Abstract
For a fifth-time redo aortic valve replacement, a Y incision was made through the left-noncommissure post into the aortomitral curtain above the mitral annulus, undermining the aortic annulus below the nadirs of left coronary and noncoronary cusps without violating the left atrium or mitral valve. A rectangular Hemashield (Maquet Cardiovascular, San Jose, CA) patch was used to extensively enlarge the aortomitral curtain. The aortic annulus was increased from 21 mm to 27 mm for a mechanical aortic valve replacement. The patient was discharged without blood transfusion or any complications. Our enlargement technique was simple and effective to enlarge the aortic annulus for mechanical aortic valve replacement.
We previously described using a Y incision and rectangular patch to enlarge the aortic annulus for aortic valve replacement (AVR) with bioprosthesis.1 Herein we report using our root enlargement technique to enlarge the aortic annulus by three valve sizes for mechanical AVR without violating any adjacent structure of the aortic root.
The patient was a 37-year-old woman who weighed 203 pounds (92 kg), with body height of 5 feet, 8 inches (172 cm) and body surface area of 2.05 m2. She had had five previous operations, including resection of subaortic membrane, myectomy with patent foramen ovale closure, aortic valve repair, aortic valve replacement with a 23-mm Magna Ease (Edwards Lifesciences, Irvine, CA), and valve-in-valve transcatheter AVR (23-mm Evolut; Medtronic, Minneapolis, MN [Supplemental Figure 1]). She presented with congestive heart failure from severe aortic stenosis and insufficiency. She underwent a fifth redo aortic root enlargement and AVR. The annulus size was measured at 21 mm after removal of the Evolut valve and Magna Ease valve and debridement of the annulus. After root enlargement, we placed a 27-mm Regent Mechanical valve (St Jude Medical, St Paul, MN). Postoperative aortic valve mean gradient was 7 mm Hg with normal coronary blood flow, no mitral regurgitation, and no blood transfusion. The patient was discharged without complications.
TECHNIQUE
The aorta was transected at mid-ascending aorta distal to the CoreValve (Video). The CoreValve was carefully peeled off the aortic wall with sharp dissection to prevent any tearing of the aorta and removed from the Magna Ease valve (Figure 1A). The Magna Ease valve was removed. The annulus was debrided and sized with a St Jude sizer to be 21 mm (Figure 1B). The aortomitral curtain was denuded from removal of the previous bioprosthesis. The adhesions at the posterior side of the root were divided. The left-noncommissure post was incised from the aortotomy into the aortomitral curtain close to the left atrial dome. The incision was extended in a “Y” fashion undermining the left coronary and noncoronary annulus to their respective nadir (Figure 1C).
FIGURE 1.

(A) The left coronary cusp of Evolut valve was fractured (white arrow), resulting in severe aortic insufficiency. Because of small bioprostheses (23-mm Magna Ease and 23-mm Evolut valve as valve-in-valve), peak gradient across valves was 61 mm Hg and mean gradient was 33 mm Hg. (B) After removal of Evolut and Magna Ease valves and debridement of pannus and pledgets, aortic annulus was sized as 21 mm. (C) After aortomitral curtain was incised with Y incision, root was open by 3 cm from nadir of left coronary cusp to nadir of noncoronary cusp. (D) Rectangular patch was sewn to mitral annulus (white arrow) at bottom and aortic annulus (white stars) on both sides, enlarging the root. (E) A 27-mm Regent mechanical valve was chosen based on 27-mm Magna Ease valve sizer touching the three nadirs of three aortic cusps. The 27-mm Regent mechanical valve was placed in the enlarged aortic root and the position was marked on the Dacron patch to guide placement of valve sutures. (F) Mark on patch was lower than divided left-noncommissural post.
A rectangular-shaped Hemashield (Maquet Cardiovascular, San Jose, CA) patch was trimmed in width slightly greater than the distance between the two cusp nadirs. This patch was sewn to the mitral annulus from left to right fibrous trigone with running 4–0 polypropylene suture. The suture line was transitioned to the undermined aortic annulus at the nadir of both left coronary and noncoronary sinuses, sutured along the longitudinal length of the patch up to the level above the divided commissural post and secured (Figure 1D).
It is difficult to use the St Jude intraannular sizer to size for the mechanical valve. Instead, we used a 27-mm Magna Ease sizer touching the three nadirs to choose a 27-mm St Jude Regent valve. The 27-mm Regent valve was placed in the enlarged root touching three nadirs of the aortic annulus, and the position of the mechanical valve on the patch was marked to guide placement of valve sutures (Figures 1E, 1F).
The pledgeted 2–0 Ethibond sutures (Ethicon Endo-Surgery, Cincinnati, OH) were placed along the native aortic annulus in an everting fashion and from outside in on the patch (Figure 2A). The mechanical valve was placed with one pivot guard facing the left-right commissural post and one facing the patch, where the sutures were tied down first (Figure 2B). After the valve was tied down, the longitudinal aortotomy was closed from proximal to distal incorporating the tapered patch (Figure 2C). The proximal aorta was then anastomosed to the distal ascending aorta.
FIGURE 2.
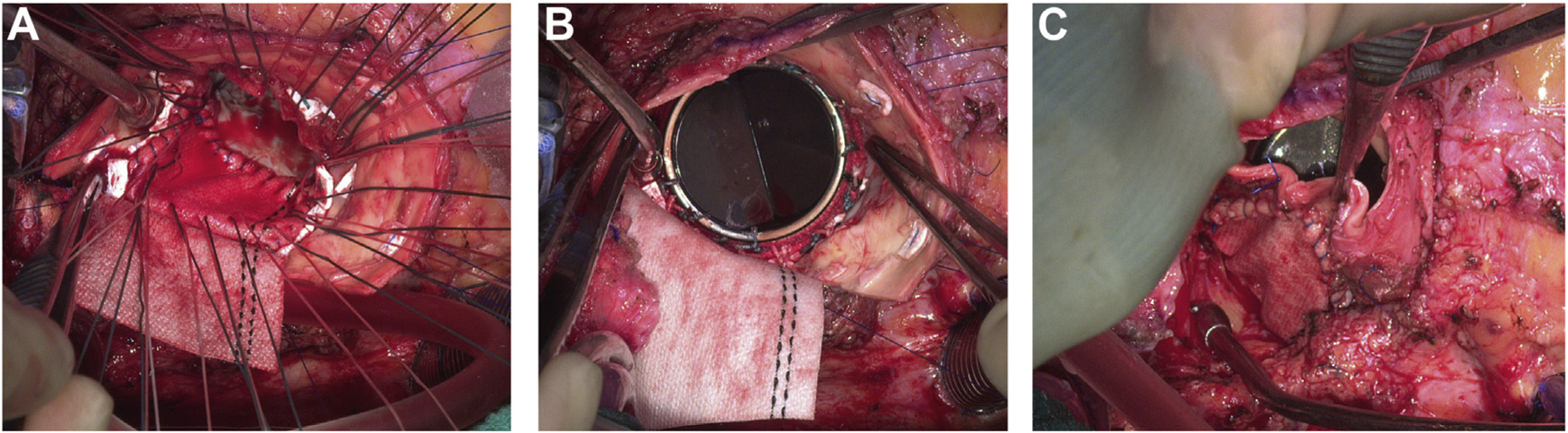
(A) Pledgeted 2–0 Ethibond sutures were placed along the aortic annulus in everting fashion and from outside in on patch. Transitional stitches were placed with one arm of suture through aortic annulus (everting: from aorta to ventricle), and the other arm through patch (one bite: inside-outside-inside). (B) Upsized Regent mechanical valve was seated intraannularly, one pivot guard facing left-right commissural post and one touching patch and two coronary ostia on each side of valve. (C) Vertical aortotomy was closed incorporating patch.
COMMENT
Patients who choose a mechanical valve often bear the hope that the AVR will be the last operation they have during their lives and that they will have high quality of life. Therefore, it is very important to give patients a large size valve for the best possible hemodynamic performance they can get.
There were some unique technical features in mechanical AVR with this root enlargement technique compared with our previous report.1 First, the methods of sizing and valve suture placement were different. Because the left ventricle outflow tract was not enlarged, it is difficult to use the St Jude valve sizer for accurate sizing. Instead, a Magna Ease valve sizer was used to size the mechanical valve by touching three nadirs of the aortic annulus. The St Jude mechanical valve was implanted in intraannular fashion with two pivot guards inside the annulus in contrast to supraannular implantation for bioprosthetic AVR.1 We used everting valve sutures for intraannular implantation and noneverting valve sutures for supraannular implantation. The valve sutures at the patch were no higher than the divided left-noncommissure post or those sutures placed at the left-right and right-noncommissure posts. It was similar to the valve suture placement in a crown-shaped native aortic annulus—the sutures at commissure posts were higher than those at the nadirs.
Second, this report emphasized the techniques in redo AVRs. Frequently, the aortomitral curtain is destroyed when the previous prosthetic valve is removed. Instead of repairing the aortomitral curtain with a triangular patch, a rectangular patch as we used in this case could simultaneously enlarge the annulus by three valve sizes. Surgeons can avoid a Konno procedure by using this technique. And third, the supplemental video demonstrates all the details of this technique, as the images in the previous video1 were not close up and some critical parts of the operation—such as how to make the Y incision and how to sew the rectangular patch—were not very clear.
In summary, because it did not require violating any adjacent structure of the aortic root, such as mitral valve or right ventricle, our technique was simpler and safer than the Manouguian and Konno procedures, and more effective than the Nicks procedure, which enlarges the annulus by one valve size, and can be very useful in young patients, including teenagers, who need a bigger mechanical valve.
Supplementary Material
REFERENCE
- 1.Yang B A novel simple technique to enlarge the aortic annulus by two valve sizes. JTCVS Tech. 2021;5:13.-. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


