Abstract
BACKGROUND:
Work-related musculoskeletal disorders are prevalent in dental hygienists. Although engineering controls and ergonomic training is available, it is unclear why this intransigent problem continues. One possible barrier is that a comprehensive, standardized protocol for evaluating dental hygiene work does not exist.
OBJECTIVE:
This study aimed to generate a valid and reliable observational protocol for the assessment of dental hygiene work.
METHODS:
An iterative process was used to establish and refine an ecologically valid video acquisition and observation protocol to assess key activities, tasks, and performance components of dental hygiene work.
RESULTS:
Good inter-rater reliability was achieved across all variables when the final coding scheme was completed by three independent raters.
CONCLUSIONS:
This work provides an exemplar of the process required to generate a comprehensive protocol for evaluating the work components of a particular job, and provides standardized nomenclature for use by scientists and practitioners interested in understanding and addressing the pervasive issue of work-related disorders in dental hygienists.
Keywords: Dental Hygienists, Research Protocol, Clinical, Ergonomics
1. Introduction
Dental hygienists have a high prevalence of musculoskeletal disorders (MSDs), with discomfort and injuries in the hand/wrist, shoulder, and neck affecting more than 70% of practitioners [1–4]. Of even greater concern is evidence that indicates dental hygienists begin experiencing musculoskeletal discomfort in their preliminary training as students [4–6]. Work-related MSD are often very complex with a plethora of contributory factors including activity-based risks, psychosocial factors, and worker-specific demographic and health factors [1,7,8]. Among the many different factors, primary work-related mechanisms of MSD development in dental hygienists have been discussed in the literature. The use of hand-held instruments for scaling calculus from the teeth [9,10] and sustained positioning of the body, oftentimes in awkward postures [11] are the most commonly cited mechanisms, both of which are impacted by the number and type of patients seen each day [12]. The negative impacts of scaling and poor posture may be even more significant in dental hygiene students as they can spend up to three times longer working with a patient than a more skilled practitioner [13].
Engineering controls to modify equipment and the work environment have been the primary focus of attempts to minimize risk related to hand force and awkward posture, and resources discussing ergonomic dental environments are available [14]. Of particular note is extensive evaluation of hand strain based on different instrument types, which has resulted in adaptations of scaling instruments [15–18]. Similarly, the development and use of loupes that attach to glasses or protective lens for augmenting direct vision and minimizing extensive neck flexion have been the primary focus of research targeted at reducing discomfort due to awkward posture [19–22]. Additional equipment and environmental modifications have been evaluated, such as alterations in seating options [23], but there is limited evidence that these proposed interventions have significantly reduced MSDs in dental professionals [24].
Despite eliminating some risk, engineering controls are not likely to fully address the pervasive issue of MSDs without an additional focus on individual worker behavior. In fact, dental professionals have indicated using individual controls (e.g., stretching, posture, relaxation) more commonly than engineering controls [25]. Furthermore, there little evidence that clinic-based or educational behavioral interventions targeted at improving individual worker behavior in dental professionals is effective [26]. The issue of MSDs in dental hygienists is further exacerbated by the propensity for investigation of MSDs causes and interventions to be broadly focused on general dentistry, with limited focused investigation of the intensive exposures and practice patterns specific to dental hygienists [24]. As a result, there is little consensus within the dental hygiene profession on acceptable practice patterns, and wide variations exist in the deployment of student and practitioner training relative to the prevention of MSDs.
In order to address these issues and provide a foundation to reduce the overall impact of MSDs in dental hygienists through effective combinations of engineering and individual behavioral interventions, it is necessary to more fully understand all aspects of dental hygiene work that contribute to increased risk. Direct observation in the workplace is a useful and valid method to assess work performance components and physical exposures that increase risk for MSDs [2,27]. Although numerous observational techniques exist to evaluate work-related MSDs, there are no well-validated measures specific to dental hygiene. As such, a standardized, practical method to observe and describe dental hygiene practice would be useful to support the advancement of injury-prevention research, practice, and education within dental hygiene.
1.1. Objective
Our overall objective was to develop a standardized process for a robust assessment of the physical activities involved in patient-oriented dental hygiene work. We achieved this objective through three successive aims: (1) establish face validity for a coding scheme designed to describe dental hygiene work; (2) establish a feasible and valid protocol for clinic-based video-recording and application of the coding scheme; and (3) establish acceptable inter-rater reliability for descriptive coding of dental hygiene work. The purpose of this manuscript is two-fold. First, it is an exemplar of the process required to generate a valid and reliable comprehensive protocol to evaluate the work components of any particular job. Second, it provides a validated observational method and standardized nomenclature for use by scientists and practitioners to understand and address the pervasive issue of work-related MSDs in dental hygienists.
1.2. Overview of Research Design
We used an iterative process to develop and test protocols for video acquisition and video coding, followed by refinement of the coding protocol through a final phase of reliability testing with three raters. A convenience sample of 14 dental hygiene students and their patients were video-recorded so their performance could be used across the various phases of the study. Students were in their first or second year of study in a bachelor’s degree educational program for dental hygiene. During treatment sessions, the students provided one-to-one dental hygiene services to patients from the local community under the supervision of a dental hygiene instructor as part of the academic requirements for their program. Recorded patient sessions lasted between approximately 1.5 and 4 hours, with visit length primarily dependent upon the skill of the student and complexity of the patient. To ensure that the final acquisition and coding protocols had wide generalizability and utility, dental hygiene student participants were heterogenous in regards to gender, handedness, and body habitus. Approval was obtained from the university’s Institutional Review Board prior to beginning research activities, and all dental hygiene student and patient participants provided informed consent to be video recorded.
2. Protocol Development
2.1. Coding Scheme Development
A preliminary descriptive video coding scheme was developed by a dental hygienist (NLC), based on a combination of expert knowledge and contemporary educational materials [28]. This hygienist worked directly with an occupational therapist with more than 15 years of experience conducting activity and ergonomic analyses for the prevention of work-related MSD (SCR). Face validity for the coding scheme was established through review and refinement by an expert clinical/faculty dental hygienist (JYS), a research dental hygienist with more than 35 years of experience (JLF), and a second occupational therapist with previous experience in development of standardized ergonomic assessment tools (NAB). Each of the contributors shared their expert knowledge of the key components of dental hygiene work during a standard treatment visit, activity analysis, and ergonomic assessment. Through consensus, we developed a comprehensive coding scheme to assess the activities, tasks, and performance components related to dental hygiene work as described below.
2.1.1. Activity
codes were segments of a dental hygiene patient visit focused on one general aim. Activities included three direct patient care activities of assessment, patient education, and instrumentation (i.e., scaling and root planing) along with one ancillary patient care activity of infection control. Because data were obtained from students in a dental hygiene program, we added an additional activity code related to the time receiving instruction from a faculty member.
Assessment was defined as the systematic collection, analysis and documentation of the patient’s oral and general health status. Assessment was typically the initial activity of the dental hygiene visit, with individualized tasks relative to the needs of each patient. During assessment, we observed the following tasks: (a) review of patient chart and discussion of the medical history with the patient; (b) obtaining blood pressure; and (c) performance of an extra-oral and intra-oral visual exam. For the extra-oral exam, the hygienist would palpate the external surfaces of the patient’s face and internal soft tissues as part of an oral cancer screening. During the intra-oral exam, a probe, explorer, and mirror were used to examine the patient’s oral cavity, complete a periodontal assessment, and conduct a caries risk assessment, as well as to examine surfaces of the teeth to detect irregularities, such as fractures, decay, and calculus. In addition to these tasks, assessment sometimes involved obtaining radiographs, photos, and other diagnostic measures.
Instrumentation was the primary activity of the dental hygiene visit. It included scaling and root planing to improve the patient’s oral health. Dental scaling, or the removal of plaque, debris, and calculus from the teeth, was completed using manual instruments, ultrasonic instruments, or both. Ultrasonic scaling devices convert a high-frequency electrical current into mechanical vibrations. These ultrasonic vibrations remove calculus and plaque from the teeth, while water is sprayed from the instrument to flush out bacteria from the teeth and gums. In contrast, calculus removed through manual scaling is completed by the hygienist providing direct force to the tooth deposits through various different hand-held instruments. Both techniques require a separate device for irrigation and suction.
Patient education activities included conducting a counseling session with the patient regarding risk factors for poor oral health and instructions on proper care of the teeth, gums, and mouth. During patient education, a disclosing solution was sometimes used (i.e., a red, pink, purple, or blue dye) to show plaque on the teeth, and the student typically offered demonstrations to the patient using a tooth brush, floss, and/or other aids. Infection control included behaviors designed to reduce the risk of spreading infection. While infection control primarily occurred prior to and following the patient care visit (e.g., disinfecting the work area, placing/removing covers on surfaces), infection control during patient care included donning or changing gloves and washing hands.
In addition to patient care activities, we used three final activity codes to classify time within the patient visit. Faculty consultation was common, as the educational program required various checks by the faculty member for a student to progress through the patient visit. Although initially included as a sub-component of instrumentation, faculty consultation was included as an activity in the final scheme, and was identified as any time during which the faculty member took the place of the student to complete direct assessment, instrumentation, or education with the patient. Other discussion or instruction by the faculty member while the student maintained a primary role in the patient-centered activity were not identified as faculty consultation.
Patient is away was used to capture any time during the patient visit where no activity was completed by the hygienist because the patient had gotten out of the chair. This behavior often occurred when the patient needed to use the restroom or if imaging was conducted at a different location. One last activity code, other activity, was added to the final coding scheme to account for any significant time spent by the dental hygiene student doing something other than the primary activities described above. Qualitative descriptions of the dental hygiene students’ behaviors were recorded each time this code was used.
2.1.2. Task
codes represented the minute-to-minute components of the larger activities the dental hygiene students completed during the patient visit. Given that instrumentation accounts for the majority of a patient visit and involves the highest opportunity for musculoskeletal risk exposure, we developed a task-level coding scheme only for this activity and none of the others. A total of nine instrumentation task codes were developed.
Hand scaling was the use of a hand-held instrument to remove plaque, stain, and calculus. During hand scaling, students usually held the scaling instruments in the dominant hand, while holding a mirror in the non-dominant hand. Hand scaling involved the application of force with visible physical movements of the forearm, wrist, or hand to manually activate a scaling stroke on the teeth. Curettage, the removal of inflamed soft tissue lining of a pocket wall using light pressure through a hand-held instrument between the gum and tooth, was indistinguishable as a separate task; thus, curettage was also coded as hand scaling. Ultrasonic scaling used a power-driven scaling instrument to remove plaque and calculus. During ultrasonic scaling, movements of the hygienists’ forearm, wrist, and hand were less pronounced than with hand scaling.
Although scaling accounted for the majority of instrumentation, four additional direct patient care tasks occurred. Pain management involved the administration of nitrous oxide through a nasal mask, injection of a local anesthesia into the gingiva, or topical application of anesthetic using a cotton swab stick or a hand-held applicator (i.e., Oraqix®). Pain management typically occurred near the beginning of instrumentation activities. Alternatively, polishing, flossing, and application of preventive materials were typically conducted near the end of the instrumentation activity. In respective order, these tasks included use of a hand-held instrument to apply polishing paste and friction to the teeth, use of dental floss to remove biofilm from the proximal surfaces of the teeth, i.e., plaque removal from in-between the teeth, and the application of fluoride varnish to the surfaces of the teeth with a small brush.
Two ancillary tasks completed by the dental hygiene students as part of instrumentation were noted. Irrigation/suction involved the act of flushing a specific area of the mouth with a continuous or pulsed stream of water to cleanse the area or provide other therapeutic purpose, followed by the removal of excess fluid from the mouth using a suction tube/saliva ejector. At the end of the scaling procedure a syringe with antimicrobial solution (e.g., betadine, diluted bleach) is used for subgingival irrigation. Instrumentation sharpening was coded with the hygienist was observed rapidly moving the cutting edge of a hand scaling instrument up and down across a sharpening stone. As with activity coding, a code for miscellaneous task was added to account for any time spent during instrumentation that did not fit within one of the predefined tasks noted above.
2.1.3. Performance components
included six additional observational elements specific to the performance of dental hygiene work. These components were included in our coding scheme due to their relevance in training dental hygiene students and their usefulness in describing positions and postures of the hygienist during patient care. Each of these purposed have potential importance to the development or remediation of MSD risk. Definitions and operational coding procedures are provided in Table 1 for each of the following six performance components: (1) hygienist position as sitting or standing; (2) patient’s chair position as supine, semi-supine, or upright; (3) patient’s chair height as too low, appropriate height, or too high; (4) clock position of the hygienist around the patient (i.e., 7:00 through 5:00); (5) patient’s head rotation as left, right, or center; (6) area of the mouth being addressed.
Table 1.
Final coding scheme for key job components, performance components, and risk exposures within a robust observational assessment of dental hygiene work.
| Activities and Tasks | |||
| Variable | Codesa | Operational Definition | Type of Coding |
| Dental Hygiene Activities |
Assessment Faculty Consultation Infection Control Instrumentation Patient Education Patient is Away Other Activity |
Activity codes represent components of the patient visit during which an over-arching goal for the visit is accomplished. Activities are characterized in large segments of time, each of which typically occur during a patient visit. Activities are identified based on the individual descriptions as detailed in section 2.1.1. | Continuous, across entire session |
| Instrumentation Tasks |
Flossing Hand Scaling Instrument Sharpening Irrigation Pain Management Polishing Ultrasonic Scaling Miscellaneous Task |
Task codes represent individual components within an Activity, and describe the moment-to-moment actions of the hygienist. Tasks are short, can occur only once, intermittently, or repetitively throughout a patient visit. Instrumentation tasks are identified based on the individual descriptions as detailed in section 2.1.2. | Continuous, during instrumentation activity |
| Performance Components | |||
| Variable | Codesa | Operational Definition | Type of Coding |
| Hygienist Sit/Stand |
Sitting Standing |
Sitting and standing are coded based on the visualized positioning of the hygienist. When the hygienist not in view, the last code used remains active until the hygienist returns to view. | Continuous, across entire session |
| Patient Chair Position |
Upright Semi-Supine Supine Patient Out of Chair |
Patient chair position is identified using the relative angle of the chair back to the floor. Supine indicates an angle of 0 to 15 degrees, Semi-Supine from 15 degrees 65 degrees, and Upright > 65 degrees. | Continuous, across entire session |
| Patient Chair Heightb |
Too High Acceptable Height Too Low |
Patient chair height is coded based on the relative position of the patients head to the torso of the hygienist, considering the effect on positioning of the hygienists’ upper body and extremities. At an acceptable chair height, the hygienist can work with a straight spine, retracted scapulae, and limited shoulder extension and 90-degrees of elbow flexion. Compressed or overextended postures are indications of chair height being too high or too low. | Descriptive observation during selected, discrete video segments |
| Clock Position |
7 O’clock – 5 O’clock Away from Patient |
Clock position refers to the location of the dental hygienist’s hips relative to the patient’s mouth as seen from above. Position is coded as a whole number starting at 7 through 12 on the patient’s right side and continuing from 12 through 5 on the patient’s left side. Coding of any movement away from patient or a change in clock position occurs when the duration of the new position is maintained for longer than 15-seconds. To improve reliability, clock position can be grouped or coded in three categories: [7–10], [11–1], [2–5] | Continuous, during instrumentation activity |
| Patient Head Position |
Neutral Left Right |
Patient head position refers to the direction of cervical rotation. Head position is coded as neutral when cervical rotation is approximated to be < 45 degrees in either direction. Left or right indicates rotation > 45 degrees or is used when the hygienist actively intervenes to position the patient’s head in a rotated position away from the midline. | Continuous, during hand scaling or ultrasonic scaling tasks, or Descriptive observation during selected video segments |
| Area of the Mouth |
Lower Left Upper Left Lower Right Upper Right |
Area of the mouth indicates the general location of the tooth or teeth that are actively being assessed, scaled, or otherwise attended to as part of the dental hygiene activity or task. In dental hygiene practice, the mouth is divided into quadrants or sextants. This protocol uses quadrants that divide the rows of teeth into upper or lower and left or right, each relative to the patient. | Continuous, during hand scaling or ultrasonic scaling tasks |
All codes for a given variable are mutually exclusive, such that no two codes can be actively applied at the same time.
Patient chair height is only evaluated as a secondary factor as a possible means for explaining poor posture or positioning in selected, discrete video segments.
2.2. Video Acquisition Protocol Development
To develop a standardized, ecologically valid video-recording protocol, we conducted preliminary field testing. In our preliminary protocol we obtained videos using two cameras positioned in orthogonal views within the dental hygiene clinic (Figure 1). A Handycam HDR (Sony Corporation; Minato, Tokyo) was mounted on a tripod and placed at a 90-degree angle from the patient’s hips, approximately 6-feet away. This camera provided a wide-view of all activities completed by the dental hygiene student during the patient visit and provided information related to the student’s neck, trunk, and leg postures. The second camera, a GoPro Hero 4 (GoPro, Inc.; San Mateo, CA), obtained a high-definition, close-up view of the hygiene student to patient interaction. This camera was mounted on a mini tripod and placed on the dental unit’s main tray, which was positioned over the patient’s hips and aimed at the patient’s mouth. To provide consistency in video observations across participants and minimize bias or error due to angle distortions, both cameras were placed in the same position for each video collection and remained stationary throughout the entire patient visit.
Figure 1.
Initial camera set-up using two orthogonal views.
We trialed this preliminary protocol with five student-patient interactions. The videos were transferred to a secure server, post-processed using editing software to sync videos from the two angles, and imported into Observer XT (Noldus, Inc.; Leesburg, VA) for analysis. One investigator (NLC) applied the proposed coding scheme to each of the five videos to evaluate the suitability of the video acquisition process and coding definitions. The investigator was able to complete activity, task, and performance coding on the videos which lasted 178 minutes (2.9 hours) on average. However, approximately 20% of the time the dental hygiene students leaned in front of the camera positioned on the over chair tray, blocking the view and making it impossible to complete a valid analysis of multiple performance components.
To ensure that we could adequately capture and document all activities, tasks, and performance components, we added a third orthogonal view by mounting a camera to the ceiling, aimed perpendicular to the floor and centered over the patient’s mouth when the patient was fully supine. To reduce post-processing challenges of syncing videos from the three views, we used three GoPro cameras and a wireless remote to start and stop all videos simultaneously. We used the refined, three-camera protocol (Figure 2) to record four hygienist-patient interactions in a final round of field testing. Across the videos, there were no instances where the patients’ mouth was blocked in all three views at the same time, allowing for 100% coding of the all activities, tasks, and performance components across the entire patient visit in all video sessions.
Figure 2.
Final protocol for video camera and sample resulting views of the hygienist and patient from cameras placed overhead (A), in front (B), and lateral (C). For purposes of general representation in this paper, sample images have been cropped from the full field of view.
3. Protocol Reliability
3.1. Video Coding Reliability for Activity, Task, and Performance Codes
We used an iterative process of coding, data review, and protocol refinement to implement and validate the coding scheme developed in section 2.1 with videos obtained using the acquisition protocol described in section 2.2. Three raters with no previous experience, knowledge, or expertise in dental hygiene practice, nor any previous experience completing observational analyses, were provided with the coding scheme and trained to use the Observer XT software. Following initial training, raters completed three rounds of independent coding. Between each round, results of the coding process, difficulties or challenges, and reliability data were reviewed and discussed among the raters and the senior investigator (SCR). Through consensus, the coding scheme was revised and process improvements were implemented prior to starting the next round. Rater agreement and inter-rater reliability for coding of each variable across the three rounds of coding is provided in Table 2, and a summary of protocol updates following each round is described below.
Table 2.
Inter-rater agreement and reliabilitya across subsequent rounds of coding the activities, tasks, and performance components of a dental hygiene patient visit.
| Round 1 | Round 2 | Round 3 | ||||
|---|---|---|---|---|---|---|
| % agreement | kappa | % agreement | kappa | % agreement | kappa | |
| Activity | 76.9 – 85.5 | .64 – .77 | 92.8 – 99.6 | .88 – .99 | 88.6 – 96.5 | .79 – .93 |
| Task | 71.1 – 86.4 | .58 – .77 | 80.0 – 90.7 | .68 – .85 | 82.1 – 88.6 | .72 – .81 |
| Sit/Stand | 66.6 – 78.2 | −.05 – .27 | 93.6 – 97.0 | .72 – .86 | 97.6 – 98.1 | .93 – .94 |
| Chair Position | 28.6 – 74.0 | −.03 – .54 | 77.6 – 89.7 | .31 – .69 | 94.0 – 99.3 | .80 – .98 |
| Chair Heightb | 35.9 – 57.0 | −.11 – .07 | 38.1 – 57.0 | −.05 – .17 | Not Applicable | |
| Clock Position | 47.2 – 63.1 | .34 – .51 | 67.1 – 67.8 | .54 – .55 | 75.6 – 79.0 | .65 – .69 |
| Head Position | 43.2 – 57.9 | .16 – .35 | 43.2 – 56.6 | .16 – .34 | 40.6 – 67.9 | .26 – .53 |
| All Codes | 76.9 – 85.5 | .64 – .77 | 75.2 – 78.3 | .73 – .77 | 83.0 – 87.3 | .81 – .86 |
Percentages and scores were calculated for all possible paired combinations across the three raters; values are presented as a range from minimum to maximum across all rater pairs.
Chair height was eliminated from the coding process and was not evaluated in round 3 due to poor agreement/reliability.
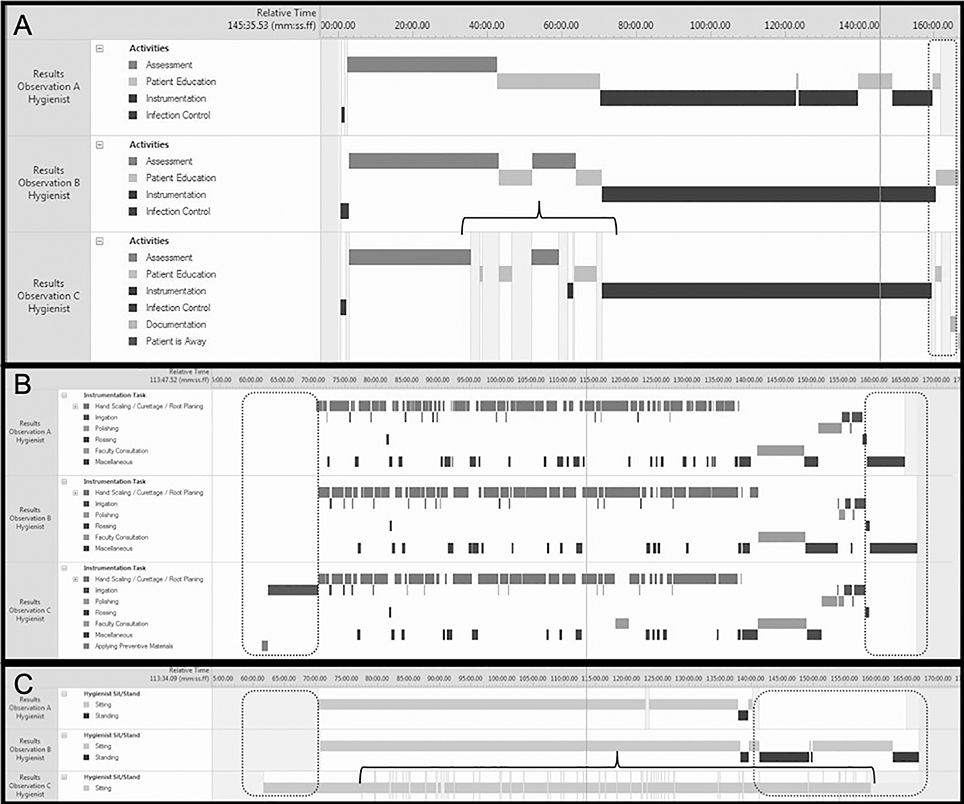
Following the first round of coding, we used data visualizations provided by our software (Figure 3) to identify two primary sources of poor reliability: (1) rater error and (2) missing concepts in the initial coding scheme. When we compared the data visualizations across the three raters for each variable we identified two primary sources of coding error: 1) gaps in continuous coding and 2) discrepancies in coding was started and stopped. To minimize these errors, the raters utilized the visualization feature within the software to check their coding after each phase of the process, going to each location where a code was missing to add the appropriate code. In addition to coding error, the raters noted that some gaps were due to missing coding options for individual variables. As a result, we added away from patient as an option to the clock position, and other and miscellaneous to the task and activity variables. Finally, we elevated faculty consultation from a task to an activity. After recoding the same video with these corrections in place, overall agreement and reliability was noted to dramatically improve for all variables with exception of chair position, chair height, and head position (i.e., Round 2 in Table 2).
Figure 3.
Sample visualizations from Round 1 of observational coding for activities (A), tasks (B), and sitting/standing (C) used to identify significant error and discrepancies in the coding process across the three raters, such as start/end (dashed circles) and intermittent periods of no-codes (brackets).
To address poor-to-fair reliability for coding patient chair and head position, the team decided on specific degree-angles for the codes within each variable. Using a goniometer, each rater indicated the angle at which a code would change from one category to the next. That is, what angle triggered a switch in coding from upright to semi-supine and from semi-supine to supine for chair position, and from neutral to either left or right for head position. The group agreed to apply chair angles of >65-degrees, 15-degrees to 65-degrees, and <15-degrees to the categories of upright, semi-supine, and supine, and cervical rotation of >45-degrees for left or right head positions.
Reliability of coding chair height remained poor. We determined that categorizing the location of the patient’s head to the hygienist’s torso as an indicator of the appropriateness of the patient’s chair height was problematic as there were a variety of factors which could influence the perception of this relationship (e.g., hygienists’ chair height, hygienist height, distance of hygienist to patient). In addition, even when the environment was set-up correctly, selected postures by the hygienist (e.g., slouching) often altered rater assumptions of ‘appropriate’ height. Given the complexity of these factors, we could not achieve consensus on an acceptable method for coding patient chair height. Instead we retained this variable in the final coding scheme (i.e., Table 1) for use in deeper examination or description of relative positioning in discrete video segments.
In addition to refinements to each of the fair-to-poor codes, the team agreed to standardize the sequence for conducting the video analysis to improve efficiency, minimize error, and improve reliability. We implemented a three-phase coding process: (1) watching the full video to continuously code activities, sit/stand, and patient chair position across the entire session; (2) watching portions of the video identified as instrumentation to code tasks and clock position; and (3) watching segments identified as hand scaling or ultrasonic scaling tasks to code patient head position and area of the mouth. Following each phase, raters used data visualizations within the software to ensure variables had been continuously coded throughout the required periods.
Using a new video, a third round of reliability testing was conducted using the refined code definitions and standardized three-phase process. Overall agreement and reliability across the three raters in Round 3 were improved, with reliability for all variables except clock position and patient head position surpassing an acceptable threshold of 80%. When we examined inconsistencies in clock position ratings we found that the majority of discrepancies were off by only one position (e.g., 9 o’clock vs. 10 o’clock). Collapsing individual codes into three categories (i.e., 7–10, 11–1, 2–5) resulted in dramatically improved agreement. In addition, these resulting categories improved ecological validity vis-à-vis general positioning described in typical dental hygiene education and training. Given fair-to-good overall reliability the final protocol reflects the most specific level of coding by individual clock position, leaving open the option to collapse the codes into groups for interpretation and analysis.
Patient head position was the final variable where reliability remained fair (kappa: .26 – .53). Since a coronal view of the patient in supine was not available, a 45-degree angle was difficult to verify. To maximize rater consistency, we added a final behavioral cue to the coding definition. Raters observed if hygienists actively repositioned the patients’ heads. This repositioning indicated that a patient’s head was either left or right. Given limitations in camera angles, we determined that, like chair height, this variable holds more value as a means to further explore specific, discrete segments of time where postures are poor or other clinical questions arise. In this case, patient head position would be deployed as a single event code to be tagged to the segment rather than as a continuously coded variable.
3.2. Reliability of Video Protocol for Conducting Postural Risk Assessment
In addition to activities, tasks, and performance components, we assessed posture during dental hygiene visits using the rapid upper limb assessment (RULA), an observational screening tool for MSD risk due to sustained or repetitive posture [29]. We used a three-stage, iterative process to confirm that we could apply the RULA to the videos and to establish inter-rater reliability across the same three raters. We specified static or sustained postures as any video segment where the hygiene student maintained the same clock position for greater than 60-seconds while completing scaling or root planing as described in section 2.1.4. Twenty, 60-second segments from four different videos (i.e., five segments per video) were randomly selected for inter-rater reliability assessment. Each rater scored the RULA once per segment, per round (i.e., a total of 60 ratings across the 3 rounds). Raters were given instruction and feedback between rounds to improve skill and build consensus on how to apply the RULA to this specific worker population. We did not encounter any significant issues in deploying the RULA using the videos obtained. Among the three raters, ICCs for the overall RULA score, upper extremity subscale score, and neck-trunk-leg subscale score were .89, .77, and .85, respectively, indicating good to excellent overall inter-rater reliability.
4. Discussion
The purpose of this study was to develop and validate an observational method to assess occupational performance and identify risk of MSD development in dental hygienists. A comprehensive observational coding scheme, including definitions of dental hygiene activities, tasks, and performance components was successfully developed, validated, implemented, and refined. The final video acquisition protocol described in this manuscript uses three orthogonal views and is feasible to complete and allows for the assessment of 100% of the activities, tasks, and performance components related to dental hygiene work. In addition, we achieved good-to-excellent inter-rater reliability for our observational coding scheme and the RULA by raters who had no previous experience with either dental hygiene work or postural assessment.
Despite engineering improvements in dental instruments and adjustable workspaces, as well as ergonomics training embedded within educational programs and continuing education, the high prevalence of MSDs for dental hygienists is seemingly intransigent. Moreover, it remains unclear why the prevalence of MSDs in dental hygienists exceeds other similar health professionals and has not improved across time despite significant research on engineering controls [24] and identification of barrier to implementation of personal controls [30]. Several possible explanations for this phenomenon deserve exploration: (1) ergonomics education in dental hygiene may not be effective or heeded by the work-force requiring a change in how ergonomic education is implemented; (2) there may be unknown risk factors related to the specific work tasks of dental hygienists requiring further evaluation of engineering controls or environmental adaptations; or (3) the psychosocial/psychophysical/stress demands of dental hygiene work, even when using best practices, may still expose hygienists to risk requiring a closer examination of administrative controls [31,32].
Protocols and terminology developed in this study provide a foundation to examine these issues within the dental hygiene profession. Deployment of this protocol in future large-scale observational studies with heterogeneous samples of dental hygiene clinicians and students, as well as varied practice settings can provide robust data to identifying risk factors for MSDs. For example, this protocol could assist in teasing out risk due to poor posture versus static muscle activity [33]. Moreover, if deployed universally, this standardized taxonomy will promote the aggregation and comparison of data across studies. In addition to examining risk, this observation protocol may be a useful tool to enhance ergonomic training. The protocol could be used as a self-assessment intervention, allowing clinicians and students to become aware of working positions. This knowledge could result in improved ergonomic training, thereby lowering risk for development of MSDs.
It is necessary to discuss limitations in the scope of impact and other considerations for implementation of this assessment protocol. Reliability assessment and overall protocol validation was completed with videos obtained in one academic clinical setting. As such, some aspects of the acquisition and analysis protocols may not be directly generalizable to other dental hygiene practice settings. Successful translation and implementation at other sites may require modifications to the specific positioning of the cameras. Following initial implementation of the observational protocol, investigators or clinicians should conduct individual validity and reliability assessments to be compared to the statistics documented in this study to ensure ecological validation of the novel implementation. Details of the process used to evaluate and refine video acquisition and coding to improve reliability in this study can serve as a guide for adapting the protocol.
In addition to translation to novel settings, future implementation of the observational protocol may be limited by the lack of a robust software package for coding. Even in situations where comprehensive continuous analysis of every activity, task, and performance component cannot be completed, this protocol provides a common nomenclature and taxonomy for evaluating and documenting the various components of dental hygiene work. Although individual investigators or clinicians may only evaluate selected components of the full protocol, dissemination of the findings across multiple studies will be more easily aggregated or compared if investigators use this standardized protocol.
Finally, the protocol described here may not directly impact remediation of MSD; instead, the protocol is provided as a standardized, valid method of activity analysis that can serve as a foundation for performing exposure-response risk assessments to identify and target preventive interventions [34]. Further examination is needed to determine if implementation of this robust analysis process to identify global risk across all activities is more effective in identifying and addressing MSD risk than are traditional observational techniques that rely on brief sampling to estimate risk. Moreover, reduction of MSD in oral health care providers will likely require an expanded assessment of activities not related to direct patient care (e.g., documentation), as well as an examination of the many psychosocial and personal factors that can contribute to MSD.
5. Conclusion
The data acquisition and analysis protocol described in this study provides a standardized, validated method for examining occupational performance and ergonomic risks in dental hygiene practice. Moreover, when deployed universally, this protocol would allow data to be more easily aggregated together across studies. In total, the validated protocol provides a foundation to support efforts toward teasing out individual risk factors and developing interventions to address the pervasive issue of MSDs in the dental hygiene profession.
Acknowledgements
The authors wish to acknowledge support provided by Cassie Tseng and Bryan van der Wyk in the early stages of development and testing of this protocol, as well as additional support for completion and refinement of the observational coding process provided by Rachel Eckerling, Yiyang (Sunny) Fang, and Samantha Randolph.
Funding: This work was supported by a grant from the Centers for Disease Control, National Institute for Occupational Safety and Health (R01-OH010665). The content is solely the responsibility of the authors and does not necessarily represent the official views of the CDC/NIOSH.
Footnotes
Declarations of interest: None
References
- [1].Lietz J, Kozak A, Nienhaus A. Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PloS one. 2018;13(12):e0208628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Occhionero V, Korpinen L, Gobba F. Upper limb musculoskeletal disorders in healthcare personnel. Ergonomics. 2014;57(8):1166–91. [DOI] [PubMed] [Google Scholar]
- [3].Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2010;35(4):419–29. [DOI] [PubMed] [Google Scholar]
- [4].Morse T, Bruneau H, Michalak-Turcotte C, et al. Musculoskeletal disorders of the neck and shoulder in dental hygienists and dental hygiene students. J Dent Hyg. 2007;81(1):10. [PubMed] [Google Scholar]
- [5].Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int J Dent Hyg. 2009;7(3):176–181. [DOI] [PubMed] [Google Scholar]
- [6].Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders in a 3 year longitudinal cohort of dental hygiene students. J Dent Hyg. 2014;88(1):36–41. [PubMed] [Google Scholar]
- [7].Cho K, Cho HY, Han GS. Risk factors associated with musculoskeletal symptoms in Korean dental practitioners. J Phys Ther Sci. 2016;28(1):56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ahuja R, Bashir U, Kushwah A, Pachauri A. Importance of ergonomics among dental professionals to prevent musculoskeletal disorders. Adv Hum Bio. 2015;5(3):14. [Google Scholar]
- [9].Anton D, Rosecrance J, Merlino L, Cook T. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. 2002;42(3):248–257. [DOI] [PubMed] [Google Scholar]
- [10].Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 2003;134(10):1344–1350. [DOI] [PubMed] [Google Scholar]
- [11].Howarth SJGD, La Delfa NJ, Cox J, Potvin JR. Working position influences the biomechanical demands on the lower back during dental hygiene. Ergonomics. 2015;59(4):545–555. [DOI] [PubMed] [Google Scholar]
- [12].Humann P, Rowe DJ. Relationship of musculoskeletal disorder pain to patterns of clinical care in California dental hygienists. J Dent Hyg. 2015;89(5):305–12. [PubMed] [Google Scholar]
- [13].Fang Y, Tung KD, Beleno-Sanchez J, Forrest JL, Roll SC. Characterization of Tasks and Time Efficiency of Dental Hygiene Students During Clinical Training. J Dent Hyg. 2020;94(5):30–7. [PMC free article] [PubMed] [Google Scholar]
- [14].Ahearn DJ, Sanders MJ, Turcotte C. Ergonomic design for dental offices. Work 2010;35(4):495–503. [DOI] [PubMed] [Google Scholar]
- [15].Dong H, Loomer P, Barr A, Laroche C, Young E, Rempel D. The effect of tool handle shape on hand muscle load and pinch force in a simulated dental scaling task. Appl Ergon. 2007;38(5):525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hayes MJ. The Effect of Stainless Steel and Silicone Instruments on Hand Comfort and Strength: A pilot study. J Dent Hyg. 2017;91(2):40–44. [PubMed] [Google Scholar]
- [17].Simmer-Beck M, Branson BG. An evidence-based review of ergonomic features of dental hygiene instruments. Work 2010;35(4):477–85. [DOI] [PubMed] [Google Scholar]
- [18].Suedbeck JR, Tolle SL, McCombs G, Walker ML, Russell DM. Effects of Instrument Handle Design on Dental Hygienists’ Forearm Muscle Activity During Scaling. J Dent Hyg. 2017;91(3):47–54. [PubMed] [Google Scholar]
- [19].Branson BG, Bray KK, Gadbury-Amyot C, et al. Effect of magnification lenses on student operator posture. J Dent Educ. 2004;68(3):384–389. [PubMed] [Google Scholar]
- [20].Branson BG, Abnos RM, Simmer-Beck ML, King GW, Siddicky SF. Using motion capture technology to measure the effects of magnification loupes on dental operator posture: A pilot study. Work. 2018;59(1):131–139. [DOI] [PubMed] [Google Scholar]
- [21].Hayes MJ, Osmotherly PG, Taylor JA, Smith DR, Ho A. The effect of loupes on neck pain and disability among dental hygienists. Work. 2016;53(4):755–62. [DOI] [PubMed] [Google Scholar]
- [22].Maillet JP, Millar AM, Burke JM, Maillet MA, Maillet WA, Neish NR. Effect of magnification loupes on dental hygiene student posture. J Dent Educ. 2008;72(1):33–44. [PubMed] [Google Scholar]
- [23].De Bruyne MA, Van Renterghem B, Baird A, Palmans T, Danneels L, Dolphens M. Influence of different stool types on muscle activity and lumbar posture among dentists during a simulated dental screening task. Appl Ergon. 2016;56:220–226. [DOI] [PubMed] [Google Scholar]
- [24].Roll SC, Tung KD, Chang H, Sehremelis TA, Fukumura YE, Randolph S, Forrest JL. Prevention and rehabilitation of musculoskeletal disorders in oral health care professionals: A systematic review. J Am Dent Assoc. 2019;150(6):489–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Sanders MJ, Turcotte CA. Ergonomic strategies for dental professionals. Work. 1997;8(1):55–72. [DOI] [PubMed] [Google Scholar]
- [26].Mulimani P, Hoe VC, Hayes MJ, Idiculla JJ, Abas AB, Karanth L. Ergonomic interventions for preventing musculoskeletal disorders in dental care practitioners. Cochrane Database Syst Rev. 2018;10:CD011261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Takala EP, Pehkonen I, Forsman M, et al. Systematic evaluation of observational methods assessing biomechanical exposures at work. Scand J Work Environ Health. 2010;36(1):3–24. [DOI] [PubMed] [Google Scholar]
- [28].Wilkins E Clinical Practice of the Dental Hygienist. 12th ed. Philadelphia: Lippincott Williams & Wilkins; 2016. [Google Scholar]
- [29].McAtamney L, Nigel Corlett E. RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergo. 1993;24(2):91–99. [DOI] [PubMed] [Google Scholar]
- [30].Droeze EH, Jonsson H. Evaluation of ergonomic interventions to reduce musculoskeletal disorders of dentists in the Netherlands. Work. 2005;25(3):211–20. [PubMed] [Google Scholar]
- [31].Warren N Causes of musculoskeletal disorders in dental hygienists and dental hygiene students: A study of combined biomechanical and psychosocial risk factors. Work. 2010;35(4):441–54. [DOI] [PubMed] [Google Scholar]
- [32].Sakzewski L, Naser-ud-Din S. Work-related musculoskeletal disorders in Australian dentists and orthodontists: risk assessment and prevention. Work. 2015;52(3):559–79. [DOI] [PubMed] [Google Scholar]
- [33].Books GJ, Klemm K. A unique approach to preventing back pain in the dental office. Work. 2012;42(2):299–306. [DOI] [PubMed] [Google Scholar]
- [34].Tung KD, Fukumura YE, Baker NA, Forrest JL, Roll SC. Identifying an Optimal Sampling Method to Estimate Postural Risk in a Dynamic Work Task. Proc Hum Factors Ergon Soc Annu Meet. 2019;63(2):1028–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]