Abstract
Purpose
Medication has been a central part of treatment for severe mental disorders in Western medicine since the 1950s. In 2015, Norwegian Health Authorities decided that Norwegian health regions must have treatment units devoted to medication-free mental health treatment to enhance service users’ freedom of choice. The need for these units has been controversial. The aim of this study was to examine why service users choose medication-free services. This article examines what purpose these units serve in terms of the users’ reasons for choosing this service, what is important for them to receive during the treatment, and what factors lay behind their concerns in terms of medication-related views and experiences.
Methods
Questionnaires were answered by 46 participants and 5 participants were interviewed in a mixed-method design integrated with a concurrent triangulation strategy applying thematic analysis and descriptive statistics.
Results
Negative effects of medications and unavailable alternatives to medication in ordinary health care were important reasons for wanting medication-free treatment. Medication use may conflict with personal values, attitudes, and beliefs.
Conclusion
This study broadens the understanding of why the demand for separate medication-free units has arisen. The findings may contribute to making medication-free treatment an option in mental health care in general. To this end, clinicians are advised to communicate all treatment alternatives to service users and to be mindful of the effect of power imbalances in their interactions with them.
Keywords: mental health care, medication-free, choice, psychotropics
Introduction
Medication has been a central part of treatment for severe mental disorders in Western medicine since the 1950s.1 However, medication adherence has been a challenge. A recent review found 49% of service users with severe psychiatric disorders were not adherent to their psychotropic medication.2 Nonadherence can be related to interactional factors between service users and health care professionals2–8 or their families and friends,5,6,8 side effects/negative effects of medication,2,3,5–8 and service users’ beliefs, attitudes, and perceptions.2,4–8 There is also evidence of some correlations with service user characteristics like “lack of insight”,2,4–7 comorbidity,2,6 severity of pathology,5,8 positive symptoms and grandiosity,5 lower quality of life/wellbeing,8 psychological reactance and internal locus of control.8 Sociodemographic factors show mixed results,2,5,6,8 although some find correlations on age,2,6 unmarried status,6 male gender,6 low education level,2,6 and unemployment.2 Service user accounts have shown experiences of one-way relationships wherein service users do not experience use of medication as their own choice, which leads to termination of medication.3 This corresponds to findings showing that service users can experience the boundary between voluntary and coerced medication as blurred.9,10 Poor service user involvement is also reflected in a study of mental health professionals’ experiences with shared decision-making with service users with psychotic disorders, concluding that shared decision-making is practiced to only a limited extent with this group.11 Involuntary medication has been found to be a particularly problematic form of coercion in service users’ experience.10
The majority of admitted service users in mental health care are treated with medication. A report indicates 88% are treated with medication, of whom 13% are medicated against their will. Additionally, 1% indicate they want medication but are not receiving it.12 Although there have been treatment programs in more recent times with less use of medication,13,14 a nationwide governmental instruction to provide specialist services devoted to medication-free treatment, such as that which was introduced in Norway in 2015, is unprecedented.
In 2009 a governmental task force suggested medication-free treatment as one of several measures to reduce coercion,15 and in 2012 it was incorporated in a national strategy to reduce coercion.16 In 2015, each of the four health regions was instructed to provide dedicated medication-free services.17 The first unit opened in 2015,18 and others followed from 2017 onward.
The Norwegian Ministry of Health and Care did not specify what was meant by a medication-free treatment unit other than what can be inferred from descriptions of its purpose. The Ministry simply refers to the aim that service users in mental health care shall, as far as clinically justifiable, have the opportunity to choose between different treatment measures, including medication-free treatment.17 A coalition of user organizations lobbying for medication-free treatment describes it as freedom from coercion, pressure, or persuasion regarding medication.19 Medication-free treatment is further interpreted in local protocols of the health regions, where it is made clear that service users in the “medication-free” units can use psychotropics if they want to.20,21 Medication-free treatment must be deemed clinically justifiable,17 which excludes service users formally subjected to involuntary medication.
In this article, “medication-free treatment” (MFT) refers to services developed as a result of the aforementioned governmental decision and which seem to be interpreted by both user organizations and health trusts to mean that the service is free from medication pressure and coercion, rather than free from all psychotropic medication.
As of 2018, MFT was offered in 25 locations in Norway.22 The services are not uniform, but the most common characteristics are the following: inpatient, open wards, prioritizing individuals with severe mental disorders, and influenced by a recovery tradition.22,23
Some initial studies and audits have been conducted of these services. Clinician accounts of service users’ reasons for wanting MFT include side effects, fear of long-term harm, not feeling ill, not feeling need for antipsychotics, stigma, lack of effect, delusions, and outside pressure or recommendations.24 Service user accounts include wanting a service with less focus on medication and diagnoses, learning to cope without medication, and escaping negative side effects of medication.25 Health care professionals’ attitudes to MFT seem to vary. A qualitative study shows some are critical, considering MFT as lacking scientific evidence, that that it reflects the wish of a minority of service users, or that MFT might not be necessary because service users already are perceived to have a crucial involvement regarding medication.26 These arguments disputing the need for dedicated MFT units are also found in the public debate.27,28 A quantitative investigation shows health care professionals are positive overall (68%, rising to 90% after a conference on the subject).24 However, clinicians report that for a substantial proportion of their psychosis service users (22%), MFT would not be clinically justifiable.24 Service users report medication discussions as sometimes challenging in general mental health care.9 There are indications that about half the population in inpatient units would be interested in an MFT alternative.29 Service users with psychosis in MFT report that having choices about treatment is important.30
Because the need for MFT units is controversial, the MFT mandate does not require service users to go off medication, and MFT wards may have several other features that might be attractive to service users, it is important to examine whether medication-issues are important for the users. This will illuminate whether the units are utilized in line with their intended purpose, as well as deepen the understanding of this eventual purpose. The reasons service users in MFT treatment have for wanting MFT have not yet been examined in detail. This is the topic of the present study, and we were particularly interested in exploring their medication-related views, concerns, and experiences.
Method
Setting
The context in this study was an MFT unit that is part of a general hospital in the metropolitan area of Oslo. The hospital has a catchment population of 500,000, containing both urban and rural communities. This medication-free unit is an inpatient unit for voluntary admissions within the recovery tradition prioritizing severe mental illness; hence, it is fairly representative of MFT services in Norway.
The target group for this MFT unit is described as service users over age 18 with severe mental disorders that are traditionally treated with medication but who want MFT. Service users with psychosis and bipolar disorders are prioritized. The level of care is intermediate, targeting a population with low functioning or prior treatment resistance (i.e. not having responded to several known treatments, including drug treatment). Service users with active addictions, suicidal behavior or aggressive/violent behavior are excluded. Service users must be willing to participate in the treatment program, and motivation and effort are highlighted on the web pages.31
The treatment program has an overarching umbrella of recovery including the program illness management and recovery (IMR).32 The recovery tradition has been characterized using the acronym CHIME.23 This entails a focus on Connectedness, Hope, Identity, Meaning of life, and Empowerment. The treatment program further incorporates focus on affect, feedback, and communication from the traditions of the affect consciousness model,33 a feedback informed framework,34 open dialogue,35 and techniques from basal exposure therapy.36
The treatment program lasts eight weeks and there are seven service users on the ward at any given time. It is organized as a “5-days-unit” where service users go home for the weekends.
Design
This article is part of a larger study, described in full at ClinicalTrials.gov (Identifier NCT03499080). Because the subject matter is a new and relatively unexplored type of treatment service where opinions and perceptions are diverse, we chose an exploratory design to address our research agenda.
The design consists of mixed methods, containing qualitative thematic analyses of interviews and open-ended questionnaire responses, as well as quantitative descriptive analyses of questionnaire data from service users and their clinicians on the ward. Quantitative and qualitative data collection and analysis were done in parallel and were integrated in the analysis using a concurrent triangulation strategy.37
The purpose of using mixed methods was to increase validity and completeness by comparing results from different methods, thereby transcending the shortcomings of each. The qualitative materials add depth and an opportunity for the participants to express themselves in their own words, thereby allowing for the discovery of themes not previously considered. The quantitative material indicates how representative the themes are within our context.
Inclusion Criteria
Eligible service users were those on planned stay in the recruitment period who were deemed capable of being interviewed and/or filling out forms in Norwegian and who consented to participation. The wards also include emergency stays and user-controlled stays that are shorter and do not follow the ordinary treatment program.
Sampling Procedures
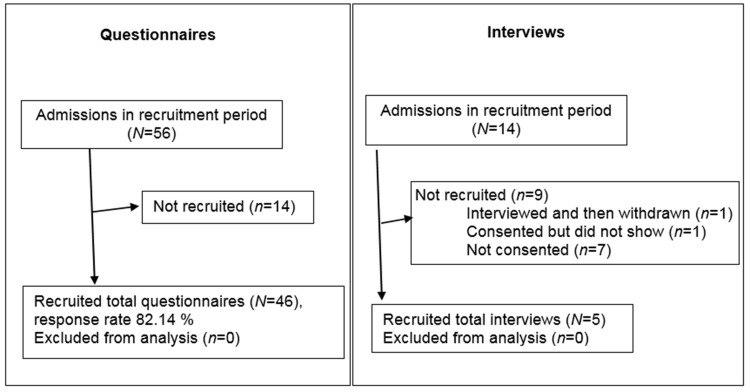
The recruitment period for the questionnaire study was 22.5 months, from May 2018 to April 2020, whereas for interviews it was three months, from January to March 2018. Service user flow can be seen in Figure 1. Therapists had standardized routines for informing service users about the project and handed out information and consent forms at the beginning of each admission. Questionnaires used in this study were to be completed within the first week of their stay.
Figure 1.
Participant flow.
Data Collection
Questionnaire data was collected by having service users and their clinicians fill out questionnaires at specific intervals during the treatment stay.
ARM performed semi-structured interviews face-to-face with participants. The interviews lasted 50–60 minutes and were audio-recorded. Service users were interviewed on the ward toward the end of their stay.
Measurements
Translated versions of questionnaires and interview guide can be found in Supplemental Material B–D.
Reasons for Wanting MFT
Because service users might be admitted to hospital for various reasons, service users in MFT were asked whether they were referred specifically for MFT. Respondents were asked who had wanted the referral to MFT with multiple-choice answers (self, next of kin, health professional, others). Those who replied that they had wanted it themselves were asked to indicate why it was important to them based on the following multiple-choice alternatives: 1= Having felt pressure to use medication, 2= Experienced lack of alternatives to medication, 3 = Use of medication does not fit my understanding of my problems, 4 =Negative experiences with effects and/or side effects of medication and 5= Other (open-ended). The first three alternatives were thought to illuminate possible reasons for the need for dedicated units, whereas the fourth is more about the medication itself.
Being Respected for the Wish Not to Use Medication
To assess the degree to which participants thought they were respected for their medication preferences in the treatment received in the 6-month period prior to the present stay, they were asked to indicate on a 5-point Likert scale their agreement with the statement “I have been respected for my wish not to use medication.” This question was taken from the Medsupport instrument.38
Sample Characteristics
Participants provided information on age, gender, and current use of psychotropic medication. Clinicians completed main diagnoses, current use of psychotropics, and details of type of psychotropics. To calculate response rate and assess how representative our sample was among all those using the MFT-unit in the study period, we accessed anonymous statistics from the electronic service user journals for all service users in the MFT unit during the study. Information included age, gender, and diagnoses for all planned regular stays at the unit during the recruitment period, excluding readmissions within 30 days.
Interview Guide
An interview guide was developed in collaboration between KS, ARM, MSH, and KSH, and was based on the literature and a previous study of medication-free services.39 Topics included users’ understanding of and expectations regarding MFT and attitudes toward this treatment approach, as well as whether, and why, MFT was important for them, how the treatment compared to other treatment experiences, and whether they experienced shared decision making.
Analyses
Numerical questionnaire data were analyzed using SPSS (version 26) and described by frequencies and percentages or means and standard deviations (SD) as appropriate. Valid percentage was reported if not otherwise specified. Psychotropic drugs were grouped according to the Norwegian medication handbook (Norsk legemiddelhåndbok). The answers to open-ended questions were analyzed thematically with the same strategy as for the interviews (see below). The program NVivo was used. In the integrated results only medication-related themes were compared, as these were the focus in the interviews.
The interview data were subject to thematic analysis40 This is a flexible stepwise qualitative analysis method wherein the data, after familiarizing, are first coded according to the most basic meaning units of interest and then analyzed into broader themes.40 Audio files were transcribed verbatim by ARM and coded and sorted with the program NVivo by KS. Initially, KS reviewed the transcripts doing predominantly inductive coding of the interviews. The coding was grouped according to the research questions in the total study.41 Our initial focus was service users’ reasons for coming to the MFT unit, their concerns on arrival, and experiences that may illuminate these concerns. These codes were grouped into themes. A theme was a concern explicitly expressed by at least one participant. In line with the concurrent triangulation strategy, findings from both quantitative and qualitative methods guided the analysis in a hermeneutic fashion. Initial findings were that the MFT concept was not sharply delineated for participants, and the quantitative finding that the majority reported medication-related reasons led us to conclude that medication-related reasons were important, but it was not possible to clearly separate them from other reasons in the interviews. We therefore narrowed the focus to concerns and experiences explicitly related to psychotropic medication to shed light on reasons that could be attributed to the official mandate of MFT units.
KS coded and grouped the data and drafted the findings. KSH and JR reviewed the transcript material constituting the final themes. KSH, ARM, MSH, and JR read transcripts and gave input into the analysis and interpretation.
Integration of Results
The integration was done by a between-method triangulation,42,43 adjusted to the present study. Herein we investigated convergence, divergence, and complementarity in the results, leading to meta-themes across all results. Results were compared regarding the meaning of themes, whereas prominence was assessed only in the quantitative material.
Ethics
The study was conducted in accordance with the Declaration of Helsinki and approved by the Regional Committee for Ethics in Research (2017/1056/REK sør-øst B.), as well as by the Privacy Ombudsman at Akershus University Hospital (17–134). Participants gave written, informed consent prior to participation. All participant names are pseudonyms, and the consent includes publication of anonymous results.
Results
Participant Flow
As shown in Figure 1, the questionnaire response rate was more than 80%, whereas about half of the potential subjects declined to participate in interviews. According to the therapists in informal discussions, the reasons for declining interviews were that there was much going on and it felt overwhelming for the service users to take part in research as well at this point.
Participants
Questionnaire Sample
In the questionnaire group, 68.57% were women and the rest were men. The majority (71.74% reported by service users, 73.91% reported by clinicians) used psychotropics at baseline. The most common psychotropic group was antidepressants (31.25% of prescribed medications), antipsychotics (27.50%), and anxiolytics/hypnotics (22.50%). The mean age was 37.85 (SD 12.94). Only one participant reported having an outservice user commitment order. Diagnoses were diverse, with the most common ones being psychosis, bipolar disorder, non-bipolar affective disorder, and personality disorder (14.89% each). Compared to all those using the MFT unit in the study period, our research sample seems reasonably representative with respect to age, gender, and diagnoses (Supplemental Material A).
Interview Sample
As can be seen in Figure 1, five interviews were included in the analysis; two of these participants were men and three were women. In the article, female pseudonyms were used for all participants to protect anonymity. Ages ranged from 25 to 50 years and the sample included people born in Norway and elsewhere. One of the participants had never used psychotropic medication. The other four had tried to withdraw from such medication, either during the current stay or earlier. Four of the service users were completely off medication at the time of interview. Collectively, participants discussed experience with SSRIs, SNRIs, anxiolytics, hypnotics, antipsychotics, and beta-blockers. Four of the five service users had previously been admitted to an open psychiatric ward. Details of diagnoses and other demographic variables were not recorded to protect anonymity. In three of the five cases (Anita, Bella, and Diana) MFT was described as someone else’s suggestion, while two (Cecilie and Elise) described it as their own initiative. One participant, Anita, said the medication-free mandate was unimportant to her. All except Anita stated that they wanted MFT and had concerns explicitly about quitting or not using medication.
Questionnaire Results
Table 1 gives an overview of findings from the questionnaire about reasons for wanting MFT. We have focused on participants indicating that MFT was their own wish.
Table 1.
Questionnaire About Reasons for Wanting MFT
| All | Participants Wanting MFT (n=38) | |||||||
|---|---|---|---|---|---|---|---|---|
| N | % of 46 | n | % of 38 | |||||
| Wanted MFT total | 38 | 82.61 | 38 | 100 | ||||
| Want MFT for medication-related reason, incl. free text | 36 | 78.26 | 36 | 94.74 | ||||
| Not own wish | 5 | 10.87 | ||||||
| Not answered question of who wanted MFT | 3 | 6.52 | ||||||
| Total | 46 | 100 | Subgroups of Questions % Chosen Either of These | |||||
| Reasons for wanting MFT | Negative effects/side effects | 26 | 56.52 | 25 | 65.79 | 89.47 | ||
| Experienced pressure about using medication | 20 | 43.48 | 19 | 50.00 | 63.16 | 78.95 | ||
| Lack of alternatives to medication | 16 | 34.78 | 16 | 42.11 | ||||
| Conflicts with my understanding of my problem | 16 | 34.78 | 13 | 34.21 | ||||
| Other reason | 9 | 19.57 | 8 | 21.05 | ||||
|
Free text (n 17): - Negative effects of medication - Having experienced pressure or coercion - Understanding of problem - Worries about medication - Belief in a better therapeutic process without medication - Finding other ways to cope than medication - Help with withdrawal - Other aspects of the treatment |
||||||||
Notes: Bold box contains the results that are our main focus: from patients indicating MFT was their own wish.
Negative effects of medication was the most common alternative chosen as reason for wanting MFT. Around 90% listed at least one medication-related reason. Of the total 46 participants, including those who had not initiated MFT themselves, 78.26% wanted MFT and stated medication-related reasons.
Experience with being respected for not wanting to use medication in the last six months prior to this treatment stay is shown in Table 2. As shown, experiences were varied. Of those who found the question applicable about half agreed with the statement that they felt respected in their decision to not use medications in the 6-month period prior to the MFT treatment; 15.63% disagreed.
Table 2.
Answers to the Question: “I Have Been Respected for My Wish Not to Use Medication” in the 6 Months Prior to Admittance
| Response Alternatives | n | Valid % | % of Applicable | ||
|---|---|---|---|---|---|
| Strongly disagree | 2 | 4,44 | 11,11 | 6,25 | 15,63 |
| Disagree | 3 | 6,67 | 9,38 | ||
| Neutral | 10 | 22,22 | 22,22 | 31,25 | 31,25 |
| Agree | 10 | 22,22 | 37,78 | 31,25 | 53,13 |
| Strongly agree | 7 | 15,56 | 21,88 | ||
| The question is applicable | 32 | 71,11 | |||
| The question does not apply | 13 | 28,89 | |||
| Total valid | 45 | 100,00 | |||
| Missing | 1 | ||||
| Total | 46 | ||||
Notes: Orange shade: disagree and strongly disagree, green shade: neutral, grey shade: agree and strongly agree.
Interview Results
Findings Affecting the Analysis: The MFT-Concept Has Unclear Borders
Although participants stated that they wanted MFT and had concerns explicitly about stopping or not commencing medication, there was not necessarily a clear distinction for them between MFT and other factors. Cecilie put it like this when asked if MFT was important to her:
Well …, it was … it was partly that it was medication-free, that was what … I did not think … I had not sort of separated IMR and medication-free treatment. I saw it as the same.
The MFT mandate seemed abstract and some struggled to answer questions about how they understood MFT and were reticent about what difference it made. However, the same participants also expressed both wanting MFT and having clear concerns regarding medication. For example, Diana said she had “no idea” whether she thought shared decision-making would be handled as well on a ward that was not MFT but expressed feeling safer from being involuntarily medicated in MFT. This finding, together with the quantitative finding that 94.74% of those wanting MFT reported medication-related reasons, led to us focusing on service users’ explicit medication-related reasons for wanting this treatment. Other themes were also present, but it was hard to determine whether they were regarding treatment in general, other aspects of the ward, or were implicitly related to MFT.
Interview Themes Illuminating Reasons for Wanting MFT
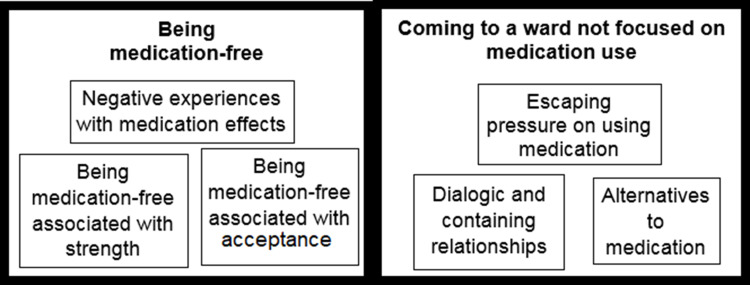
As shown in Figure 2, we divided themes from the interview data into two broad areas: being medication-free and coming to a ward not focused on medication use, both with subthemes as described below.
Figure 2.
Interview themes illuminating reasons for wanting MFT.
Being Medication-Free
Being medication-free was expressed as a key motivation for being at the MFT unit in the sense of wanting to withdraw medication during the stay, consolidate previous withdrawal, or simply avoid starting medication. This was connected to the subthemes (i) negative experience with medication effects, (ii) an association between being medication-free and being strong, and (iii) acceptance of themselves without medication.
All the informants reported some negative experience with medication effects, mainly psychotropic medication. There were, however, reports of benefits of sleep medication. Experiences included emotional flattening, feeling “zombielike” or “less human,” feeling empty and tired, having suicidal thoughts, and developing abuse of the medicine.
Along with negative experiences with medication, there were also expressions of an association between being medication-free and being strong. Elise put it like this “ … for me personally, it has been very important to avoid medication. Because I wanted to go the hard route.” Diana described using a “happy pill” as defeat. Anita expressed a view that the choice of MFT depends on, among other things, “how strong you are.”
Some participants explained the wish for MFT as wanting to achieve acceptance of themselves without medication, as Elise expressed it, without “chemical modifications.” This implies a notion of the unmedicated self as the real self. Elise said, in connection with being cautious about medication, that “I want to live as the person I am, for better or worse.” Diana described how the medicines promoted and legitimized her defense against emotions that made her feel worse:
My challenges on the outside have been to put a lid on all emotions. So all my emotions have sort of been fused …. And that has given me anxiety. And I was afraid that if I was put on medication again, that it would just like … that it would be okay to continue covering up my emotions. And repressing emotions sort of was okay because the medications were on my side regarding that. So I needed to be challenged on experiencing my emotions and tackle things. Experiencing standing up for myself, to feel that I exist and to have a voice.
Coming to a Ward Not Focused on Using Medication
Coming to a ward with another focus was expressed as important in the sense that other wards lacked alternatives to medication, in the MFT unit the participants could escape medication pressure, and there were expectations of relationships with health care professionals characterized more by dialogue and containment when there was no medication focus. Diana said it was important to her that the ward was not focused on medication use. Similarly, Elise said that she would have been skeptical if the ward was not medication-free, and Cecilie viewed the MFT ward as an interesting approach for someone like her who did not want to use medication.
Searching for alternatives to medication was expressed by, for instance, getting tools to tackle challenges that they have not gotten elsewhere. For example, when Elise was asked whether she previously had wanted such a service, she said:
That I have thought those times I have been on [ward x] because, as I said, on [ward x] it is more for stabilization. Ehh … that will do for a while, but when you don’t get the tools you get here … then it becomes a little hopeless. So to speak.
Similarly, Cecilie described her motivation like this:
I came here to learn a tool for managing my life further on. I had no need to come here and be “in storage”. (…) if I had had that need, I would not come here, I think.
Cecilie had experienced a strong focus on medication in other services and sometimes that had been the only help she had been offered. When asked if she previously had thought about wanting treatment with less focus on medication, she responded:
Not really. It has never really, like, been heard about or talked about. There has never been a focus on that for me. They’ve had two, or three really, diagnoses that they’ve touched on but that are now removed and that really were, the only treatment I have received for those has been medication.
Cecilie seemed to search for an explicit service focus on the opportunity to become medication-free. She was surprised that medication was such a prevalent topic in the IMR handouts at the MFT unit. When asked about how the service could be improved, she said:
Perhaps it could have been more in focus so people had been a little more … (…) aware that it is possible to do it without medication. Interviewer: So more focus on what medications do to you and how it is possible to manage without? Cecilie: Yes. And focus on that it is at least possible to try without, at least give it a chance. And there is not much focus on that, directly, in the [IMR] modules we’ve had until now.
Escaping medication pressure was an issue. Diana and Elise directly expressed this was a reason for wanting MFT. Overall there were mixed experiences with discussing medication practices in other treatment settings. Diana expressed feeling safer when being admitted at the MFT unit because the possibility of coerced medication was absent:
… this was not a place where I needed to stress about them wanting to medicate me involuntarily. And that made me calmer when I was admitted, because I understood they worked in another way here.
Diana discussed her experiences of medication pressure when she had been in a vulnerable situation, and her arguments against the professionals had fallen short:
There was a very strong pressure. I was very insecure about myself, was very low in confidence … It is hard to oppose medication when you sort of feel your arguments don’t float.
She also said that her previous psychiatrist had been angry with her for being determined about not wanting medication. Elise said her wish not to use medication had been respected but attributed this in large part to her being strong and knowledgeable about her rights.
Elise: The experience I have had on (ward x) among other things it was more like … how shall I put it … they did not pressure, but it was more like, you felt this was what they wanted all along, and … but then you are informed. And you know they can just forget about that legal option [ie, the use of the Mental Health Act], at least regarding medication.
Cecilie similarly described that her attempts at stopping her medication had been accepted in previous treatment because she was so determined: ” … I do not think they really wanted to take the fight.” While not agreeing she was directly supported, she was nevertheless guided in stopping her medication and she expressed overall satisfaction with the help she received. When on medication, on the other hand, she experienced a lack of follow up regarding medication effects, dosage, continued need for medication, and the effect on her blood pressure. She felt that this lack of follow up contributed to her starting to misuse the medication.
There were descriptions of recovery notions of dialogic and containing relationships with health care professionals that were seen to be at odds with focus on medication. Elise said that she had no faith that medication would solve her problems and that she believed more in talking therapies. She said she would have been skeptical if the ward was not an MFT unit, as she believed “chemical adjustment should not be necessary.” She made a connection between medication and focus on clinical assessment, rejecting both:
Elise: I do see now that by simply making a diagnosis many [clinicians] have moved on from those 90 or several hundred questions that you have to go through over 4 hours or whatever it is. And I find that positive because many years ago I listened to a family therapist called Jesper Juul [A public figure in Scandinavia], and he was very opposed to assessments. And he said something to me that has stuck with me since that lecture, and that is that all psychologists must learn to talk to people.
Interviewer: Yes, that is very important.
Elise: Yes, it has stuck with me all the way. And that is why I have been so adamant in keeping away from medication. And therefore I am very positive about what I see now, which is about to change.
It seems that reliance on medication was at odds with her understanding of recovery, and that she expected more room for talking therapy as opposed to assessment and medication on the MFT unit. Similarly, Diana associated “not being laid flat” with medication as being given room for expressing feelings. Diana expressed that it was important for her to
Diana: … meet a therapist who actually accepted that I wanted to get in touch with my emotions.
Interviewer: Yes, have you previously experienced that that was not accepted?
Diana: I have. I have many experiences, bad experiences in health care. And that too … it was important to me not having to use medication, it was important for me to have a space where I could develop a little more contact with myself and connect the brain a little to the body and understand what goes in with me when emotions take over.
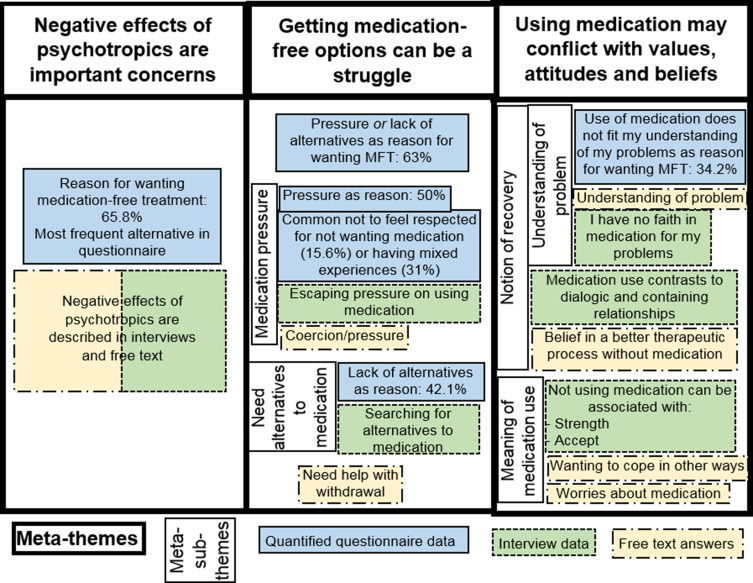
Integrated Results
We found no direct dissonance between the findings from the questionnaires and the interviews. We found widespread agreement and some complementary findings leading to three meta-themes, as shown in Figure 3. Negative effects of medications was the most prevalent reason chosen in the questionnaire for wanting MFT, and this theme was also present in open-ended questions and interviews, strengthening this as an important issue for participants. Experiences with pressure, lack of alternatives, not being respected for not wanting medication, and needing help with withdrawal can be reasonably subsumed under the heading that getting medication-free alternatives can be a struggle. Finally, values, attitudes, and beliefs conflicting with using medication were expressed in all the data sources. The questionnaire results showed a large minority (34.21%) indicated that reliance on medication does not fit their understanding of their problem, a theme also present in the interviews and open-ended questions. The qualitative results indicated a broader theme of notions of recovery in conflict with medication use (dialogic and containing relationships with health care providers, belief in a better therapeutic process without medication). In addition, qualitative findings indicated the meaning attached to not using medication (strength, acceptance, wanting to cope in other ways, worries) may be at odds with using medication.
Figure 3.
Integrated results.
Discussion
A majority of participants reported that MFT was their own desire and stated reasons that were related to the intended purpose of MFT (78.26%). Important reasons seem to be the negative effects of medication, struggle with getting alternatives in ordinary health care, and medication use conflicting with values, attitudes, and beliefs. Together with previous findings,29 our study demonstrates the presence of a desire for MFT as an alternative to mainstream treatment services. This contradicts the views of MFT as representing the wish of only a minority of service users.26 It also contradicts the view that service users already have a crucial impact on choice regarding medication.26
Side effects or negative effects of medication were an important issue for our participants, which is in line with previous research.2,3,5–9,24 It was the most frequently chosen reason for wanting MFT both in our questionnaire (65.79%) and in Øvernes24 interviews with clinicians (39%).
Our study shows that getting medication-free options can be a struggle in mainstream mental health care and that medication use may conflict with values, attitudes, and beliefs. This may explain why the wish for dedicated units for MFT has arisen. Service users search not just to avoid medication but for services in which medication plays a less central role. Pressure to use medication and lack of alternatives are concrete obstacles for service users not wanting medication. In addition, a shared understanding of the nature of their problem, the notion of the recovery process, and the meaning of using medication can be important elements of a therapeutic alliance.
Service-related factors such as experiencing pressure to take medication or lack of alternatives were a large part of the reasons for wanting MFT (63.16%). Lack of respect for not wanting medication was a common experience in recent treatment, and it can be difficult to quit medications without help. As shown by Yeisen, Bjørnestad, Joa, Johannessen, Opjordsmoen,26 some clinicians consider MFT unprofessional, unscientific, harmful, and unethical. Service users report strong informal pressure for medication during previous admissions, mirroring the staff sentiments found by Yeisen, Bjørnestad, Joa, Johannessen, Opjordsmoen.26 Notably, one of our interviewed participants seeking alternatives conveyed that medication was the only thing she had been offered, and alternatives had never really been discussed. Some of our interviewed participants who said they had been respected simultaneously conveyed that the respect was due to their own determination, strength, and/or knowledge. That is, even when agreeing to having been respected, they often conveyed an element of struggle. Our findings regarding these struggles correspond to previous qualitative research showing that discussing medication with professionals can be difficult.3,9 Further, quantitative research has found relationships between negative interactions with health care workers and not taking medication.2–8
Service users’ right to choose medication-free alternatives is limited by whether it is considered clinically justifiable.44 Therefore, mental health professionals still have defining power as to who is offered this option. Interestingly, critics of MFT have objected to both the safety of MFT as well as the notion that this alternative is not sufficiently available at present. Critics have questioned the need for MFT, saying there are already alternatives, for example, for people with psychosis being treated in ordinary health care.27 Yeisen, Bjørnestad, Joa, Johannessen, Opjordsmoen26 found many psychiatrists believed service users had a crucial impact on treatment choice and, accordingly, on adherence to medication.
Taken together, our findings support that although experiences are varied, a large proportion of service users had previous experience being disrespected for not wanting medication, and more than half of the service users report experiencing pressure to take medication or lack of alternatives to medication. This sheds important light on why the need for MFT units has arisen. It also highlights gaps in perception of reality among service users and health care professionals regarding the availability of options. As Blindheim9 has pointed out, health care professionals might not be sufficiently aware of the impact of power imbalance in communication about these issues.
Participants’ understanding of their problem, notions of recovery, and meaning attached to using medication were sometimes at odds with using psychotropics. Understanding of the problem was indicated as a reason for wanting MFT by 34.21%. MFT was associated with more dialogical and containing relationships in contrast to being assessed and medicated or “laid flat.” Belief in a better therapeutic process without medication, wanting to cope without medication, and associations between strength, acceptance, and being medication-free were also themes in the qualitative material. Previous research has found associations with freedom and not using medication.5 Taken together, these themes may be seen as wanting to be treated more as a subject and/or feeling more as a subject in their lives; in contrast, medication is associated with objectification. In our view, there is no necessary connection between medication and objectification. This association may be understood in light of the above-mentioned experiences with pressure regarding medication. There may also be correlations between emphasis on medication and a more authoritative stance that has to do with traditions within the mental health field.45 Additionally, one might imagine that the act of taking a substance that is supposed to affect a person’s thoughts and feelings in itself may collide with feeling in charge of the self. In previous research, involuntary medication has been described as a particularly invasive form of coercion.10
Strengths and Limitations
Our study was an exploratory study of one fairly typical medication-free unit. Mixed methods provide the opportunity for more in-depth knowledge of the influences at play in this context, which facilitates theoretical generalization as well as triangulation of results obtained with different methods.
The downside of the local nature of the study is that data from different contexts are not available. What service users want or expect to get out of MFT might be influenced by unique characteristics of the local medication-free unit in comparison to available alternatives and how this is presented to the service users via referrers, media, the medication-free unit, or other sources. For example, focus on motivation, effort, and empowerment might attract service users with certain attitudes and values or shape their narrative. How this translates to health care services at large must be inferred through theoretical generalization, including comparison of contexts and other research findings.
The response rate for questionnaires was high (82.14%), strengthening the representativeness of our sample in this context. There might be biases in selection for interviews, given that about half of service users declined the interview. From what is known about reasons for declining, we might have missed out on reports from the most distressed service users. The interview sample is on the smaller side because of difficult recruitment and so might not be saturated. The open-ended questions section of the questionnaire compensates somewhat for this.
There is the possibility that participants may feel they have to justify being on a medication-free ward when asked about this, even though their anonymity is protected. The exploration of this issue from different angles (interviews, different questionnaires, open-ended questions) may reduce this risk.
Conclusions
The majority of service users coming to the medication-free ward in our study confirm this was their own wish and give reasons in line with the goals of the government and user organizations. The findings demonstrate that these service users want an alternative to mainstream medication treatment. Negative effects of medications and difficulty in obtaining alternatives are important reasons for wanting this kind of service. Some also believe that taking medications does not fit with their concept of their problem and recovery. Our study highlights a gap in perception of the status quo between service users and critics of MFT regarding whether treatment without medication is perceived as available by service users who want this.
Future Implications
According to government authorities, service users have the right to choose MFT everywhere in mental health care as long as it is clinically justifiable.46 To make this option a reality, clinicians are advised to be mindful of communicating alternatives as well as the effect of power imbalances in their interactions with service users who disagree with them so that the medication-free choice does not become a struggle. The presence of informal pressure indicates potential for more shared decision making within the boundaries of what is considered clinically justifiable. It also indicates the need to further clarify these boundaries and the potential of medication-free alternatives.
Acknowledgments
We thank our participants for sharing their thoughts and experiences. We thank all the personnel involved in the treatment services for their invaluable efforts in gathering data. We especially thank the former leader of the hospital department at Åråsen Wenche Brandtzæg Nikolaisen for allocating resources to this project, the former leader of the inpatient treatment units at Åråsen Anders Skogen Wenneberg for supporting the project, research coordinator Bodil Skiaker for help with data management, assistant Shko Nagmadin Karim and Pia Jensen for plotting of data, Jorunn Iversen and Gunn Borgen for help in coordinating the data collection at the Myrvegen inpatient unit, Camilla Kvaase and Lene Paulsen for important roles in the data collection at Åråsen inpatent units, and Jill Arild for providing the user perspective as our user representative.
Funding Statement
The study was funded by Akershus University Hospital.
Data Sharing Statement
Raw data cannot be shared because of privacy regulations.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sohler N, Adams BG, Barnes DM, Cohen GH, Prins SJ, Schwartz S. Weighing the evidence for harm from long-term treatment with antipsychotic medications: a systematic review. Am J Orthopsychiatry. 2016;86(5):477–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev. 2020;9(1):17. doi: 10.1186/s13643-020-1274-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bjornestad J, Lavik KO, Davidson L, Hjeltnes A, Moltu C, Veseth M. Antipsychotic treatment-a systematic literature review and meta-analysis of qualitative studies. J Ment Health. 2019;29(5):513.523. doi: 10.1080/09638237.2019.1581352 [DOI] [PubMed] [Google Scholar]
- 4.Chapman SCE, Horne R. Medication nonadherence and psychiatry. Curr Opin Psychiatry. 2013;26(5):446–452. doi: 10.1097/YCO.0b013e3283642da4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Ribera C, Bulbena A. Determinants of medicine-taking in psychiatric patients. Curr Clin Pharmacol. 2011;6(2):100–107. doi: 10.2174/157488411796151156 [DOI] [PubMed] [Google Scholar]
- 6.Julius RJ, Novitsky MA Jr, Dubin WR. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Pract. 2009;15(1):34–44. doi: 10.1097/01.pra.0000344917.43780.77 [DOI] [PubMed] [Google Scholar]
- 7.Velligan DI, Sajatovic M, Hatch A, Kramata P, Docherty JP. Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Prefer Adherence. 2017;11:449–468. doi: 10.2147/PPA.S124658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marrero RJ, Fumero A, de Miguel A, Peñate W. Psychological factors involved in psychopharmacological medication adherence in mental health patients: a systematic review. Patient Educ Couns. 2020;103(10):2116–2131. doi: 10.1016/j.pec.2020.04.030 [DOI] [PubMed] [Google Scholar]
- 9.Blindheim A. Sluttrapport for brukerundersøkelse. prosjekt for medikamentfrie behandlingsforløp for psykose [Final Report from User Investigation. Project for Medication-Free Treatment Courses for Psychosis.]. Helse Bergen, Haukeland universitetssjukehus; 2020. Available from: https://helse-bergen.no/avdelinger/psykisk-helsevern/medikamentfritt-behandlingstilbod. Accessed June22, 2021. [Google Scholar]
- 10.Nyttingnes O, Ruud T, Rugkåsa J. ‘It’s unbelievably humiliating’—patients’ expressions of negative effects of coercion in mental health care. Int J Law Psychiatry. 2016;49:147–153. doi: 10.1016/j.ijlp.2016.08.009 [DOI] [PubMed] [Google Scholar]
- 11.Haugom EW, Stensrud B, Beston G, Ruud T, Landheim AS. Mental health professionals’ experiences with shared decision-making for patients with psychotic disorders: a qualitative study. BMC Health Serv Res. 2020;20(1):1093. doi: 10.1186/s12913-020-05949-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bjerkan AM, Pedersen PB, Lilleeng S. Brukerundersøkelse blant døgnpasienter i psykisk helsevern for voksne 2003 og 2007 [User investigation among inpatiens in mental health care for adults 2003 to 2007]. SINTEF Teknologi og samfunn. 2009. SINTEF A11409. Available from: https://www.sintef.no/globalassets/upload/helse/psykisk-helse/rapport-a11409-brukerundersokelse-blant-dognpasienter.pdf. Accessed June22, 2021.
- 13.Wunderink L, Nieboer RM, Wiersma D, Sytema S, Nienhuis FJ. Recovery in remitted first-episode psychosis at 7 years of follow-up of an early dose reduction/discontinuation or maintenance treatment strategy: long-term follow-up of a 2-year randomized clinical trial. JAMA Psychiatry. 2013;70(9):913–920. doi: 10.1001/jamapsychiatry.2013.19 [DOI] [PubMed] [Google Scholar]
- 14.Calton T, Ferriter M, Huband N, Spandler H, Systematic A. Review of the soteria paradigm for the treatment of people diagnosed with schizophrenia. Schizophr Bull. 2007;34(1):181–192. doi: 10.1093/schbul/sbm047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helsedirektoratet [Norwegian Directorate of Health]. Vurdering av behandlingsvilkåret i psykisk helsevernloven. gjennomgang og forslag til nye tiltak i tiltaksplan for redusert og kvalitetssikret bruk av tvang i psykisk helsevern [Evaluation of the Treatment Criterion in the Mental Health Care Act. Evaluation and Proposal for New Actions in the Action Plan for Reduced and Quality Assured Use of Coercion in Mental Health Care]; 2009. [Google Scholar]
- 16.Det kongelige helse- og omsorgsdepartement [Norwegian ministry of Health and Care]. Nasjonal strategi for redusert og riktig bruk av tvang i psykiske helsetjenester [National Strategy for Reduced and Correct Use of Coercion in Mental Health Services]; 2010. [Google Scholar]
- 17.Helse- og omsorgsdepartementet [Norwegian ministry of health and care]. Medikamentfrie tilbud i psykisk helsevern - oppfølging av oppdrag 2015 [Medication-free services in mental health care - follow up of mission 2015]. Helse- og omsorgsdepartementet, ed. Available from: www.regjeringen.no2015. Accessed June22, 2021.
- 18.NHO Service og Handel. Lyttet til pasientene - skapte det første medisinfrie psykiatriske sykehuset [Listened to the patients - made the first medication-free hospital]. NHO Service og Handel. Available from: https://www.nhosh.no/bransjer/helse-og-velferd/nyheter-helse-og-velferd/2019/horte-pa-pasientene--laget-sykehus-slik-brukerne-ville-ha-det/. 2019. [updated April 26, 2019]. Accessed July8, 2020.
- 19.Aksjon for medisinfrie tilbud [User coalition for medication-free services]. Grunndokument [positioning paper]. n.d.. Available from: http://medisinfrietilbud.no/grunndokument/. Accessed July31, 2018.
- 20.Helse Nord [Health region of northern Norway]. Protokoll for Medikamentfritt Døgntilbud I Helse Nord [Protocol for Medication-Free Inpatient Treatment in Helse Nord]; 2016. [Google Scholar]
- 21.Helse Sør-Øst [Health region of southeastern Norway]. Overordnet protokoll for medisinfri behandling innen psykisk helsevern [Overarching Protocol for Medication-Free Treatment in Mental Health Care]; 2016. [Google Scholar]
- 22.Standal K, Heiervang KS. Medisinfri behandling – et omstridt og etterlengtet tilbud [Medication-free treatment - controversial and awaited]. Tidsskrift Psykisk Helsearbeid. 2018;15(4):335–346. doi: 10.18261/issn.1504-3010-2018-04-07 [DOI] [Google Scholar]
- 23.Slade M, Leamy M, Bacon F, et al. International differences in understanding recovery: systematic review. Epidemiol Psychiatr Sci. 2012;21(4):353–364. doi: 10.1017/S2045796012000133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Øvernes LA. Medikamentfrie behandlingsforløp for personer med psykoselidelser. Erfaringer fra pilotprosjektet i Helse Bergen. [Medication-Free Treatment Courses for Persons with Psychosis. Experiences from the Pilot Project in Bergen]. Helse Bergen HF, Helse Vest RHF; 2019. https://helse-bergen.no/avdelinger/psykisk-helsevern/medikamentfritt-behandlingstilbod:. Accessed June22, 2021. [Google Scholar]
- 25.Bjørgen D, Kvisle IM, Johansen KJ, Leinan TBS, Benschop AR, Kildal C. Legemiddelfri behandling - Mitt liv, mitt valg! Bruker spør Bruker-evaluering av de legemiddelfrie behandlingstilbudene i fire helseregioner [Medication-Free Treatment - My Life, My Choice! User Asks User-Evaluation of the Medication-Free Treatment Services in Four Health Regions]. Stiftlesen Kompetansesenter for brukererfaring og tjenesteutvikling (KBT); 2020. [Google Scholar]
- 26.Yeisen RAH, Bjørnestad J, Joa I, Johannessen JO, Opjordsmoen S. Psychiatrists’ reflections on a medication-free program for patients with psychosis. J Psychopharmacol. 2019;33(4):459–465. doi: 10.1177/0269881118822048 [DOI] [PubMed] [Google Scholar]
- 27.Røssberg JI, Andreassen OA, Ilner SO. Re: psykiatriens indre konflikter eksponert [Reply to Inner conflicts of psychiatry exposed]. Tidsskr nor Laegeforen. 2017;9:137. [DOI] [PubMed] [Google Scholar]
- 28.Røssberg JI, Andreassen OA, Malt U. Medisinfrie tiltak for psykoselidelser er fortsatt et sjansespill [Medication-free measures for psychotic disorders is still a risky game]. Aftenposten. 2016;17(7):16. [Google Scholar]
- 29.Heskestad S, Kalhovde AM, Jakobsen ES, Tytlandsvik M, Horpestad L, Runde IKS. Medikamentfri psykiatrisk behandling - hva mener pasientene? [Medication-free treatment - what do the patients say?]. Tidsskr nor Laegeforen. 2019;139(14). [DOI] [PubMed] [Google Scholar]
- 30.Oedegaard CH, Davidson L, Stige B, et al. “It means so much for me to have a choice”: a qualitative study providing first-person perspectives on medication-free treatment in mental health care. BMC Psychiatry. 2020;20(1):399. doi: 10.1186/s12888-020-02770-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akershus universitetssykehus [Akershus university hospital]. Medisinfri behandling [Medication-free treatment]. n.d.. Available from: https://www.ahus.no/behandlinger/medisinfri-behandling. Accessed December8, 2018.
- 32.Mueser KT, Gingerich S. IMR. Kurs i personlige ferdigheter og mestringsstrategier for personer med alvorlige psykiske lidelser. Minnesota: Dartmouth PRC. Hazelden; 2011. [Google Scholar]
- 33.Monsen JT, Monsen K. Affekter og affektbevissthet: et bidrag til integrerende psykoterapimodell [Affects and affect consciousness: a contribution to an integrative psychotherapy model]. In: Holte A, Nielsen GH, Rønnestad H, editors. Psykoterapi og psykoterapiveiledning. Teori, empiri og praksis. Oslo: Gyldendal akademisk; 2000:71–90. [Google Scholar]
- 34.Miller SD, Hubble MA, Chow D, Seidel J. Beyond measures and monitoring: realizing the potential of feedback-informed treatment. Psychotherapy. 2015;52(4):449–457. doi: 10.1037/pst0000031 [DOI] [PubMed] [Google Scholar]
- 35.Seikkula J, Arnkil TE. Åpen dialog i relasjonell praksis. Respekt for annerledeshet i øyeblikket. [Open Dialogue in Relational Practice. Respect for Difference in the Moment.]. Oslo: Gyldendal akademisk; 2013. [Google Scholar]
- 36.Hammer J, Heggdal D, Lillelien A, Lilleby P, Fosse R. Drug-free after basal exposure therapy. Tidsskr nor Laegeforen. 2018;138(6). [DOI] [PubMed] [Google Scholar]
- 37.Creswell JW Mixed methods procedures. In: Creswell JW, editor. Research Design. Qualitative, Quantitative and Mixed Methods Approaches. California: Sage; 2009:203–227. [Google Scholar]
- 38.Drivenes K, Vederhus J-K, Haaland VØ, et al. Enabling patients to cope with psychotropic medication in mental health care: Evaluation and reports of the new inventory MedSupport. Medicine. 2020;99(1) doi: 10.1097/MD.0000000000018635. [DOI] [PMC free article] [PubMed]
- 39.Ødegaard C. Medication Free Treatment in Psychosis: The Meaning of Choice for People with Psychosis - a Qualitative Exploration. University of Bergen; 2018. Available from: https://www.uib.no/en/cih/122122/christine-%C3%B8degaard-medication-free-treatment-psychosis. Accessed March6, 2019. [Google Scholar]
- 40.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 41.Medication Free Treatment: Characteristics, Justification and Outcome. ClinicalTrials.Gov. 2018. Available from: https://clinicaltrials.gov/ct2/show/NCT03499080?term=Kristin+Heiervang&recrs=ab&cntry=NO&rank=1. Accessed June22, 2021.
- 42.O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ. 2010;341(7783):341:c4587. doi: 10.1136/bmj.c4587 [DOI] [PubMed] [Google Scholar]
- 43.Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res. 2006;16(3):377–394. doi: 10.1177/1049732305285708 [DOI] [PubMed] [Google Scholar]
- 44.Helse- og omsorgsdepartementet [Norwegian ministry of health and care]. Oppdragsdokument 2015, Helse Sørøst [Mission document 2015, South-eatsern health region of Norway]. Helse- og omsorgsdepartementet, ed. Available from: www.regjeringen.no2015. Accessed June22, 2021.
- 45.Bentall R. Doctoring the Mind. Why Psychiatric Treatments Fail. London: Penguin Books; 2009. [Google Scholar]
- 46.Meland C, Dammen C Medikamentfrie tilbud i psykisk helsevern - oppfølging av oppdrag 2015 [Medication-free services in mental health care - follow up of mission 2015]. omsorgsdepartementet H-o, ed. 2015. Available from: www.regjeringen.no. Accessed June22, 2021.