Abstract
The SARS-CoV-2 pandemic continues to spread relentlessly, associated with a high frequency of respiratory failure and mortality. Children experience largely asymptomatic disease, with rare reports of a Multisystem Inflammatory Syndrome in Children (MIS-C). Identifying immune mechanisms that result in these disparate clinical phenotypes in children could provide critical insights into COVID-19 pathogenesis. Using Systems Serology, here we observed in 25 children with acute mild COVID a functional phagocyte and complement activating IgG response to SARS-CoV-2, comparable to the acute responses generated in adults with mild disease. Conversely, IgA and neutrophil responses were significantly expanded in adults with severe disease. Moreover, weeks after the resolution of SARS-CoV-2 infection, children who develop MIS-C maintained highly inflammatory monocyte activating SARS-CoV-2 IgG antibodies distinguishable from acute disease in children but with antibody levels comparable to convalescent adults. Collectively, these data provide unique insights into the potential mechanisms of IgG and IgA that may underlie differential disease severity as well as unexpected complications in SARS-CoV-2 infected children.
Editor summary:
A study of Multisystem Inflammatory Syndrome in Children (MIS-C) shows maintenance of elevated levels of monocyte-activating pathogen-specific IgG, not seen in SARS-CoV-2-infected children who don’t develop MIS-C.
Introduction
The SARS-CoV-2 pandemic remains an enormous global challenge due to its persistent spread and unpredictable disease course. While adults can exhibit moderate to severe disease with high mortality, children surprisingly experience largely benign disease characterized by mild cold-like symptoms despite high viral loads1–3. Several hypotheses for this disparate phenotype have emerged, including the presence of distinct Angiotensin converting enzyme 2 (ACE2) receptor expression patterns in children3, the potential for pre-existing cross-coronavirus humoral immunity that may attenuate early infection4,5, and the potential for a more naïve immune repertoire compared to adults. However, a small but significant fraction of SARS-CoV-2-infected or exposed children develop a Kawasaki-disease (KD)-like syndrome, now termed Multisystem Inflammatory Syndrome in Children (MIS-C)6–8. Weeks after SARS-CoV-2 exposure or infection, children with MIS-C present with fever, clinical markers of inflammation, and multi-organ involvement, which can include hypotensive shock, cardiac aneurysms, and ventricular failure9.
Emerging data have linked the humoral immune response to SARS-CoV-2 in adults to both protection as well as pathology10. To begin to define whether differences in the humoral immune response may account for differences in severity of disease across adults and children and point to pathological changes in MIS-C, here we deeply profiled the functional humoral immune response in 60 adults with acute SARS-CoV-2 infection (26 severe, 34 mild), 25 children with acute but mild SARS-CoV-2 infection, and 17 children with PCR or serology confirmed (n=14) or suspected (e.g. household contacts, n=3) SARS-CoV-2 exposure who developed MIS-C (11 severe, 6 mild). The data point to a pathological role for SARS-CoV-2-specific IgA responses linked to neutrophil activation in severe adult infection, which are not amplified in children or in mildly infected adults. Conversely, sustained levels of inflammatory macrophage-activating, Fc-receptor binding antibodies specific for different pathogens— including SARS-CoV-2— were selectively maintained in severe MIS-C disease. Collectively, these data identify unique functional antibody responses that implicate neutrophils and/or macrophages in SARS-CoV-2 disease pathology, revealing biomarkers and pathways to guide clinical care and therapeutic development.
Results
Within days of symptom onset, SARS-CoV-2-specific antibodies are detectable, marking SARS-CoV-2 exposure. However, beyond their absolute quantities, shifts in polyclonal antibody composition mark different responses to infection and disease trajectory11. Whether the polyclonal antibody composition differs across adults and children, the latter who largely experience asymptomatic to mild disease, is currently unknown. Thus, we comprehensively profiled the SARS-CoV-2-specific humoral immune response across a group of acutely infected adults and children, including 25 paucisymptomatic children/young adults (ages 0–21 years, median = 15y) compared to 34 adults (ages 22–76 years, median = 34y) with mild disease who did not require hospitalization, and 26 adults (age range: 32–79years, median = 56y) with more severe SARS-CoV-2 infection and all of whom required hospitalization (Supplemental Table 1). Acute SARS-CoV-2 infection was diagnosed by related symptoms and positive PCR and/or serology. Samples were collected 0 to 52 days after symptoms onset (median = 9 days), depending on patient availability (e.g. during outpatient clinic visit).
Low IgA and phagocytic activity track with mild disease in children and adults
As expected, high titers of SARS-CoV-2 spike (S)-specific IgM, IgG and IgA titers were observed in adults with severe infection (Figure 1A and B). Conversely, S-specific IgG and IgM levels were comparable in paucisymptomatic children and adults with mild acute infection but significantly lower compared to severe disease. In contrast to more attenuated but similar SARS-CoV-2 receptor-binding domain (RBD), spike (S) and nucleocapsid (N)-specific isotype, subclass, and Fc-receptor binding levels in children and adults with mild disease, severely ill patients exhibited robustly expanded humoral immune responses (Figure 1B and Supplemental Figure 1–3). Next, we tested the ability of plasma antibodies to induce Fc-mediated effector function. Antigen:antibody immune-complexes (ICs) were generated by incubating plasma with antigen-coated fluorescent beads, and ICs were then cultured with complement, THP-1 monocytes or HL60 differentiated neutrophils to analyze complement deposition or phagocytic activity. Similar levels of complement, neutrophil, and monocyte activating antibodies were observed in children and mildly infected adults, but significantly lower compared to adults with severe infection (Figure 1C and Supplemental Figure 4). Interestingly, pediatric patients, typically diagnosed earlier, exhibited a tendency to develop antibodies earlier after symptom onset compared to adults. Within seven days after symptom onset only 2 of 18 adults vs. 5 of 18 children were positive for Spike-specific IgG1 and 3 of 18 adults vs 7 of 18 children positive for Spike-specific IgM, potentially contributing to reduced pathology and differences in kinetics of overall symptomatology across the ages (Supplemental Figure 5), however responses in children were similar to those observed in adults that experienced mild disease (Figure 1A and B). These data suggest that children may not necessarily make a stronger or more effective functional humoral immune response compared to adults.
Figure 1: Disease severity tracks with enhanced humoral immunity to COVID-19.
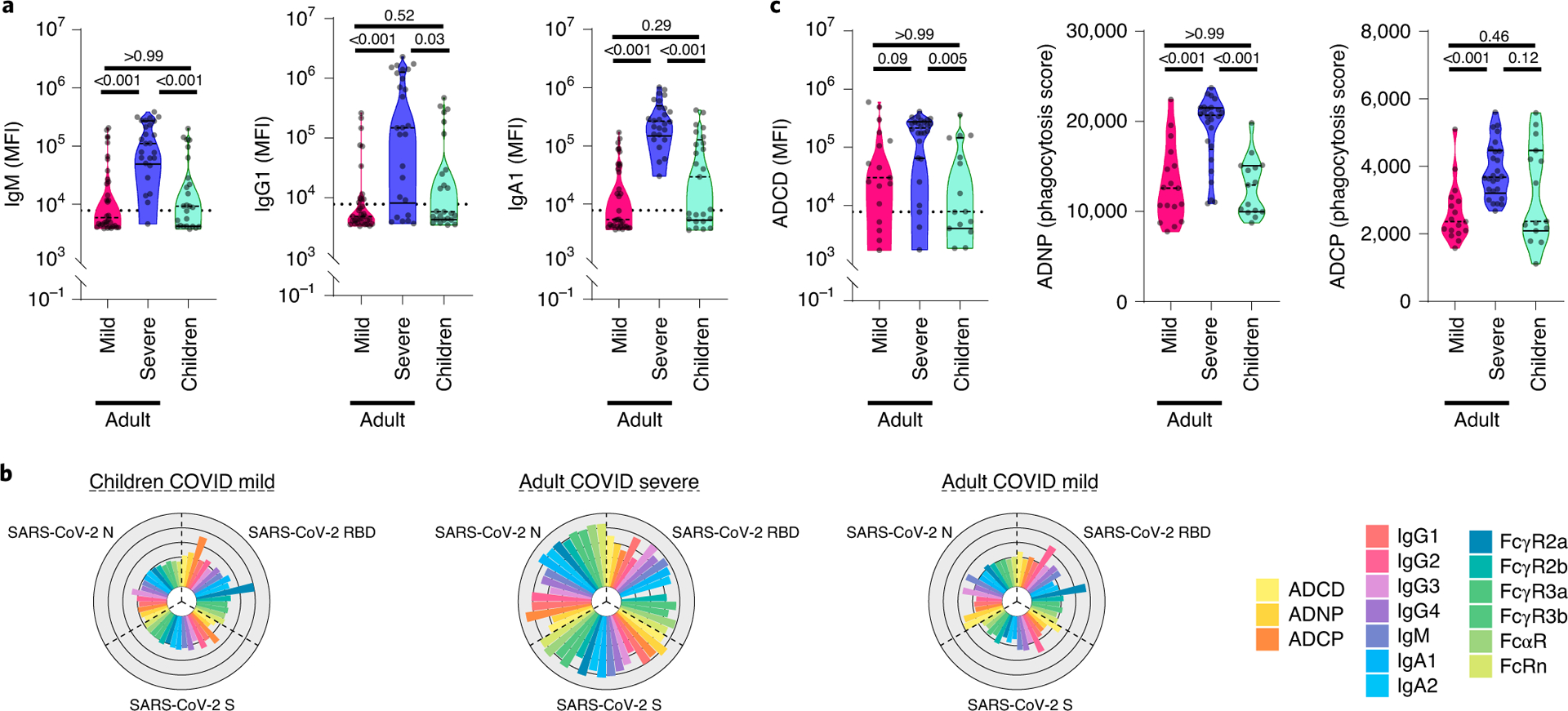
SARS-CoV-2 specific plasma antibody responses in mild (non-hospitalized) or severe (hospitalized) adult COVID-19 patients and children with mild COVID-19 patients were analyzed. A) SARS-CoV-2 Spike (S) protein specific IgM, IgG1 and IgA1 titers were analyzed by Luminex (nmild=34, nsevere=26, nchildren=25). The dotted line represents the average plus 5 times the standard deviation of the negative plasma samples used to determine seropositivity (see Methods). B) IgG subclasses 1–4, isotypes IgM, IgA1 and IgA2, and antibody-mediated functions (complement deposition (ADCD), neutrophil phagocytosis (ADNP) and THP-1 monocyte phagocytosis (ADCP)) for SARS-CoV-2 RBD, S and N were analyzed in all seropositive individuals (nmild=17, nsevere=26, nchildren=15). Each flower plot summarizes the data from the respective group and the length of each petal represents the average of the Z-scored value for the indicated feature (Supplemental Figures 1–4). C) Univariate comparison of ADCD, ADNP and ADCP against SARS-CoV-2 S in seropositive individuals are shown. The dashed line in the violin plots indicate the median per group and solid lines indicate quartiles. A non-parametric Kruskal-Wallis test was used to test for statistically significant differences between multiple groups.
To next determine whether any multivariate differences exist among the adult and pediatric profiles of seropositive individuals, an unsupervised Uniform Manifold Approximation and Projection (UMAP) was initially used to collapse the multivariate data into 2 dimensions, with proximity representing similarities in the overall dataset. Separation was observed visually across children and severely ill individuals in the UMAP, pointing to substantial global humoral profile differences across the groups (Figure 2A). Similarly, discrete antibody profiles were observed across severely and mildly ill adults (Figure 2B). In contrast, adults with mild disease and children overlapped extensively, highlighting the multivariate similarity in the overall SARS-CoV-2 antibody profiles between the groups (Figure 2C). The integration of all 3 groups in a single UMAP further highlighted the similarity in mild disease antibody profiles among adults and children, that were largely distinct from, albeit along a continuum with, those in severely ill adults, suggesting that severity of disease, rather than age, may influence antibody profiles predominantly (Supplemental Figure 6).
Figure 2: SARS-CoV-2 specific IgA titers and augmented antibody functionality discriminate severe from mild disease.
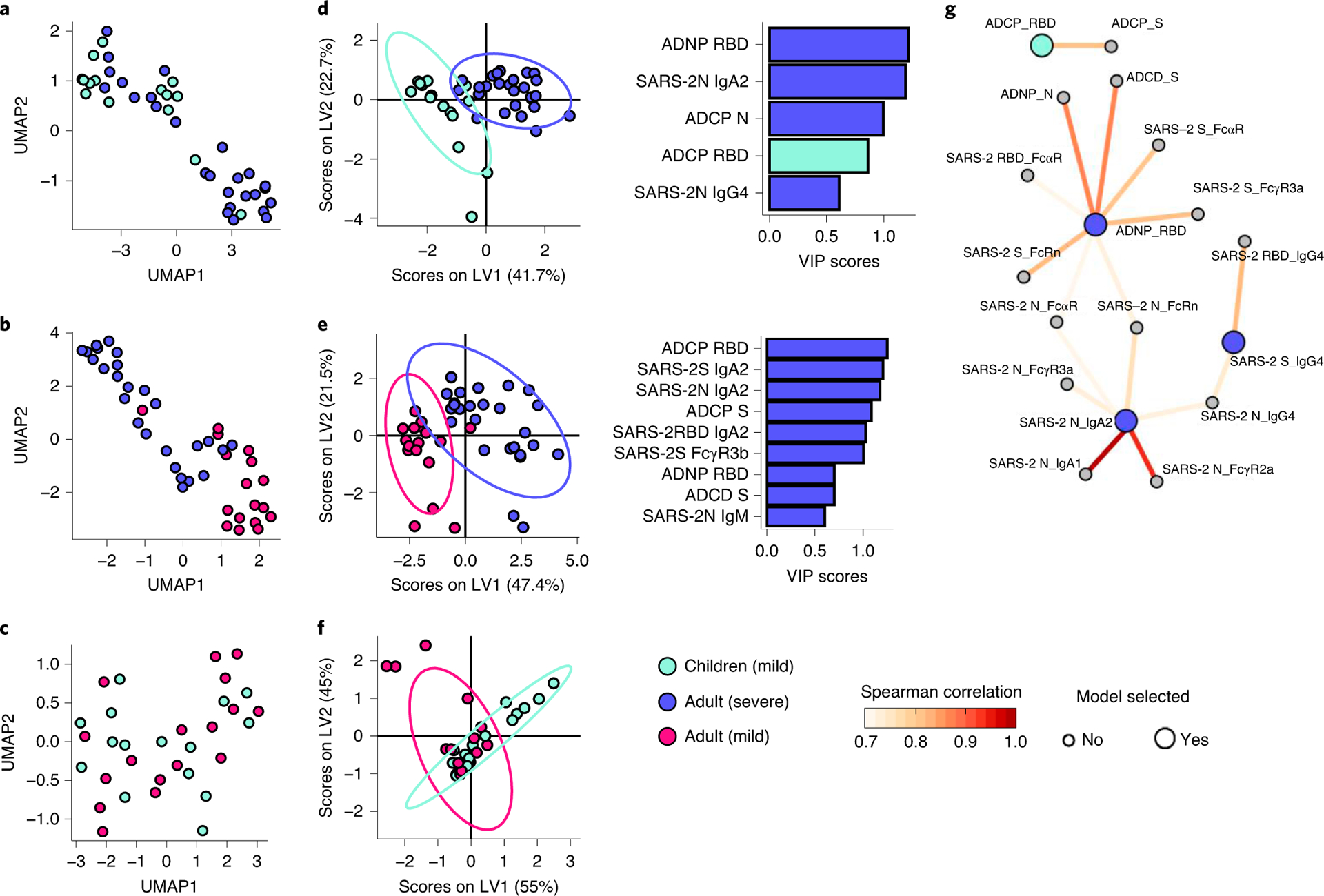
Pair-wise comparisons were performed between seropositive mild diseased children and severely ill adults (A and D), mild and severe diseased adults (B and E) or mild diseased children and adults (C and F) (nmild=17 nsevere=26, nchildren=15). A, B, C) Multivariate UMAP analyses show the variation in the multivariate humoral profiles across the groups. Proximity of points indicate homology in the overall dataset. D, E, F). In a second approach, a supervised multivariate comparison was performed across groups, where features were initially reduced using LASSO, to avoid overfitting, and then visualized by PLS-DA (left panel). Cross-validation accuracy for D, E, F) was: 0.91, 0.97, 0.65, respectively. The LASSO selected features were also plotted and ranked in a VIP score plot (right panel, color of bars indicate in which group the feature was enriched). G) Network correlations depict the additional non-LASSO-selected Fc-profile features (small circles) that were correlated with the LASSO selected features (big circles) based on pair-wise comparisons between children and severely ill adults. The connections between points (features) indicate significant (p>0.05) Spearman correlations. Fill color of the circles indicate in which group the selected feature were enriched (grey = feature was not selected), the color of connecting lines indicate the strengths of the correlation coefficient.
To further define the individual features that distinguished children or adults with mild infection from adults with severe disease, we used Least Absolute Shrinkage and Selection Operator (LASSO) feature selection to initially reduce the total 48 antibody variables to a minimal set that represented the overall variation in the antibody profiles, followed by classification using Partial Least-Squares Discriminant Analysis (PLS-DA). Nearly perfect separation was observed between children and severely ill adults (Figure 2D). The model used only 5 of the total 48 measured features to resolve the 2 groups, including RBD-specific-neutrophil phagocytosis, N-specific IgA2 levels and monocyte phagocytosis enriched in severely ill adults, and RBD-specific monocyte phagocytosis enriched in children. These data point to significantly expanded IgA and phagocytic functional responses in severely ill individuals, suggesting IgA-driven immune complex phagocyte activation as a marker of disease severity. Likewise, near complete separation was observed between adults with mild and severe disease (Figure 2E), marked again by high levels of monocyte phagocytic functions, IgA2 responses, and S-specific binding to FcγR3b expressed on neutrophils, neutrophil phagocytosis, as well as complement activation and IgM titer in severely ill adults. In contrast, antibody profiles between children and adults with mild disease could not be resolved (Figure 2F).
A correlation network was constructed between LASSO-selected features and the overall immune response to deeply probe the distinct relationships that diverged between severe and mild disease (Figure 2G and Supplemental Figure 7). N-specific IgA, N-, S-, and RBD-specific Fcα-receptor (FcαR) binding (found constitutively on neutrophils12), neutrophil phagocytosis and complement activation were all induced in a synchronized manner, pointing to a central axis of IgA:neutrophil activation in severe disease. Moreover, while depletion of IgG, our dominant serum antibody, resulted in attenuated neutrophil phagocytosis across all groups, depletion of IgA reduced ADNP significantly only among severely ill individuals (Figure 3A–C). Moreover, while depletion of IgG was sufficient to eliminate ADNP in mild adults and children (Figure 3A and C), combined depletion of IgG and IgA resulted in complete loss of ADNP in severe adults (Figure 3C), pointed to an added role of IgA in neutrophil activation in severe disease.
Figure 3. Unique functional and evolutionary profiles of SARS-CoV-2 IgA antibodies.
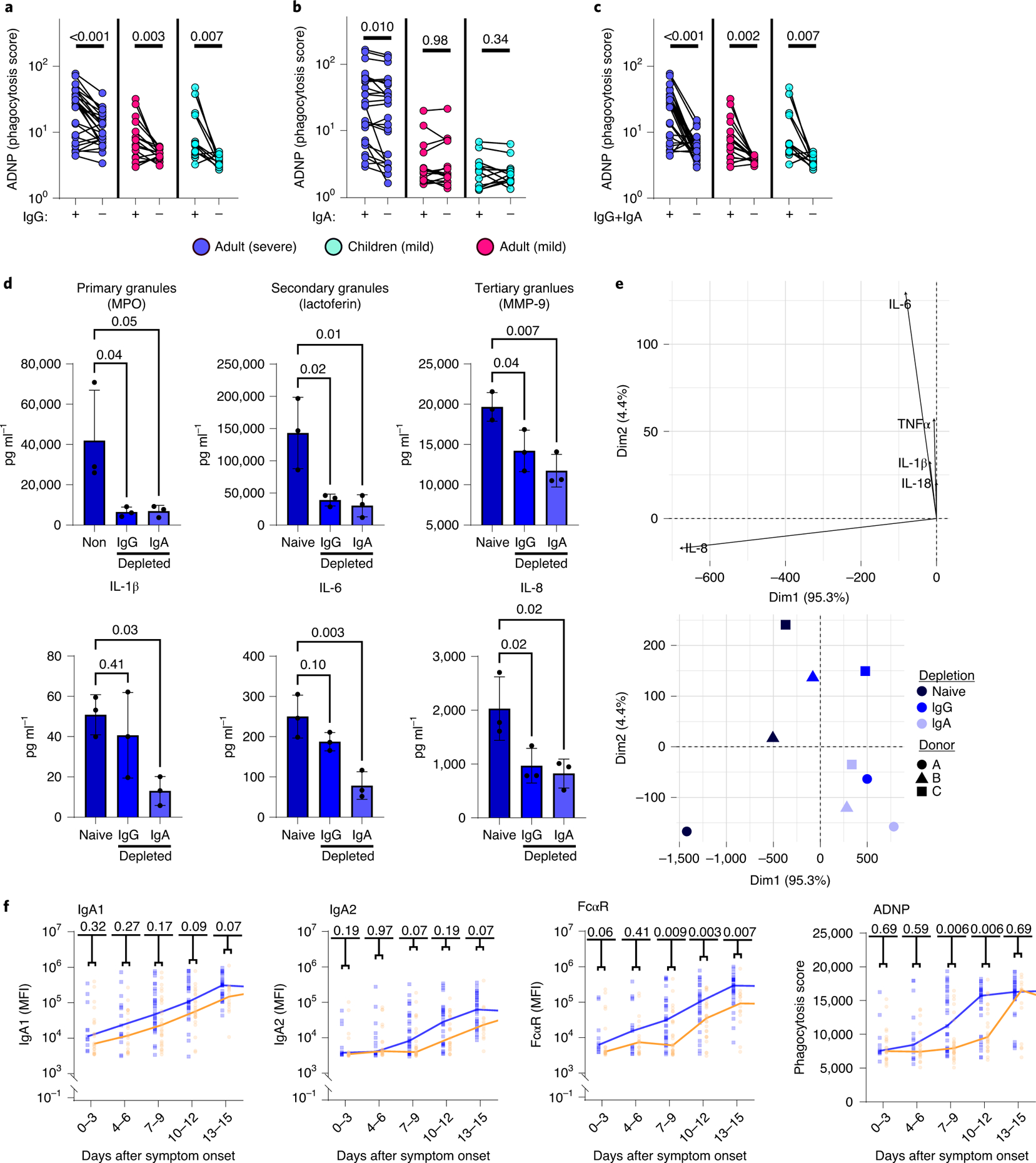
The matched-line graphs show the impact of IgG (A) and IgA (B) and IgG+IgA (C) depletion on ADNP activity across severely ill adults (dark blue, n=25), mildly ill adults (red, n=16), or children with mild disease (light blue, n=12). (D) The bar graphs show the level of degranulation of MPO, lactoferrin and MMP-9, and cytokine secretion of IL-1β, IL-6, and IL-8 in pooled naïve/undepleted plasma from severe adult COVID patients compared to IgG or IgA depleted plasma. Data are presented as mean values +/− SD of three individual blood neutrophil donors. (E) The principal component analysis highlights the multivariate functional profiles observed in undepleted, IgG or IgA depleted plasma, highlighting the distinct inflammatory cascades associated with IgA depletion (light blue) that intermingled with IgG depleted plasma (medium blue), both of which were distinct from naïve undepleted plasma (black). (F) The line graphs show the longitudinal evolution of IgA1, IgA2, FcαR binding, and ADNP at different timepoints in severely (n=59) or moderately (n=77) ill individuals followed within the first 2 weeks following symptom onset (not all timepoints for all individuals were available). Statistical significance in A–C was calculated by non-parametric two-sided Wilcoxon matched-pairs signed rank test and a parametric One-way ANOVA in D. A Mann-Whitney test was used to assess statistical difference between the groups at each interval in F) and p-values were corrected for multiple hypothesis testing using the Benjamini-Hochberg procedure.
Given our emerging appreciation for excessive neutrophil activity in COVID-19 pathology13,14, we further probed the functional role of IgA in neutrophil IC-responsiveness in vitro. Despite the pronounced effect of IgG in attenuating neutrophil phagocytosis, the depletion of both IgG and IgA resulted in a loss of degranulation-mediated release of myeloperoxidase (MPO), lactoferrin and matrix metalloproteinase-9 (MMP-9), as well as attenuated cytokine secretion (Figure 3D and Supplemental Figure 8). Specifically, compared to IgG depletion, elimination of IgA further decreased tertiary MMP-9 granule, interleukin-1β (IL-1β), IL-6, and IL-8 release from neutrophils (Figure 3D), resulting in a unique IgA-driven multivariate functional cascade marked by enhanced inflammatory neutrophil activity in the presence of SARS-CoV-2-specific IgA (Figure 3E), as has been noted previously15,16. Furthermore, longitudinal profiling of an orthogonal cohort of hospitalized individuals pointed to the selective evolution of enhanced IgA2 levels in severely ill individuals, particularly 1 week after symptom onset, linked to disproportionately higher levels of FcαR binding and ADNP activity (Figure 3F), potentially implicating IgA2 emergence as a unique mechanistic marker of severe SARS-CoV-2 disease. Thus, collectively these data strongly implicate IgA-driven functions in severe disease that do not evolve in children or adults with mild disease. However, while exploratory, additional investigation is needed to completely resolve the contribution of IgA driven neutrophil activation to the full severity cascade observed in severe SARS-CoV-2 infection.
Persistence of inflamed SARS-CoV-2 antibodies track with MIS-C
Despite the largely mild nature of pediatric SARS-CoV-2 infection, a subset of children develop a severe inflammatory-mediated illness after infection, MIS-C, including potential antibody-driven immunopathology similar to KD6,8. While early data has pointed to differences in IgM levels in children with MIS-C compared to acutely infected adults and children17, this loss of IgM could simply be attributable to the resolution of infection in MIS-C that occurs weeks after infection. Thus, to begin to delineate whether particular polyclonal antibody signatures could provide mechanistic insights into MIS-C, SARS-CoV-2 specific humoral immunity was profiled across children with mild (n=6) or severe (n=11) MIS-C compared to a group of non-hospitalized convalescent adults (n=18) who had mild disease symptoms (not hospitalized and no oxygen therapy required), the latter matched for time from suspected infection (days from COVID-19 symptom onset: 11– 38, median: 27 days) (Figure 4 and Supplemental Table 1). A total of 17 children/young-adults (0 −21.9 years, median 3.5y, 83 % male, days from MIS-C symptom onset: 2- 23, median: 3 days) were diagnosed with MIS-C per CDC criteria (reference: https://www.cdc.gov/mis-c/hcp/): patients had fever, laboratory evidence of inflammation, multisystem involvement that required hospitalization, with no alternative diagnosis. In addition, all MIS-C patients had evidence of SARS-CoV-2 infection (positive SARS-CoV-2 RT-PCR or antigen test, or positive SARS-CoV-2 antibodies) or confirmed SARS-CoV-2 exposure (e.g. household or childcare contacts). Of note, one of our patients was 21.9 years old but otherwise met CDC MIS-C criteria. Patients with MIS-C were stratified by severity, with severe patients defined as experiencing cardiac complications (see Methods and Supplemental Table 2). The severe MIS-C cohort exhibited comparable IgM and IgG1 titers to those observed in convalescents adults. Conversely, despite a positive RT-PCR result in 50% of the children, SARS-CoV-2 antibodies were not detectable in the majority of mild MIS-C cases here (only one child in this group had detectable levels of S and RBD-specific IgG3 and IgA1 by Luminex; Figure 4A and Supplemental Figure 1–3). However, all MIS-C patients had evidence of previous SARS-CoV-2 exposure defined by either by positive PCR or serology or confirmed contact. Focusing on convalescent adults and severe MIS-C children, that both harbored robust SARS-CoV-2 humoral immune responses weeks after infection, a broad isotype, subclass, and functional antibody profile was observed (Figure 4B and Supplemental Figure 4), although the specific expanded humoral features differed across the groups (Figure 4B). For example, while similar levels of complement deposition and neutrophil phagocytosis were observed in the convalescent adults and severe MIS-C cases (Figure 4B and C), MIS-C cases exhibited enhanced monocyte activating capacity (Figure 4C). This suggests convalescent-like profiles in the severe MIS-C cases, but the presence of a select set of altered antibody features that uniquely emerge in this pathological setting.
Figure 4: Distinct SARS-CoV-2 specific antibody responses in children with severe MIS-C.
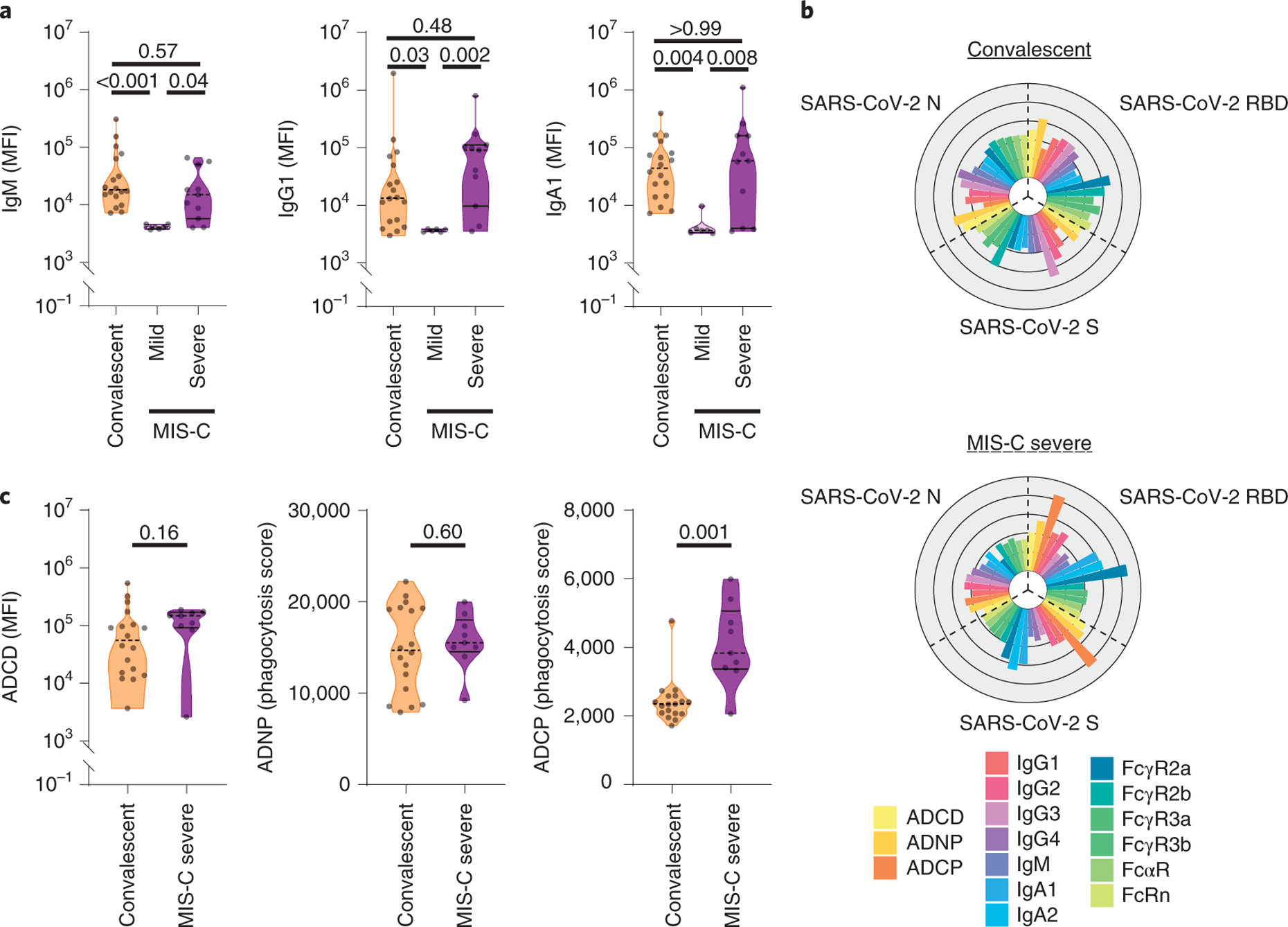
SARS-CoV-2 specific plasma antibody responses were analyzed in children with mild or severe MIS-C or convalescent adults. A) SARS-CoV-2 Spike (S) protein specific IgM, IgG1 and IgA1 titers were analyzed by Luminex (nconv=18, nmild=6, nsevere=11). The dotted line represents the average plus 5 times the standard deviation of the negative plasma samples used to determine seropositivity (see Methods). B) IgG subclasses 1–4, isotypes IgM, IgA1 and IgA2, and antibody-mediated functions (ADCD, ADNP, and ADCP) for SARS-CoV-2 RBD, S and N in all seropositive individuals were analyzed (nconv=18, nsevere=9). Each flower plot summarizes the data of the respective group and each petal represents the average of the Z-scored value for the indicated feature (Supplemental Figures 1–4). C) Univariate analysis of ADCD, ADNP, and ADCP against SARS-CoV-2 S are shown. Dashed lines in the violin plots indicate the median per group and solid lines indicate quartiles. A non-parametric two-sided Mann-Whitney test was used to test for statistically significant differences between the two groups.
To gain deeper insights into the specific immune alterations that define MIS-C, we next performed multivariate analysis. Clear separation was observed in the multivariate SARS-CoV-2 response in mild and severe MIS-C (Figure 5A) both by UMAP and LASSO/PLSDA, driven by the presence of SARS-CoV-2-specific IgG and IgM responses in the severe cases. Interestingly, severe MIS-C cases were distinguishable from both convalescent adults (Figure 5B) and mild children (Figure 5C) largely linked to higher SARS-CoV-2-specific antibody titers with more phagocytic and functional activity distinct from immune responses in severe acute disease in adults (Supplemental Figure 9). Network analysis highlighted the over-representation of functional humoral immune responses in the MIS-C children, pointing to a potential IC-based activity in disease pathology (Figure 5D). Additionally, comparison of MIS-C children to adults with severe acute disease revealed distinct antibody profiles across the 2 groups, with expanded IgG driven function in MIS-C and IgA/neutrophil expanded immune responses in the severe adults, pointing to a persistent IgG-related disease in MIS-C (Supplemental Figure 10)17 and IgA-related disease in acute SARS-CoV-2 infection.
Figure 5: Dysregulated and pro-inflammatory antibody-profiles in children with severe MIS-C.
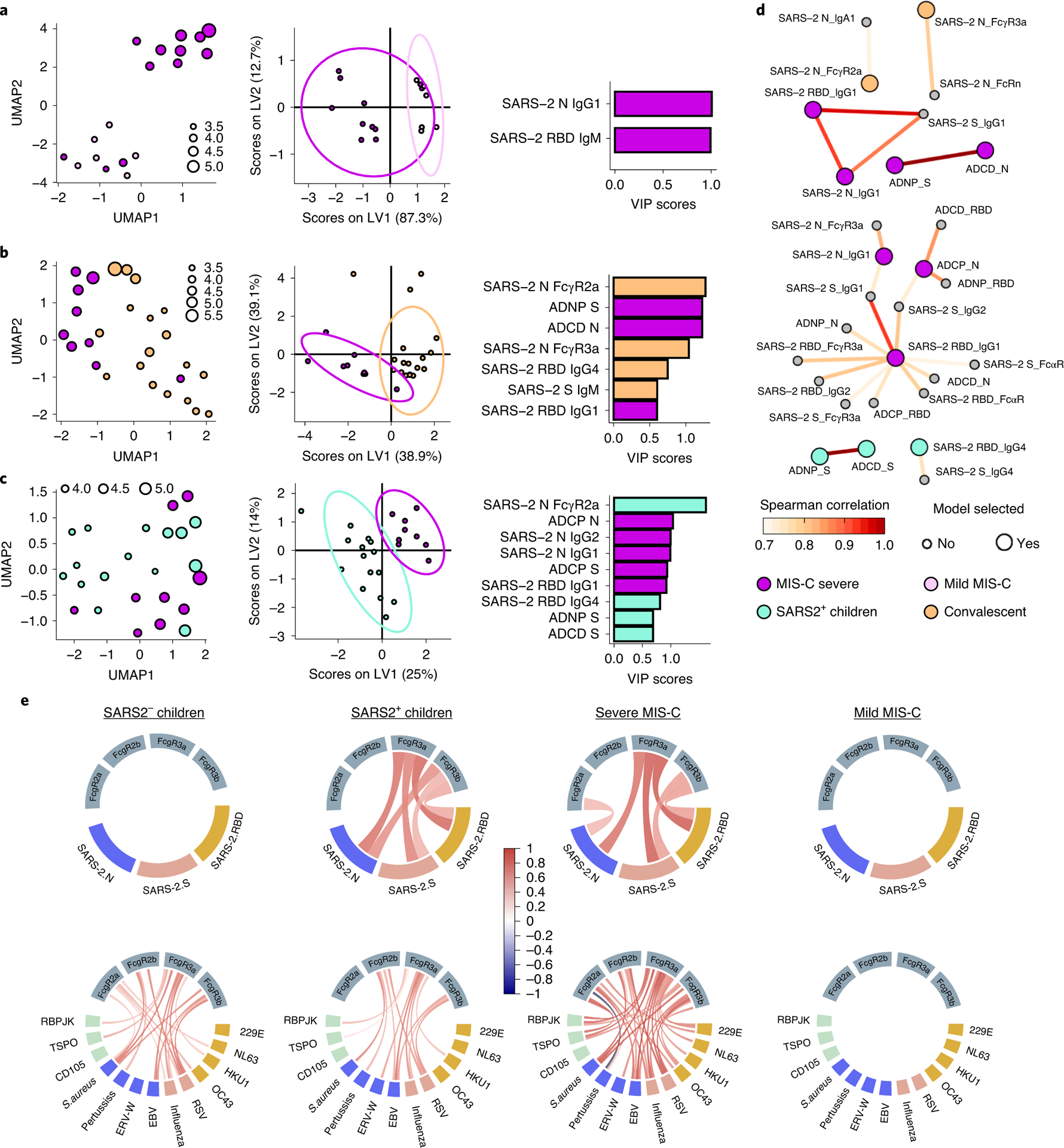
Pairwise comparisons by UMAP and LASSO/PLS-DA analyses are shown across mild and severe MIS-C (A), severe MIS-C and convalescent (B) or severe MIS-C and acutely infected children (C) (nmild_MIS-C=6, nsevere MIS-C=9, nSARS+ children=15, nconvalescent=18). The size of each dot represents the log10 scaled value of IgG1 titer to SARS2 RBD. The cross-validation accuracy in B) and C) were: 0.89, 0.88, respectively. D) The correlation network of LASSO selected (big circles) or unselected (small circles) features are shown across children and severely ill adults. Connection between points (features) indicate significant relationships (p>0.05) defined by a Spearman correlation after Benjamini-Hochberg correction. Fill color of the circles indicate in which group the selected feature was enriched (grey = feature was not selected), the color of the connecting lines indicates the correlation coefficient. E) The chord diagrams show the relationships of Luminex defined IgG1 titers across SARS-CoV-2 antigens (upper panel, yellow =RBD, red =S, and blue =N) and other pathogens and auto-antigens (lower panel, yellow = common CoVs RBD, red = other respiratory viruses, blue = KD associated pathogens, green = MIS-C associated auto-antigens) assessed by Spearman correlation. The connecting lines between colored boxes (antigen-specific IgG1 titer) and grey boxes (FcγRs) indicate a significant (p<0.05) correlation between antigen-specific IgG1 titers and binding to the indicated FcγR for the respective antigen. A color-gradient was used to indicate the correlation coefficient (from r=−1 (dark blue) over r=0 (white) to r=1 (dark red)) for the individual correlations.
However, why the children with MIS-C maintained a response able to continue to recruit a SARS-CoV-2-specific phagocytic and complement activating response remains unclear, but collectively points to more inflamed antibody profiles among severe MIS-C cases. Strikingly, this inflamed antibody profile was not only observed in the SARS-CoV-2 specific humoral immune response: as shown in Figure 5E (and Supplemental Figure 11), an expansion of highly functional antibodies were observed specific for multiple pathogens that have been implicated, but not proven to drive, KD (EBV, measles, endogenous retrovirus (ERV), B. pertussis and S. aureus), auto-antigens linked to MIS-C, common respiratory pathogens (influenza and RSV) - as well as to common-coronaviruses (CoVs, strains: OC43, 229E, HKU1 and NL63)18,19. While no difference was observed in overall IgG levels (Supplemental Figure 12), these findings point to a significantly expanded Fc-receptor binding humoral antibody repertoire among severe MIS-C cases, but not in severe acute adult cases (Figure 5E and Supplemental Figure 11). In the absence of hypergammaglobulinemia, this points to a significant non-specific amplification of functional pathogen-specific IgG driven immunity, able to drive broad inflammation in severe MIS-C. Together these data argue for a generalized dysregulated pro-inflammatory IgG-response to SARS-CoV-2 and beyond in severe MIS-C.
Discussion
The unpredictable nature of SARS-CoV-2 disease severity is alarming, with severe acute-disease emerging in adults and a KD-like Multisystem-Inflammatory Syndrome in Children8. In the absence of therapeutics able to reverse these clinical manifestations, understanding the immunological mechanisms that underlie these unusual complications of SARS-CoV-2 infection may provide critical insights for the design and delivery of therapeutics for these unique populations. Here we note divergent, but unique humoral immune profiles among mild symptomatic children/young adults and children with severe MIS-C that implicate distinct humoral immune functions in disease pathology. The induction of SARS-CoV-2-specific IgA responses, linked to neutrophil activation, was enriched in severely ill adults, but was less pronounced in the humoral immune response in children and mildly affected adults. Conversely, children that developed MIS-C exhibited persistent, enhanced Fc-receptor binding antibodies, capable to recruit monocytes in a selective manner.
Beyond the pivotal role of IgG mediated functions, IgA is the most highly produced antibody isotype in the body (66 mg/kg/day), and while highly enriched at mucosal surfaces20, serum IgA has emerged as a highly potent activator of innate immune effector function21. In the blood, immune complexes including IgA interact with FcαR, constitutively expressed on neutrophils, but also upregulated on several mucosal immune cell subsets. While neutrophils also express Fc-receptors for IgG, both IgA and IgG result in different neutrophil functions, where IgG drives phagocytosis and cytokine secretion and IgA can augment these functions and additionally drive robust degranulation, cytokine secretion, and NETosis22. Along these lines, depletion of both IgG and IgA in severely affected adults resulted in attenuated neutrophil activation, however, the depletion of IgA resulted in more robust attenuation of tertiary degranulation and cytokine release. Thus, in addition to IgG, elevated IgA levels, observed in adults with more severe disease23 may be linked to enhanced disease severity via the recruitment of FcαR driven inflammatory cascades downstream of phagocytosis (Figure 1 and Supplemental Figure 1–3). Given the presence of functional IgG, but not IgA responses in both children and adults with mild disease, the data potentially argue that IgG alone may be sufficient to control and contain the infection in mild infection. Our work, exploiting patient derived antibodies and neutrophils derived from healthy individuals, may not recapitulate the full spectrum of the antibody/innate cascade. In fact, significant changes have been noted in the frequency24, distribution25, and function13,14 of neutrophils across the SARS-CoV-2 spectrum of disease. Thus, future studies focused on the autologous interaction of immune complexes and activated innate immune cells may reveal critical insights related to the fully pathological cascade that may tip the response from immunoprotective to immunopathological.
Although IgA could simply represent a biomarker of enhanced viremia in the lung, it is thought to play a critical role in mucosal immunity. However, the potent inflammatory activity of IgA may also contribute to enhanced inflammation and symptomatic disease in adults. Interestingly, sero-surveillance studies in otherwise healthy children have shown that IgA levels increase with age peaking in the late teenage years in the blood26. Conversely, children have been noted to have more severe disease following other respiratory infections including influenza, pertussis, respiratory syncytial virus, and group B streptococci27, hypothesized to be related to the lower capacity to generate IgA. While it is critical to note that children with MIS-C generated SARS-CoV-2 IgA responses, these responses tended to be lower than those observed in adults (Supplemental Figure 1–4). Thus collectively, these data may point to a potentially unexpected pathological role of IgA in adult SARS-CoV-2 infection that may contribute to enhanced disease in the elderly via the over-activation of neutrophil degranulation and inflammation.
Children diagnosed with MIS-C, conversely, exhibited a persistence of functional SARS-CoV-2-specific monocyte-activating antibodies and expanded pan-pathogen FcγR binding antibodies, in the absence of hypergammaglobulinemia (Supplemental Figure 12). Given that monocyte activation and immune-complexes have both been associated with KD disease severity28,29, these data point to potential mechanistic disease associated parallels between KD and MIS-C. Moreover, similar to enhanced FcγR2a binding observed here in MIS-C, FcγR2a, a receptor essential for monocyte phagocytosis30, has been described as a susceptibility locus for KD31. Furthermore, effective IVIG treatment of KD has been linked to direct inhibition of FcγR2a mediated immune-complex activation32,33, further supporting the importance of FcγR binding antibodies in this pediatric disease.
As reported for other MIS-C cases34, none of our mild MIS-C cases had detectable SARS-CoV-2 titers in our hands but experienced more symptoms including a cough compared with severe MIS-C cases (3 out 6 vs. 2 of 11 in severe MIS-C). Conversely, as one would expect from a previous exposure, most of our severe MIS-C cases were seropositive for SARS-CoV-2. Two children lacked SARS-CoV-2 specific antibodies, thus we cannot exclude that these were KD cases. However, most notable was the persistence of SARS-CoV-2 immunity among the severe MIS-C cases over time (Supplemental Figure 10)17, in contrast to emerging reports of rapid humoral waning in both symptomatic and asymptomatic adults35,36. Whether persisting functional-antibodies are the result of sustained viral replication in these children, or related to an aberrant ongoing germinal center reaction, durable specific immune complexes, or a general activation of the humoral immune response remains unclear. Yet, a recent report of non-specific plasmablast expansion in MIS-C, together with elevated levels of IL,6, Il-10 and TNFα, all of which can drive B cell proliferation, support the observed non-specific B cell activation in MIS-C reported here37–39. However, here we did not observe evidence of hypergammaglobulinemia in children with MIS-C or drastic shifts in antibody glycosylation (Supplemental Figure 12), both associated with autoimmune disease and aberrant humoral immunity. Yet, we found elevated responses to several respiratory, common coronaviruses, other pathogens previous associated with KD, or auto-antigens previously linked to aberrant MIS-C19, pointing to a potential overactivated, but not generally enhanced, humoral immune response. Interestingly, IgG1, but not IgM, titers were expanded in children with severe MIS-C, potentially indicating a predominant reactivation of previously primed B cells, rather than the elicitation of novel B cell responses. Moreover, expanding IgG1 and FcγR titers were highly correlated indicating a generalized more pro-inflammatory potential within the humoral immune response, similar to the response typically observed following a secondary recall response. Given our emerging appreciation for the presence of virus in distal tissues, including the heart and kidney, it is possible that these persisting overactive antibodies may drive tissue-localized macrophage or monocyte activation within these sites, contributing to disease activity. Given the cross-sectional nature of this study, precise insights into the mechanism of sustained inflammatory antibody production remains unclear. Emerging longitudinal studies will provide key insights into the specific events that drive B cell activation as well as the precise antibody specificities that may contribute to tissue damage and pathology.
Taken together, our findings suggest that IgA and monocyte-activating antibodies play an unexpected pathological role in COVID-19 and MIS-C, respectively. Given the low probability that children are exposed to less virus that might cause milder disease in this population, the data argue that severity of disease may be linked to the reduced IgA responses in youth. Conversely, monocyte-activating IgG that exhibit enhanced and persistent Fc-receptor binding capacity, rather than IgA, in MIS-C, may contribute to organ-attack via the recognition of SARS-CoV-2 or other pathogen or auto-antigens. Thus overall, comparisons of humoral immunity in children provide clues related to the potential pathological functions of antibodies following SARS-CoV-2 infection.
Material and Methods
Cohort
Plasma samples were obtained from pediatric and adult patients at Massachusetts General Hospital under the Institutional Review Board (IRB)-approved MGH Pediatric COVID-19 Biorepository (#2020P000955). Additionally, plasma samples from adult patients were collected under the IRB-approved ‘MGH COVID-19 Biorepository’ (#2020P000804) and ‘Biorepository for Samples from those at increased risk for or infected with SARS-CoV-2’ (#2020P000849). Informed consent, and assent when appropriate, were obtained in accordance with IRB guidelines, by the patients or parent/guardian, prior study enrollment. Informed consent of the pediatric cohort included approval to publish results from research studies using patient’s de-identified samples. A detailed description of the pediatric cohort characteristics was previously published3,40. Patients were diagnosed with COVID-19 related symptoms and positive PCR and/or serology for SARS-CoV-2. MIS-C was diagnosed according to CDC criteria. Severe MIS-C was defined by presence of hypotension or cardiac abnormalities that required intervention including steroids, IVIG and/or anakinra (Supplemental Table 2). All analyzed samples were taken before treatment with IVIG. If not stated otherwise only one timepoint per individual was available and blood was drawn during visit in the outpatient clinic for mild (adult cohort was collected 0–52 days after symptom onset, median = 7 days; and the pediatric cohort collected 0–21 days after symptom onset, median = 3 days) and convalescent cases (11–38 days after symptom onset, median = 27days) or as regular blood collection during hospital stay for the severe COVID (10–37 days after symptom onset, median = 16 days) and MIS-C cases (2–23 days after MIS-C symptom onset, median = 3 days) (Supplemental Table 1). This study was approved by the MGH Human Subjects Institutional Review Board.
Antigens and biotinylation
The receptor binding domains (RBD) of SARS2-CoV-2 and coronavirus strains NL63, HKU1, OC43 and 229 were generously provided by Aaron Schmidt. SARS2-CoV2-S was provided by LakeLake Pharma Inc. SARS2-CoV2-NC (Aalto Bio Reagents Ltd), Flu HAs and EBV p18 (both ImmuneTech Corp), RSV postF (was generously provided from Barney Graham), Measles (Bio-Rad Laboratories), Endogenous retrovirus-W antigen and TSPO (both from Abnova), Pertussix toxin (List Biological Laboratories) CD105 (Novus Biological) and RBPJK (OriGene) were purchased from the different vendors.
If indicated, antigens were biotinylated using Sulfo-NHS LCLC biotin (Thermo Fisher) and excessive biotin removed with ZebaSpin desalting colums (7KDa cut-off, Thermo Fisher).
IgG subclass, isotype and FcγR binding
Antigen specific antibody subclass and isotypes, and FcγR binding was further analyzed by Luminex multiplexing. The antigens were coupled to magnetic Luminex beads (Luminex Corp, TX, USA) by carbodiimide-NHS ester-coupling with an individual region per antigen. Coupled beads were incubated with different plasma dilutions (between 1:100 and 1:1,000 depending on the secondary reagent) for 2 hours at room temperature in 384 well plates (Greiner Bio-One, Germany). Unbound antibodies were washed away and subclasses, isotypes were detected with a respective PE-conjugated antibody at a 1:100 dilution (SouthernBiotech, AL, USA, see Life Sciences Reporting Summary). For the FcγR binding a respective PE-Streptavidin (Agilent Technologies, CA, USA) coupled recombinant and biotinylated human FcγR protein was used as a secondary probe. After 1 h incubation, excessive secondary reagent was washed away and the relative antibody concentration per antigen determined on an IQue analyzer (IntelliCyt). Samples were defined seropositive when they had detectable titer (by Luminex) for IgG1, IgM, and/or IgA1 and a negative cut-off was defined as the average value of SARS-CoV-2 negative samples plus five times the standard deviation. Luminex results for IgG1 were validated by RBD-IgG ELISA as previously described (Supplemental Figure 13)41.
ADCD
Antibody-Dependent-Complement-Deposition was assessed as described before42. In brief, biotinylated antigen was coupled to fluorescence Neutravidin beads (Thermo Fisher). Plasma antibodies were diluted 1:10 in 0.1% BSA and incubated with the coupled antigen beads for 2h at 37°C. Beads were washed and incubated with complement factors from guinea pig for 20 minutes at 37°C. The complement reaction was then stopped by washing with 15mM EDTA in PBS. C3 deposition on the beads was detected with a 1:100 diluted FITC conjugated anti-guinea pig C3 polyclonal antibody (MP Biomedical) and relative C3 deposition was analyzed by flow cytometry.
ADNP
For antibody-Dependent Neutrophil Phagocytosis HL-60 cells were differentiated into neutrophils in media containing 1.2 % DMSO for seven days. On the day of the assay, biotinylated antigens were incubated with Neutravidin beads and immune complexes formed by incubation with 1:100 diluted plasma for 2h at 37°C in 96 well plates (Greiner Bio-One). Differentiated HL-60 cells were added afterwards and incubated for 20h at 37°C. Neutrophils were surface stained against CD11b (1:100, BD Bioscience, clone: ICRF44), fixed with 4% para-formaldehyde and analyzed on a iQue flow cytometer. Phagocytosis score calculated as the product of frequency bead positive CD11b neutrophils and bead fluorescent intensity using ForeCyt Standard Edition 8.1 software (Supplemental Figure 14).
ADCP
THP-1 monocyte phagocytosis was performed as described43. Briefly, biotinylated antigens were conjugated to Neutravidin beads and incubated with 1:100 diluted plasma samples. THP-1 monocytes (0.25M cells/well) were added to the immune complexes and incubated for 16h at 37°C, fixed with 4% para-formaldehyde and analyzed by flow cytometry (Supplemental Figure 14).
Plasma IgA and IgG depletion
IgA and or IgG was depleted from human plasma samples using CaptureSelect™ IgA Affinity Matrix and IgG was depleted with Protein A/G Agarose (Thermo Fisher). The capture matrices were washed three times with PBS and incubated over night with 1:5 diluted plasma samples in a low protein binding MultiScreen® filter plate (Millipore). Depleted plasma was recovered by centrifugation of the filter plate and depletion confirmed by ELISA. Non-depleted plasma was treated similarly but without affinity matrix.
Primary neutrophil ADNP
Neutrophil phagocytic activity of IgA depleted plasma samples was tested on primary human neutrophils44. Biotinylated antigens were coupled to fluorescent neutravidin beads (Thermo Fisher) and incubated 1:100 diluted plasma. Primary neutrophils were incubated with immune complexes for 1h at 37°C. Next, cells were stained for surface CD66b expression with a 1:100 diluted antibody (Biolegend, CA, USA; clone: G10F5), fixed with 4% paraformaldehyde, analyzed by flow cytometry, and phagocytosis score calculated as described above (Supplemental Figure 14).
Secondary Neutrophil assays
Blood neutrophils of healthy donors were isolated using EasySep™ Direct Human Neutrophil Isolation Kit (Stemcell Technologies). Neutrophils were stimulated with bead based immune-complexes and supernatants harvested after 4 hours. Supernatants were diluted 1:5 and release of MPO (Thermo Fisher), MMP9 and Lactoferrin (Abcam) were measured using the Human Elisa Kits according to manufacturer’s instructions. Cytokines were detected in undiluted supernatant using custom-made multiplex cytokine kit (Thermo Fisher).
Plasma isotype ELISA
Plasma IgG, IgM and IgA concentrations were analyzed by ELISA. Respective goat anti-human capture antibody against IgG, IgM or IgA (5 μg/ml) (all Bethyl Laboratories, see Life Sciences Reporting Summary) were coated to an MaxiSorp 384 well ELISA plates (Thermo Fisher). Unspecific binding sites were blocked with 5% BSA. Plasma samples were diluted 1:500,00 for IgG and 1:50,000 for IgM and IgA. After sample incubation IgG, IgM or IgA was probed with 1:10,000 of HRP conjugated goat anti-human IgG, IgM or IgA antibody (all Bethyl Laboratories). The ELISA was developed with 3,3’,5,5’-Tetramethylbenzidine (TMB, Thermo Fisher) and reaction stopped with sulfuric acid. The absorbance was acquired at 450/570nm on a Tecan infinite M1000pro plate reader and Tecan-i-control V.3.4.2 software (both Biotek Instruments). Concentrations were calculated from a two-fold serial dilution curve pooled normal IgG (Bethyl Laboratories, see Life Sciences Reporting Summary) or IgM (Sigma-Aldrich) starting at 125 ng/ml.
IgG-Fc glycosylation
Plasma samples were diluted 1:10 with PBS and incubated overnight at 4°C with magnetic Protein G beads (Millipore). Fab fragments were enzymatically separated from the ProteinG bound Fc parts using IdeZ (NEB). IgG-Fc glycans were released from the protein and APTS labeled with GlycanAssure APTS Kit (Thermo Fisher) and analyzed on 3500xL Genetic Analyzer (Thermo Fisher) capillary electrophoresis instrument. Glycans were assigned based on retention times of known standard glycans with the Glycan Acquisition Software Version 3500 V1.0.3 as described before45.
Computational analysis
Microsoft Excel 365 was used to compile experimental data and patient information. For each paired group, we collected all the measurements from Luminex, functional profiling, and neutralization antibody assays; we eliminated features with missing values across samples. As a quality filter we required features to have values across samples greater than 65% compared to PBS control. The filtered data from Luminex were log transformed by log10 function and all the selected features were scaled and centered.
To visualize relationships between measurements and labels qualitatively, we employed UMAP46 based methods to compress this high-dimensional serological data into a two-dimensional space. First principle components (PCs) that explain more than 90% of the variance were extracted by principal component analysis (PCA)47 using the ‘prcomp’ function in R package ‘stats’ (v.4.0.3). Next, the selected PCs were mapped into a two-dimensional space through the UMAP technique implemented using the R package ‘umap’ (v.0.2.7.0) with fine-tuning parameters (neighbor = 10, min.dist = 0.1).
Classification models were trained to distinguish different paired groups with a minimal set of features. First, we applied the least absolute shrinkage and selection operator (LASSO) feature selection algorithm, to extract significant features48. We ran LASSO 10 times on the whole dataset and identified the features chosen in more than 80% of the repetitions, which were implemented in the function ‘select_lasso’ in systemseRology R package (v.1.0) (https://github.com/LoosC/systemsseRology). A Partial Least-Squares Discriminant Analysis (PLS-DA) classifier was then trained using the extracted features. Model performance was evaluated by five-fold cross-validation, and negative control models were constructed from permuted data with multiple iterations. The permuted control models were generated 20 times by shuffling labels randomly for each repetition. Predicted and true outcomes were compared to determine cross-validation accuracy. The exact P values were calculated as the tail probability of the true value within the control distributions. For PLS-DA we used the ‘opls’ function in ropls R package (v.1.22.0) for classification and functions in systemsseRology R package for the purpose of visualization.
We used correlation networks to visualize the additional humoral immune features significantly associated with the selected minimal features, offering enhanced insights of biological mechanisms. Antibody features that were significantly (p value < 0.05) correlated with a Benjamini-Hochberg correction to the final selected PLS-DA features were defined as co-correlates. Significant spearman correlations about a threshold of |r| > 0.7 were visualized within the networks.
For implementation, spearman correlation coefficients were calculated using ‘rcorr’ function in ‘Hmisc’ package (v4.4.2) and the p values were corrected by ‘Benjamini-Hochberg’ correction in ‘stats’ package (v.4.0.3). Finally, The correlation networks were properly lay-outed and visualized using ‘ggraph’ (v.2.0.4) and ‘igraph’ (v1.2.6) packages with later manual adjustment using Adobe Illustrator (v2020).
Statistical analysis
If not stated otherwise, we assumed non-normal distributions and violin plots were generated and statistical differences between two groups were calculated using a two sided Mann Whitney test. Solid lines in the violin plot indicate 25th or 75th quartile and dashed line the median value. To compare multiple groups, a Kruskal-Wallis test was used with a Dunnett test correcting for multiple comparisons in Graph Pad Prism V.8 (significance levels: *:p<0.05, **:p<0.01, ***:p<0.001, ****:p<=0.0001). Flower plots were visualized with the ggplot package (v.0.7) and correlation chord diagrams were plotted using circlize package (v.0.4.1) in R (v.4.0.1) and R Studio (v.1.3) and the average of the Z-scored data per variable and group is shown.
Life Sciences Reporting Summary
Additional information about this study is available in the Life Sciences Reporting Summary which is published online along with this paper.
Supplementary Material
Acknowledgement
LMY received funding from the National Heart Lung and Blood Institute (5K08HL143183), and the Cystic Fibrosis Foundation (YONKER18Q0). DAL was partially supported by the National Institute for Allergy and Infectious Disease (U19 AI135995). NIH R01 AI146779 and a Massachusetts Consortium on Pathogenesis Readiness(MassCPR) was awarded to AGS. We thank Nancy Zimmerman, Mark and Lisa Schwartz, an anonymous donor (financial support), Terry and Susan Ragon, and the SAMANA Kay MGH Research Scholars award for their support. We would also like to thank Yongfei Cai and Bing Chen for S protein production efforts and Jared Feldman, Blake Marie Hauser, Tim Caradonna and Aaron Schmidt for generating receptor binding domain antigens. We acknowledge support from the Ragon Institute of MGH, MIT, the Massachusetts Consortium on Pathogen Readiness (MassCPR), the NIH (3R37AI080289-11S1), “Immune Response to Pathogens” (2007P002451), Centers for Disease Control and Prevention U01CK000490, NIH SeroNet U01CA260476, and the Gates foundation Global Health Vaccine Accelerator Platform funding (OPP1146996). We would also like to thank Dr. Xu Yu, Alicja Piechocka-Trocha, and Kristina Lefteri for their support on the collection and processing of adult MassCPR cohorts.
Footnotes
Conflict of interest
Galit Alter is a founder of Seromyx Systems Inc, a company developing platform technology that describes the antibody immune response. Dr. Alter’s interests were reviewed and are managed by Massachusetts General Hospital and Partners HealthCare in accordance with their conflict of interest policies. All other authors have declared that no conflict of interest exists.
Code availability statement
There was no specific custom code used in this manuscript. All code is publicly available, and the source indicated in the text and/or methods section. Scripts will be made available upon request.
Data availability statement
All relevant data are included in this manuscript. Source data are provided with this paper.
References
- 1.CDC-Covid-Response-Team. Coronavirus Disease 2019 in Children - United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep 69, 422–426, doi: 10.15585/mmwr.mm6914e4 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bi Q et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis, doi: 10.1016/S1473-3099(20)30287-5 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yonker LM et al. Pediatric SARS-CoV-2: Clinical Presentation, Infectivity, and Immune Responses. J Pediatr, doi: 10.1016/j.jpeds.2020.08.037 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braun J et al. SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19. Nature, doi: 10.1038/s41586-020-2598-9 (2020). [DOI] [PubMed] [Google Scholar]
- 5.Ladner JT et al. Epitope-resolved profiling of the SARS-CoV-2 antibody response identifies cross-reactivity with an endemic human CoV. bioRxiv, doi: 10.1101/2020.07.27.222943 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verdoni L et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet 395, 1771–1778, doi: 10.1016/S0140-6736(20)31103-X (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N & Theocharis P Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 395, 1607–1608, doi: 10.1016/S0140-6736(20)31094-1 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feldstein LR et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med 383, 334–346, doi: 10.1056/NEJMoa2021680 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belhadjer Z et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation, doi: 10.1161/CIRCULATIONAHA.120.048360 (2020). [DOI] [PubMed] [Google Scholar]
- 10.Zohar T & Alter G Dissecting antibody-mediated protection against SARS-CoV-2. Nat Rev Immunol 20, 392–394, doi: 10.1038/s41577-020-0359-5 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atyeo C et al. Distinct Early Serological Signatures Track with SARS-CoV-2 Survival. Immunity, doi: 10.1016/j.immuni.2020.07.020 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamre R, Farstad IN, Brandtzaeg P & Morton HC Expression and modulation of the human immunoglobulin A Fc receptor (CD89) and the FcR gamma chain on myeloid cells in blood and tissue. Scand J Immunol 57, 506–516, doi: 10.1046/j.1365-3083.2003.01220.x (2003). [DOI] [PubMed] [Google Scholar]
- 13.Veras FP et al. SARS-CoV-2-triggered neutrophil extracellular traps mediate COVID-19 pathology. J Exp Med 217, doi: 10.1084/jem.20201129 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laforge M et al. Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat Rev Immunol 20, 515–516, doi: 10.1038/s41577-020-0407-1 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Witko-Sarsat V, Rieu P, Descamps-Latscha B, Lesavre P & Halbwachs-Mecarelli L Neutrophils: molecules, functions and pathophysiological aspects. Lab Invest 80, 617–653, doi: 10.1038/labinvest.3780067 (2000). [DOI] [PubMed] [Google Scholar]
- 16.Zuo Y et al. Neutrophil extracellular traps in COVID-19. JCI Insight 5, doi: 10.1172/jci.insight.138999 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weisberg SP et al. Distinct antibody responses to SARS-CoV-2 in children and adults across the COVID-19 clinical spectrum. Nat Immunol, doi: 10.1038/s41590-020-00826-9 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Menikou S, Langford PR & Levin M Kawasaki Disease: The Role of Immune Complexes Revisited. Front Immunol 10, 1156, doi: 10.3389/fimmu.2019.01156 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Consiglio CR et al. The Immunology of Multisystem Inflammatory Syndrome in Children with COVID-19. Cell, doi: 10.1016/j.cell.2020.09.016 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fagarasan S & Honjo T Intestinal IgA synthesis: regulation of front-line body defences. Nature reviews. Immunology 3, 63–72, doi: 10.1038/nri982 (2003). [DOI] [PubMed] [Google Scholar]
- 21.Woof JM & Kerr MA IgA function--variations on a theme. Immunology 113, 175–177, doi: 10.1111/j.1365-2567.2004.01958.x (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aleyd E et al. IgA enhances NETosis and release of neutrophil extracellular traps by polymorphonuclear cells via Fcalpha receptor I. J Immunol 192, 2374–2383, doi: 10.4049/jimmunol.1300261 (2014). [DOI] [PubMed] [Google Scholar]
- 23.Yu HQ et al. Distinct features of SARS-CoV-2-specific IgA response in COVID-19 patients. Eur Respir J, doi: 10.1183/13993003.01526-2020 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Y et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect 81, e6–e12, doi: 10.1016/j.jinf.2020.04.002 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnes BJ et al. Targeting potential drivers of COVID-19: Neutrophil extracellular traps. J Exp Med 217, doi: 10.1084/jem.20200652 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weemaes C et al. Development of immunoglobulin A in infancy and childhood. Scand J Immunol 58, 642–648, doi: 10.1111/j.1365-3083.2003.01344.x (2003). [DOI] [PubMed] [Google Scholar]
- 27.Pattemore PK & Jennings LC Chapter 31 - Epidemiology of Respiratory Infections. 435–452 (2008). [Google Scholar]
- 28.Takahashi K, Oharaseki T, Yokouchi Y, Hiruta N & Naoe S Kawasaki disease as a systemic vasculitis in childhood. Ann Vasc Dis 3, 173–181, doi: 10.3400/avd.sasvp01003 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mason WH, Jordan SC, Sakai R, Takahashi M & Bernstein B Circulating immune complexes in Kawasaki syndrome. Pediatr Infect Dis 4, 48–51, doi: 10.1097/00006454-198501000-00012 (1985). [DOI] [PubMed] [Google Scholar]
- 30.Richards JO et al. Optimization of antibody binding to FcgammaRIIa enhances macrophage phagocytosis of tumor cells. Mol Cancer Ther 7, 2517–2527, doi: 10.1158/1535-7163.MCT-08-0201 (2008). [DOI] [PubMed] [Google Scholar]
- 31.Khor CC et al. Genome-wide association study identifies FCGR2A as a susceptibility locus for Kawasaki disease. Nat Genet 43, 1241–1246, doi: 10.1038/ng.981 (2011). [DOI] [PubMed] [Google Scholar]
- 32.Nagelkerke SQ et al. Inhibition of FcgammaR-mediated phagocytosis by IVIg is independent of IgG-Fc sialylation and FcgammaRIIb in human macrophages. Blood 124, 3709–3718, doi: 10.1182/blood-2014-05-576835 (2014). [DOI] [PubMed] [Google Scholar]
- 33.Abe J et al. Gene expression profiling of the effect of high-dose intravenous Ig in patients with Kawasaki disease. J Immunol 174, 5837–5845, doi: 10.4049/jimmunol.174.9.5837 (2005). [DOI] [PubMed] [Google Scholar]
- 34.Shana Godfred-Cato D et al. COVID-19–Associated Multisystem Inflammatory Syndrome in Children — United States, March–July 2020. MMWR Morb Mortal Wkly Rep 69, 1074–1080, doi: 10.15585/mmwr.mm6932e2externalicon (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ibarrondo FJ et al. Rapid Decay of Anti-SARS-CoV-2 Antibodies in Persons with Mild Covid-19. N Engl J Med, doi: 10.1056/NEJMc2025179 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Long QX et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med 26, 1200–1204, doi: 10.1038/s41591-020-0965-6 (2020). [DOI] [PubMed] [Google Scholar]
- 37.Gruber CN et al. Mapping Systemic Inflammation and Antibody Responses in Multisystem Inflammatory Syndrome in Children (MIS-C). Cell, doi: 10.1016/j.cell.2020.09.034 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diorio C et al. Multisystem inflammatory syndrome in children and COVID-19 are distinct presentations of SARS-CoV-2. J Clin Invest, doi: 10.1172/JCI140970 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carter MJ et al. Peripheral immunophenotypes in children with multisystem inflammatory syndrome associated with SARS-CoV-2 infection. Nat Med, doi: 10.1038/s41591-020-1054-6 (2020). [DOI] [PubMed] [Google Scholar]
- 40.Lima R et al. Establishment of a Pediatric COVID-19 Biorepository: Unique Considerations and Opportunities for Studying the Impact of the COVID-19 Pandemic on Children. Res Sq, doi: 10.21203/rs.3.rs-42030/v1 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roy V et al. SARS-CoV-2-specific ELISA development. J Immunol Methods 484–485, 112832, doi: 10.1016/j.jim.2020.112832 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fischinger S et al. A high-throughput, bead-based, antigen-specific assay to assess the ability of antibodies to induce complement activation. J Immunol Methods 473, 112630, doi: 10.1016/j.jim.2019.07.002 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ackerman ME et al. A robust, high-throughput assay to determine the phagocytic activity of clinical antibody samples. J Immunol Methods 366, 8–19, doi: 10.1016/j.jim.2010.12.016 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karsten CB et al. A versatile high-throughput assay to characterize antibody-mediated neutrophil phagocytosis. J Immunol Methods 471, 46–56, doi: 10.1016/j.jim.2019.05.006 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mahan AE et al. A method for high-throughput, sensitive analysis of IgG Fc and Fab glycosylation by capillary electrophoresis. J Immunol Methods 417, 34–44, doi: 10.1016/j.jim.2014.12.004 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McInnes L, Healy J & Melville J UMAP: Uniform Manifold Approximation and Projection for Dimension Reduction. arXiv preprint (2018). [Google Scholar]
- 47.Wold S, Esbensen K & Geladi P Principal component analysis. Chemometrics and Intelligent Laboratory Systems 2, 37–52, doi: 10.1016/0169-7439(87)80084-9 (1987). [DOI] [Google Scholar]
- 48.Tibshirani R Regression shrinkage and selection via the lasso: a retrospective. J. R. Statist. Soc. B 73, 273–282 (2011). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are included in this manuscript. Source data are provided with this paper.


