Abstract
Physical exercise benefits cognitive functioning and can protect against neurodegeneration. Neighborhood environments may be pivotal to physically active aging, and thus help shape older adults’ cognitive function. This mixed-methods study investigated where older adults exercised outside the home, and whether availability of these neighborhood sites was associated with cognitive function. We thematically analyzed qualitative data from semi-structured interviews in 2015 with 125 older adults (mean age = 71) in the Minneapolis (MN) metropolitan area. Results identified nearby public parks, fitness/sports amenities, and walkable destinations as motivators for recreational exercise and active transit among participants. These findings informed quantitative analysis of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, a national sample of older Black and White Americans (n = 21,151; mean age at assessment = 67; data collected 2006-2017). We used generalized additive multilevel models to examine whether neighborhood features that qualitative participants identified as encouraging physical activity were associated with elevated levels of cognitive function. Results indicated that residing in neighborhoods with greater availability of local parks, access to recreational amenities, and business density was associated with higher levels of cognitive function. We found no evidence to suggest a significant association between availability of these neighborhood resources and rate of cognitive decline. This study identifies specific neighborhood active aging infrastructure that may support cognitive function among older adults aging in place.
Keywords: Neighborhood environment, aging in place, physical activity, leisure, cognitive aging, mixed-methods
Introduction
The health benefits for older adults who engage in moderate-to-vigorous physical activity are widely recognized. Regular exercise can positively influence cognitive ability, limit cognitive aging, and reduce risk for Alzheimer’s disease and related dementias.1-3 The neuro-protective pathways in which exercise may maintain cognitive functioning include neurogenesis and neuroplasticity, improved cardiovascular function and associated influence on the cerebrovascular system, reduced stress and anxiety, reduced inflammation, and improved insulin sensitivity.4
Emerging research also points to the importance of neighborhood environments for cognitive aging. Neighborhoods expose residents to pollutants and influence behaviors related to cognition such as walking, diet, and social engagement.5-7 Urban density, walkability, parks, and green space have been associated with better cognition, lower risk for Alzheimer’s disease and dementia, and slower cognitive decline in older adults.5,8-15 Greater land use mix was associated with lower odds of dementia.11 These neighborhood features can support opportunities to be physically active.16 They may be especially important to older adults, who tend to spend more time in their immediate surroundings,17 to encourage exercise such as walking for pleasure or errands.18
The potential role of neighborhood active aging infrastructure in cognitive aging is still emerging, and evidence is particularly limited in sociodemographic diversity and geographic scope. In this mixed-methods study, socioeconomically and racially diverse older adults living in a range of urban and suburban neighborhoods expressed that nearby parks, fitness/sports amenities, and walkable destinations encouraged regular exercise. The qualitative findings extend understanding of perceptions and usage of active aging infrastructure. This prompted testing whether these neighborhood resources supported cognitive function in a large national aging cohort of Black and White adults. In addition to validating emerging links between parks, walkable destinations, and later-life cognitive outcomes in a diverse longitudinal sample, this study is the first to our knowledge to test associations between access to fitness/sports amenities and cognition. The findings contribute new evidence to the emerging ecological model of cognitive health,19 and inform active aging health promotion at the neighborhood scale.
Methods
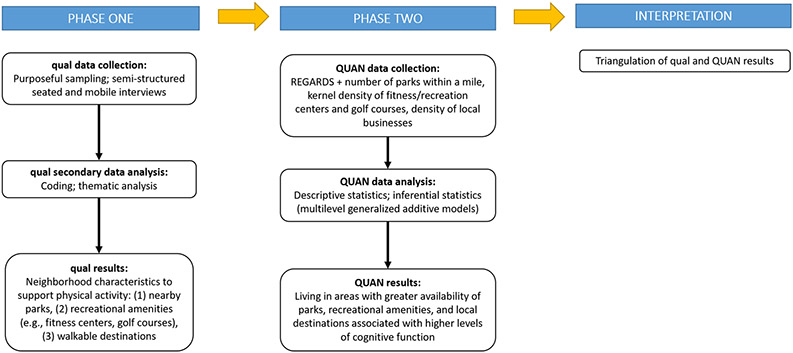
In Phase I, we collected and analyzed qualitative data, which generated the hypothesis that specific neighborhood infrastructure—local parks, recreational amenities, and nearby destinations—are associated with cognitive function by encouraging regular physical activity among older residents. In Phase II, we tested this hypothesis in the in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study sample (Figure 1).
Figure 1.
Exploratory sequential mixed-methods study design.
Phase I: Aging in the Right Place Study
This research investigated how older adults perceived and navigated aging in place across three case study areas in the Minneapolis (Minnesota) metropolitan area (Supplementary Figure 1). Participants volunteered in response to flyers placed in senior centers, residential buildings, sites of worship, civic group newsletters, and health fairs. Eligibility criteria included at least 55 years old, independent-dwelling, and demonstrated cognitive capacity to participate. The University of Minnesota Institutional Review Board approved study procedures, and all participants provided written informed consent.
Lead author JF conducted semi-structured interviews with 125 older adults in 2015. Questions probed for daily routines, social interactions, service provision, and well-being (Supplementary Table 1).20-22 Audio-recorded interviews ranged from 30-90 minutes. 96 participants engaged in a mobile interview that was on average 17 minutes and 0.86 kilometers.
Audio files were professionally transcribed verbatim, and materials organized in NVivo 12. The guiding research question was: How and where did participants exercise outside of their homes? JF thematically analyzed the data: familiarization, generation of initial codes, search for themes, review, define themes, and write-up.23 Debriefing, member checking, persistent observation, negative case analysis, and audit trails enhanced transparency and credibility in the analysis.24
Phase II: REGARDS Study
REGARDS is a national prospective cohort study investigating racial differences in stroke and cognitive function. Investigators recruited 30,329 Black and White community-dwelling adults, aged 45+ (mean age 64), from 2003-2007.25 Baseline telephone interviews collected socio-demographics, behavioral information, and medical history for respondents. A cognitive battery, first implemented in 2006, was conducted during follow-up calls at 2-year intervals. Study investigators at the University of Alabama at Birmingham (UAB) document residential addresses over the follow-up period. The study procedures are reviewed and approved annually by the UAB, and all participants provided written informed consent.
Measures
Cognitive Function.
Cognitive testing to detect late-life cognitive decline often involves a battery of tests assessing multiple cognitive domains.12 We captured global cognitive function through five validated measures of verbal learning, memory, orientation, language, and executive function.26-29 Executive function and episodic memory are components of cognition that can show early and consistent decline with age.30-32 We used a confirmatory factor analysis of all five tests: see Table 1 and Supplementary Figure 2 for further details on the cognitive tests and the factor structure of the model. Standardized factor scores were output for each participant at each assessment and used in all subsequent analyses, with higher scores indicating better cognition.
Table 1.
Cognitive battery tests contributing to the global cognitive function factor score.
| Cognitive Test | Score Range | Mean Score (±SD) | Cognitive Domain |
|---|---|---|---|
| Animal Fluency Test (AFT) | Number of unique animals named in 1 minute (range 0-59) | 16.1 (5.7) | Language and executive function |
| Letter Fluency Test (LF) | Number of unique words beginning with the letter “F” named in 1 minute (range 0-38) | 10.8 (4.7) | Language and executive function |
| World List Learning (WLL) | 0-30 | 17.6 (5.3) | Verbal learning |
| Word List Delayed (WLD) | 0-10 | 6.6 (2.2) | Verbal memory |
| Montreal Cognitive Assessment (MoCA) subset a | 0-11 | 9.6 (1.7) | Verbal memory and orientation |
Note. Higher scores on each cognitive test indicate better cognitive functioning. Factor loadings ranged from 0.43 (MoCA) to 0.79 (AFT), and model fit improved when allowing for correlated error among the memory items (WLL, WLD, MoCA) (Root Mean Square Error of Approximation=0.013; Comparative Fit Index=0.999).
MoCA subset: 5-word delayed memory recall, 6-item orientation
Neighborhood Context.
Our measures of neighborhood active aging infrastructure are based upon the Phase I results. Because qualitative study participants suggested that both proximity and availability was important to usage, we calculated the number of parks within a 1-mile radius of REGARDS participants’ home addresses from the ParkServe 2018 database.33 For recreational amenities, we used the National Establishment Time-Series (NETS) longitudinal database.34 We selected all records for North American Industry Classification System (NAICS) codes 713910 (golf courses) and 713940 (fitness and recreational sports centers) over the 12-year study period.35 We applied a kernel density method:36 the surface value was highest at the exact location of each recreational amenity, and diminished in value over a 1-mile circular buffer. We summed any overlapping recreational kernel density values at the location of each participant’s home to develop a distance-weighted average of nearby recreational amenities. A high kernel value represented multiple sites in close proximity. Business density captured the qualitative result of walkable destinations. We spatially joined and counted all businesses in the NETS database aside from heavy industry (NAICS codes 11-33), and then divided by the census tract’s land area (data retrieved from the National Neighborhood Data Archive).37 We log transformed business density and square root transformed park count and recreational amenity kernel density to rein in potential high leverage observations.
Covariates.
Demographic characteristics associated with cognitive function—including age (at first assessment; centered at 65 years); gender (male; female); race (Black; White), educational attainment (less than high school diploma; high school diploma; some college; college degree or more) were incorporated as controls. Years of follow-up from baseline cognitive test and an indicator for a respondent’s first cognitive test (0 if first test; 1 if subsequent test) were also considered as controls to adjust for changes in cognitive function with age and potential practice effects associated with re-testing.38 Neighborhood-level covariates—derived from the 2008-2012 and 2013-2017 American Community Surveys—included proportion of a census tract population living below the poverty line; proportion of a census tract population that is Non-Hispanic Black; and proportion of housing units in a tract that are owner occupied.39
Analytical Sample
REGARDS respondents who participated in at least one data collection point between 2006-2017 comprised our sample. Respondents varied in when they contributed their first cognitive score, with the majority contributing their first test between 2006-2008. Most respondents were tested 3-5 times over this interval. To match the qualitative data, we restricted the sample to individuals living in urban areas (identified by Rural-Urban Commuting Area Codes as “urban core” or “other urban”).40 Our final analytic sample included 21,151 individuals with 73,228 observations.
Analysis
To examine how cognitive function varied among respondents living in areas with different levels of active aging infrastructure, we fit a Gaussian generalized additive multilevel model (GAMM) to the REGARDS sample. We regressed respondents’ cognitive test scores on neighborhood park count; recreation amenity kernel density; and business density while also controlling for the demographic and neighborhood-level covariates described above. To allow for potential nonlinear associations among our response and focal predictors, we modeled each neighborhood physical activity resource using thin-plate regression splines.41 These penalized splines balance accurate estimates of nonlinear associations with model parsimony. This approach allowed us to discover well-supported, complex patterns hidden in the sample while avoiding overfitting.
To leverage the entire sample to describe the association between cognitive function and active aging infrastructure, we included additional model parameters to explicitly account for the longitudinal design. To account for changes in respondents’ cognitive function as they aged throughout the survey, we controlled for years from baseline test. To allow for the association between time and cognitive function to vary by respondent, we also included a subject-specific random slope for years from baseline test. To account for the fact that respondents contributed multiple, uneven numbers of cognitive tests to the sample, we included subject-specific random intercepts.42 To model potential practice effects, we included a binary indicator of whether a test was a respondent’s first.38 To account for the spatial clustering of respondents within tracts, we also included random, tract-specific intercepts. The inclusion of these additional parameters allowed us to summarize the general association between cognitive function and neighborhood resources while simultaneously: (1) not discarding salient data; and (2) accounting for several aging, spatial, and testing-related effects. Models were fit using gamm443 in the R statistical programming language.a,44
Results
Qualitative
Table 2 shows characteristics of the qualitative sample. The average age was 71 years. Two-thirds of the sample were female, participants were largely White or Black, one-third were married, and 43% had at least some college education. Thematic analysis generated three primary neighborhood features that supported and encouraged regular exercise: nearby parks, recreation centers, and destinations (Table 3).
Table 2.
Descriptive statistics of qualitative sample (n = 125): Aging in the Right Place Study (2015).
| Measure | Mean or % |
|---|---|
| Age (in years) | 71.3 (SD=7.8) |
| Female | 67% |
| Race/ethnicity: White | 57% |
| Race/ethnicity: Black | 25% |
| Race/ethnicity: Other | 18% |
| Married | 34% |
| Education: High school or less | 57% |
Note. SD denotes standard deviation. “Other” self–identified races/ethnicities include (in alphabetical order) African, American Indian, Arabic, Asian, Bohemian, French, German, Hispanic/Latin American, Irish, Jewish, Norwegian, Polish, Swedish.
Table 3.
Qualitative thematic analysis of active aging neighborhood infrastructure: Aging in the Right Place Study (2015).
| Neighborhood feature |
Summary of findings | Exemplar Quotes |
|---|---|---|
| Parks | Local parks and paved trails were popular places to walk. Additional physical activities included bicycling, dog-walking, and skiing. Nearby neighborhood parks and small ‘pocket parks’ were favorite places to exercise and informally socialize. Heavily-wooded parks and large nature preserves were less frequented given distance and safety concerns. Fall risk and lack of safety from crime dissuaded park use, particularly among low-income neighborhoods. Participants requested supportive senior-specific park infrastructure to encourage park usage and exercise. |
Rhonda (85y): I walk through the park all the time, and [it] keeps changing. There’s always some event or affair going on… Once in the park, I was cutting through the park and it was solid ice. I had no traction. I ended up getting down on my knees and getting through the ice puddle. I couldn't maneuver it… And nobody came along to help. Just when you wanted somebody. Annie (83y): There are walking trails along the river, I use those a great deal. Warren (65y): I’d like a pool. I know that I have the use of the community center, but that’s three miles away. I would like a more neighborly park. We have a kids’ park relatively close down the street, but nothing really for seniors. Pamela (61y): We have this park over here, and there is nothing for seniors. It's got two tennis courts. Which are never used. In one court, I've asked for years, can they make a pickleball [court] for seniors? Barbara (67y): I used to walk the trails here but… it's a little scary walking the trails now [given the perceived risk of being mugged or attacked in the heavily-forested area]. |
| Fitness and sports recreation centers | Gyms, swimming pools, tennis courts, and golf courses were valued places to exercise and socialize among select participants. Affluent participants living in condominiums and townhomes utilized on-site private facilities such as gyms and pools. Participants with disabilities particularly appreciated pools for low-impact exercise and rehabilitation. |
Ingrid (66y): They built a YMCA for us 50-plus … The people there, we’re all older. It’s just like a big social club. We work out, but we also laugh and have fun. It’s just a bunch of old people getting together and hanging out. I always felt that laughter is very healthy for you. I feel rejuvenated going there, both mentally and spiritually. It’s just like a safe haven to go to, plus we get healthy. Barbara (67y): [The fitness center] has an indoor pool, so now I’ve got swimming year-round. Besides the indoor pool has a Jacuzzi, sauna, and a full workout [gym]. I mean everything. That has become my life. I go five days a week. In the winter, their indoor pool is 95 degrees. I feel like I’m in a resort area. Kurt (82y): I’m able to play some golf still, and that gets me out of the house… I golf every Monday, so I see those guys. Denise (72y): [Pool exercise] is the only exercise I really can do without hurting my back… I’ve got friends there and I like the exercise… It’s wonderful. It's warm water… I'm pain-free for an hour of the day when I'm there. |
| Walkable destinations | Nearby destinations motivated everyday walking for leisure and exercise. Pedestrian infrastructure, such as wide and smoothly-paved sidewalks, long-timed crosswalks, and indoor walkways, encouraged active transit to services and amenities. Low-density suburban-dwelling participants often drove regularly for appointments, groceries, and socializing given lack of walkable destinations. Low-income participants were less likely to walk from home for leisure or exercise given lack of safety and nearby destinations. |
Salma (67y): I like walking, especially in the spring and the summer and autumn. It’s so good to walk and get around and go to the shops around here, nearby. I enjoy. Michael (73y): Everything’s walking distance for me. I hardly drive anymore… I’m willing to walk to [the big-box store]. In fact, I consider that a good motivation for doing my walking to stay fit… I’m so grateful for the skyway because then we can walk during the long cold months and walk a half hour every day. Maggie (69y): It’s a suburb, so it’s quite far away from things. It’s the first time I had to drive to a grocery store, you know what I mean? I was used to [living] just within a mile you had grocery stores, doctors, and everything. Here … you just have to be able to drive. Thelma (66y): That's something, as I age, I'm not thrilled with. That there aren't a lot of places I can walk to. Harry (75y): [Services] are close enough to be convenient in the car, but it would be nice to be able to walk to the grocery store or walk to a coffee shop or a bar or something. I sort of miss that. That's the disadvantage of living in a suburb, you know. |
Parks.
Local parks and trails were popular places to walk. Sharon (65y) walked to and around a nearby park “all the time,” while Thomas (67y) frequented a trail “because it’s so close.” Participants such as Brady (60y) and Warren (65y) bicycled regularly to local parks and lakes, while Maggie (69y) described cross-country skiing during wintertime looping the park visible from her back window.
Positive park recreation was common among downtown and suburban participants living in areas with heavy park investment and activity. In contrast, participants who resided in low-income areas less-frequently described park usage. Some took grandchildren to play in local playgrounds, but others noted that nearby parks were unsafe. Suburban participants such as Warren (65y) expressed desires for senior-specific amenities including a pool, chess boards, benches to rest and talk, shady trees, and quiet areas. Pamela (71y) requested pickleball courts and outdoor park exercise classes to stay motivated and engaged in exercise.
Fitness and recreation centers.
Many female participants visited a recreation center recently constructed in a low-income neighborhood regularly to exercise and socialize. They appreciated age-appropriate classes, subsidized rates, and socio-culturally relevant activities for Black attendees. Victoria (65y) attended six times a week to walk four miles and take cycling, core, and cardio classes.
Affluent condo-dwellers such as Joey (89y) and Michelle (74y) described exercising in private association facilities including fitness centers, swimming pools, and tennis courts. Suburban homeowners Oliver (73y) and Harry (75y) used a local fitness center several times a week, though both were careful on the treadmill given health and mobility concerns. Wheelchair-bound Gary (83y) had felt unmotivated over the past four years to exercise, but his goal was to return to the nearby municipal recreation center. His inspiration was a 90-year-old friend who played tennis there three times a week.
Male participants more-often mentioned playing tennis and golf. Their activities blended exercise and socialization, as explained by Brad (81y): “I usually play tennis a few times a week, so I see there a total of 10, 9 guys… Whether you win or lose, I tell the guys, it’s mostly about getting out there.” Low-mobility participants expressed particular appreciation for swimming as an “easier on the joints exercise” (Linda, 69y). Jim (55y) demonstrated his route traveled by motorized scooter early each weekday to swim at a local pool during the mobile interview. Denise (72y) took assisted mobility transit to a pool at least four times per week to engage in a physical therapy routine, water-walking, and balance exercises. It was an anchor point in her daily life to move and socialize.
Destinations.
Having nearby destinations and people to encounter in and around these places encouraged many participants to be more active. Salma (67y), a recent immigrant residing in subsidized housing, enjoyed walking regularly around the shops of her neighborhood. Spouses Michael (73y) and Penny (64y) loved living on the edge of downtown because they had numerous restaurants, stores, a library, sports stadiums, and sites of arts and entertainment in close proximity. The “perfect mixture” of nature and urban culture motivated Penny, while Michael walked up to five miles a day through frequent errands. Walking in high-density service areas to soak up the “hustle and bustle” made him feel less lonely and bored.
Destination-based walks were popular, and the reason why Oliver (73y) walked regularly to the nearby coffee shop, grocery store, and barber shop. Kim (71y) was proud to walk a mile daily to the senior center for yoga and cardio classes. Kurt’s (82y) “idea of a walk” was up to a coffee shop and back, while his wife Michelle (74y) walked “someplace more interesting”, such as around the art center. Low-density suburban-dwelling participants more often drove for appointments, groceries, and socializing. Cynthia (62y) joked: “I’m fat (laughter). We need to get more exercise,” while her husband Charles (71y) was unable to walk a mile. They lamented the lack of walkable services.
Few low-income participants exercised regularly from home. Several mentioned that their neighborhoods were undesirable and unsupportive of walking and cycling, such as lack of destinations, broken sidewalks, and risk of crime. Others preferred to drive to the local YMCA and other places for exercise classes and walking groups. Local opportunities for both active transport and enjoyable recreation were limited.
Quantitative
Characteristics of the quantitative sample are displayed in Table 4. The average cognitive function score across all observations was 0.015 (SD = 2.355). Forty percent of the sample was Black; more than half identified as female; and the average respondent was 67 years old (SD=8.83) during their first cognitive test. Respondents lived in 12,669 unique metropolitan tracts with varying levels of active aging infrastructure.
Table 4.
Descriptive statistics of quantitative sample: Reasons for Geographic and Racial Differences in Stroke Study (2006-2017).
| Variable | Mean/proportion | Std. deviation |
|---|---|---|
| Cognitive function score | 0.015 | 2.355 |
| Number of parks | 3.819 | 6.086 |
| Businesses per square mile | 260.941 | 658.704 |
| Recreation center kernel density | 3e-07 | 9e-07 |
| Age (at baseline test, in years) | 66.995 | 8.825 |
| Black | 0.398 | - |
| Female | 0.556 | - |
| Education: less than high school | 0.089 | - |
| Education: high school | 0.237 | - |
| Education: some college | 0.269 | - |
| Education: college degree or higher | 0.405 | - |
| Census tract: proportion of housing owner occupied | 0.634 | 0.205 |
| Census tract: proportion non-Hispanic Black | 0.425 | 0.351 |
| Census tract: proportion earning below poverty line | 0.188 | 0.133 |
| Years since baseline test | 3.445 | 3.177 |
| Number of cognitive tests contributed to sample | 3.462 | 1.713 |
Note. Respondents (n = 21,151) contributed 73,228 observations to the sample and were clustered within 12,669 unique census tracts. Summaries for recreation center kernel density are given in scientific notation, given their scale relative to the other covariates. 53% of respondents contributed between 3 to 5 cognitive tests to the sample. 16% of respondents contributed only 1 test, while 4% of respondents contributed 7 tests. No respondent contributed more than 7 cognitive test the data.
Table 5 displays our GAMM of cognitive function. This table includes parameter estimates for the parametric and random terms, and summarizes the complex, multidimensional smooth terms using p-values and effective degrees of freedom. According to our model, neighborhood business density (p-value=<0.001); park count (p-value=<0.001); and recreation center kernel density (p-value=0.022) were all significant predictors of respondents’ cognitive function.
Table 5.
(Gaussian) generalized additive multilevel model of cognitive function: Reasons for Geographic and Racial Differences in Stroke Study (2006-2017).
| Parametric terms: | |||
|---|---|---|---|
| parameter | estimate | std. error | t-value |
| Intercept | 0.472 | 0.070 | 6.786 |
| Age at baseline test | −0.093 | 0.001 | −76.230 |
| Years from baseline test | −0.078 | 0.003 | −28.087 |
| White | 0.945 | 0.030 | 31.236 |
| Male | −0.342 | 0.022 | −15.219 |
| Education: college degree (ref.) | - | - | - |
| Education: some college | −0.678 | 0.028 | −24.275 |
| Education: high school | −1.171 | 0.029 | −39.902 |
| Education: less than high school | −1.774 | 0.041 | −43.166 |
| Tract, proportion owner occupied housing | 0.309 | 0.071 | 4.332 |
| Tract, proportion non-Hispanic Black | −0.134 | 0.045 | −2.978 |
| Tract, proportion below poverty line | −0.342 | 0.109 | −3.136 |
| First test indicator (0: first test; 1: second test+) | 0.059 | 0.016 | 3.630 |
| Random terms: | |||
| parameter | std. deviation | ||
| Person-specific intercepts | 1.259 | ||
| Person-specific time slopes | 0.127 | ||
| Tract-specific intercepts | 0.256 | ||
| Smooth terms: | |||
| parameter | EDF | p-value | |
| (log) Business density | 1.000 | < 0.001 | |
| (square root) Recreation center kernel density | 1.003 | 0.022 | |
| (square root) Park count | 3.706 | < 0.001 | |
Note. EDF denotes “effective degrees of freedom” and summarizes the number of parameters associated with each smooth. Ref. indicates “reference category.” For reference, the Akaike information criterion (AIC) of a model that excluded all three measures of active ageing infrastructure was 286,982.3, while the AIC of a model that included all three as smooth terms (as presented in Table 5) was 286,876.0.
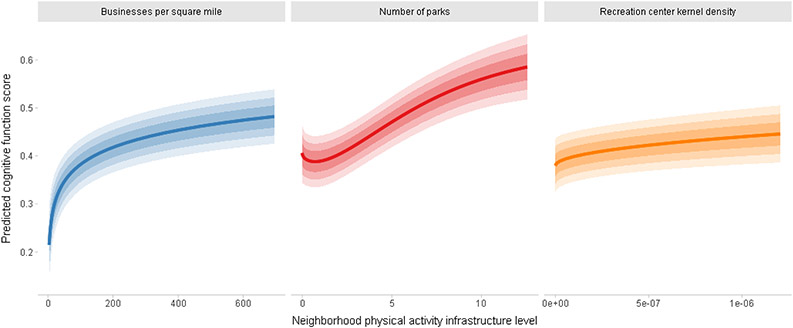
For a better understanding of the substantive implications of our model, Figure 1 presents predicted cognitive test scores for individuals between the 5th to 95th percentiles of each active aging resource. The first panel of Figure 1 displays a positive association among neighborhood business density and cognitive function. Respondents living in areas with business densities near the 5th percentile of the sample distribution had predicted cognitive test scores of approximately 0.215. In contrast, respondents living in areas that were most densely packed with businesses—i.e., those near the 95th percentile of observed business density values—had expected cognitive scores of 0.482. This 0.27-point difference in cognitive scores approximates 3-years of age in our estimated model (where a 1-year increase in age corresponds to a 0.09-point decrease in cognitive function).
Figure 1 also illustrates a positive association among cognitive function and both the number of parks and kernel density of recreation amenities in a respondent’s surrounding environment. With all other variables held at their sample medians, individuals who had zero parks within 1-mile of their home had predicted cognitive function scores of 0.406, while individuals who lived in areas with 12 nearby parks had expected cognitive scores of 0.585. Similarly, respondents living in areas near the bottom of the observed distribution of recreation amenity densities had predicted cognitive scores of 0.380, while respondents who resided in areas near the top of this distribution displayed expected cognitive function scores of 0.446.
Discussion
Using an innovative mixed-methods approach, we identified that neighborhood active aging infrastructure is significantly related to level of cognitive function among older American adults. The number of studies investigating neighborhood built and social environments and late-life cognitive health has recently increased, but evidence to-date is extremely limited—particularly in diversity, geographic scope,12 and longitudinal follow-up. Our results build evidence that neighborhoods may be associated with opportunities to be more physically active and cognitively healthy in later life5,6,8-12,45 in two racially- and geographically-diverse samples. A primary strength of the study is its mixed-methods design.46-48 Rich qualitative insights extend understanding of neighborhood motivations and barriers to be physically active among socioeconomically and racially diverse older adults. This directly informed quantitative inquiry to validate and extend understanding of neighborhood determinants of cognitive function in a large, diverse, national sample.
Consistent with previous research,16 physical activity among qualitative study participants often occurred close to home and through walking for recreation and active transport. Local parks were highly-discussed places to exercise, which confirms existing literature finding positive associations between park proximity and physical activity among older adults.49,50 The quantitative results corroborated this: study respondents living in areas with a greater number of parks displayed elevated levels of cognitive function relative to their peers. Our finding deepens limited parks-cognition research among older adults. In three previous studies investigating associations between neighborhood park space and late-life cognition, a cross-sectional Chicago study found no association with global cognition;51 a Scottish longitudinal study found that greater early-life neighborhood park space was associated with slower cognitive decline;13 and a cross-sectional study of six US cities/counties found that park space was associated with better processing speed in the overall sample, but associations with global cognition varied by geography.12
Quantitative study respondents living in areas with greater density of businesses also displayed higher cognitive functioning. This corroborates related research finding positive associations between urban density, walkability, and better cognition in older adults.5,11,15 It also converges with the qualitative results where participants discussed destination-based walking for exercise, errands, and pleasure, such as to coffee shops, grocery stores, senior centers, and art shows. Some urban walkability indices account for retail and services.52 Previous research supports that older adults frequent local malls and commercial areas to walk, including indoor mall walking during inclement weather.16,22,49,53 Our findings suggest that these sites encouraging routine walking, as well as social interaction and civic engagement therein, may protect cognitive function. Being physically and socially active can enhance cognitive reserve and maintain or improve cognitive functioning.1-4
Because our qualitative results identified the role of nearby fitness/recreational amenities to encourage physical activity, this study is the first to our knowledge to test the local availability of such places and cognition. We found that recreation center kernel density was a significant predictor of cognitive function, suggesting that these sites may encourage cognitive-enhancing lifestyle activities including exercise.3,54,55
In our supplementary longitudinal analyses, neighborhood active aging infrastructure was not significantly associated with cognitive decline. As such, the results should be considered hypothesis-generating for further investigation. Both samples did not include perspectives from those residing in residential long-term care facilities or rural environments. Minneapolis heavily invests in active infrastructure including parks and public transit. Interviews did not explicitly ask participants about their cognitive health in relation to everyday behaviors and neighborhood contexts. In the quantitative analysis, we cannot rule out potential sources of selection bias due to unmeasured variables (e.g., wealth). The results are descriptive associations, rather than causal processes. Future research, which may utilize rich longitudinal data describing how respondents’ cognitive function and access to physical activity-promoting neighborhood environments co-evolved over the lifespan, is needed to make more definitive statements about potential causal relationships between active aging infrastructure and cognitive health.
Additionally, the quantitative study is limited by some degree of slippage between underlying concepts and our quantitative measures. For instance, the number of neighborhood parks may not be the sole or best indicator of park access among older adults. Additional dimensions such as distance to nearest part, amount of park space, and park quality may provide further insights. Likewise, businesses per square mile averages many different business types, some of which may be more or less salient destinations for older adults. Our models also assume that the association between neighborhood features is fixed across metropolitan regions. These associations likely vary by socio-geographic context.12
Conclusion
Nearly six million people in the US are currently living with Alzheimer’s dementia,56 and around 50 million people worldwide.57 It is critical to better understand how neighborhood environments may benefit cognition and help buffer against cognitive decline. Given that availability of parks, fitness/recreation centers, and walkable destinations was associated with higher cognitive functioning in this study, future research investigating causal mechanisms may inform policy decisions and community interventions regarding resource allocation and urban development to support aging populations. This includes park infrastructure and recreational amenities for users of all ages and abilities, and strategically blending residential and commercial areas. Frequent benches, shady trees, quiet nature areas, pickleball courts, park chess boards, smoothly-paved sidewalks and trails, accessible community pools, social golf and tennis leagues, senior-specific indoor and outdoor exercise classes, and subsidized gym rates may encourage higher physical activity levels among aging residents. Neighborhood features that support safe, social, and accessible exercise may promote physical and cognitive health in later life.
Supplementary Material
Figure 2.
Predicted cognitive function scores for individuals between the 5th to 95th percentiles of each active aging resource.
Note: Shaded regions represent 50%, 75%, and 90% uncertainty intervals.
Highlights.
Mixed-methods study linking neighborhoods to physical activity and cognitive aging
Parks, fitness amenities, walkable destinations motivated physically active aging
These sites were associated with higher cognitive function in diverse older adults
Acknowledgements
This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the NIA. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at: https://www.uab.edu/soph/regardsstudy/. Additional funding for this project was provided by NIH/NIA grant 1RF1AG057540-01 (Clarke, PI), the Michigan Institute for Clinical & Health Research Postdoctoral Translational Scholar Program UL1 TR002240-02 (Finlay), and NIH/NIA Ruth L. Kirschstein National Research Service Award Individual Postdoctoral Fellowship F32 AG064815-01 (Finlay).
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
As an additional analysis, we also examined whether individuals’ cognitive function over time was conditional on their access to active aging infrastructure. Details of this analysis can be found in the supplemental materials.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mandolesi L, Polverino A, Montuori S, et al. Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Front Psychol. 2018;9:509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fernandes J, Arida RM, Gomez-Pinilla F. Physical exercise as an epigenetic modulator of brain plasticity and cognition. Neurosci Biobehav Rev. 2017;80:443–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baumgart M, Snyder HM, Carrillo MC, Fazio S, Kim H, Johns H. Summary of the evidence on modifiable risk factors for cognitive decline and dementia: A population-based perspective. Alzheimers Dement. 2015;11(6):718–726. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy G, Hardman RJ, Macpherson H, Scholey AB, Pipingas A. How Does Exercise Reduce the Rate of Age-Associated Cognitive Decline? A Review of Potential Mechanisms. J Alzheimers Dis. 2017;55(1):1–18. [DOI] [PubMed] [Google Scholar]
- 5.Besser L, Galvin JE, Rodriguez D, et al. Associations between neighborhood built environment and cognition vary by apolipoprotein E genotype: Multi-Ethnic Study of Atherosclerosis. Health & place. 2019;60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finlay J, Esposito M, Tang S, et al. Fast-food for thought: Retail food environments as resources for cognitive health and wellbeing among aging Americans? Health & place. 2020;64:102379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Finlay J, Esposito M, Li M, et al. Can Neighborhood Social Infrastructure Modify Cognitive Function? A Mixed-Methods Study of Urban-Dwelling Aging Americans. Journal of Aging and Health. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Besser LM, McDonald NC, Song Y, Kukull WA, Rodriguez DA. Neighborhood Environment and Cognition in Older Adults: A Systematic Review. American journal of preventive medicine. 2017;53(2):241–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown SC, Perrino T, Lombard J, et al. Health Disparities in the Relationship of Neighborhood Greenness to Mental Health Outcomes in 249,405 U.S. Medicare Beneficiaries. Int J Environ Res Public Health. 2018;15(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clarke PJ, Weuve J, Barnes L, Evans DA, Mendes de Leon CF. Cognitive decline and the neighborhood environment. Ann Epidemiol. 2015;25(11):849–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu YT, Prina AM, Jones AP, et al. Community environment, cognitive impairment and dementia in later life: results from the Cognitive Function and Ageing Study. Age Ageing. 2015;44(6):1005–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Besser LM, Hirsch J, Galvin JE, et al. Associations between neighborhood park space and cognition in older adults vary by US location: The Multi-Ethnic Study of Atherosclerosis. Health & place. 2020;66:102459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cherrie MPC, Shortt NK, Mitchell RJ, et al. Green space and cognitive ageing: A retrospective life course analysis in the Lothian Birth Cohort 1936. Soc Sci Med. 2018;196:56–65. [DOI] [PubMed] [Google Scholar]
- 14.Guo Y, Chan CH, Chang Q, Liu T, Yip PSF. Neighborhood environment and cognitive function in older adults: A multilevel analysis in Hong Kong. Health & place. 2019;58:102146. [DOI] [PubMed] [Google Scholar]
- 15.Cassarino M, O'Sullivan V, Kenny RA, Setti A. Environment and cognitive aging: A cross-sectional study of place of residence and cognitive performance in the Irish longitudinal study on aging. Neuropsychology. 2016;30(5):543–557. [DOI] [PubMed] [Google Scholar]
- 16.Chaudhury H, Campo M, Michael Y, Mahmood A. Neighbourhood environment and physical activity in older adults. Soc Sci Med. 2016;149:104–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haselwandter EM, Corcoran MP, Folta SC, Hyatt R, Fenton M, Nelson ME. The built environment, physical activity, and aging in the United States: a state of the science review. J Aging Phys Act. 2015;23(2):323–329. [DOI] [PubMed] [Google Scholar]
- 18.Finlay J, Franke T, McKay H, Sims-Gould J. Therapeutic landscapes and wellbeing in later life: Impacts of blue and green spaces for older adults. Health & place. 2015;34:97–106. [DOI] [PubMed] [Google Scholar]
- 19.Cerin E. Building the evidence for an ecological model of cognitive health. Health & place. 2019;60. [DOI] [PubMed] [Google Scholar]
- 20.Finlay JM, Bowman JA. Geographies on the Move: A Practical and Theoretical Approach to the Mobile Interview. The Professional Geographer. 2017;69(2):263–274. [Google Scholar]
- 21.Finlay JM, Kobayashi LC. Social isolation and loneliness in later life: A parallel convergent mixed-methods case study of older adults and their residential contexts in the Minneapolis metropolitan area, USA. Soc Sci Med. 2018;208:25–33. [DOI] [PubMed] [Google Scholar]
- 22.Finlay JM, Gaugler JE, Kane RL. Ageing in the margins: expectations of and struggles for ‘a good place to grow old’ among low-income older Minnesotans. Ageing & Society. 2018;40(4):759–783. [Google Scholar]
- 23.Braun V, Clarke V. Using Thematic Analysis In Psychology. Qualitative Research in Psychology. 2006;3(2):77–101. [Google Scholar]
- 24.Marshall C, Rossmann G. Designing qualitative research. 6th Edition ed. Newbury Park, CA: Sage; 2016. [Google Scholar]
- 25.Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3): 135–143. [DOI] [PubMed] [Google Scholar]
- 26.Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD): Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology. 1989;39(1159–1165). [DOI] [PubMed] [Google Scholar]
- 27.Hachinski V, Iadecola C, Petersen RC, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37(9):2220–2241. [DOI] [PubMed] [Google Scholar]
- 28.Lucas JA, Ivnik RJ, Smith GE, et al. Mayo's Older African Americans Normative Studies: norms for Boston Naming Test, Controlled Oral Word Association, Category Fluency, Animal Naming, Token Test, WRAT-3 Reading, Trail Making Test, Stroop Test, and Judgment of Line Orientation. Clin Neuropsychol. 2005;19(2):243–269. [DOI] [PubMed] [Google Scholar]
- 29.Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. JAGS. 2005;53:695–699. [DOI] [PubMed] [Google Scholar]
- 30.Kirova AM, Bays RB, Lagalwar S. Working memory and executive function decline across normal aging, mild cognitive impairment, and Alzheimer's disease. Biomed Res Int. 2015;2015:748212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hayes SM, Alosco ML, Hayes JP, et al. Physical Activity Is Positively Associated with Episodic Memory in Aging. J Int Neuropsychol Soc. 2015;21(10):780–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baudic S, Barba GD, Thibaudet MC, Smagghe A, Remy P, Traykov L. Executive function deficits in early Alzheimer's disease and their relations with episodic memory. Arch Clin Neuropsychol. 2006;21(1):15–21. [DOI] [PubMed] [Google Scholar]
- 33.Trust for Public Land. ParkServe shapefiles. In: ParkServe, ed. Trust for Public Land (2018b). Parkserve shapefiles (October 8, 2018) [Data set]. 2018. [Google Scholar]
- 34.Finlay J, Esposito M, Kim MH, Gomez-Lopez I, Clarke P. Closure of 'third places'? Exploring potential consequences for collective health and wellbeing. Health & place. 2019;60:102225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Census Bureau. North American Industry Classification System. 2019; https://www.census.gov/eos/www/naics/.
- 36.Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. International Journal of Health Geographics. 2004;3(3):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clarke P, Melendez R. National Neighborhood Data Archive (NaNDA): Neighborhood Socioeconomic and Demographic Characteristics of Census Tracts, United States, 2000-2010. . In: Archive NND, ed. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2019. [Google Scholar]
- 38.Vivot A, Power MC, Glymour MM, et al. Jump, Hop, or Skip: Modeling Practice Effects in Studies of Determinants of Cognitive Change in Older Adults. Am J Epidemiol. 2016;183(4):302–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.U.S. Census Bureau. 2008-2012 American Community Survey 5-year Estimates. 2013; https://www.census.gov/programs-surveys/acs/data.html.
- 40.United States Department of Agriculture. Rural-Urban Commuting Area Codes. 2019; https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. Accessed December 4, 2019.
- 41.Wood S. Generalized Additive Models: An Introduction with R. London, UK: Chapman & Hall; 2006. [Google Scholar]
- 42.Gelman A, Hill J. Data Analysis Using Regression and Multilevel/Hierarchical Models New York: Cambridge University Press; 2007. [Google Scholar]
- 43.Wood S, Scheipl F. gamm4: Generalized Additive Mixed Models using 'mgcv' and 'lme4'. R package version 0.2-5. . 2017; https://CRAN.R-project.org/package=gamm4.
- 44.R: A language and environment for statistical computing. R Foundation for Statistical Computing [computer program]. Vienna, Austria: 2020. [Google Scholar]
- 45.Besser LM, Rodriguez DA, McDonald N, et al. Neighborhood built environment and cognition in non-demented older adults: The Multi-Ethnic Study of Atherosclerosis. Soc Sci Med. 2018;200:27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Regnault A, Willgoss T, Barbic S, International Society for Quality of Life Research Mixed Methods Special Interest G. Towards the use of mixed methods inquiry as best practice in health outcomes research. J Patient Rep Outcomes. 2017;2(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Creswell JW, Klassen AC, Plano Clark VL, Smith KC. Best Practices for Mixed Methods Research in the Health Sciences. Washington, DC: Office of Behavioral Social Sciences Research; 2011. [Google Scholar]
- 48.Tariq S, Woodman J. Using mixed methods in health research. JRSM Short Rep. 2013;4(6):2042533313479197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barnett DW, Barnett A, Nathan A, et al. Built environmental correlates of older adults' total physical activity and walking: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Van Cauwenberg J, Cerin E, Timperio A, Salmon J, Deforche B, Veitch J. Park proximity, quality and recreational physical activity among mid-older aged adults: moderating effects of individual factors and area of residence. Int J Behav Nutr Phys Act. 2015;12:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clarke PJ, Ailshire JA, House JS, et al. Cognitive function in the community setting: the neighbourhood as a source of 'cognitive reserve'? Journal of epidemiology and community health. 2012;66(8):730–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Glazier RH, Creatore MI, Weyman JT, et al. Density, destinations or both? A comparison of measures of walkability in relation to transportation behaviors, obesity and diabetes in Toronto, Canada. PLoS One. 2014;9(1):e85295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Finlay JM. 'Walk like a penguin': Older Minnesotans' experiences of (non)therapeutic white space. Soc Sci Med. 2017;198:77–84. [DOI] [PubMed] [Google Scholar]
- 54.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet. 2020;396(10248):413–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Livingston G, Sommerland A, Orgeta V, et al. Dementia prevention, intervention, and care. The Lancet. 2017;390(10113):2673–2734. [DOI] [PubMed] [Google Scholar]
- 56.Alzheimer's Association. 2019 Alzheimer's disease facts and figures. Alzheimer's & Dementia. 2019;15(3):321–387. [DOI] [PubMed] [Google Scholar]
- 57.World Health Organization. Dementia: Key facts. 2020; https://www.who.int/news-room/fact-sheets/detail/dementia#:~:text=Worldwide%2C%20around%2050%20million%20people%20have%20dementia%2C%20with%20nearly%2060,is%20between%205%2D8%25. Accessed October 27, 2020.
- 58.Finlay J. Cities of (In)Difference: A Mixed-Methods Analysis of Place and Wellbeing in Later Life. Minneapolis, MN: Department of Geography, Environment, and Society, University of Minnesota; 2018. [Google Scholar]
- 59.Long SL, Freese J. Regression Models for Categorical Dependent Variables Using Stata. Second ed. College Station, TX: Stata Press; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.