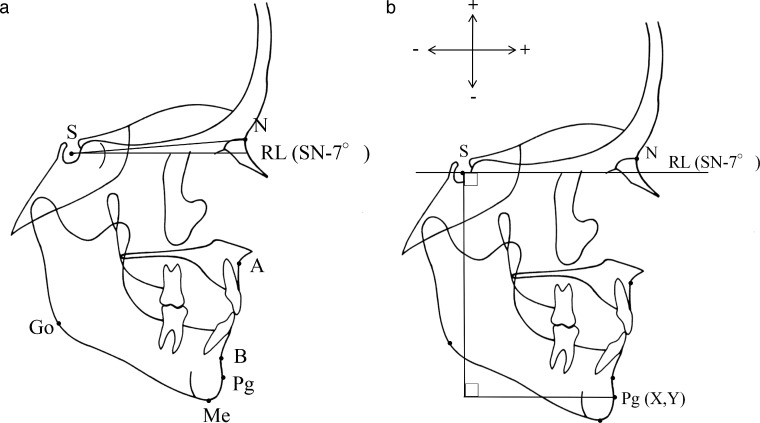
Cranial base superimpositions of the pre- and posttreatment cephalograms were performed using naturally stable structures.31 To quantify the horizontal and vertical changes of the chin, a horizontal reference line (RL) was constructed on the T1 tracing, registered on Sella, and oriented 7° below the SN plane (Figure 1a). AP and vertical changes in pogonion were measured parallel and perpendicular to RL, respectively (Figure 1b). Anterior and superior changes were recorded as positive.
Figure 1.
(a) Cephalometric landmarks and horizontal reference line (RL) oriented on the T1 SN-plane minus 7°, registering on T1 Sella. (b) Anteroposterior and vertical cephalometric positions measured parallel and perpendicular to RL.
True rotation was computed by adding the amount of apparent rotation to the amount of mandibular border modeling. Apparent rotation was measured as the change in the Go-Me after cranial base superimposition. Mandibular lower border modeling was measured based on the angular changes of the mandibular plane (Go-Me) after mandibular superimposition.31
Statistical Methods
Changes between T1 and T2 were annualized to represent changes per year. The distributions of all variables were normal based on the skewness and kurtosis statistics. Treatment effects were evaluated in relation to the subjects' divergence. They were grouped as hyper- or hypodivergent based on T1 MPAs <34° or ≥34°, respectively. The 34° division approximates average normative values of untreated subjects of similar age.29 The T1 MPAs of the hypo- and hyperdivergent groups were 30.2 ± 3.4° and 37.7 ± 2.5°, respectively. Independent samples t tests were used to evaluate between-group differences. Paired t tests were used to evaluate within-group differences.
RESULTS
There were no statistically significant pretreatment between-group differences in terms of age, gender, MPA, or sagittal jaw positions (Table 2). The SNA and SNB angles indicated relatively normal maxillary positions and mandibular retrusion, respectively.
Table 2.
Pretreatment Group Differences Between Herbst and Control Groups
| T1 (Pretreatment) | Herbst (n = 45) |
Controls (n = 45) |
Group Differences | ||
| 23 Boys, 22 Girls |
23 Boys, 22 Girls |
||||
| Measurement |
Mean |
SD |
Mean |
SD |
P Value |
| Age, y | 12.57 | 1.08 | 12.44 | 0.76 | .530 |
| SN-GoMe, ° | 33.70 | 6.04 | 34.82 | 2.89 | .270 |
| SNA, ° | 81.5 | 3.07 | 80.28 | 3.00 | .064 |
| SNB, ° | 75.81 | 2.78 | 76.65 | 2.39 | .127 |
The hypodivergent Herbst patients showed significant improvements in ANB due to decreases in the SNA angle and increases in the SNB angle (Table 3). The hypodivergent controls showed no significant changes in these three measurements. There were statistically significant (P < .05) group differences in the SNA and ANB angles. Changes of the SNB angle showed no significant group difference. Both the hypodivergent Herbst and hypodivergent controls showed statistically significant forward mandibular true rotation. Pogonion came forward and down slightly more in the Herbst group than in the control group, but the between-group difference was not statistically significant. There was a significant group difference in the change of the NAPg angle, which increased significantly (became less convex) in the Herbst patients but not in the controls.
Table 3.
Comparison of Annualized Changes (T1–T2) of Hypodivergent Herbst Patients and Hypodivergent Controlsa
| Measurement |
Hypodivergent |
Hypodivergent |
Group Differences | ||
| Herbst (n = 23) |
Controls (n = 18) |
||||
| Mean |
SD |
Mean |
SD |
P Value |
|
| SNA, °/y | −0.71 | 0.83 | 0.05 | 0.65 | .003 |
| SNB, °/y | 0.45 | 0.47 | 0.18 | 1.02 | .317 |
| ANB, °/y | −1.16 | 0.72 | −0.13 | 0.59 | <.001 |
| SN-GoMe, °/y | −0.29 | 0.71 | −0.25 | 0.79 | .870 |
| Rotation, °/y | −0.67 | 0.73 | −0.58 | 1.23 | .781 |
| Pg horizontal, mm/y | 1.16 | 0.96 | 0.78 | 1.32 | .298 |
| Pg vertical, mm/y | −2.90 | 1.84 | −2.55 | 1.06 | .442 |
| NAPg, °/y | 2.00 | 2.10 | 0.09 | 1.02 | .001 |
Bold indicates significant changes between T1 and T2 (P < .05).
The ANB angle of the hyperdivergent Herbst patients improved primarily because of decreases in the SNA angle; the control subjects showed no significant changes in either measurement (Table 4). The between-group difference in the ANB changes was statistically significant. While the SNB angle increased slightly in the Herbst patients and decreased slightly in the controls, neither the changes that occurred nor the between-group differences were statistically significant. There was a significant group difference in true rotation, with the hyperdivergent controls showing slight forward rotation and the hyperdivergent Herbst patients undergoing slight backward rotation. Neither group showed statistically significant chin advancements. NAPg increased significantly in hyperdivergent Herbst patients, whereas the controls showed no change, resulting in a significant between-group difference.
Table 4.
Comparison of Annualized Changes (T1–T2) of Hyperdivergent Herbst Patients and Hyperdivergent Controlsa
| Measurement Annualized Changes |
Hyperdivergent |
Hyperdivergent |
Group Differences | ||
| Herbst (n = 22) |
Controls (n = 27) |
||||
| Mean |
SD |
Mean |
SD |
P Value |
|
| SNA, °/y | −0.59 | 0.95 | −0.19 | 0.76 | .110 |
| SNB, °/y | 0.23 | 0.67 | −0.15 | 0.83 | .090 |
| ANB, °/y | −0.82 | 0.48 | −0.04 | 0.56 | <.001 |
| SN-GoMe, °/y | −0.06 | 0.79 | 0.07 | 1.19 | .671 |
| Rotation, °/y | 0.37 | 0.58 | −0.35 | 1.12 | .006 |
| Pg horizontal, mm/y | 0.00 | 1.30 | 0.29 | 1.25 | .427 |
| Pg vertical, mm/y | −3.32 | 1.80 | −2.55 | 0.99 | .081 |
| NAPg, °/y | 1.82 | 0.93 | 0.28 | 1.15 | <.001 |
Bold indicates significant changes between T1 and T2 (P < .05).
Comparison of the hypo- and hyperdivergent Herbst patients showed no statistically significant differences in the SNA, SNB, or ANB angles (Table 5). True rotation was significantly different, with the hypodivergent patients rotating forward and the hyperdivergent patients rotating back. The hypodivergent Herbst patients also underwent significant anterior displacement of pogonion, while the hyperdivergent patients did not, resulting in statistically significant between-group differences. The hyperdivergent Herbst patients also showed greater vertical displacement at pogonion than the hypodivergent Herbst patients, but the difference was not statistically significant. There also was no statistically significant group difference in NAPg; both groups exhibited increases.
Table 5.
Comparison of Annualized Changes (T1–T2) of Hypodivergent and Hyperdivergent Herbst Patientsa
| Measurement |
Hypodivergent |
Hyperdivergent |
Group Differences | ||
| Herbst (n = 23) |
Herbst (n = 22) |
||||
| Mean |
SD |
Mean |
SD |
P Value |
|
| SNA, °/y | −0.71 | 0.83 | −0.59 | 0.95 | .639 |
| SNB, °/y | 0.45 | 0.47 | 0.23 | 0.67 | .202 |
| ANB, °/y | −1.16 | 0.72 | −0.82 | 0.48 | .072 |
| SN-GoMe, °/y | −0.29 | 0.71 | −0.06 | 0.79 | .306 |
| Rotation, °/y | −0.67 | 0.73 | 0.37 | 0.58 | <.001 |
| Pg horizontal, mm/y | 1.16 | 0.96 | 0.00 | 1.30 | .001 |
| Pg vertical, mm/y | −2.90 | 1.84 | −3.32 | 1.80 | .443 |
| NAPg, °/y | 2.00 | 2.10 | 1.82 | 0.93 | .701 |
Bold indicates significant changes between T1 and T2 (P < .05). Positive increases in NAPg represent decreases in convexity.
DISCUSSION
The primary effect of the Herbst was in the maxilla. It restricted maxillary growth in both the hypo- and hyperdivergent patients, supporting the headgear effect reported previously.5,10 Both groups underwent significant reductions of the SNA angle during treatment. The Herbst appliance has previously been shown to restrict maxillary growth.5 The annualized reductions reported in the tables were substantial (1.8° and 1.5°) over the course of treatment. They were similar to reductions described for cervical-pull (−0.6 to −0.8°/y) and high-pull (−0.5 to −1.1°/y) headgear.32,33 This was a dentoalveolar treatment effect. Since the Herbst appliance is attached with rigid steel arms to the first molars, the same force that displaces the mandible down and forward is reciprocally exerted on the maxilla. Thus, a backward force is placed on the maxillary dentition with the Herbst, which may explain the headgear effect.
The Herbst had a positive, although limited, effect on the SNB angle in hypodivergent patients. The changes observed in the present study were consistent with the increases previously reported with Herbst treatment.5,10 In contrast, hyperdivergent patients did not show significant changes in the SNB angle, as previously demonstrated.5
In the present study, pogonion came forward the same amount in the treated and untreated Class II patients. Existing studies comparing patients undergoing Herbst treatment to untreated controls have reported either no significant differences in AP changes of pogonion or inferior displacements.5,10,17,22,23 Reports of chin projection with functional appliances have consistently failed to specify the patients' pretreatment divergence.9 If the patients were more hypodivergent than the controls, greater increases in chin projection would be expected. Without knowing the patients' growth tendencies, it cannot be determined whether changes in chin position are growth or treatment related.
Herbst treatment reduces skeletal convexity in both hypo- and hyperdivergent patients, but the reductions are not due to greater chin advancements. Profile improvements and decreases in facial convexity with Herbst treatment have been established.22,34 Those with adequate controls have found that the decreases in convexity were primarily due to maxillary changes, with no significant treatment effect on AP positional changes of the chin.5,10,17,22,23 Therefore, profile improvements and reductions of skeletal convexity with Herbst treatment are primarily due to the restriction of anterior maxillary growth.
The Herbst appliance has little or no effect on the mandibular plane angle. The present study showed that hypo- or hyperdivergent Herbst patients underwent the same changes as their respective controls. This is consistent with studies reporting either no changes or slight increases in the MPA with Herbst treatment.5,9,10 Despite the lack of change in the MPA, the present study showed significant true rotation, which was masked by modeling of the lower mandibular border. However, the true rotational effects of the Herbst are different in hypo- than in hyperdivergent patients. During normal growth, hypo-, normo-, and hyperdivergent untreated individuals generally exhibit forward true rotation.35 The difference is that untreated hypodivergent patients have significantly more forward rotation than untreated hyperdivergent patients.35 In contrast, the hyperdivergent Herbst patients in the present study exhibited significant backward rotation, while the hypodivergent Herbst patients rotated forward. This difference was clinically significant, amounting to 2.6° of true rotation and 2.9 mm of anterior chin projection over the 2.5 years of treatment. This suggests that hypodivergent patients are able to overcome the backward rotational effects of the Herbst appliance.
The mechanism producing these rotational effects may be inherent to the design of the Herbst. As the Herbst appliance postures the mandible downward and forward, the condyles slide down the articular eminence, which redirects condylar growth in a more posterior direction.10,16,18 The downward and forward posturing of the mandible with the Herbst appliance should restrict forward, or cause backward, mandibular rotation. One possible explanation for the rotational differences between hypo- and hyperdivergent patients may be the orofacial musculature. Since euryprosopic patients with powerful jaw musculature undergo more forward true rotation,36 they may be better able to overcome the negative rotational effects of Herbst treatment. Another possible explanation for the rotational differences may be morphological. Logically, advancing the mandible should produce less backward rotation in patients with flatter than with steeper occlusal planes, and hyperdivergent patients often have steeper occlusal planes than hypodivergent patients.
The rotational effects of the Herbst also clarify why increases in overall mandibular length reported with Herbst treatment15,37,38 do not necessarily contribute to the sagittal skeletal corrections. More posterior redirection of condylar growth has been reported to increase overall mandibular length in treated Class II patients, but it does not increase AP chin projection any more than in untreated controls.5,10,17 It does not increase chin projection because it can cause inferior displacement of the anterior mandible.10,21 In other words, increases in mandibular length often associated with Herbst treatment can be negated by rotation that displaces the chin down rather than forward.
CONCLUSIONS
In terms of maxillomandibular correction, the primary treatment effect of the Herbst appliance is dentoalveolar: a maxillary growth restriction or a headgear effect.
Hyperdivergent patients undergo undesirable backward true mandibular rotation during Herbst treatment, while hypodivergent patients undergo forward true mandibular rotation, similar to the rotation exhibited by hypodivergent controls.
Anterior chin displacement in Class II patients treated with the Herbst is similar to the anterior displacement seen in untreated Class II subjects.
ACKNOWLEDGEMENTS
We thank Dr. John Valant, Private Practice of Orthodontics, Cedar Hill, Texas, for allowing us to work with his patient records.
REFERENCES
- 1.Proffit WR, Fields HW, Jr, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthod Orthognath Surg. 1998;13:97–106. [PubMed] [Google Scholar]
- 2.Beresford JS. Tooth size and class distinction. Dent Pract Dent Rec. 1969;20:113–120. [PubMed] [Google Scholar]
- 3.Milacic M, Markovic M. A comparative occlusal and cephalometric study of dental and skeletal anteriorposterior relationships. Br J Orthod. 1983;10:53–54. doi: 10.1179/bjo.10.1.53. [DOI] [PubMed] [Google Scholar]
- 4.Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA., Jr Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop. 2006;129:599.e1–12. doi: 10.1016/j.ajodo.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 5.LaHaye MB, Buschang PH, Alexander RG, Boley JC. Orthodontic treatment changes of chin position in Class II Division 1 patients. Am J Orthod Dentofacial Orthop. 2006;130:732–741. doi: 10.1016/j.ajodo.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 6.Czarnecki ST, Nanda RS, Currier GF. Perceptions of a balanced facial profile. Am J Orthod Dentofacial Orthop. 1993;104:180–187. doi: 10.1016/S0889-5406(05)81008-X. [DOI] [PubMed] [Google Scholar]
- 7.Spyropoulos MN, Halazonetis DJ. Significance of the soft tissue profile on facial esthetics. Am J Orthod Dentofacial Orthop. 2001;119:464–471. doi: 10.1067/mod.2001.113656. [DOI] [PubMed] [Google Scholar]
- 8.Barnett GA, Higgins DW, Major PW, Flores-Mir C. Immediate skeletal and dentoalveolar effects of the crown- or banded type Herbst appliance on Class II division 1 malocclusion. Angle Orthod. 2008;78:361–369. doi: 10.2319/031107-123.1. [DOI] [PubMed] [Google Scholar]
- 9.Siara-Olds NJ, Pangrazio-Kulbersh V, Berger J, Bayirli B. Long-term dentoskeletal changes with the Bionator, Herbst, Twin Block, and MARA functional appliances. Angle Orthod. 2010;80:18–29. doi: 10.2319/020109-11.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Croft RS, Buschang PH, English JD, Meyer R. A cephalometric and tomographic evaluation of Herbst treatment in the mixed dentition. Am J Orthod Dentofacial Orthop. 1999;116:435–443. doi: 10.1016/s0889-5406(99)70230-1. [DOI] [PubMed] [Google Scholar]
- 11.LeCornu M, Cevidanes LH, Zhu H, Wu CD, Larson B, Nguyen T. Three-dimensional treatment outcomes in Class II patients treated with the Herbst appliance: a pilot study. Am J Orthod Dentofacial Orthop. 2013;144:818–830. doi: 10.1016/j.ajodo.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.VanLaecken R, Martin CA, Dischinger T, Razmus T, Ngan P. Treatment effects of the edgewise Herbst appliance: a cephalometric and tomographic investigation. Am J Orthod Dentofacial Orthop. 2006;130:582–593. doi: 10.1016/j.ajodo.2005.01.030. [DOI] [PubMed] [Google Scholar]
- 13.Valant JR, Sinclair PM. Treatment effects of the Herbst appliance. Am J Orthod Dentofacial Orthop. 1989;95:138–147. doi: 10.1016/0889-5406(89)90392-2. [DOI] [PubMed] [Google Scholar]
- 14.Wigal TG, Dischinger T, Martin C, Razmus T, Gunel E, Ngan P. Stability of Class II treatment with an edgewise crowned Herbst appliance in the early mixed dentition: skeletal and dental changes. Am J Orthod Dentofacial Orthop. 2011;140:210–223. doi: 10.1016/j.ajodo.2010.02.036. [DOI] [PubMed] [Google Scholar]
- 15.Franchi L, Baccetti T, McNamara JA., Jr Treatment and posttreatment effects of acrylic splint Herbst appliance therapy. Am J Orthod Dentofacial Orthop. 1999;115:429–438. doi: 10.1016/s0889-5406(99)70264-7. [DOI] [PubMed] [Google Scholar]
- 16.Pancherz H, Michailidou C. Temporomandibular joint growth changes in hyperdivergent and hypodivergent Herbst subjects: a long-term roentgenographic cephalometric study. Am J Orthod Dentofacial Orthop. 2004;126:153–161. doi: 10.1016/j.ajodo.2003.07.015. [DOI] [PubMed] [Google Scholar]
- 17.Serbesis-Tsarudis C, Pancherz H. “Effective” TMJ and chin position changes in Class II treatment. Angle Orthod. 2008;78:813–818. doi: 10.2319/082707-391.1. [DOI] [PubMed] [Google Scholar]
- 18.Araujo AM, Buschang PH, Melo AC. Adaptive condylar growth and mandibular remodelling changes with bionator therapy—an implant study. Eur J Orthod. 2004;26:515–522. doi: 10.1093/ejo/26.5.515. [DOI] [PubMed] [Google Scholar]
- 19.Ruf S, Baltromejus S, Pancherz H. Effective condylar growth and chin position changes in activator treatment: a cephalometric roentgenographic study. Angle Orthod. 2001;71:4–11. doi: 10.1043/0003-3219(2001)071<0004:ECGACP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Paulsen HU. Morphological changes of the TMJ condyles of 100 patients treated with the Herbst appliance in the period of puberty to adulthood: a long-term radiographic study. Eur J Orthod. 1997;19:657–668. doi: 10.1093/ejo/19.6.657. [DOI] [PubMed] [Google Scholar]
- 21.Pancherz H, Ruf S, Kohlhas P. “Effective condylar growth” and chin position changes in Herbst treatment: a cephalometric roentgenographic long-term study. Am J Orthod Dentofacial Orthop. 1998;114:437–446. doi: 10.1016/s0889-5406(98)70190-8. [DOI] [PubMed] [Google Scholar]
- 22.Flores-Mir C, Major MP, Major PW. Soft tissue changes with fixed functional appliances in Class II division 1. Angle Orthod. 2006;76:712–720. doi: 10.1043/0003-3219(2006)076[0712:STCWFF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Deen E, Woods MG. Effects of the Herbst appliance in growting orthodontic patients with different underlying vertical patterns. Aust Orthod J. 2015;31:59–68. [PubMed] [Google Scholar]
- 24.Ruf S, Pancherz H. The mechanism of Class II correction during Herbst therapy in relation to the vertical jaw base relationship: a cephalometric roentgenographic study. Angle Orthod. 1997;67:271–276. doi: 10.1043/0003-3219(1997)067<0271:TMOCIC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Bjork A, Skieller V. Facial development and tooth eruption: an implant study at the age of puberty. Am J Orthod. 1972;62:339–383. doi: 10.1016/s0002-9416(72)90277-1. [DOI] [PubMed] [Google Scholar]
- 26.Buschang PH, Jacob HB. Mandibular rotation revisited: what makes it so important? Semin Orthod. 2014;20:299–315. [Google Scholar]
- 27.Baumrind S, Ben-Bassat Y, Korn EL, Bravo LA, Curry S. Mandibular remodeling measured on cephalograms. 1. Osseous changes relative to superimposition on metallic implants. Am J Orthod Dentofacial Orthop. 1992;102:134–142. doi: 10.1016/0889-5406(92)70025-6. [DOI] [PubMed] [Google Scholar]
- 28.Buschang PH, Gandini LG., Junior Mandibular skeletal growth and modelling between 10 and 15 years of age. Eur J Orthod. 2002;24:69–79. doi: 10.1093/ejo/24.1.69. [DOI] [PubMed] [Google Scholar]
- 29.Riolo ML. An Atlas of Craniofacial Growth: Cephalometric Standards from the University school Growth Study, the University of Michigan. Ann Arbor, MI: Center for Human Growth and Development, University of Michigan;; 1974. [Google Scholar]
- 30.Demirjian A, Dubuc MB, Jenicek M. Comparative study of growth in Canadian children of French origin in Montreal [in French] Can J Public Health. 1971;62:111–119. [PubMed] [Google Scholar]
- 31.Bjork A, Skieller V. Normal and abnormal growth of the mandible: a synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;5:1–46. doi: 10.1093/ejo/5.1.1. [DOI] [PubMed] [Google Scholar]
- 32.Jacob HB, Buschang PH, dos Santos-Pinto A. Class II malocclusion treatment using high-pull headgear with a splint: a systematic review. Dental Press J Orthod. 2013;18:21.e21–27. doi: 10.1590/s2176-94512013000200009. [DOI] [PubMed] [Google Scholar]
- 33.Firouz M, Zernik J, Nanda R. Dental and orthopedic effects of high-pull headgear in treatment of Class II, division 1 malocclusion. Am J Orthod Dentofacial Orthop. 1992;102:197–205. doi: 10.1016/S0889-5406(05)81053-4. [DOI] [PubMed] [Google Scholar]
- 34.Ruf S, Pancherz H. Orthognathic surgery and dentofacial orthopedics in adult Class II Division 1 treatment: mandibular sagittal split osteotomy versus Herbst appliance. Am J Orthod Dentofacial Orthop. 2004;126:140–152. doi: 10.1016/j.ajodo.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 35.Chung CH, Wong WW. Craniofacial growth in untreated skeletal Class II subjects: a longitudinal study. Am J Orthod Dentofacial Orthop. 2002;122:619–626. doi: 10.1067/mod.2002.129195. [DOI] [PubMed] [Google Scholar]
- 36.Kiliaridis S, Kalebo P. Masseter muscle thickness measured by ultrasonography and its relation to facial morphology. J Dent Res. 1991;70:1262–1265. doi: 10.1177/00220345910700090601. [DOI] [PubMed] [Google Scholar]
- 37.Perinetti G, Primozic J, Furlani G, Franchi L, Contardo L. Treatment effects of fixed functional appliances alone or in combination with multibracket appliances: a systematic review and meta-analysis. Angle Orthod. 2015;85:480–492. doi: 10.2319/102813-790.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baysal A, Uysal T. Dentoskeletal effects of Twin Block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur J Orthod. 2014;36:164–172. doi: 10.1093/ejo/cjt013. [DOI] [PubMed] [Google Scholar]