Abstract
Background/aims
Despite the proven benefits of vaccine prevention and the continuous development of this important public health measure, vaccine hesitancy is among the top ten threats to global health according to the World Health Organization in 2019. Those who contract the influenza virus will typically develop a mild illness. However, for populations at a higher risk, including those diagnosed with dementia, influenza is proven to be more detrimental. Persons with dementia (PWD) face a serious threat to influenza on an annual basis, and vaccine hesitancy may further potentiate this risk. The purpose of this paper is to explore and understand the barriers PWD face in receiving the influenza vaccine.
Methods
A literature review was conducted to examine the barriers that prevent PWD from seeking out the annual influenza vaccine. A thematic analysis provided an understanding of the overarching relationships found among the influences between the identified themes.
Results
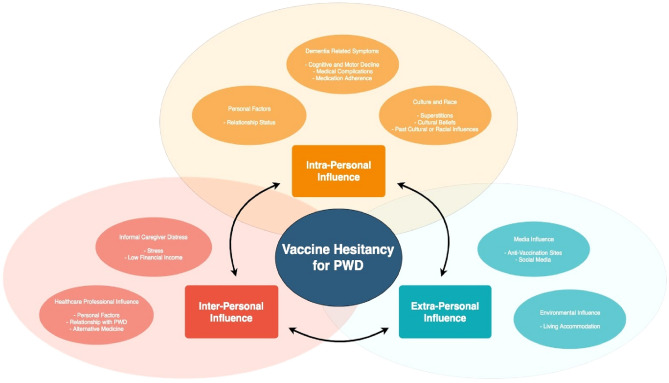
Three main influences were identified: (1) intra-personal, (2) inter-personal, and (3) extra-personal, with each influence containing several subsequent sub-themes.
Discussion/conclusion
The literature review found that there is a lack of research involving this high-risk population and the barriers they face, especially within the extra-personal influences. Further research is required to understand how each barrier relates and connects with each other. Understanding this connection will aid public health organizations in decreasing the threat of vaccine hesitancy, thus decreasing the incidents of preventable deaths.
Keywords: Influenza vaccine, Vaccine uptake, Vaccine hesitancy, Dementia, Barriers, Public health
Introduction
The Center for Disease Control and Prevention (CDC) describes that most individuals affected by influenza will have mild illness [1]. However, for a population that is considered high risk, influenza prevalence is higher, and complications are more detrimental. Cognitive impairment as result of dementia may present major barriers for the individual to fight against infection, thus resulting in an increased likelihood to develop serious complications [2]. In fact, dementia is an independent risk factor for influenza complications and can be especially dangerous as early symptoms of influenza are difficult to recognize in persons with dementia (PWD) [3]. As a result, PWD are hospitalized more frequently and for longer durations [4]. Consequently, due to the higher morbidity rates, individuals with chronic neurological diseases such as dementia also face higher mortality rates. This population is 40 times more likely to die from complications due to influenza than those who are not affected by neurological conditions [2].
The best influenza prevention strategy is receiving the annual vaccine. In Canada, during the 2017/2018 influenza season, the overall adult vaccine coverage was 38.3%, while coverage for the high-risk population of seniors over 65 years of age was 70.7%, which is below the national coverage goal of 80% [5]. Even more specifically, a Canadian study about influenza vaccine uptake showed that approximately 55% of the sample population living with dementia had received the flu vaccine [6]. It is an alarming result as close to half of the participating PWD population had not received the influenza vaccine, despite this population having a greater risk of contracting influenza and its deadly complications [6].
A systematic review of influenza vaccine efficacy for older persons concluded that the influenza vaccine reduces the risk for pneumonia, hospitalization, and death in older persons if the strain of the vaccine is the same or similar to the influenza epidemic strain [7]. The review also discussed that all persons older than 65 should have the influenza vaccine as a part of their care plan, and this requires involvement from informal caregivers, physicians, and public health organizations. Despite these factors posing as motivations for PWD to receive influenza vaccine, uptake among this population is inferior.
Objectives
The objection or rejection of vaccines, despite their availability, is known as vaccine hesitancy [8]. It is evident that PWD have an increased risk for influenza complications. This, coupled with the lack of vaccine uptake specifically in this population, makes the seemingly harmless annual influenza season a deadly threat to PWD. To combat this public health issue of vaccine hesitancy, it is essential to identify and understand the various barriers that this population faces when it comes to accessing the influenza vaccine. The purpose of this literature review is to explore the barriers PWD face in receiving the influenza vaccine.
Methods
A literature review was conducted to examine the barriers PWD face in receiving the influenza vaccination. This included barriers that may be a result of care from informal caregivers (ICs) and health care providers (HCPs). The three concepts used for the initial search were (1) vaccines, (2) dementia, and (3) barriers. Within each concept, there were different keywords used. The vaccine concept used vaccine*, immuniz*, or immunis*; the dementia concept used Alzheimer* or dementia; and the barriers concept used access*, barrier*, or convenien*. A variety of databases were accessed for the search, primarily PubMed, CINAHL, the Ontario Tech University database, and Google Scholar. Each database search consisted of using the same keywords and pairing either two or three of the concepts together. On CINAHL, for example, pairing all three concepts yielded only 22 results, so a broader search of pairing two concepts at the same time was used. Titles and abstracts were first screened for relevance to the research question, and only articles published in English were used. Reference pages from peer-reviewed articles were scanned for relevant resources. Overall, 24 resources were used to conduct a thematic analysis (See Table 1).
Table 1.
Summary table of research studies included in the literature review
| References | Title | Author and date | Study purpose | Study or resource design | Summary of key findings |
|---|---|---|---|---|---|
| [22] | Is performance of influenza vaccination in the elderly related to treating physician’s self-immunization and other physician characteristics? | Abramson and Levi 2008 | To examine the association between physician characteristics including self-immunization status and patient immunization status | Data extraction and Questionnaire |
-Patients were more likely to get vaccinations if the physician was also vaccinated -There were physician characteristics that impacted the likeliness of a patient being immunized: (1) If a physician was a female, (2) If a physician was trained in West Europe or America, (3) If a physician exercised regularly, (4) If physicians understood that the vaccine can’t cause influenza |
| [23] | Seasonal influenza vaccination among homebound elderly receiving home-based primary care in New York City | Banach et al. 2012 | To assess the factors associated with flu shot refusal in community-dwelling elderly that were receiving care urban home-based primary care (HBPC) | Cross sectional |
-For the participants that were eligible for the flu shot, 84% accepted, and 16% denied -Flu shot denial was positively associated with female gender, black race, and living independently. It was negatively associated with dementia |
| [24] | Immunology beliefs as a factors in vaccine opposition among complementary and alternative medical providers | Bean and Catania 2018 | To examine the beliefs that complementary and alternative medical providers have about vaccinations to derive how this may impact parents deciding about vaccinations for their children | Semi-structured interview |
-The beliefs discovered about CAM providers attitudes towards vaccines included “natural is best”, “innate intelligence”, and “the fragile immune system” -CAM providers that also accepted mainstream medicine were more likely to be vaccine supporters. These providers associated with the themes “vaccines prevent illness” and “herd immunity” -CAM providers do provide advice to their patients but often provide the advice as what they would do for their children rather than what the parent should do -The CAM providers that were not vaccine supporters had come to their standpoints through post-grad education that is unregulated |
| [15] | Factors influencing influenza vaccination uptake in an elderly, community-based sample | Burns et al. 2005 | To examine the factors involved in flu shot uptake in the elderly community-dwelling population | Cross sectional interview study |
-The most common reasons given for vaccine refusal were fear and vaccine side effects -Most participants that received the flu shot mentioned it was because of a reminder from a health care provider -Participants that had a health care provider that explained the importance and side effects of the flu shot -Participants that lived with others, had higher occupational status, and had a car or were able to walk to a doctor’s office were the participants with higher rates of flu shot uptake |
| [4] | Dementia in Canada: Summary | Canadian Institute for Health Information 2019 | To present a summary of information about dementia in Canada | Report |
-The number of PWD continues to increase in Canada, and this can be related to the overall increase in an aging population. The number of seniors in Canada is predicted to increase by 68% over the next 20 years -Most seniors with dementia live in the community -PWD over 65 years old are hospitalized more frequently and for longer durations. This makes them more susceptible to hospital acquired harm including UTIs, pneumonia, and falls. They also wait longer in emergency departments -Approximately 1 in 4 Canadians over 85 years old have been diagnosed with dementia -Canadians with young-onset dementia are more likely to experience stigma related to the disease |
| [14] | The effect of patient characteristic upon uptake of the influenza vaccination: A study comparing community-based older adults in two healthcare systems | Crawford et al. 2011 | To examine the relationship between flu shot uptake and community-dwelling patient characteristics for two differently structured healthcare systems | Interviews |
-Uptake rates were higher than set community targets -Flu shot uptake is higher in older age, widowhood, greater functional impairment, and for those who have greater use of services such as chiropody, meals-on-wheels, social work, and occupational therapy -Increased exposure to health care services may positively impact flu shot uptake rates |
| [29] | The overlooked dangers of anti-vaccination groups social media presence | Evrony and Caplan 2017 | To draw attention to and provide information about well-developed and highly visible antivaccination websites that provide the public with information that is not scientifically supported | Research Article |
-Outbreaks are becoming increasingly common due to lowered vaccination rates, and this is partially due to antivaccination online resources that have strong visibility in the online community -A Voice for Choice in an antivax website that claims to provide evidence-informed information for users to then make evidence-informed decisions, but it is actually an anti-vax website that does not support their claims with scientific research -A Voice for Choice provides information about vaccine ingredients and harms that are not backed with scientific rigour. This website promotes debunked myths and encourages individuals to blog about vaccine adverse effects |
| [3] | Dementia diagnosis and influenza vaccination in French nursing home residents | Gallini et al. 2015 | To investigate the impact dementia status has on flu shot uptake in nursing home residents | Cross-sectional study |
-The nursing home that was included in this study exceeded the WHO goals for flu shot rates for seniors (> 75%) and 89.9% of their residents were vaccinated -Residents with dementia were more likely to have received a flu shot than those without dementia, and this is consistent with UK and US studies -Authors discussed the reasons for these findings as the recognition by nursing staff that dementia is an independent risk factor for influenza complications -Another reason for the increased rate in flu shot uptake in PWD was that PWD and associated family members were less likely to have been asked permission to get the vaccine. As a result, they were less likely to have had the option to refuse |
| [17] | Under the shadow of Tuskegee | Gamble 1997 | To provide social context to the Tuskegee Syphilis Study | Research paper |
-The Tuskegee Syphilis Study continues to impact African American’s trust in western medicine practices -The Tuskegee Syphilis Study led to discussion about informed consent, communication of diagnosis, and accurate reporting of test results -African American men were not told about the length of the study (told 6 months but actually lasted 40 years) or that they would not actually be treated after funding was lost |
| [20] | Caregiver Distress Report—The Reality of Caring | Health Quality Ontario 2016 | To report findings on caregiver distress associated with long-stay home care residents | Report |
-In 2013/14, among the 97% of home-care residents that received care from informal caregivers (ICs), 33% of the ICs reported caregiver distress. This number doubled from the 2009/10 data -There was more distress seen for ICs looking after residents with higher levels cognitive impairment, functional disablement, and frailty -The amount Canada relies on ICs is increasing with the aging population |
| [26] | Rural Disparities in Alzheimer’s Disease-Related Community Pharmacy Care in the United States | Henkel and Marvanova 2017 | To examine the relationship between area population density and community pharmacy-based Alzheimer’s Disease-related services including pharmacist’s medication knowledge, immunizations, in-stock cognitive enhancers | Standardized interviews |
-Pharmacists in more rural areas were 50% less likely to offer immunizations -Rural pharmacists were less likely to have cognitive enhancing drugs in stock and were also less likely to name as many adverse effects of medications compared to pharmacists in less rural areas |
| [13] | Evidence of bias in estimated of influenza vaccine effectiveness in seniors | Jackson et al. 2005 | To assess the risk of death from any cause or hospitalization for pneumonia or influenza before, during, and after flu season | Observational |
-Seniors that receive the flu shot are at lower risk of hospitalization and death during flu season -The greatest reductions in risk of death and pneumonia hospitalization were in the time period before flu season when there is no real vaccine effect -Persons with chronic conditions had higher proportions of vaccinated compared to unvaccinated persons. The only exception was dementia |
| [9] | The assessment of language and communication in dementia: A synthesis of evidence | Krein et al. 2019 | To review tools used for the language and communication for persons with dementia | Scoping review |
-Language and communication impairment impact most of the population of persons with dementia -Three tools were identified as valid and were reviewed in depth: Arizona Battery of Communication Disorders in Dementia, Sydney Language Battery, and Addenbrooke’s Cognitive examination |
| [19] | Do superstitions beliefs affect influenza vaccine uptake through shaping health beliefs? | Lu et al. 2019 | To examine the relationship between superstitious beliefs and influenza vaccine uptake | Cross sectional survey |
-Of the participants in Singapore, 60% had never received the flu shot -Superstitious beliefs showed mixed results for flu shot uptake -Superstitious beliefs predicted higher perceived barriers and lower perceived benefits of the flu shot. Both of these factors predicted a lower intent to get the flu shot the next year. However, superstitious beliefs also predicted higher perceived severity and susceptibility of the flu leading to a higher intent to receive the flu shot |
| [18] | Why Blacks do not take part in HIV vaccine trials | Moutsiakis and Chin 2007 | To examine why HIV vaccine trials have a low percent of Blacks | Interviews |
-There were three reasons for HIV vaccine trial hesitancy: (1) misinformation. (2) mistrust and fear, and (3) stigma -If a participant was homosexual or had a close friend with HIV, this increased the likelihood of participating in an HIV vaccine trial |
| [10] | Pneumonia and influenza hospitalizations in elderly people with dementia | Naumova et al. 2009 | To examine the relationship between healthcare accessibility and pneumonia and influenza by looking at demographic and geographic patterns of PWD hospitalization in comparison to the US population | Observational study |
-Rural and poorer areas had higher rates of pneumonia and influenza -PWD had a lower number of influenza diagnoses, shorter hospital stays, and 1.5 times as high a death rate when compared to the national average |
| [12] | Behavioral, psychological and physical symptoms in group homes for older adults with dementia | Onishi et al. 2006 | To compare symptoms of persons with dementia living in group homes vs. nursing homes vs. long-term care homes | Questionnaires |
-The most common symptoms in group homes were as follows: requests/desire to go home, UTIs, general complaints -Level of coping was worst in LTC homes -Anxiety, depression, and disorientation were frequently found in all three settings |
| [25] | Shah et al. 2011 | To examine the relationship between dementia diagnosis and flu shot uptake in community and care home residents in England and Wales | Retrospective Analysis |
-There is less uptake in residents that live at home compared to those living in home care facilities -The difference in uptake with home care vs. care home residents shows organizational barriers may be a factor with it being harder for home care residents to access all services at home -consent does not seem to be a factor in accessibility of flu shot with care home residents |
|
| [27] | Why do parents decide against immunization? The effect of health beliefs and health professionals | Smailbegovic et al. 2003 | To examine vaccine and vaccine-preventable infection knowledge, attitudes, and concerns of parents whose children have not completed the recommended immunizations | Observational, case–control study (Questionnaire & Interviews) |
-MMR and meningitis C were most frequently omitted vaccines with primary concern being vaccine safety -34% of parents expressed concern about the side effects of vaccines being more dangerous than the vaccine-preventable infection -Of the respondents that were interviewed, it was reported that the information provided by health professionals about vaccines is poor |
| [11] | A systematic review of medication non-adherence in persons with dementia or cognitive impairment | Smith et al. 2017 | To compile research that examined medication adherence in PWD and cognitive impairment | Systematic Review |
-Individuals with cognitive impairment have adherence rates of 10.7–38% which is lower compared to individuals without cognitive impairment -The definition of medication adherence is broadly defined, and multiple factors were considered impactful in medication adherence |
| [16] | Cultural Perspectives on Vaccination | The College of Physicians of Philadelphia 2018 | To provide information about cultural perspectives on vaccines | Website article |
-Cultural perspectives on vaccines often stem from religious standpoints, suspicion and mistrust, and rights surrounding vaccines -Religious standpoints can be based on ethical dilemmas with the products used in vaccines and/or what should be put in to the sacred human body along with the belief that healing should come from God or natural means -Suspicion and mistrust of vaccines may stem from “Western plot” theories or the history of inequality in healthcare and research |
| [21] |
Caregiver psychological distress as a barrier to influenza vaccination among community-dwelling elderly with dementia |
Thorpe et al. 2006 | To examine if informal caregiver distress decreased the likeliness of PWD receiving a flu-shot. The secondary aim was to examine how psychological distress affected other medical need variables or vaccines | Data retrieved from a National Longitudinal Survey and then multivariate variables were observed |
-Caregiver distress was associated with decreased likeliness of flu-shot -Out of 1406 care-recipients, 503 received flu shot -29.7% of caregivers were distressed -Likelihood of having distressed caregiver was higher in unvaccinated recipients -Unvaccinated recipients were more likely to exhibit ADL and IADL limitations, higher level dementia-related behavioural problems -Unvaccinated recipients were more likely to have private insurance or Medicaid, live farther away from medical facilities, and have caregivers with lower perceived financial adequacy -Predicted probability of vaccination for non-distress was 37.7%, distress was 29.4% -Greater care-recipient behavioural problems and greater caregiver limitations from comorbidities decreased likelihood of vaccination -Increased social isolation and feelings of hopelessness may interfere with adherence |
| [31] | Content and Design Attributes of Antivaccination Web sites | Wolfe et al. 2002 | To identify and delineate the claims and concerns on antivaccination websites | Metasearch review |
-There were common content claims on antivaccination websites: (1) vaccines cause idiopathic illness; (2) vaccines destroy immunity; (3) vaccine adverse reactions are underreported; and (4) profit drives vaccine policies -Antivaccination websites often included resources on how to get further anti-vax information as well as how to legally avoid vaccines. These websites also regularly used emotive appeals about children that have been harmed or killed by vaccines |
Results
Altogether, we classified the themes among three major influences: (1) intra-personal, (2) inter-personal, and (3) extra-personal. A summary and relationship between these three themes and their sub-themes is presented in Fig. 1. Table 1 presents the details of the contributions from each study, while Table 2 presents a summary chart of each sub-theme.
Fig. 1.
Summary and relationship between the three major influences identified, along with their sub-themes
Table 2.
Summary of findings, including factors of each theme, as well as the negative outcomes that prevent PWD from actively seeking out an influenza vaccine
| Summary of findings | ||
|---|---|---|
| Themes | Factors | Outcomes |
| Dementia-related symptoms |
Cognitive and motor decline Medical complications |
Decreased accessibility Medication adherence |
| Personal factors | Relationship status |
Decreased accessibility Potential misinformation Lack of motivation |
| Culture and ethnicity |
Superstitions Cultural beliefs Past cultural or ethnic influences |
Medication adherence Lack of trust in vaccine and healthcare providers |
| Healthcare professional (HCP) impact |
Personal factors Relationship status with PWD and/or IC Alternative medicine beliefs |
Lack of trust in HCP Lack of positive influence Misinformation |
| Informal caregiver (IC) distress |
Stress Low financial income |
Lack of motivation Decreased accessibility Misinformation |
| Environmental factors | Living accommodation |
Decreased accessibility to healthcare services Potential misinformation |
| Media impact |
Anti-vaccination sites Social media |
Misinformation Lack of trust in vaccine and healthcare providers |
Intra-personal influences include themes that directly relate to the PWD, including dementia-related symptoms, personal factors, and culture and race. Dementia-related symptoms relate to the cognitive and motor decline that PWD experience. As a result of this decline, PWD may have difficulty accessing, understanding, and adhering to the influenza vaccine [9–13]. Personal factors of PWD, specifically marital/relationship status, was a common theme found among the literature [14, 15]. Culture and ethnicity play a role in this public health crisis as cultural traditions, beliefs, and superstitions may influence decisions made by PWD, HCPs, and ICs [16–19]. Some sources discussed how past public health controversies involving minorities continue to create distrust, thus resulting in low influenza vaccine uptake in these specific minority populations [17, 18].
Inter-personal influences extend beyond the PWD, instead involving those who directly aid in their care, primarily IC and HCP. Literature suggests that caregiver distress may influence the decision to seek out a vaccination for the PWD in their care [20, 21]. In a similar way, the financial burden that some ICs experience can influence the accessibility aspect of vaccines [4]. HCP impact refers to all the factors a HCP may possess that can alter the likelihood of a PWD receiving the vaccine. Personal factors for HCPs refer to gender, lifestyle, and immunization status [22, 23]. Additionally, the level of trust between HCP, IC, and PWD was found to be a contributing factor. Finally, the beliefs of complementary and alternative medicine (CAM) providers play an important role in accessing vaccination as they often offer vaccine advice to patients and families [24].
The final major influence is extra-personal, which involves everything beyond those in direct care of the PWD. A common environmental influence was accommodation and accessibility of the vaccine based on living situations [25, 26]. Our research also indicated that media influence was one of the driving factors in vaccine hesitancy [27–31]. With online and social media usage being at an all-time high, finding misinformation and anti-vaccination movements can be easy, thus negatively changing the perception of influenza vaccinations.
Discussion
This literature review revealed the over-arching three types of influences that affect persons with dementia’s access to vaccination of influenza: (1) intra-personal influence (dementia-related symptoms; personal factors; culture and ethnicity); (2) inter-personal influence (informal caregiver distress; healthcare professional impact; and (3) extra-personal influence (environmental factors; media impact). The review of the existing evidence highlighted the gaps in the literature that examined the barriers of access to influenza vaccine and factors related to vaccine hesitancy among persons with dementia.
Intra-personal influence
Dementia-related symptoms
Given that language impairment is among the first cognitive functions to be affected by the onset of dementia, the lack of communication is widespread among PWD [9]. As a result, PWD are unable to access the medical support they require in a timely manner, putting them at an increased risk of hospitalization, complications, and death. One study illustrated that PWD who are hospitalized present more severe conditions and worse outcomes [10]. Another common cognitive deficit experienced by PWD is a decline in memory. Memory loss and difficulty learning contributes to an increase of non-adherence. Researchers found that participants who scored higher on memory tests had greater medication adherence [11] which has implications to PWD’s compliance of receiving annual vaccination. PWD also experience motor decline and have limited access to specialized care and testing practices. Due to motor decline, including bradykinesia and walking disturbances [12], transporting PWD may present as a barrier to access influenza vaccination. Additionally, PWD are more likely to have poor oral hygiene and difficulty swallowing. One study found that these symptoms can increase the risk of developing influenza and consequently the difficulty of treating it [10]. These two factors of cognitive and motor decline together make it extremely difficult for a PWD to seek medical help and access influenza vaccination. Another study conducted in the US explored the percentage of vaccine uptake among seniors with a variety of diagnosed chronic conditions, including heart disease, diabetes, cancer, and dementia [13]. Interestingly, every population with the exception of PWD had a greater proportion of vaccinated than unvaccinated people [13]. As a whole, it is evident that the symptoms of a dementia diagnosis illustrate poor outcomes when it comes to influenza and its vaccine uptake.
Personal factors
Relationship status, specifically widowhood, was another factor found to have an influence on the likelihood of an older adult seeking out the influenza vaccination. Researchers theorized that due to the increased vulnerability of widows, this population may have an increased likelihood of vaccination [14]. On the other hand, it may be possible that due to the increased caregiving and monitoring of PWD, family caregivers often have the assumptions that PWD may not necessarily require to receive the influenza vaccine. Another study found that participants who lived with others were more likely to get the vaccine than those who were living alone [15]. A limitation of this study was that the participants included were recruited randomly from the general populations, which had different characteristics than persons with dementia. Due to these mixed results, it is essential to conduct further research to truly understand how relationship status may affect influenza vaccine uptake. Regardless, it is evident from the existing literature that personal factors play a role in influencing PWD’s access to influenza vaccination.
Culture and ethnicity
Cultural beliefs may impact vaccine uptake. These cultural beliefs are typically based around the usage of human tissue cells in vaccines, with the belief that the body is sacred and should not receive chemicals, blood, or tissues from animals; as well as the idea that God or natural means will heal the body [16]. Further, the distrust of modern medicine can stem from historical and social inequality and mistrust. This is displayed by the African Americans’ distrust in medical treatments, including vaccination, after being denied appropriate treatment during the Tuskegee Syphilis study [17]. Another study also indicated that Black populations were more likely to refuse the vaccine, expressing concerns about vaccine safety and efficacy [18].
Lu et al. [19] studied how superstitious beliefs may specifically impact influenza vaccine uptake in Singapore. It was found that superstitions do have an impact on flu vaccine uptake. However, the impacts were mixed. Superstitious beliefs led to a predicted lower uptake because of higher perceived barriers and lower perceived benefits of vaccines. In contrast, some superstitious beliefs led to a higher uptake because of higher perceived susceptibility and severity of influenza. The impact of intra-personal factors has implications about persons with dementia’s vaccine uptake, and future health education about vaccination should take into considerations about factors related to personal beliefs, cultural background, and ethnicity.
Inter-personal influence
Informal caregiver distress
Health Quality Ontario reports an ongoing increase in caregiver distress [20], and this may impact vaccine uptake. Caregiver distress refers to the stress and exhaustion some ICs feel due to the responsibility of caring for a PWD. Thorpe et al. examined caregiver psychological distress as a barrier to influenza vaccination uptake in community-dwelling PWD [21]. From a sample of 1406 PWD who were male veterans, and their corresponding female IC, it was found that caregiver distress was associated with decreased likeliness of the PWD receiving the influenza vaccine. The likelihood of having a distressed caregiver was higher in unvaccinated care recipients. Unvaccinated recipients were more likely to exhibit limitations in their activities of daily living (ADLs) and instrumental activities of daily living (IADLs), and had higher level dementia-related behavioural problems. Additionally, unvaccinated recipients were more likely to have private insurance or use Medicaid, suggesting that financial barrier play an important role in vaccine uptake. Unvaccinated recipients were more likely to have caregivers with lower perceived financial adequacy and who lived farther away from medical facilities [4].
Healthcare professional impact
Healthcare providers, especially family physicians, are typically the first link or connection to the healthcare system. Several different factors were found to influence influenza vaccine uptake, including HCP’s personal characteristics and the relationship between the HCP and their patients. A study conducted in Israel found that patients were more likely to be immunized if their physician was also immunized [22]. Female doctors were more likely to be vaccinated than male doctors, which coincides with the finding that female doctors give stronger recommendations for vaccination than their male counterparts. In addition to physician’s gender, their background and lifestyle also contributed to the findings [22]. Physicians who were educated in Western Europe or America, as well as physicians who exercised were more likely to be vaccinated. Furthermore, physicians who had greater knowledge about the complex risk factors associated with influenza, such as the high risk of lower respiratory infections and mortality rates among PWD, were more likely to make stronger recommendations to PWD for getting the vaccine, while being more reluctant to accept refusal [23].
Bean and Catania [24] examined CAM providers’ beliefs regarding vaccinations since these providers may play an influential role in vaccine uptake for their clients. For the CAM providers that endorsed vaccinations, their reasoning was likely to fall within two themes: “vaccines prevent illness” and “herd immunity”. In contrast, for the CAM providers that did not endorse vaccines, their reasoning was likely to fall within three themes: “natural is best”, “innate intelligence”, and “the fragile immune system”. The non-endorsers focus was on providing health for the person rather than health for the population, and this emphasis has implications about the potential vaccine uptake among persons with dementia, who relied heavily on the advice from healthcare professionals to access vaccinations.
Extra-personal influence
Environmental factors
One of the more common environmental factors contributing to vaccine uptake among PWD was living accommodation. PWD were less likely than their counterparts to get the vaccine if they lived alone in their community. Researchers suggested that this result can be attributed to poor access of preventative care by PWD living in their own homes [25]. For those living in rural neighbourhoods, PWD may face even greater difficulty in accessing care and vaccination. Henkel and Marvanova [26] found that pharmacies in more rural areas are about 50% less likely to offer immunizations compared to less rural areas. Furthermore, Shah et al. [25] found that dementia does have an impact on influenza vaccine uptake in PWD who live in their homes. There is less vaccine uptake among PWD who live at home compared to those living in congregate and institutionalized settings. On the other hand, PWD were more likely to get the vaccine while living in a nursing or residential home compared to those without dementia [25]. Research found that 89.6% of PWD living in French nursing homes had the influenza vaccine administered, which is higher than the recommendation made by the WHO for that year (≥ 75% of older persons) [3]. One of the reasons the authors provided for this positive finding is that nursing home staff recognize that dementia is an independent risk factor for influenza complications.
Media impact
Media can impact an individual’s belief as he/she seeks out information from a variety of external sources. It was proposed that the strongest predictor of immunization uptake for children was parental attitude [27], so it is essential to have evidence-informed information for those who make decisions about vaccination. A study examining MMR (Mumps, Measles, Rubella) vaccine uptake reported that parents that have confidence in vaccination effectiveness are more likely to have their children vaccinated. However, respondents felt that the information they received from HCPs about vaccinations was biased, and vaccination safety information was not forthcoming [27]. If individuals feel that the information they are receiving from HCPs is biased, they are more likely to seek information elsewhere. There are dangers associated with this approach. Specifically, not all internet resources are credible or reliable for an individual to use when making informed decisions, for example A Voice for Choice. A Voice for Choice is a non-profit website that has a strong online following, and it claims to be promotive of evidence-informed decision-making. However, there is a clear intention of promoting anti-vaccination [28, 29]. Davies et al. [30] investigated the likelihood of finding anti-vaccination sites when people search “immunization” or “vaccination”. They found that 43% of resultant websites were related to anti-vaccination, and this result shows that there is a high probability that individuals seeking information about vaccinations are likely to discover anti-vaccination information. These anti-vax websites most commonly use emotional appeal to display the idea that vaccines cause idiopathic illness and destroy immunity. They also commonly impact vaccine confidence by sharing those adverse reactions to vaccines are underreported and that vaccination policies are motivated by profit [31]. The analogy of MMR vaccination and parental attitudes has implications for understanding persons of dementia’s vaccine hesitancy because they often rely on caregivers to make decisions on their behalf.
Study limitations
There is a lack of existing literature that examines the barriers PWD face in receiving the influenza vaccine. While this topic is under-studied, our current literature review was able to highlight some of the factors that may impact the vaccine uptake among dementia populations. However, this literature review has limitations that need to be acknowledged. Most evidently, some literature being examined may not related directly to the study topic, but rather it provides implications to enhance our understanding about the potential factors that impact PWD’s influenza vaccine uptake. A systematic review may potentially offer a more comprehensive approach to understanding the phenomenon of interest, as well as providing an appraisal of the included literature to assess the strength and quality of the available evidence.
Conclusion
Despite the categorization into the three over-arching themes, it is important to underscore that each theme, sub-theme, and stakeholder group is interconnected, and altogether influencing access to influenza vaccination among PWD. Based on this literature review, certain sub-themes may need to be examined more closely to help advance our understanding and implement effective strategies to improve vaccine uptake among PWD. Today, social media and online sources play a major role in contributing to vaccine hesitancy. Future research needs to focus on examining the facilitating factors to overcome the challenges of this important public health issue.
Funding
Partial financial support was received from Social Sciences and Humanities Research Council of Canada (SSHRC) Small Grant Program.
Availability of data and material
The data supporting the findings of this literature review are available within the article and/or supplementary materials. Additional data are available on request from the corresponding author, [WS].
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not required (not a human study).
Consent to participate
Not applicable.
Consent for publication
All named authors have contributed to the creation of the submission and grant Aging Clinical and Experimental Research permission to review and (if selected) publish their work.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention . Who is at high risk for flu complications. U.S. Department of Health & Human Services; 2018. [Google Scholar]
- 2.Alzheimer’s Society UK . Why everyone affected by Dementia should have a flu jab. Alzheimer’s Society UK; 2018. [Google Scholar]
- 3.Gallini A, Gardette V, Lapeyre-Mestre M, et al. Dementia diagnosis and influenza vaccination in French nursing home residents. J Am Geriatr Soc. 2015;63:1256–1258. doi: 10.1111/jgs.13515. [DOI] [PubMed] [Google Scholar]
- 4.Canadian Institute for Health Information . Dementia in Canada: Summary. Canadian Institute for Health Information; 2019. [Google Scholar]
- 5.Government of Canada . Vaccine uptake in Canadian adults 2019. Government of Canada; 2019. [Google Scholar]
- 6.Campitelli MA, Rosella LC, Stukel TA, et al. Influenza vaccination and all-cause mortality in community-dwelling elderly in Ontario, Canada, a cohort study. Vaccine. 2010;29:240–246. doi: 10.1016/j.vaccine.2010.10.049. [DOI] [PubMed] [Google Scholar]
- 7.Gross P, Hermogenes A, Sacks H, et al. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann Intern Med. 1996;123:518–527. doi: 10.7326/0003-4819-123-7-199510010-00008. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization (2019) Ten threats to global health in 2019. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019. Accessed 20 Jan 2020
- 9.Krein L, Jeon YH, Amberber AM, et al. The assessment of language and communication in dementia: a synthesis of evidence. Am J Geriatr Psychiatry. 2019;27:363–377. doi: 10.1016/j.jagp.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Naumova EN, Parisi SM, Castronovo D, et al. Pneumonia and influenza hospitalizations in elderly people with dementia. J Am Geriatr Soc. 2009;57:2192–2199. doi: 10.1111/j.1532-5415.2009.02565.x. [DOI] [PubMed] [Google Scholar]
- 11.Smith D, Lovell J, Weller C, et al. A systematic review of medication nonadherence in persons with dementia or cognitive impairment. PLoS ONE. 2017;12(2):e0170651. doi: 10.1371/journal.pone.0170651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Onishi J, Suzuki Y, Umegaki H, et al. Behavioral, psychological and physical symptoms in group homes for older adults with dementia. Int Psychogeriatr. 2006;18:75–86. doi: 10.1017/S1041610205002917. [DOI] [PubMed] [Google Scholar]
- 13.Jackson LA, Jackson ML, Nelson JC, et al. Evidence of bias in estimates of influenza vaccine effectiveness in seniors. Int J Epidemiol. 2006;35:337–344. doi: 10.1093/ije/dyi274. [DOI] [PubMed] [Google Scholar]
- 14.Crawford VLS, O’Hanlon A, McGee H. The effect of patient characteristics upon uptake of the influenza vaccination: a study comparing community-based older adults in two healthcare systems. Age Ageing. 2011;40:35–41. doi: 10.1093/ageing/afq152. [DOI] [PubMed] [Google Scholar]
- 15.Burns VE, Ring C, Carroll D. Factors influencing influenza vaccination uptake in an elderly, community-based sample. Vaccine. 2005;23:3604–3608. doi: 10.1016/j.vaccine.2004.12.031. [DOI] [PubMed] [Google Scholar]
- 16.The College of Physicians of Philadelphia . Cultural perspectives on vaccination. The College of Physicians of Philadelphia; 2018. [Google Scholar]
- 17.Gamble VN. Under the Shadow of Tuskegee: African Americans and Health Care. Am J Public Health. 1997;87:1773–1778. doi: 10.2105/AJPH.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moutsiakis D, Chin P. Why blacks do not take part in HIV vaccine trials. J Natl Med Assoc. 2007;99:254–257. [PMC free article] [PubMed] [Google Scholar]
- 19.Lu J, Luo M, Yee AZH, et al. Do superstitious beliefs affect influenza vaccine uptake through shaping health beliefs? Vaccine. 2019;37:1046–1052. doi: 10.1016/j.vaccine.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Health Quality Ontario . The reality of caring. Distress among the caregivers of home care patients. Health Quality Ontario; 2016. [Google Scholar]
- 21.Thorpe JM, Sleath BL, Thorpe CTK, et al. Caregiver psychological distress as a barrier to influenza vaccination among community-dwelling elderly with dementia. Med Care. 2006;44:713–721. doi: 10.1097/01.mlr.0000215905.36968.76. [DOI] [PubMed] [Google Scholar]
- 22.Abramson ZH, Levi O. Is performance of influenza vaccination in the elderly related to treating physician’s self Immunization and other physician characteristics? Prev Med (Baltim) 2008;47:550–553. doi: 10.1016/j.ypmed.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 23.Banach DB, Ornstein K, Factor SH, et al. Seasonal influenza vaccination among homebound elderly receiving home-based primary care in New York City. J Community Health. 2012;37:10–14. doi: 10.1007/s10900-011-9409-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bean SJ, Catania JA. Immunology beliefs as a factor in vaccine opposition among complementary and alternative medical providers. SAGE Open Med. 2018;6:205031211880762. doi: 10.1177/2050312118807625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah SM, Carey IM, Harris T, et al. The impact of dementia on influenza vaccination uptake in community and care home residents. Age Ageing. 2012;41:64–69. doi: 10.1093/ageing/afr135. [DOI] [PubMed] [Google Scholar]
- 26.Henkel PJ, Marvanova M. Rural Disparities in Alzheimer’s disease-related community pharmacy care in the United States. J Rural Heal. 2018;34:347–358. doi: 10.1111/jrh.12279. [DOI] [PubMed] [Google Scholar]
- 27.Smailbegovic MS, Laing GJ, Bedford H. Why do parents decide against immunization? The effect of health beliefs and health professionals. Child Care Health Dev. 2003;29:303–311. doi: 10.1046/j.1365-2214.2003.00347.x. [DOI] [PubMed] [Google Scholar]
- 28.A Voice for Choice (2018) No Title [Internet]. http://avoiceforchoice.org. Accessed 20 Jan 2020
- 29.Evrony A, Caplan A. The overlooked dangers of anti-vaccination groups’ social media presence. Hum Vaccines Immunother. 2017;13:1475–1476. doi: 10.1080/21645515.2017.1283467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davies P, Chapman S, Leask J. Antivaccination activists on the world wide web. Arch Dis Child. 2002;87:22–25. doi: 10.1136/adc.87.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wolfe RM, Sharp LK, Lipsky MS. Content and design attributes of antivaccination Web sites. J Am Med Assoc. 2002;287:3245–3248. doi: 10.1001/jama.287.24.3245. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this literature review are available within the article and/or supplementary materials. Additional data are available on request from the corresponding author, [WS].
Not applicable.